Abstract
Background:
After SARS-CoV-2 vaccines become available, they will be deployed to many countries with limited immunization systems.
Methods:
We conducted a cold chain capacity assessment of a simulated country in the WHO African Region. We combined region-specific data regarding immunization, population, healthcare workforce, and cold storage capacity (upper and lower range and quartile values for national and subnational levels). We used seasonal influenza vaccines as proxies for SARS-CoV-2 vaccines. We evaluated the increase in vaccine doses to be administered, doses administered per vaccinator, and cold storage volumes for SARSCoV-2 campaigns targeting risk groups compared to routine immunization baselines.
Findings:
Compared to routine immunization, a SARS-CoV-2 vaccination campaign would increase monthly doses administered when targeting risk groups: ≥65 years (29.9%), chronic diseases patients (101.5%), and healthcare workers (1.2%). SARS-CoV-2 vaccination campaigns would increase doses administered per vaccinator for risk groups: ≥65 years (32.5%), chronic diseases patients (110.4%), or healthcare workers (1.4%). Routine vaccine volumes already exceed national level storage capacity for at least 75% of African Region countries, but subnational levels would have sufficient storage capacity for SARS-CoV-2 vaccines in all but the lower 25% of African Region countries.
Interpretation:
SARS-CoV-2 vaccination campaigns would substantially increase doses per vaccinator and cold chain capacity requirements over routine immunization baselines. Pandemic vaccination campaigns would add volume to national level stores already at their limits, but substantial capacity exists at subnational levels for SARS-CoV-2 vaccines. Immediate attention to strengthening delivery systems is essential to support pandemic vaccine responses in the African Region.
Funding:
None
BACKGROUND
There is a robust pipeline of SARS-CoV-2 vaccine candidates in various stages of preclinical and clinical development.1,2 While the challenges of developing a vaccine at an accelerated timeline for this newly-emerged pathogen have been well described,2 less attention has been given to the challenges of vaccine deployment and delivery. Lessons from the 2009 H1N1 pandemic vaccine deployment may be instructive for the current situation. In a survey about the 2009 H1N1 pandemic response published in 2013, WHO African Region (subsequently called “African Region”) countries reported 62% overall utilization of the 32,096,290 deployed H1N1 vaccine doses,3,4 covering approximately 1% of the region’s population.4 Most of these vaccine doses arrived after June 2010, despite the fact that H1N1 vaccines were prequalified by WHO for procurement beginning November 2009.3 This delay, largely due to obstacles in vaccine deployment and delivery, resulted in many preventable illnesses.
The SARS-CoV-2 pandemic has already caused more severe health impact than the 2009 influenza pandemic,5 and national governments, and technical and partner agencies should aspire to higher goals than the population coverage achieved during the prior pandemic.4 A WHO report following the 2009 pandemic concluded that existing health systems, immunization infrastructures, and deployment training played key roles during the vaccine response.6 Critical to immunization infrastructure is the cold chain, defined as the series of actions and equipment necessary to maintain a vaccine within a specific low temperature range from production to the point of administration. While the number of deployed H1N1 vaccine doses covered only a fraction of at-risk populations identified, 29% of countries of the WHO African Region reported having insufficient cold chain and logistics capacity for a comprehensive H1N1 response.4
Since 2014, a concerted global effort has improved cold chain infrastructure in developing countries,7,8 which may facilitate a more rapid, widespread, and equitable SARS-CoV-2 vaccine response. We undertook this study to investigate the impact SARS-CoV-2 vaccination programs would have on vaccine delivery and storage systems in the WHO African Region. Our goal was to assess the operational feasibility of mass vaccination programs targeting SARS-CoV-2 risk groups.
METHODS
This analysis is similar to cold chain capacity assessments that are performed routinely by countries in preparation for new vaccine introductions.9 Rather than describe any individual country or countries, we simulated a 20 million population country using the 2017 age distribution for the WHO African Region.10 We compared the number of doses and vaccine storage volumes required for routine immunization alone and with SARS-CoV-2 mass vaccination campaigns. We then compared the required vaccine storage volumes for both scenarios to available cold storage capacities from countries in the African Region. Our outcomes of interest included the monthly percentage increases in vaccine doses to be administered, doses administered per vaccinator, and cold storage volume requirements for SARS-CoV-2 mass vaccination campaigns compared to routine immunization baselines.
Immunization strategies
We used a standard routine immunization schedule for the simulated country based on current WHO policy recommendations (Supplemental Table 1).11 We then adopted a SARS-CoV-2 vaccination campaign strategy targeting the following risk groups: persons aged ≥65 years, persons with certain chronic medical conditions (chronic diseases), healthcare workers (HCWs), and all risk groups combined.12 We assumed the SARS-CoV-2 vaccination campaign would span 4 months in duration and would require two doses, one month apart. To evaluate the fraction of the population in the chronic diseases group, we applied age-based estimates of comorbid risk factors for severe SARS-CoV-2 illness specific to the African Region.13 For HCWs, we used WHO estimates of skilled health personnel for the African Region, distributing these workers evenly across ages 20 through 64 years.14 For the all risk groups combined category, we assumed HCWs had the same prevalence of chronic diseases as the general population and adjusted to avoid double counting.
Vaccine storage
We identified WHO prequalified routine vaccine products,15 and we recorded the cold storage volumes required per dose in multi-dose vials for the standard routine immunization schedule (Supplemental Table 1). As no licensed SARS-CoV-2 vaccines are available, we adopted a proxy of cold storage volumes required for WHO prequalified influenza vaccines in multi-dose vials (10 doses per vial).15 Cold storage volume is the total volume of vaccines maintained at refrigerated temperatures throughout storage and transport. Cold storage in countries is organized by levels, with the national level being where procured vaccines are received and stored before distribution to subnational levels (region, district, and health facility). Vaccines (and diluents, for reconstituted products) are produced by the manufacturer in vials or other primary packaging that are then packed together in labeled boxes called “secondary packaging”.15 Products in secondary packaging are packed in cartons called “tertiary packaging”.15 Vaccines are typically maintained in tertiary packaging at the national level.16 Tertiary packaging volumes per dose are often ten times the secondary packaging volumes per dose due to additional insulation and thermal packing materials. At subnational levels, packaging materials are removed and vaccines are stored in their secondary packaging.16,17 Cold storage temperature for routine vaccines is typically 2° to 8°C, although some more thermostable products are becoming available.15 Vaccine vials used in most developing countries carry individual thermo-chemical temperature monitors that indicate when a vial has been outside of the recommended storage temperature range and should be discarded.18,19
Vaccine delivery
We estimated vaccine storage volumes using WHO tools and guidance.9,15,17,18,20 We compared routine immunization to SARS-CoV-2 vaccination campaigns according to evidence-based assumptions about vaccine wastage (doses that are damaged or unused),21 reserve stock (excess supply in case of increased demand or stock outs),9,18,22 and resupply intervals (Supplemental Table 2).20 In the case of SARS-CoV-2 vaccines, we assumed 7.5% wastage, 0% reserve stock and monthly resupply intervals given high global demand and limited supply. We received summary cold storage capacity data from Gavi, the Vaccine Alliance, for African Region countries that are eligible to receive Gavi support. These data included the minimum, 25th percentile, 50th percentile, 75th percentile, and maximum values of total country storage capacities, as well as the median proportion of national level stores and health facility level stores to total country capacity. For comparisons, capacity data were standardized by dividing the total cold storage capacity by the population of children aged < 2 years in each country.
Analysis
We calculated the monthly doses and cold storage volumes required for routine immunization programs and SARS-CoV-2 vaccination campaigns to reach 90% of target populations.17 We developed a vaccine flow-down schematic (Figure 1) to depict the quantity of routine vaccine doses maintained at each immunization system level by month under normal circumstances and used this to calculate the total quantity of vaccine doses and their storage volumes at each level. To assess the feasibility of storing SARS-CoV-2 vaccines, we compared the anticipated vaccine volumes for routine immunization and SARS-CoV-2 vaccination campaigns to actual vaccine cold storage capacities at national and subnational levels under normal circumstances. We defined “immunization program workloads” as the doses delivered per vaccinator. To determine this, we calculated the number of monthly doses for each activity divided by the estimated number of vaccinators available in the country. We calculated the median nurse density per capita from African Region countries (7.48 per 10,000 population) multiplied by the proportion of nurses estimated to provide immunization services (43%).14,23 We assumed baseline 3% nurse absenteeism and an additional 8% absenteeism for the SARS-CoV-2 pandemic months.24,25 To place results within the global context, we used median number of vaccinators per capita from other WHO regions calculated similarly. For the monthly comparisons and time series, we assumed constant routine immunization demand throughout the year and constant SARS-CoV-2 immunization demand during a mass vaccination campaign of four months duration. We performed all analyses using standard spreadsheet software including the made-for-purpose “WHO Vaccine Volume Calculator 2012” (Microsoft Corp, Redmond, WA, US).26 As there was no involvement of human participants or personal identifiable information, institutional review board approval was not required.
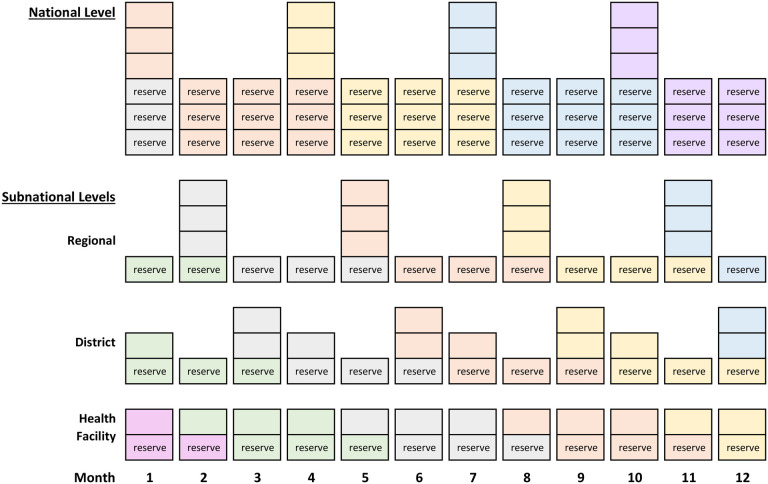
Figure 1. Schematic describing vaccine flow-down through the immunization system.
Notes:
a. Each color represents a supply shipment as it moves through the immunization system.
b. Each box represents routine vaccine doses to immunize the target population in one month, except reserve stock boxes at the health facility level which represent routine vaccine doses for 0.5 months.
c. Resupply occurs every three months at national, regional, and district levels, and monthly at the health facility level.
d. Reserve stock (excess supply in case of increased demand or stock outs) is three months at the national level, one month at regional and district levels, and 0.5 months at health facility level.
e. Vaccines stored at the national level use tertiary packaging volumes while vaccines stored at subnational levels use secondary packaging volumes.
f. This schematic does not depict stock rotations which would preferentially use vaccines received earlier.
Role of the funding source
This work had no specific funding support.
RESULTS
Description of population and vaccination target groups
We simulated a country of 20 million people in the WHO African Region (Table 1). The percentage of the total population within each risk group was 3.1% for persons ≥65 years, 10.4% for persons with chronic diseases, 0.1% for HCWs, and 11.8% for all risk groups combined.
Table 1.
Total and SARS-CoV-2 vaccine target group populations by age group
| Age group | Total population1 | ≥65 years | Chronic diseases | HCWs | All risk groups combined | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % of total age group population | n | % of total age group population | n | % of total age group population | n | % of total age group population | ||
| Under 5 | 3,139,586 | 0 | 0.0% | 50,940 | 1.6% | 0 | 0.0% | 50,940 | 1.6% |
| 5 to 9 | 2,828,076 | 0 | 0.0% | 45,886 | 1.6% | 0 | 0.0% | 45,886 | 1.6% |
| 10 to 14 | 2,500,943 | 0 | 0.0% | 40,578 | 1.6% | 0 | 0.0% | 40,578 | 1.6% |
| 15 to 19 | 2,128,524 | 0 | 0.0% | 240,909 | 11.3% | 0 | 0.0% | 240,909 | 11.3% |
| 20 to 24 | 1,817,105 | 0 | 0.0% | 205,662 | 11.3% | 2,842 | 0.2% | 208,183 | 11.5% |
| 25 to 29 | 1,559,398 | 0 | 0.0% | 176,495 | 11.3% | 2,842 | 0.2% | 179,015 | 11.5% |
| 30 to 34 | 1,331,654 | 0 | 0.0% | 150,718 | 11.3% | 2,842 | 0.2% | 153,239 | 11.5% |
| 35 to 39 | 1,109,669 | 0 | 0.0% | 125,594 | 11.3% | 2,842 | 0.3% | 128,114 | 11.5% |
| 40 to 44 | 898,313 | 0 | 0.0% | 101,672 | 11.3% | 2,842 | 0.3% | 104,193 | 11.6% |
| 45 to 49 | 717,631 | 0 | 0.0% | 81,222 | 11.3% | 2,842 | 0.4% | 83,743 | 11.7% |
| 50 to 54 | 571,040 | 0 | 0.0% | 174,724 | 30.6% | 2,842 | 0.5% | 176,697 | 30.9% |
| 55 to 59 | 448,210 | 0 | 0.0% | 169,635 | 37.8% | 2,842 | 0.6% | 171,402 | 38.2% |
| 60 to 64 | 338,046 | 0 | 0.0% | 156,064 | 46.2% | 2,842 | 0.8% | 157,595 | 46.6% |
| 65 to 69 | 238,867 | 238,867 | 100.0% | 134,012 | 56.1% | 0 | 0.0% | 238,867 | 100.0% |
| 70+ years | 372,940 | 372,940 | 100.0% | 225,615 | 60.5% | 0 | 0.0% | 372,940 | 100.0% |
| Total | 20,000,000 | 611,807 | 3.1% | 2,079,729 | 10.4% | 25,580 | 0.1% | 2,352,301 | 11.8% |
Notes:
Total population of simulated country with the age distribution of the African Region per 2017.10
From estimates of chronic diseases risk factors for severe SARS-CoV-2 illness for Africa.13
HCWs population used per capita estimates from the WHO African Region (12.79 per 10,000 population) multiplied by the simulated country population and distributed evenly from ages 20 to 64.14
Vaccine doses
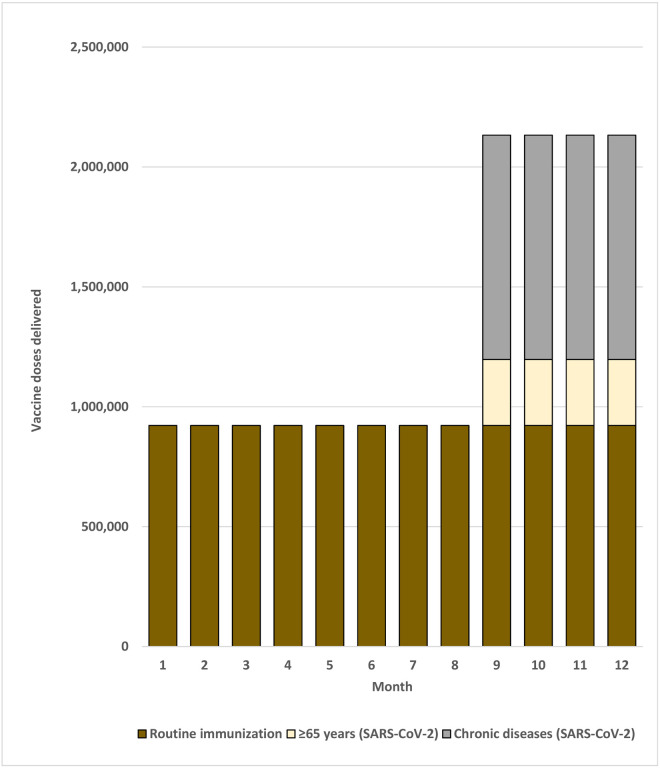
As in most developing countries, all routine vaccination services in the simulated country would be received by children aged <5 years and 9 through 14 years. Assuming systems would also be in place to provide immunization services to HCWs, established routine immunization platforms reached 31.0% of the national population. A total of 921,695 routine vaccine doses would be given each month. With a SARS-CoV-2 vaccination campaign 275,313 doses would be delivered targeting persons ≥65 years, 935,878 targeting persons with chronic diseases, 11,511 targeting HCWs, and 1,058,536 targeting all risk groups combined (Table 2 and Figure 2). Targeting SARS-CoV-2 vaccination of risk groups would therefore increase monthly doses administered over the routine immunization baseline by 29.9% for persons ≥65 years, 101.5% for persons with chronic diseases, 1.2% for HCWs, and 114.8% for all risk groups combined.
Table 2.
Monthly vaccine doses for routine immunization and SARS-CoV-2 mass vaccination campaigns by target groupa
| Age group | Routine immunizationb (doses) | ≥65 years (SARS-CoV-2 vaccine doses) | Chronic diseases (SARS-CoV-2 vaccine doses) | HCWs (SARS-CoV-2 vaccine doses) | All risk groups combined (SARS-CoV-2 vaccine doses) |
|---|---|---|---|---|---|
| Under 5 | 840,233 | 0 | 22,923 | 0 | 22,923 |
| 5 to 9 | 81,462 | 0 | 20,649 | 0 | 20,649 |
| 10 to 14 | 0 | 0 | 18,260 | 0 | 18,260 |
| 15 to 19 | 0 | 0 | 108,409 | 0 | 108,409 |
| 20 to 24 | 0 | 0 | 92,548 | 1,279 | 93,682 |
| 25 to 29 | 0 | 0 | 79,423 | 1,279 | 80,557 |
| 30 to 34 | 0 | 0 | 67,823 | 1,279 | 68,958 |
| 35 to 39 | 0 | 0 | 56,517 | 1,279 | 57,651 |
| 40 to 44 | 0 | 0 | 45,753 | 1,279 | 46,887 |
| 45 to 49 | 0 | 0 | 36,550 | 1,279 | 37,684 |
| 50 to 54 | 0 | 0 | 78,626 | 1,279 | 79,514 |
| 55 to 59 | 0 | 0 | 76,336 | 1,279 | 77,131 |
| 60 to 64 | 0 | 0 | 70,229 | 1,279 | 70,918 |
| 65 to 69 | 0 | 107,490 | 60,305 | 0 | 107,490 |
| 70+ years | 0 | 167,823 | 101,527 | 0 | 167,823 |
| Total | 921,695 | 275,313 | 935,878 | 11,511 | 1,058,536 |
| Immunization program workload | Routine immunization (monthly doses / vaccinatorc) | ≥65 years (monthly SARS-CoV-2 vaccine doses / vaccinatorc) | Chronic diseases (monthly SARS-CoV-2 vaccine doses / vaccinatorc) | HCWs (monthly SARS-CoV-2 vaccine doses / vaccinatorc) | All risk groups combined (monthly SARS-CoV-2 vaccine doses / vaccinatorc) |
| Routine immunization (prepandemic baselined) | 160.1 | -- | -- | -- | -- |
| Routine immunization (pandemicd) | 174.1 | 52.0 | 176.7 | 2.2 | 199.9 |
| % of routine immunization prepandemic baseline | 108.7% | 32.5% | 110.4% | 1.4% | 124.8% |
Notes:
Analysis assumes 90% coverage of target groups and a two-dose series for SARS-CoV-2 vaccines
We assumed that both HPV doses were delivered to girls at 9 years of age.
Vaccinators = nurse density per capita (6.9 per 10,000) × country population (20,000,000) × %nurses that provide immunization services (43%). Nurse data are from WHO Global Health Workforce Statistics.14 We used the median value from African Region countries at the most recent available date and divided by country population estimates to calculate per capita values.10
Figure 2. Monthly doses delivered for routine and SARS-CoV-2 risk group vaccination.
Notes:
a. Figure includes sufficient doses for 90% coverage of target groups.
b. Figure assumes constant routine immunization demand over the year and constant SARS-CoV-2 immunization demand over the four-month mass vaccination campaign.
c. For illustrative purposes only, the mass vaccination campaign is conducted during months 9 through 12.
d. HCWs target group removed because volume contribution was too small to depict in the figure.
Immunization workload
There were an estimated 13,800 nurses in the simulated country, of which an estimated 5,934 (43%) provide vaccination services. Accounting for baseline and pandemic absenteeism, one vaccinator would administer 160.1 routine doses per month at baseline and 174.1 routine doses per month during the pandemic (Table 2).
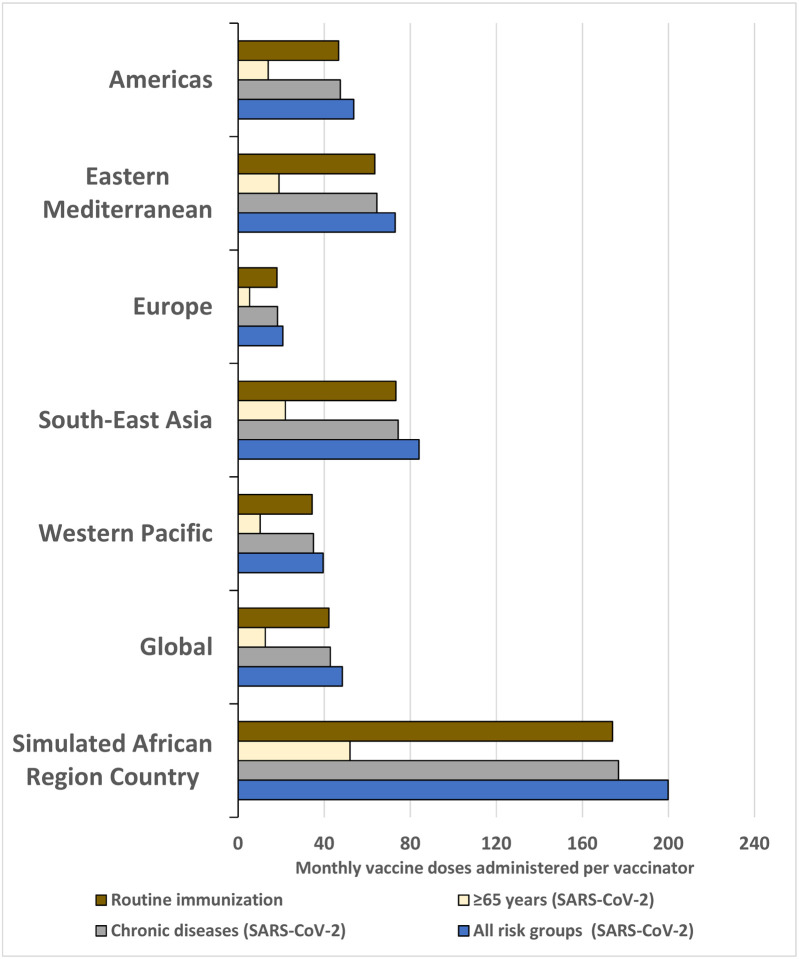
During the SARS-CoV-2 vaccination campaign, the number of persons vaccinated monthly per vaccinator would be 52.0 targeting persons ≥65 years, 176.7 targeting persons with chronic diseases, 2.2 targeting HCWs, and 199.9 targeting all risk groups combined. Compared to routine vaccines given at baseline, SARS-CoV-2 vaccination of risk groups would increase the immunization program workload for vaccinators by 32.5% for persons ≥65 years, 110.4% for persons with chronic diseases, 1.4% for HCWs, and 124.8% for all risk groups combined. Due to nursing personnel shortages in the African Region, the immunization program workload would be substantially lower in other WHO Regions. Repeating the analysis using nurse density estimates from other WHO Regions, the immunization program workload would be 26.8% using estimates from the Americas, 36.5% using estimates from the Eastern Mediterranean, 10.4% using estimates from Europe, 42.1% using estimates from South-East Asia, 19.8% using estimates from the Western Pacific, and 24.2% using global estimates (with the relative proportions being the same regardless of risk group) (Supplemental Table 4 and Figure 3).
Figure 3. Monthly routine and SARS-CoV-2 campaign vaccine doses per vaccinator, by WHO Region estimated nurse density.
Notes:
a. Data points represent the total monthly vaccines delivered divided by the total number of vaccinators in a country. Vaccinators = nurse density per capita × country population (20,000,000) × %nurses that provide immunization services (43%).
b. Nurse data are from WHO Global Health Workforce Statistics.14 We used the median value from countries at the most recent available date and divided by country population estimates10 to calculate per capita values and then categorized by WHO Region. Not all countries were represented in the WHO dataset.
c. Routine immunization programs account for 3% absenteeism (baseline). SARS-CoV-2 vaccination programs account for 3% absenteeism (baseline) and an additional 8% absenteeism (during pandemic).
d. HCWs target group removed because volume contribution was too small to depict in the figure.
Routine vaccine storage
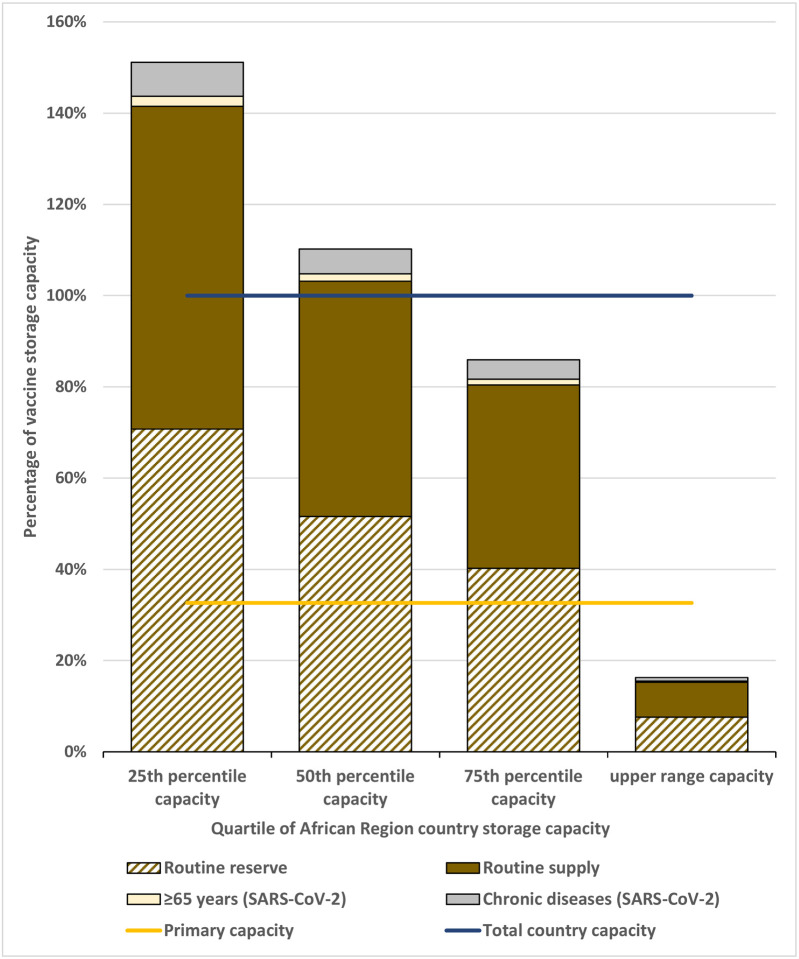
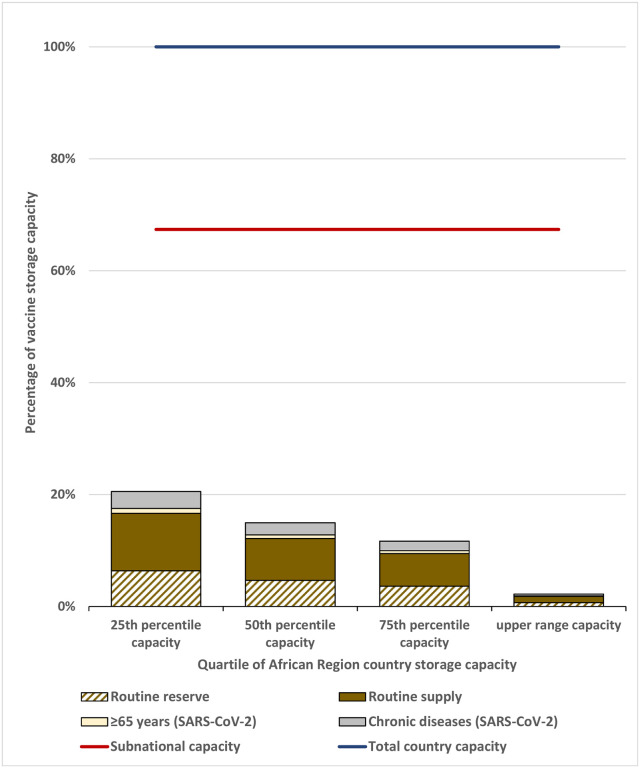
We applied standardized African Region vaccine storage capacity range and quartiles to the simulated country. The total vaccine storage capacity would range from 38,403 L to 1,605,826 L, and national level storage capacity would range from 12,534 L to 524,141 L (Table 3). We assessed the storage capacity during the month with the highest vaccine volumes. Using the vaccine flow-down schematic and adding the SARS-CoV-2 vaccination campaign during months 9 to 12, the maximum vaccine volumes were during month 10 for the national level and month 11 for the subnational levels (Supplemental Figures 1 and 2). We found that the maximum monthly routine vaccine volumes for the national level would be 244,963 L and for the aggregate subnational levels would be 28,793 L. At the national level, only the country with the highest value capacity has sufficient cold storage capacity to accommodate all routine vaccines according to our vaccine storage assumptions. Routine vaccine volumes exceeded that available at the national level for more than 75% of African Region country storage capacities (Figure 4). At subnational levels, substantial excess available space existed at the 25th percentile or higher of African Region country storage capacities, but not for the lower 25% (Figure 5).
Table 3.
Maximum monthly storage volume for routine and SARS-CoV-2 vaccines by quartile of African Region country storage capacity
| Lower range capacity | 25th percentile capacity | 50th percentile capacity | 75th percentile capacity | Upper range capacity | ||
|---|---|---|---|---|---|---|
| Country vaccine storage capacity | % of total country capacity | volume (L) | volume (L) | volume (L) | volume (L) | volume (L) |
| Total Country Capacity | 100.0% | 38,403 | 173,159 | 237,433 | 304,609 | 1,605,826 |
| National level | 32.6% | 12,535 | 56,519 | 77,498 | 99,424 | 524,142 |
| Subnational level | 67.4% | 25,868 | 116,640 | 159,935 | 205,185 | 1,081,685 |
| National level maximum monthly vaccine volumes | Vaccine volume (L) | % of national level capacity | % of national level capacity | % of national level capacity | % of national level capacity | % of national level capacity |
| Routine immunization | 244,963 | 1954.3% | 433.4% | 316.1% | 246.4% | 46.7% |
| ≥65 years (SARS-CoV-2) | 3,809 | 30.4% | 6.7% | 4.9% | 3.8% | 0.7% |
| Chronic diseases (SARS-CoV-2) | 12,948 | 103.3% | 22.9% | 16.7% | 13.0% | 2.5% |
| HCWs (SARS-CoV-2) | 159 | 1.3% | 0.3% | 0.2% | 0.2% | 0.0% |
| All risk groups combined (SARS-CoV-2) | 14,645 | 116.8% | 25.9% | 18.9% | 14.7% | 2.8% |
| Subnational level maximum monthly vaccine volumes | Vaccine volume (L) | % of subnational level capacity | % of subnational level capacity | % of subnational level capacity | % of subnational level capacity | % of subnational level capacity |
| Routine immunization | 28,794 | 111.3% | 24.7% | 18.0% | 14.0% | 2.7% |
| ≥65 years (SARS-CoV-2) | 1,533 | 5.9% | 1.3% | 1.0% | 0.7% | 0.1% |
| Chronic diseases (SARS-CoV-2) | 5,211 | 20.1% | 4.5% | 3.3% | 2.5% | 0.5% |
| HCWs (SARS-CoV-2) | 64 | 0.2% | 0.1% | 0.0% | 0.0% | 0.0% |
| All risk groups combined (SARS-CoV-2) | 5,894 | 22.8% | 5.1% | 3.7% | 2.9% | 0.5% |
Notes:
We developed a vaccine flow-down schematic (Figure 1) to depict the routine vaccine doses maintained at each immunization system level by month and used it to calculate the total monthly vaccine doses and volumes stored throughout the immunization system. This table uses the maximum monthly national level (month 10) and subnational level (month 11) vaccine storage volumes from the schematic.
The overall vaccine storage capacity for Gavi-eligible African Region countries was standardized by dividing by the <2 years country population in 2017. The range and quintiles of these values were calculated and then applied to the simulated African country. We used the median percentage of national level stores to total stores (32.6%) and health facility stores to total stores (34.9%) from the same data set for our analyses.
Vaccine coverage, reserve stock, resupply, and wastage assumptions are in Supplemental Table 2.
Figure 4. Maximum national level monthly routine and SARS-CoV-2 vaccine volumes as a proportion of total country capacity, by quartile of African Region country storage capacity.
Notes:
1. Based on the maximum monthly national level vaccine storage volume (month 10) of the vaccine flow-down schematic (Figure 1).
2. HCWs target group removed because volume contribution was too small to depict in the figure.
3. Lower range capacity category excluded from figure
Figure 5. Maximum subnational level monthly routine and SARS-CoV-2 vaccine volumes as a proportion of total country capacity, by quartile of African Region country storage capacity.
Notes:
1. Based on the maximum monthly subnational vaccine storage volume (month 11) of the vaccine flow-down schematic (Figure 1).
2. HCWs target group removed because volume contribution was too small to depict in the figure.
3. Lower range capacity category excluded from figure
SARS-CoV-2 vaccine storage
We estimated the volume required to store SARS-CoV-2 vaccines in tertiary packaging at the national level and in secondary packaging at subnational levels (Supplemental Figures 1 and 2). At the national level, monthly SARS-CoV-2 vaccines would occupy 3,809 L for persons ≥65 years, 12,948 L for persons with chronic diseases, 159 L for HCWs, and 14,645 L for all risk groups combined (Table 3). Excluding the lowest range value for country capacity, the percentage of total national level stores displaced by these vaccines by quartile of African Region country capacities ranged from 0.7%−6.7% for persons ≥65 years, 2.5% to 22.9% for persons with chronic diseases, <0.01% to 0.3% for HCWs, and 2.8% to 25.9% for all risk groups combined (Table 3 and Figure 4). At the subnational levels, monthly SARS-CoV-2 vaccines targeting risk groups would occupy 1,533 L for persons ≥65 years, 5,211 L for persons with chronic diseases, 64 L for HCWs, and 5,894 L for all risk groups combined. The percentage of subnational level stores displaced by these vaccines by quartile of African Region country storage capacity ranged from 0.1% to 5.9% for persons ≥65 years, 0.5% to 20.1% for persons with chronic diseases, <0.01% to 0.2% for HCWs, and 0.5% to 22.8% for all risk groups combined (Table 3 and Figure 5).
DISCUSSION
We used WHO tools and guidelines to estimate the operational impact of a SARS-CoV-2 vaccination campaign in the WHO African Region.15,20 While we simulated a country of 20 million population for this analysis, we used actual immunization, population, healthcare worker density, and cold storage capacity data available for the region. As no SARS-CoV-2 vaccines are currently licensed,1 we assumed a two dose vaccine series, multidose vials, and vaccine storage and volume characteristics similar to influenza vaccines.
Our analysis revealed that the national level storage capacity would be insufficient to accommodate additional SARS-CoV-2 vaccines for a vaccination campaign targeting risk groups as large as persons ≥65 years (3.1% of the population) in at least 75% of African Region countries. However, all African Region countries likely have sufficient subnational levels storage capacity to accommodate SARS-CoV-2 vaccines for mass vaccination campaigns. This means that there is insufficient excess cold storage capacity at the national level, whereas once vaccines are distributed to subnational levels in the health system there should be adequate storage capacity. This bottleneck in the vaccine cold chain at the national level can be addressed in advance by decreasing reserve stocks, shortening supply intervals, removing products from tertiary packaging earlier in the chain, distributing vaccines to the subnational levels, and/or installing more refrigeration capacity. However, implementation of SARS-CoV-2 vaccination campaigns will also require increases in accompanying dry goods, such as syringes, safety boxes, cotton, alcohol, and personal protective equipment, necessitating additional planning and budget for operations and waste management. More in-country vaccine shipments will be required to distribute routine and SARS-CoV-2 vaccines if transportation capacities are not increased, adding costs and logistical challenges. Care should be taken not to disrupt routine vaccine supply and distribution, as stockouts of routine vaccines will exacerbate national immunization programs already impacted by the pandemic.
While we found that the aggregate subnational level storage capacities are adequate for SARS-CoV-2 vaccines, with very large margins expected for a majority of countries, it should be noted that it is not possible nor practical to fill all available subnational level storage capacity. For example, at the health facility level, standard vaccine refrigerators may have multiple times the capacity needed for vaccines used at that facility, but that excess capacity cannot be easily used to store vaccines for other facilities. The logistics of maximizing available storage capacity at the lower levels of the cold chain makes it impractical. Nevertheless, our findings show that there is ample vaccine storage capacity available at subnational levels, and creative management of both routine and campaign vaccines could leverage some of that excess capacity during the SARS-CoV-2 vaccination campaign period.
Another major obstacle for SARS-CoV-2 vaccine delivery in the African Region will be the availability of qualified vaccinators. The African Region has the smallest health workforce of any WHO Region,14 and the workload required to vaccinate risk groups would increase by 32.5% for persons ≥65 years and 110.4% for persons with chronic diseases, compared to routine immunization baselines. SARS-CoV-2 vaccination activities targeting HCWs will require less additional workload given their small population size and ease of access to vaccination services. Our analysis highlights the need for significant planning, and investment in equipment, training, and logistics for SARS-CoV-2 vaccine deployment.
There is reason for optimism that the African Region SARS-CoV-2 vaccination response will be much improved from the 2009 H1N1 pandemic experience. Over the last ten years, a concerted global effort has greatly improved cold chain infrastructures and increased storage capacity.7,8 Furthermore, countries in the African Region have successfully implemented mass vaccination campaigns with meningococcal type A conjugate vaccine. From 2010–2017, the MenAfriVac introduction strategy targeted all persons aged one through 29 years in 23 Meningitis Belt countries.27 From 2010–2011, six West African countries implemented mass vaccination campaigns achieving 98% coverage in the target population.27 Over a tenday period in Burkina Faso, a team of 5,328 vaccinators and as many volunteers vaccinated 11,425,391 persons (73% of the country population).27 The lyophilized vaccine was supplied in 10-dose vials, requiring reconstitution.15 Each vaccinator vaccinated an average of 214 persons daily. With sufficient planning and resources, similar success could be achieved for SARS-CoV-2 vaccination programs.
A SARS-CoV-2 vaccination campaign would be greatly facilitated if vaccine delivery were simplified.19 While a one dose vaccine would be ideal, initial Phase 1 data indicate that two doses will likely be needed.2 Nasal spray or transdermal patch vaccines that could be administered by trained lay persons would free skilled health workers to provide other essential services, but no such vaccines are currently in human trials.1 While single dose vial vaccine presentations limit vaccine wastage,4,18 and prefilled syringe presentations limit wastage and greatly simplify administration,18 their cold storage volumes per dose make them highly problematic for use in mass vaccination campaigns in the African Region. For influenza vaccines (our proxy for SARS-CoV-2 vaccines in this analysis), secondary and tertiary packaging volumes per dose for multidose vials (5.2 mL and 12.9 mL)15 are much lower than for single dose vials (median of WHO prequalified products: 18.4 mL and 87.3 mL)15 and prefilled syringes (Flublok® Quadrivalent: 86.5 mL and 111.8 mL) (personal communication Dr. Ferdaus Hassan, Sanofi Pasteur).
WHO has advised that certain products would be challenging to include in national immunization schedules if they do not meet specific Programmatic Suitability Criteria.28 Vaccine products must meet these mandatory criteria to achieve WHO prequalification: include an anti-microbial preservative (for injectable liquid vaccines in multi-dose containers), be relatively thermostable (not requiring storage at less than −20°C), have a dose volume ≤1 ml (for injectable vaccines), and not require intravenous administration.28 Exceptions to the programmatic suitability criteria are made for the prequalification of certain emergency-use vaccines, such as for the prevention of Ebola Virus Disease, which are stored at −80°C to −60°C.27 The first SARS-CoV-2 vaccine candidates to enter human trials in the United States used a mRNA platform.1,2 Most mRNA vaccines for early phase studies are frozen at −70°C,29 although more stable product are anticipated to be used for the later phase trials. The final storage temperature for any future licensed mRNA vaccines is unknown. DNA vaccine candidates are more thermostable, but would likely require administration via electroporation devices. Any licensed products requiring freezing for storage or nonstandard devices for vaccine administration would be prohibitive to use at scale in developing countries.
Our study should be interpreted in light of its strengths and limitations. Our use of real-world data inputs and WHO tools and guidance strengthen the generalizability of the results and comparability to other cold chain capacity assessments. Since there is no currently licensed SARS-CoV-2 vaccine, we used the characteristics of influenza vaccines as proxies. If a SARS-CoV-2 vaccine requiring only one dose for protection is eventually licensed, the estimated doses and storage volumes required could substantially decrease. Conversely, if only products requiring ultra-cold chain or extra effort and training to administer are licensed, the operational feasibility of mass vaccination campaigns for developing countries would be very limited. We applied WHO recommended routine vaccination schedules and product characteristics,15,30 however, as of 2017, some of the routine vaccines we assumed for the simulated country had limited adoption in African Region countries (Supplemental Table 3). If we overestimated routine vaccine volumes, then there would be even more available capacity for SARS-CoV-2 vaccines.
The development of candidate SARS-CoV-2 vaccines must take operational realities and suitability in developing countries into account. While we believe that African Region countries currently have sufficient overall cold chain capacity to accommodate SARS-CoV-2 mass vaccination campaigns, our study highlights the limitations in cold storage capacity at national levels and in workforce availability to administer these vaccines. Vaccination of risk groups with SARS-CoV-2 vaccines is possible with sufficient planning and infrastructure strengthening, but we anticipate risks to routine immunization and significant logistical challenges. Further, the development of products that are not programmatically suitable for use in developing country contexts will result in massive inequities, and concerted global efforts are urgently required to ensure that preventive interventions are made available to all who need them globally. We believe that resources must be mobilized urgently to ensure that infrastructures and training are in place to maximize the impact of future SARS-CoV-2 vaccines in the African Region and other developing country settings.
Supplementary Material
ACKNOWLEDGMENTS:
The work of two authors (JR and JSH) was supported by the Bill & Melinda Gates Foundation (OPP1177124). The views expressed herein are solely those of the authors and do not necessarily reflect the views of the Foundation. The work of one author (AJD) was supported by National Institute of Allergy and Infectious Diseases at National Institutes of Health (T32AI007524).
Contributor Information
Justin R. Ortiz, Center for Vaccine Development and Global Health, 685 W. Baltimore St., University of Maryland School of Medicine, Baltimore, Maryland, USA..
Sarah R. Williams, Division of Pulmonary and Critical Care Medicine, 110 S. Paca St, University of Maryland School of Medicine, Baltimore, Maryland, USA..
Samba Sow, Centre pour le Développement des Vaccins, Ministère de la Santé, BP251Bamako, Mali..
Robin J. Biellik, Independent Consultant, Tranchepied 10, 1278 La Rippe, Switzerland..
Jean-Marie Okwo-Bele, Independent Consultant, Chemin de la Poste 6, 1295 Founex, Switzerland..
Kathleen M. Neuzil, Center for Vaccine Development and Global Health, 685 W. Baltimore St., University of Maryland School of Medicine, Baltimore, Maryland, USA..
REFERENCES
- 1.World Health Organization. Draft landscape of COVID-19 candidate vaccines. 2020. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed June 27, 2020).
- 2.O’Callaghan KP, Blatz AM, Offit PA. Developing a SARS-CoV-2 Vaccine at Warp Speed. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Report of the WHO Pandemic Influenza A(H1N1) Vaccine Deployment Initiative 2012. https://apps.who.int/iris/bitstream/handle/10665/44795/9789241564427_eng.pdf (accessed May 1, 2020).
- 4.World Health Organization. Global Survey on National Vaccine Deployment and Vaccination Plans for pandemic A(H1N1) 2009 vaccine – 2010 Report of Findings. 2013. https://www.who.int/influenza_vaccines_plan/resources/2010_H1N1_NVDP_WHO_Survey.pdf (accessed May 1, 2020).
- 5.Dawood FS, Iuliano AD, Reed C, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. The Lancet Infectious diseases 2012; 12(9): 687–95. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization; Main operational lessons learnt from the WHO Pandemic Influenza A(H1N1) Vaccine Deployment Initiative: Report of a WHO Meeting held in Geneva, Switzerland, 13–15 December 2010. 2011. https://apps.who.int/iris/bitstream/handle/10665/44711/9789241564342_eng.pdf (accessed May 1, 2020). [Google Scholar]
- 7.Azimi T, Franzel L, Probst N. Seizing market shaping opportunities for vaccine cold chain equipment. Vaccine 2017; 35(17): 2260–4. [DOI] [PubMed] [Google Scholar]
- 8.Gavi the Vaccine Alliance. 2016–2020 Strategy: Progress, Challenges and Risks. 2019. https://www.gavi.org/sites/default/files/board/minutes/2019/2019-Mtg-1_03%20-%202016-2020%20Strategy_Progress%20challenges%20and%20risks.pdf (accessed 2020_07_03).
- 9.World Health Organization. Principles and considerations for adding a vaccine to a national immunization programme: from decision to implementation and monitoring. 2014. https://apps.who.int/iris/handle/10665/111548 (accessed June 29, 2020).
- 10.Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2017 (GBD 2017) Population Estimates 1950–2017. 2019. http://ghdx.healthdata.org/record/ihme-data/gbd-2017-population-estimates-1950-2017 (accessed December 20, 2019).
- 11.World Health Organization. Summary of WHO Position Papers - Recommendations for Routine Immunization. 2019. https://www.who.int/immunization/policy/Immunization_routine_table1.pdf (accessed December 20, 2019).
- 12.World Health Organization. A global framework to ensure equitable and fair allocation of COVID-19 products. 2020. https://apps.who.int/gb/COVID-19/pdf_files/18_06/Global%20Allocation%20Framework.pdf (accessed June 26, 2020).
- 13.Clark A, Jit M, Warren-Gash C, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. The Lancet Global Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. WHO Global Health Workforce Statistics: December 2018 update. 2018. https://www.who.int/hrh/statistics/hwfstats/en/ (accessed January 22, 2020).
- 15.World Health Organization. WHO Prequalified Vaccines. 2019. https://extranet.who.int/gavi/PQ_Web/ (accessed March 22, 2019).
- 16.World Health Organization. Generic Preferred Product Profile for Vaccines. 2015. https://www.who.int/immunization/policy/committees/VPPAG_Generic_PPP_and_Workplan.pdf (accessed June 29, 2020).
- 17.World Health Organization. How to calculate vaccine volumes and cold chain capacity requirements. 2017. https://apps.who.int/iris/bitstream/handle/10665/255749/WHO-IVB-17.06-eng.pdf (accessed June 27, 2020).
- 18.World Health Organization. Training for mid-level managers (MLM) module 1: cold chain, vaccines and safe-injection equipment management. 2008. http://apps.who.int/iris/bitstream/10665/70184/1/WHO_IVB_08.01_eng.pdf (accessed January 4, 2020).
- 19.Kartoglu UH, Moore KL, Lloyd JS. Logistical challenges for potential SARS-CoV-2 vaccine and a call to research institutions, developers and manufacturers. Vaccine 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Guideline for establishing or improving primary and intermediate vaccine stores. 2002. https://apps.who.int/iris/bitstream/handle/10665/67807/WHO_V-B_02.34_eng.pdf).
- 21.World Health Organization. WHO Vaccine Wastage Rates Calculator. 2020. https://www.who.int/immunization/programmes_systems/supply_chain/resources/WHO_Vaccine_Wastage_Rates_Calculator_Tool.xlsx (accessed 25 April 2020).
- 22.World Health Organization. Vaccine Introduction Guidelines. 2005. https://www.who.int/immunization/hpv/plan/vaccine_introduction_guidelines_who_2005.pdf (accessed 02 March 2020).
- 23.International Council of Nurses. The Role of Nurses in Immunisation: a Snapshot from OECD Countries. 2018. https://www.icn.ch/sites/default/files/inline-files/IMMUNISATION_Report%20%28002%29.pdf (accessed June 3, 2020).
- 24.Ticharwa M, Cope V, Murray M. Nurse absenteeism: An analysis of trends and perceptions of nurse unit managers. J Nurs Manag 2019; 27(1): 109–16. [DOI] [PubMed] [Google Scholar]
- 25.Chin ET, Huynh BQ, Lo NC, Hastie T, Basu S. Healthcare worker absenteeism, child care costs, and COVID-19 school closures: a simulation analysis. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Vaccine Management and Logistics Support. 2020. https://www.who.int/immunization/programmes_systems/supply_chain/resources/tools/en/index5.html (accessed June 29, 2020).
- 27.Djingarey MH, Barry R, Bonkoungou M, et al. Effectively introducing a new meningococcal A conjugate vaccine in Africa: the Burkina Faso experience. Vaccine 2012; 30 Suppl 2: B40–5. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Assessing the Programmatic Suitability of Vaccine Candidates for WHO Prequalification (Revision 2014). 2014. https://apps.who.int/iris/bitstream/handle/10665/148168/WHO_IVB_14.10_eng.pdf (accessed March 2, 2020).
- 29.Pardi N, Hogan MJ, Porter FW, Weissman D. mRNA vaccines - a new era in vaccinology. Nat Rev Drug Discov 2018; 17(4): 261–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. Table 1: Summary of WHO Position Papers - Recommendations for Routine Immunization. 2019. https://www.who.int/immunization/policy/Immunization_routine_table1.pdf (accessed December 17, 2019).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.