Abstract
Introduction
Autism spectrum disorder (ASD), a heterogeneous neurodevelopmental disorder, impacts social experience and functioning throughout the lifespan. Although the postnatal phase of neuroplasticity has been a focus for early interventions in ASD, a second critical period in adolescence has emerged as a promising target for experience-dependent remediation. Interventions addressing the multidimensional construct of social cognition have also shown potential as a therapeutic approach. Yet, to date, evidence-based social cognitive interventions (SCIs) designed for adolescents with ASD are still lacking. In this review, we aim to survey and synthesize the extant literature on SCIs for adolescents with ASD in order to inform next steps for treatment research.
Methods
Using the PRISMA guidelines, we limited our queries to peer-reviewed, English-language journal articles describing SCI trials for adolescents with ASD using a randomized controlled design.
Results
Eighteen articles in total met our inclusion/exclusion criteria. We present and discuss these trials using the non-exclusive categories of group-based social skills interventions, experiential-based interventions, and computer-assisted interventions.
Limitations
To ensure a focus on adolescence, we excluded trials with teen-age participants if mean subject age was not between 12–18 years. Also, given the variability across studies in outcome measures, study designs, samples, and effect sizes, findings were incommensurable.
Conclusions
Several reviewed SCIs reported post-treatment improvements in varied domains but findings were inconsistent. Further investigations of existing and novel interventions are warranted; attention to assessing and improving long-term skill transfer is essential. Technology-assisted augmentations may improve treatment efficacy and ecological validity of therapeutic gains.
1. Introduction
Autism spectrum disorder (ASD) is a heterogeneous neurodevelopmental disorder (NDD) with diagnostic criteria specifying persistent deficits in social communication, social interaction, and restricted, repetitive patterns of behavior, interests, or activities (American Psychiatric Association, 2013). The prevalence of ASD in the U.S. has been on the rise, reaching a recent estimate of 1-in-54, with most diagnoses occurring during the preschool years (Maenner et al., 2020). Boys are more than four times as likely to be identified with ASD than girls, and amongst children with IQ scores available, one-third also have intellectual disability (ID). In addition to core symptoms, individuals with ASD often present with a variety of co-occurring medical, developmental, behavioral, or psychiatric conditions that further impact daily functioning and quality of life (Kuhlthau et al., 2017), with many comorbid conditions persisting across the lifespan (Lai et al., 2014).
Treatment approaches for ASD may include intensive behavioral therapy, medication, educational programming, and ancillary services such as speech/language, occupational, and physical therapy. Timing plays a significant role in therapeutic efficacy, and early intervention has been strongly emphasized so as to coincide with postnatal time-limited epochs of stimulus-driven neuroplasticity. Yet, a second key target for remediation occurs later in development during the mutable stage of adolescence (Ismail et al., 2017); this incipient area of intervention research holds great promise. The onset of puberty creates a cascade of hormonal changes that stimulate numerous structural and functional changes in the brain (Juraska and Willing, 2017). As such, adolescence is a period of heightened socio-affective experience-dependent learning and neural plasticity (Cohen Kadosh et al., 2013, Fuhrmann et al., 2015) that manifest as heightened regulation of emotional reactivity and increased social understanding. During this period, neural circuitry sensitive to social cognitive processes undergo adaptive change and maturation; these networks include regions involved in thinking about mental states (dorsal medial prefrontal cortex (PFC), temporoparietal junction), observing faces and biological motion (posterior superior temporal sulcus), applying social knowledge (anterior temporal cortex), and understanding the actions and emotions of others (inferior frontal gyrus) (Blakemore, 2008, Vetter et al., 2013).
For typically-developing (TD) individuals, the onset of novel, adolescent-specific challenges (e.g., forming caring and supportive relationships with peers, making independent decisions, acquiring autonomy from parents) and their success in accomplishing these tasks is predictive of adaptive functioning in adulthood (e.g., work competence, romantic competence) (Roisman et al., 2004). For individuals with ASD, social impairments in childhood may become more pronounced during adolescence when increasingly complex social demands exceed their competencies. Indeed, an estimated 30% of children with ASD experience functional setbacks when undergoing pubertal changes (Picci and Scherf, 2014). Adverse exposure to interpersonal situations and peer networks may preclude the experience of meaningful social interactions and the development of important social skills. Indubitably, further investigation at this juncture of potentially heightened susceptibility in adolescence is vital to the establishment of efficacious interventions for ASD.
Several areas of struggle for individuals with ASD are subsumed by the multidimensional construct of social cognition outlined as four partially-overlapping critical domains - emotion processing, social perception, theory of mind/mental state attribution, and attributional style/bias (Pinkham et al., 2014). Impairment in or across these domains while navigating a complex social world can have a substantial impact on individual functioning and long-term quality of life for persons with ASD. Accordingly, interest in interventions that address these domains of social cognition has been on the rise. Consistent with the trajectory of research in ASD, the development of social cognitive interventions (SCIs) for adolescents with ASD has lagged behind treatments designed for younger children and adults. Although some studies have included participants within the adolescent age range, those programs were rarely designed specifically for teenagers. Hence, the goals of this review are to survey and synthesize the extant literature on SCIs for adolescents with ASD in order to inform next steps for treatment research.
2. Methods
Search Strategy
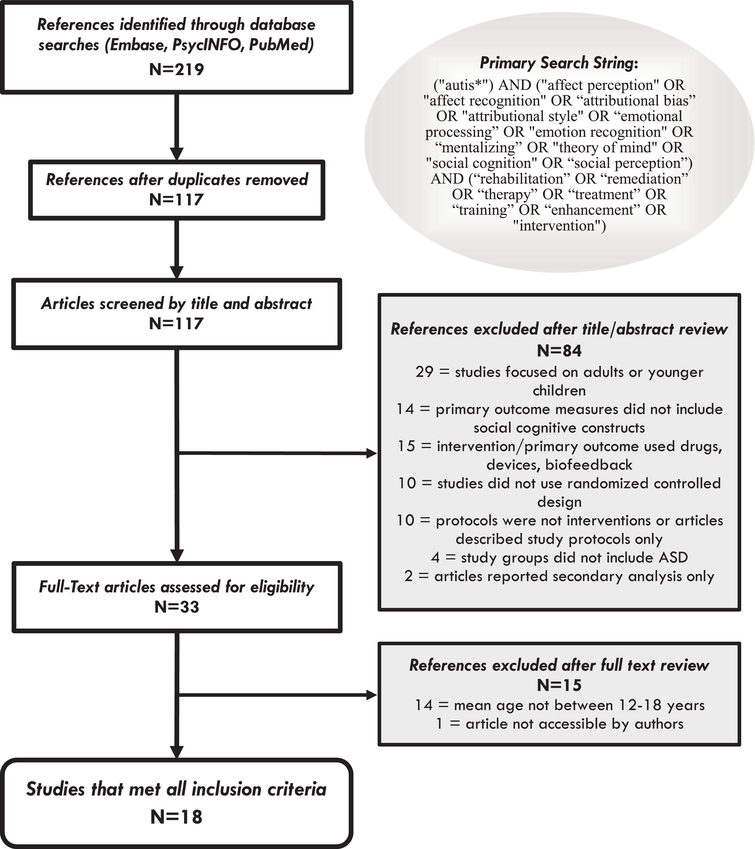
We conducted this review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (Moher et al., 2009). Our overarching search strategy involved querying electronic databases (Embase, Elsevier; PsycINFO, APA; PubMed, APA) with customized search strings, followed by manual filtering of query results using predefined inclusion and exclusion criteria (See Figure 1). In an effort to capture social-cognition-based interventions whether or not they were labeled as such, we included key domain terms as well as terms analogous to “interventions” and variations of “autism” in our queries. We used Boolean operators (AND, OR) to delineate our results.
Figure 1.
PRISMA Flow Diagram.
Eligibility Criteria and Study Selection
We first identified studies by restricting our search to peer-reviewed, English-language journal articles; non-human, review, and meta-analytic reports were excluded. We also included the MeSH term “adolescence” as an age group limiter which returned studies with any participants between 13–17 years of age. Ultimately, studies were included if they: (1) reported findings from randomized controlled trials (RCTs); (2) recruited and reported data for individuals with ASD diagnoses; (3) recruited and reported data for participant groups within the adolescent age-range; and (4) reported findings from an SCI. Studies were excluded if they (1) focused on adults or younger children; (2) did not include social cognitive constructs as an independent variable; or (3) included secondary analyses only. In order to reduce biological confounds due to the heterogeneity of study design and samples, we also excluded studies wherein the independent variables were primarily physiological, e.g., drugs (e.g., Oxytocin, Risperidone, d-Cycloserine), devices (tDCS, rTMS), neuroimaging (EEG, fMRI), physical therapy, or biofeedback.
Finally, all authors reviewed the remaining articles in-depth. Several investigations identified by our initial query included teen-age participants even though full study samples largely comprise adults or younger children. Thus, in order to better circumscribe the adolescent age group, we agreed to limit our review to studies in which the mean age of participants with ASD was between 12–18 years. Consensus for inclusion was reached after discussion with all authors involved.
3. Results
We conducted full database queries in February 2020. Our search strategy returned 117 unique results after duplicates were removed. After initial screening by the lead author (AT) and group review of titles and abstracts, 84 articles were excluded. We ruled out 14 additional reports because mean age of participants was not between 12–18 years, and 1 report was not reviewed because the full-text was inaccessible. Eighteen articles in total were included in the final review. Study design and key findings are presented and discussed below under the broad, non-exclusive categories of group-based social skills interventions, experiential-based interventions, and computer-assisted intervention; key details about study methods are presented in supplementary material.
Group-Based Social Skills Interventions (GSSI)
Over the last decade, group-based social skills interventions have grown in availability and popularity as a means to address social cognitive deficits in individuals with ASD. GSSIs vary considerably in their content, teaching strategy, mode of delivery, and intensity. However, often, GSSIs are informed by a cognitive behavioral therapy (CBT) framework and utilize behavioral modeling of a specific social skill, role play activities to practice skills, and individualized feedback on performance. Teaching strategies may employ structured lessons or in vivo skills-practice with differing levels and combinations of therapist, parent, peer, or teacher involvement. Whereas several systematic reviews have evaluated GSSIs for use in ASD (e.g., Gates et al., 2017, Wolstencroft et al., 2018), to our knowledge, none have assessed RCTs for the adolescent age-range specifically.
We identified 12 RCTs that used a GSSI approach and met our inclusion criteria. All of these trials included ASD participants with Verbal IQs > 70 or the equivalent; this is not surprising given that GSSIs are generally designed for high-functioning individuals. Six reports described implementations of PEERS (Program for the Education and Enrichment of Relationship Skills), one of the few evidence-based social skills programs available for adolescents with ASD. Five trials applied the following manualized, group-based, in-person programs: Multimodal Anxiety and Social Skills Intervention (MASSI), Social Skills Group Training (SSGT; “KONTAKT”), and SOSTA-FRA (Social Skills Training Autism-Frankfurt). One additional study used a multi-family group psychoeducation approach (Transitioning Together) designed for families of individuals with ASD during the transition to adulthood.
PEERS (Program for the Education and Enrichment of Relationship Skills) utilizes principles of CBT to teach skills for solving real-life social dilemmas, appraising affect and social contexts, and initiating and maintaining conversations while receiving feedback from peers and clinicians. Structured practice interactions during socialization activities (e.g., playing sports, games) are integrated into the curricula. Concurrently, parents attend separate sessions and are taught how to assist teens in making and keeping friends by providing feedback during weekly socialization homework assignments. In the initial RCT testing PEERS, Laugeson and colleagues (2011) reported gains in social skills and responsiveness that were largely maintained at a 14-week follow-up assessment. Subsequently, Schohl et al. (2013) completed an independent replication and extension of PEERS with additional measures of social anxiety and problem behaviors. This treatment group also demonstrated social skills improvement along with a reduction in social anxiety, core ASD symptoms, and problem behaviors. Overall, findings contributed to knowledge of treatment efficacy and support the application of PEERS as an intervention. However, one potential caveat is the use of TASSK (Test of Adolescent Social Skills Knowledge), a self-report measure created by the developers of PEERS (Laugeson et al., 2009), to assess PEERS outcomes. TASSK tests knowledge of specific, key social skills that are taught during the intervention. Ideally an outcome measure would also gauge real-world skills application and generalizability to novel situations. In a recent trial, Matthews and colleagues (2018) contrasted a novel, peer-mediated PEERS (PwP) against the traditional PEERS curriculum and a delayed treatment control group. Findings suggest that PwP is feasible and may have a modest advantage in improving social skills knowledge and social functioning relative to traditional PEERS. RCTs of adaptations of PEERS to Hebrew, Chinese, and Korean (Rabin et al., 2018, Shum et al., 2018, Yoo et al., 2014) have also reported significant social skills improvements for their treatment groups along with cross-cultural validation of the translated/adapted versions.
MASSI (Multimodal Anxiety and Social Skills Intervention) was developed in response to the high co-occurrence of social anxiety disorder with ASD and evidence that social disability in ASD may be driven in part by social anxiety (White et al., 2012). MASSI uses CBT strategies to target concurrent anxiety (e.g., exposure, cognitive restructuring, psychoeducation) and social skills deficits (e.g., modeling, feedback, role-play practice) with specific, individualized content selected by the therapist. All group sessions include one unaffected peer tutor volunteer. White and colleagues conducted a feasibility trial of MASSI in 30 adolescents with ASD and anxiety symptoms of moderate or greater severity. Their data suggest the possibility that this intervention may have more specific effects on core ASD-related social deficits than on anxiety symptoms, such that participants improved significantly on the Social Responsiveness Scale (SRS) but not on anxiety measures. Subsequently, Ireri et al. (2019) adapted MASSI for a special educational setting in Kenya; parents, teachers, and 40 children with ASD were randomized by school to either MASSI or treatment as usual (1 active and 1 control school). This version of MASSI applied a higher treatment dose by including a second phase of 20 more sessions focused on skills practice. Results from this trial demonstrated significant improvements in both ASD-related social impairment and anxiety, suggesting that adding teacher-mediated skills practice and additional training sessions may improve outcomes. These findings support the cross-cultural expansion of MASSI to a school-based implementation model. It should be noted, however, that no measure of cognitive function was reported and concurrent interventions were not tracked in this trial.
SOSTA-FRA (Social Skills Training Autism-Frankfurt), a highly structured, CBT-based GSSI developed in Germany, combines computer-assisted and social learning methods of teaching and practicing social skills. Freitag et al. (2016) conducted a multicenter RCT comparing SOSTA-FRA to treatment as usual that featured a rigorous design, including sample characterization using ADOS and IQ testing, large sample size, follow-up through 3 months, and a naturalistic inclusion criterion that allowed concurrent pharmacotherapy and psychosocial interventions.. Attrition was low and therapy quality was rated positively by participants. Pre-treatment parent-rated (p)SRS and IQ were positively associated with stronger improvement at follow-up. The authors also report a descriptive observation that female participants improved more than males on the pSRS. However, due to the high male:female ratio common to ASD studies, power was too low to compare effect sizes. These findings underscore the importance of assessing the relationship between IQ, sex, and SCI outcomes in future trials.
KONTAKT or SSGT (Social Skills Group Training), a Swedish CBT-based GSSI for youth with ASD, includes exercises in social skills as well as discussions of social cognition, social interaction, self-reflection, and descriptions of self and others. The program is conducted in cooperation with both parents and teachers and can be delivered in a brief (12 sessions) or long (24 sessions) format. Each therapy group consists of 4–8 youth (child or adolescent sub-groups) with two group leaders. Similar to SOSTA-FRA, KONTAKT trials featured a rigorous design including multiple sites, large N, follow-up through 3 months, ADOS characterization, and IQ assessment, while affording a pragmatic implementation (natural clinical setting, common comorbidities allowed, delivered by regular clinic staff). Choque-Olsson and colleagues (2017) compared KONTAKT to treatment as usual and reported that significant treatment effects on primary outcome measures were limited to pSRS-2 for the adolescent and female subgroups, suggesting that age and gender may moderate the effects of GSSIs for ASD. While findings were moderate and inconsistent, this trial demonstrated the feasibility of delivering KONTAKT in real-world mental health service settings. Subsequently, Jonsson and colleagues (2018) conducted the long form (24 sessions) of KONTAKT with a comparatively smaller group of youth with ASD (N=50). Scores on the pSRS-2 revealed large effects post-treatment which were maintained at follow-up, indicating that dosing and duration of treatment play key roles in SCI efficacy.
Transitioning Together is a multi-family group psychoeducation intervention designed to reduce family distress and improve social functioning for adolescents with ASD. In a preliminary evaluation, DaWalt et al. (2017) found significant improvements in social interactions following treatment for the intervention group, but not for controls. Also, parental depressive symptoms decreased and problem-solving improved for parents in the intervention condition. Notably, IQ was significantly higher in the intervention group despite random assignment; this may have influenced outcomes and future studies should consider the role of cognitive ability as a moderating variable.
Experiential-Based Interventions
Many existing SCIs rely on systematic instructional methods to address social cognition deficits associated with ASD. However, embedded opportunities for practice in real-world situations are limited; while structured interventional context may confer a therapeutic effect, the predominantly didactic approaches do not address ecological barriers to application. For example, an individual with ASD may not be able to practice a newly acquired social skill with peers who reject or ignore them. Interventions that take these obstacles into consideration may improve transfer of skills to novel, everyday interactions.
The START (Social Tools And Rules for Teen) program (Vernon et al., 2017) is an immersive socialization intervention that focuses on improving social motivation, insight, and skills by incorporating a club-like environment that emphasizes learning through experiential and interactive lessons. Adolescent participants, college-aged social facilitators, high school peers, and parents (only at end of session) attended each group. Significant improvements between pre- and post-intervention assessments were reported for multiple social cognitive outcome measures, suggesting that experience-based SCIs can help improve social readiness in adolescents with ASD. One selection bias concern is that, despite random assignment, the treatment group endorsed significantly lower adolescent-reported SSIS scores at pre-intervention and this may have skewed results.
Strickland et al. (2013) evaluated JobTIPS, an internet-accessed tool designed to teach job interview skills to nearing transition-age individuals. Treatment included multimedia educational content with ToM-based guidance, video models, and visual supports for 1 week and virtual reality practice session with avatars led remotely by an experienced clinician. Training was associated with significant improvements in the verbal content of responses to job interview questions along with a trend toward improving the delivery (e.g., posture, eye contact, facial expression) of those responses. This trial is one of the few to assess and demonstrate generalization, such that JobTIPS afforded skill-transfer to face-to-face mock interviews that simulate real-world situations.
CONTACT (Conflict Orientation and Negotiation Training Among Children and Teens), a computerized video modeling and video self-modeling application, was developed to improve conflict negotiation strategies in adolescents with ASD who may be inclined toward avoidance of social conflict (Hochhauser et al., 2017). Negative socialization experiences often lead to poor quality peer friendships or isolation. Video modeling interventions typically involve watching video demonstrations of an adaptive behavior before imitation; video self-modeling involves watching and learning from one's own positive behavior. CONTACT was designed for pairs of participants, matched on similarities in their social and cognitive abilities, to engage in training with mediation (e.g., prompts, guided questions, and explanations) by an experienced moderator. One advantage to this experiential approach is that it enables participants to practice their adaptive responses to socially-relevant stimuli in simulated conflict situations that may be less threatening than real-world interactions. Hochhauser and colleagues reported significant improvements for the treatment group in their self-reported negotiation attitudes and behaviors, specifically in their self-confidence, communication factors, and willingness to engage in cooperative negotiation.
The Referential Communication Training Program (Olivar-Parra et al., 2011) addressed participants’ ability to select and organize information for a communicative exchange. Training sessions included pairs of verbal-mental-age and sex-matched ASD and TD participants as speakers and listeners with an adult to guide and facilitate learning. Notably, this trial is one of the few that did not exclude participants for ID. Although introducing a wide range of verbal ages and cognitive levels amongst participants impacts interpretation of results from a small sample (N=20 pairs), the inclusion of varying levels of cognitive ability is more reflective of the heterogeneous presentation of ASD. Further, speakers in the trained and untrained groups did not differ in chronological age, level of receptive language, IQ, or number of ASD symptoms. Finding showed significant increases in the complexity of emitted messages in the treatment group; however, these improvements were not maintained at the follow-up generalization stage.
Computer-Assisted Interventions
Rapid progress in the fields of technology offer tremendous possibilities for innovation in treatment for individuals with ASD. In recent years, computer-assisted and other technology-aided approaches to supplement existing therapies or as the primary delivery modality have been proliferating, with varying levels of efficacy and generalizability. Computer-based technologies may be particularly beneficial to individuals with ASD because of their capacity to limit distractions from extraneous sensory stimuli, to provide consistent and predictable responses, and to offer clearly defined tasks. Surprisingly, in addition to the CONTACT program described earlier, only two RCTs fit our criteria, in large part because we excluded programs where the mean age of participants was not within the adolescent age-range.
The earliest trial meeting our criteria (Silver and Oakes, 2001) used The Emotion Trainer, an interactive multimedia computer program with corrective feedback; significant improvements were reported on emotion recognition in cartoon but not human faces for the experimental group. Although these gains did correlate significantly with the number of times each participant used the computer program, it was unclear whether these skills would be transferred to real-world situations.
More recently, Fage and colleagues (2018) tested a tablet-based intervention using a set of mobile applications, School+, to support school inclusion of children with ASD in mainstream classrooms. Assistive and rehabilitation applications were used for three months by 33 youth (ASD: 14, ID: 19 ) from special-education classrooms during their first inclusion in mainstream classrooms in secondary schools. Fifteen children with ASD, who were not equipped with School+, participated as a comparative group. Both tablet-equipped groups exhibited significant improvements on socio-cognitive functioning measures. Tablet-ASD participants, but not Tablet-ID participants, exhibited improvements on socio-adaptive behaviors and social response. It is difficult to draw conclusions about the use of School+ in individuals with ID as a non-equipped ID comparative group was not included in the study. However, in contrast to the equipped-ASD group, the non-equipped ASD group demonstrated no significant changes across time. These findings provide support for the efficacy of using the School+ program with individuals with ASD.
4. Discussion
Summary of findings
For this systematic review, we aimed to ascertain the current state of knowledge in the development of social cognitive interventions for adolescents with ASD. Altogether, eighteen studies met our inclusion criteria. Two-thirds of the publications used CBT-informed group-based social skills interventions; half of those applied versions of PEERS. A small number of programs integrated experiential-based learning paradigms to augment CBT approaches by enabling real-world practice and reflection. Technological advancements such as virtual reality platforms have emerged as a means to include remote interactions between participants and clinician or teacher facilitators (e.g., Strickland et al., 2013). Immersive technology that affords opportunities for practice in a simulated but realistic environments may improve ecological validity of programs. Further, the use of computer-assisted modalities to enhance existing interventions may increase their versatility and overall appeal, enabling individualized mediation and facilitation by trained professionals (Khan et al., 2019).
Several shortcomings exist in the field across all ages. For example, most GSSIs are time and resource intensive so sample sizes tend to be small, thus limiting power. In-person treatments may be geographically inaccessible to families who live in remote areas. While technology-assisted interventions may offset some of these constraints, they may also require a means to connect to internet. Further, most SCIs have been designed for and tested in individuals without ID (IQ >70), effectively neglecting one-third of individuals with ASD. Moreover, given the prevalence ratio of about 4 males for every 1 female diagnosed with ASD, it is not surprising that SCIs have been evaluated with more males than females. However, research suggests that IQ and sex may moderate SCI outcomes for ASD (Choque-Olsson et al., 2017, Freitag et al., 2016), necessitating further investigation with these under-sampled individuals.
Limitations
The present systematic review has limitations. In order to restrict our results to SCIs for adolescents with ASD, we did not include several trials that included teen-age participants but did not focus on the adolescent age group. The majority of therapeutic advances in the field have been developed for younger children or adults; often adolescent trials are essentially extensions of child- or adult-directed programs. However, as noted, the period during and after puberty is a unique developmental stage and considering adolescent-specific variables in treatment design and outcomes is warranted. In addition, given the diversity of social, cognitive, and clinical assessments used across investigations, as well as the heterogeneity of study designs, samples, and effect sizes, outcome findings were incommensurable.
5. Conclusions & Future Directions
Findings from our review highlight the paucity of social cognitive interventions designed specifically for adolescents with ASD. Although much attention is given to ASD in early childhood (Wolff et al., 2018), the interval of neuroplasticity between puberty and the transition to adulthood affords an opportunity to capitalize on the dynamic structural and functional reorganization of neurons susceptible to developmental and experiential demands (Blakemore, 2010). In particular, for individuals with NDDs, neuroplasticity may subserve the compensatory mechanisms modulating symptom severity (Dow-Edwards et al., 2019). Notably, PFC, the nucleus of higher-level cognitive functions, undergoes the most protracted development; synaptic spines within PFC exhibit overproduction during childhood with remodeling and pruning of spines continuing beyond adolescence and throughout the third decade of life (Petanjek et al., 2011). Hence, interventions directed at this sensitive phase of neurodevelopment may result in more significant impact on long-term outcomes.
Potential areas for advancement in the development of SCIs for adolescents with ASD are substantial. We have identified several promising areas that warrant further investigation. For example, a primary concern in the application of treatment programs is whether skills acquired during therapy transfer to real-world settings over time. Extended follow-up of participants would help evaluate the longevity and generalizability of therapeutic gains. SCIs that incorporate simulated or real-world practice of skills have shown favor; technology-based augmentations of existing evidence-based strategies may not only enhance treatment uptake but also enable remote delivery of efficacious interventions.
Supplementary Material
HIGHLIGHTS.
A second window of neuroplasticity that occurs in adolescence has emerged as a promising target for experience-dependent remediation in autism spectrum disorder (ASD)
Evidence-based, social cognitive interventions (SCIs) for ASD that target the critical period between puberty and the transition to adulthood are lacking
Extant treatments that address the multidimensional construct of social cognition in adolescents with ASD include group-based social skills interventions, experiential-based interventions, and computer-assisted interventions
Some programs demonstrated post-treatment improvement but findings are inconsistent; further research is needed to assess and improve long-term transfer of skills and to develop technology-assisted tools that augment efficacy and ecological validity of treatments
Acknowledgments
Role of the Funding source
This study was supported by the National Institute of Mental Health under Award Numbers R43 1 R43 MH121209-01 (BB, CC) and R01MH115046-02 (SJ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Conflict of Interest
BB is Senior Scientist at Posit Science, a company that produces cognitive training and assessment software. CC is a site principal investigator for a Small Business and Innovation Research grant awarded to Posit Science that tests the effects of a cognitive behavioral digital intervention for adolescents with social anxiety. SJ, AT, and SF report no conflict of interest to the therapeutic modalities and topic of this review.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association, A. (2013). Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Blakemore SJ (2010). The Developing Social Brain: Implications for Education. Neuron, 65(6), 744–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore SJ (2008). The social brain in adolescence. Nat Rev Neurosci, 9(4), 267–277. [DOI] [PubMed] [Google Scholar]
- Choque-Olsson N, Flygare O, Coco C, Görling A, Råde A, Chen Q, … Bölte S (2017). Social Skills Training for Children and Adolescents With Autism Spectrum Disorder: A Randomized Controlled Trial. Journal of the American Academy of Child & Adolescent Psychiatry, 56(7), 585–592. [DOI] [PubMed] [Google Scholar]
- Cohen Kadosh K, Linden DE, & Lau JY (2013). Plasticity during childhood and adolescence: innovative approaches to investigating neurocognitive development. Dev Sci, 16(4), 574–583. [DOI] [PubMed] [Google Scholar]
- DaWalt LS, Greenberg JS, & Mailick MR (2017). Transitioning Together: A Multi-family Group Psychoeducation Program for Adolescents with ASD and Their Parents. Journal of Autism and Developmental Disorders, 48(1), 251–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dow-Edwards D, MacMaster FP, Peterson BS, Niesink R, Andersen S, & Braams BR (2019). Experience during adolescence shapes brain development: From synapses and networks to normal and pathological behavior. Neurotoxicology and Teratology, 76. [DOI] [PubMed] [Google Scholar]
- Fage C, Consel CY, Balland E, Etchegoyhen K, Amestoy A, Bouvard M, & Sauzéon H (2018). Tablet Apps to Support First School Inclusion of Children With Autism Spectrum Disorders (ASD) in Mainstream Classrooms: A Pilot Study. Frontiers in Psychology, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freitag CM, Jensen K, Elsuni L, Sachse M, Herpertz-Dahlmann B, Schulte-Rüther M, … Cholemkery H (2016). Group-based cognitive behavioural psychotherapy for children and adolescents with ASD: the randomized, multicentre, controlled SOSTA - net trial. Journal of Child Psychology and Psychiatry, 57(5), 596–605. [DOI] [PubMed] [Google Scholar]
- Fuhrmann D, Knoll LJ, & Blakemore S-J (2015). Adolescence as a Sensitive Period of Brain Development. Trends in Cognitive Sciences, 19(10), 558–566. [DOI] [PubMed] [Google Scholar]
- Gates JA, Kang E, & Lerner MD (2017). Efficacy of group social skills interventions for youth with autism spectrum disorder: A systematic review and meta-analysis. Clinical Psychology Review, 52, 164–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochhauser M, Weiss PL, & Gal E (2017). Enhancing conflict negotiation strategies of adolescents with autism spectrum disorder using video modeling. Assistive Technology, 30(3), 107–118. [DOI] [PubMed] [Google Scholar]
- Ireri NW, White SW, & Mbwayo AW (2019). Treating Anxiety and Social Deficits in Children with Autism Spectrum Disorder in Two Schools in Nairobi, Kenya. Journal of Autism and Developmental Disorders, 49(8), 3309–3315. [DOI] [PubMed] [Google Scholar]
- Ismail FY, Fatemi A, & Johnston MV (2017). Cerebral plasticity: Windows of opportunity in the developing brain. European Journal of Paediatric Neurology, 21(1), 23–48. [DOI] [PubMed] [Google Scholar]
- Jonsson U, Olsson NC, Coco C, Görling A, Flygare O, Råde A, … Bölte S (2018). Long term social skills group training for children and adolescents with autism spectrum disorder: a randomized controlled trial. European Child & Adolescent Psychiatry, 28(2), 189–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juraska JM, & Willing J (2017). Pubertal onset as a critical transition for neural development and cognition. Brain Res, 1654(Pt B), 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan K, Hall CL, Davies EB, Hollis C, & Glazebrook C (2019). The Effectiveness of Web-Based Interventions Delivered to Children and Young People With Neurodevelopmental Disorders: Systematic Review and Meta-Analysis. Journal of Medical Internet Research, 21(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhlthau KA, McDonnell E, Coury DL, Payakachat N, & Macklin E (2017). Associations of quality of life with health-related characteristics among children with autism. Autism, 22(7), 804–813. [DOI] [PubMed] [Google Scholar]
- Lai M-C, Lombardo MV, & Baron-Cohen S (2014). Autism. The Lancet, 383(9920), 896–910. [DOI] [PubMed] [Google Scholar]
- Laugeson EA, Frankel F, Gantman A, Dillon AR, & Mogil C (2011). Evidence-Based Social Skills Training for Adolescents with Autism Spectrum Disorders: The UCLA PEERS Program. Journal of Autism and Developmental Disorders, 42(6), 1025–1036. [DOI] [PubMed] [Google Scholar]
- Laugeson EA, Frankel F, Mogil C, & Dillon AR (2009). Parent-assisted social skills training to improve friendships in teens with autism spectrum disorders. J Autism Dev Disord, 39(4), 596–606. [DOI] [PubMed] [Google Scholar]
- Maenner MJ, Shaw KA, Baio J, EdS, Washington A, Patrick M., … Dietz PM (2020). Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016: MMWR Surveill Summ, 69(4), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews NL, Orr BC, Warriner K, DeCarlo M, Sorensen M, Laflin J, & Smith CJ (2018). Exploring the Effectiveness of a Peer-Mediated Model of the PEERS Curriculum: A Pilot Randomized Control Trial. Journal of Autism and Developmental Disorders, 48(7), 2458–2475. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj, 339(July21 1), b2535–b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivar-Parra J-S, De-La-Iglesia-Gutiérrez M, & Forns M (2011). Training Referential Communicative Skills to Individuals with Autism Spectrum Disorder: A Pilot Study. Psychological Reports, 109(3), 921–939. [DOI] [PubMed] [Google Scholar]
- Petanjek Z, Judaš M, Šimic G, Rašin MR, Uylings HBM, Rakic P, & Kostovic I (2011). Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proceedings of the National Academy of Sciences, 108(32), 13281–13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picci G, & Scherf KS (2014). A Two-Hit Model of Autism. Clinical Psychological Science, 3(3), 349–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, Green MF, Buck B, Healey K, & Harvey PD (2014). The social cognition psychometric evaluation study: results of the expert survey and RAND panel. Schizophr Bull, 40(4), 813–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin SJ, Israel-Yaacov S, Laugeson EA, Mor-Snir I, & Golan O (2018). A randomized controlled trial evaluating the Hebrew adaptation of the PEERS® intervention: Behavioral and questionnaire-based outcomes. Autism Research, 11(8), 1187–1200. [DOI] [PubMed] [Google Scholar]
- Roisman GI, Masten AS, Coatsworth JD, & Tellegen A (2004). Salient and Emerging Developmental Tasks in the Transition to Adulthood. Child Development, 75(1), 123–133. [DOI] [PubMed] [Google Scholar]
- Schohl KA, Van Hecke AV, Carson AM, Dolan B, Karst J, & Stevens S (2013). A Replication and Extension of the PEERS Intervention: Examining Effects on Social Skills and Social Anxiety in Adolescents with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 44(3), 532–545. [DOI] [PubMed] [Google Scholar]
- Shum KK-M, Cho WK, Lam LMO, Laugeson EA, Wong WS, & Law LSK (2018). Learning How to Make Friends for Chinese Adolescents with Autism Spectrum Disorder: A Randomized Controlled Trial of the Hong Kong Chinese Version of the PEERS® Intervention. Journal of Autism and Developmental Disorders, 49(2), 527–541. [DOI] [PubMed] [Google Scholar]
- Silver M, & Oakes P (2001). Evaluation of a new computer intervention to teach people with autism or Asperger syndrome to recognize and predict emotions in others. Autism, 5(3), 299–316. [DOI] [PubMed] [Google Scholar]
- Strickland DC, Coles CD, & Southern LB (2013). JobTIPS: A Transition to Employment Program for Individuals with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 43(10), 2472–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon TW, Miller AR, Ko JA, Barrett AC, & McGarry ES (2017). A Randomized Controlled Trial of the Social Tools And Rules for Teens (START) Program: An Immersive Socialization Intervention for Adolescents with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48(3), 892–904. [DOI] [PubMed] [Google Scholar]
- Vetter NC, Leipold K, Kliegel M, Phillips LH, & Altgassen M (2013). Ongoing development of social cognition in adolescence. Child Neuropsychol, 19(6), 615–629. [DOI] [PubMed] [Google Scholar]
- White SW, Ollendick T, Albano AM, Oswald D, Johnson C, Southam-Gerow MA, … Scahill L (2012). Randomized Controlled Trial: Multimodal Anxiety and Social Skill Intervention for Adolescents with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 43(2), 382–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JJ, Jacob S, & Elison JT (2018). The journey to autism: Insights from neuroimaging studies of infants and toddlers. Dev Psychopathol, 30(2), 479–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolstencroft J, Robinson L, Srinivasan R, Kerry E, Mandy W, & Skuse D (2018). A Systematic Review of Group Social Skills Interventions, and Meta-analysis of Outcomes, for Children with High Functioning ASD. Journal of Autism and Developmental Disorders, 48(7), 2293–2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo H-J, Bahn G, Cho I-H, Kim E-K, Kim J-H, Min J-W, … Laugeson EA (2014). A Randomized Controlled Trial of the Korean Version of the PEERS®Parent-Assisted Social Skills Training Program for Teens With ASD. Autism Research, 7(1), 145–161. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.