Abstract
Importance: Head-mounted displays for virtual reality (HMD–VR) may be used as a therapeutic medium in physical rehabilitation because of their ability to immerse patients in safe, controlled, and engaging virtual worlds.
Objective: To explore how HMD–VR has been used in adult physical rehabilitation.
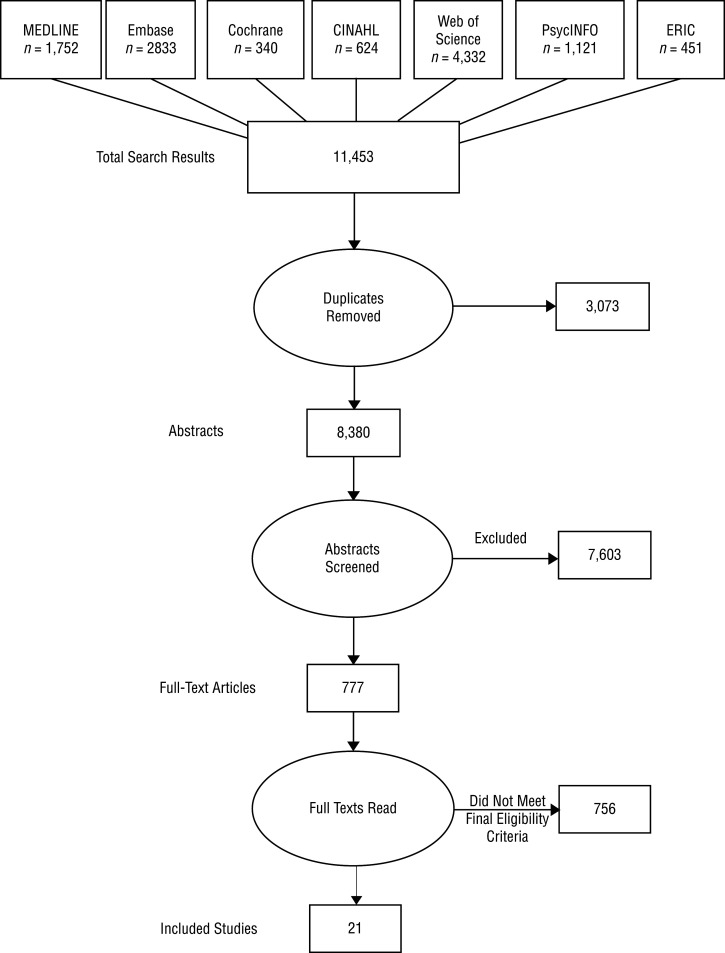
Data Sources: A systematic search of MEDLINE, Embase, Cochrane Library, CINAHL, Web of Science, PsycINFO, and ERIC produced 11,453 abstracts, of which 777 underwent full-text review.
Study Selection and Data Collection: This scoping review includes 21 experimental studies that reported an assessment or intervention using HMD–VR in a physical rehabilitation context and within the scope of occupational therapy practice.
Findings: HMD–VR was used for assessment and intervention for patients with a range of disorders, including stroke, multiple sclerosis, spinal cord injury, and Parkinson’s disease.
Conclusions and Relevance: HMD–VR is an emerging technology with many uses in adult physical rehabilitation. Higher quality clinical implementation studies are needed to examine effects on patient outcomes.
What This Article Adds: We review existing research on how immersive virtual reality (e.g., using head-mounted displays) has been used for different clinical populations in adult physical rehabilitation and highlight emerging opportunities in this field for occupational therapists.
Virtual reality (VR) refers to “a range of computing technologies that present artificially generated sensory information in a form that people perceive as similar to real-world objects or events” (Wilson et al., 1997, p. 219). Whereas primitive VR appeared in the late 1800s as stereoscopic photo viewers that added depth to two-dimensional images, the first fully immersive head-mounted display for virtual reality (HMD–VR) was developed by computer scientist Ivan Sutherland in 1968 (Sherman & Craig, 2002). Sutherland’s initial technology was complex, costly, and so physically massive that it had to be suspended from the ceiling (Sherman & Craig, 2002). Since then, HMD–VR has advanced such that, starting with the release of the Oculus Rift (Oculus VR, Menlo Park, CA) in 2015, the devices are lightweight, portable, and affordable, providing opportunities in a variety of realms, including medicine and rehabilitation (Rizzo et al., 1997).
HMD–VR is an ideal medium for assessment and intervention in physical rehabilitation because it can be tailored to the needs of the patient, can provide personalized feedback on performance, and can allow intervention to take place in a safe and nonthreatening yet realistic environment (Henderson et al., 2007). In general, VR, whether on a screen or via HMD–VR, can enable simulated practice of functional tasks at higher dosages than in traditional therapies (Laver et al., 2017). Moreover, because users consider the virtual tasks more interesting and enjoyable, the use of VR encourages greater participation and higher levels of engagement in therapy (Laver et al., 2017). Compared with VR on a traditional computer screen or tablet, HMD–VR provides an enhanced sense of immersion in the virtual world (Juliano et al., 2020). Such immersion can result in increased embodiment, which has been shown to improve motor-related processes (Juliano et al., 2020), making HMD–VR especially applicable in the realm of physical rehabilitation.
Although HMD–VR emerged only recently, research on its use in rehabilitation is growing rapidly. It is therefore crucial to identify appropriate clinical uses and ensure that adequate evidence exists to support clinical applications of HMD–VR for physical rehabilitation. We conducted a scoping review to identify current applications of HMD–VR in adult physical rehabilitation, describe uses that fit within the occupational therapy practice domain, and identify gaps and potential directions to guide future research.
Method
Scoping reviews are a methodical form of literature review used to describe the landscape of available evidence, identify gaps in existing literature, and illuminate areas for further research (Arksey & O’Malley, 2005, p. 21; Tricco et al., 2018). A scoping review differs from a systematic review in that it is designed not to evaluate the quality of the evidence but to describe the extent, range, and nature of research activity in a given area (Levac et al., 2010). Although the purposes of scoping and systematic reviews differ, they both use a systematic process to safeguard against bias, maximize rigor, and ensure replicability of results (Arksey & O’Malley, 2005). The objective of this scoping review was to describe how HMD–VR is being used in the assessment and rehabilitation of adults with physical disabilities, with a focus on uses relevant to occupational therapy. A scoping review methodology was selected because of the relatively young nature of the field, given that HMD–VR became commercially available in 2015. No protocol version of this scoping review exists.
A research librarian (Lynn Kysh) collaborated with the authors to create and document comprehensive literature searches in MEDLINE, Embase, Cochrane Library, CINAHL, Web of Science, PsycINFO, and ERIC for articles published between 2008 and 2018 using search terms focused on HMD–VR; the searches were conducted on July 25, 2018. A combination of subject headings (when available) and key words was used for the concepts of VR and head-mounted devices, including specific technology brands. Appendix A provides database details and full search strategies. No additional efforts were made to search the gray literature. The librarian compiled search results into an EndNote library using EndNote X8 (Clarivate Analytics, Philadelphia, PA). Duplicates were identified and deleted in the EndNote software using methods described by Bramer and colleagues (2016). The remaining abstracts were imported into Covidence (Melbourne, Victoria, Australia) and independently screened by at least two of the three reviewers (David Saldana, Meghan Neureither, Esther Jahng). The full text of each article that passed the abstract screening was then independently reviewed by at least two of those three reviewers. Another reviewer (Sook-Lei Liew) settled all disagreements regarding inclusion at both the abstract screening and full-text article review phases.
To be included, articles had to report on the use of HMD–VR in an experimental study with human participants in a rehabilitation context relevant to the scope of occupational therapy practice. Occupational therapy supports health and participation through active engagement in occupations supported by evaluation and intervention in its practice domain, which includes occupations (e.g., activities of daily living, work, play, leisure), client factors (e.g., body function, body structures, values), performance skills (e.g., motor skills, social interaction skills), performance patterns (e.g., habits, routines), and context and environment (American Occupational Therapy Association [AOTA], 2014). For the purposes of this review, we focused on articles describing occupational therapy–relevant assessments and interventions in adult physical rehabilitation contexts. Articles were excluded if the study used a non-head-mounted VR display (e.g., computer screen, augmented reality, cave automatic virtual environment), the study was conducted in a setting not relevant to occupational therapy, or the article was not available in English. Gray literature (e.g., letters, commentaries, textbook chapters), technical or theoretical descriptions without assessment of human behavior, and abstracts or conference proceedings of four pages or less were not included.
We assigned level of evidence and rigor designations to each article as follows: Level I, systematic review or meta-analysis of randomized controlled trials (RCTs); Level II, RCT; Level III, controlled trial without randomization; Level IV, case-control or cohort study; Level V, case study or systematic review of descriptive and qualitative studies (Melnyk & Fineout-Overholt, 2011). Descriptive data were extracted for each study, including patient population, provider type, type of HMD–VR, and focus of assessment or intervention. To more easily identify clinical and research opportunities for the use of HMD–VR in occupational therapy, we grouped and qualitatively summarized the included studies by patient population.
Results
Results at each stage of the systematic search and scoping review process are shown in Figure 1. The searches produced a total of 11,453 abstracts from the seven databases. After 3,073 duplicates were removed, we screened 8,380 abstracts and excluded 7,603. Of the 777 full-text articles retrieved for further evaluation, 21 met the inclusion criteria for this scoping review and are summarized in Table 1 (placed at the end of this article, after the reference list). Many of the excluded abstracts and articles either did not use HMD–VR or were beyond the scope of occupational therapy (e.g., technical development of HMD–VR, applications beyond physical rehabilitation such as pain management and education).
Figure 1.
Flow of search results through the scoping review process.
Table 1.
Articles Included in the Scoping Review on Head-Mounted Displays for Virtual Reality in Adult Physical Rehabilitation, by Population
| Author/Year | Level of Evidence/Study Design | Population | Participants | Provider Type | Type of HMD–VR | Focus of Assessment or Intervention |
|---|---|---|---|---|---|---|
| Stroke | ||||||
| Huang et al. (2018) |
|
Stroke | N = 8 | Physiotherapist | Oculus Rift DK2 (Oculus VR, Menlo Park, CA) with Amadeo 5 degrees of freedom robotic device; Tyromotion, Graz, Austria) | Fine motor exercises |
| Jannink et al. (2009) |
|
Stroke, visuospatial neglect | N = 18 (n = 6 healthy, n = 6 acute stroke, n = 6 chronic stroke) | Unspecified | HMD Proview XL (Kaiser Electronics, Cedar Rapids, IA) | Visual searching task for assessment of visual neglect |
| Kang et al. (2012) | Level II RCT | Stroke | N = 30 (n = 10 optic flow group, n = 10 healthy control group, n = 10 treadmill group) | Physical therapist | MSP-209 (Kowon Technology, Seoul, South Korea) | Gait and balance training |
| Lupu et al. (2018) |
|
Stroke | N = 7 | Unspecified | Oculus Rift (Oculus VR, Menlo Park, CA) with TRAVEE BCI–FES subsystem | Fine motor exercises |
| Peskine et al. (2011) |
|
Stroke, visuospatial neglect | N = 18 (n = 9 stroke patients, n = 9 healthy control) | Unspecified | Unspecified | Navigation of virtual town for assessment of visual neglect |
| Subramanian et al. (2007) |
|
Stroke | N = 32 stroke patients | Unspecified | Kaiser XL 50, resolution 1024 × 768, frequency 60 Hz (Mindflux, Roseville, New South Wales, Australia) with CAREN VR simulation system (CAREN, Amsterdam, the Netherlands) | Upper extremity training exercises and reaching task |
| Subramanian & Levin (2011) |
|
Stroke | N = 30 (n = 20 stroke, n = 10 healthy) | Unspecified | IREX Integrated Rehabilitation & Exercise System (GestureTek, Toronto, Ontario, Canada) | Repetitive task-based training and reaching task |
| Spinal Cord Injury | ||||||
| Carlozzi et al. (2013) |
|
SCI | N = 52 (n = 26 HMD, n = 26 screen display) | Unspecified | eMagin Z800 3D visor and hand controls for acceleration and deceleration (eMagin, Hopewell Junction, NY) with adaptive equipment for steering (e.g., spinner knob, tri-pin) | HMD–VR-based driving simulator |
| Nunnerley et al. (2017) |
|
SCI | N = 12 (n = 7 SCI, n = 5 clinicians) | Unspecified | Oculus Rift (Oculus VR, Menlo Park, CA) with Dynamic Controls wheelchair joystick (Dynamic Controls, Christchurch, New Zealand) | Feasibility of HMD–VR-based wheelchair training |
| Vestibular Impairment and Balance | ||||||
| Lubetzky et al. (2018) |
|
Healthy adults | N = 21 | Unspecified | Oculus Rift DK2 (Oculus VR, Menlo Park, CA) with Unity Version 5.2.1f (Unity Technologies, San Francisco, CA) | Assessment of balance and postural control |
| Micarelli et al. (2017) |
|
Unilateral vestibular hypofunction | N = 47 (n = 23 HMD–VR + conventional training, n = 24 conventional training only) | Unspecified | Revelation 3D headset (Chinavasion, Hong Kong) with Windows phone (Microsoft, Redmond, WA) | HMD–VR-based vestibular exercise program |
| Rausch et al. (2018) |
|
Healthy adults | N = 28 | Athletic trainer | Google Cardboard V2 (Google, Mountain View, CA) with smartphone | Assessment of postural control |
| Saldana et al. (2017) |
|
Older adults at risk for falls | N = 13 (n = 5 high fall risk, n = 8 low fall risk) | Unspecified | Oculus Rift DK2 (Oculus VR, Menlo Park, CA) with force plate | Assessment of balance |
| Tossavainen et al. (2001) |
|
Healthy adults | N = 3 | Unspecified | Virtual Research VR8 and head orientation tracker (Virtual Research Systems, Aptos, CA) | Assessment of balance |
| Viziano et al. (2018) |
|
Unilateral vestibular hypofunction | N = 47 (n = 23 HMD–VR + conventional training, n = 24 conventional training only) | Unspecified | Revelation 3D headset (Chinavasion, Hong Kong) with Windows phone (Microsoft, Redmond, WA) | HMD–VR-based vestibular exercise program |
| Zalewski-Zaragoza & Viirre (2003) |
|
Vertigo | N = 15 with vertigo | Medical doctor | Virtual IO HMD (Virtual IO Solutions, Alpharetta, GA) with Pentium-driven personal computer | Assessment of vertigo symptoms |
| Cervical Range of Motion | ||||||
| Sarig Bahat et al. (2015) |
|
Healthy adults | N = 46 | Unspecified | i-glasses HRV Pro (I-o Display Systems, Menlo Park, CA), Virtual Realities HMD (Virtual Realities, Wintersville, OH), and Fastrak electromagnetic tracking system (Polhemus, Colchester, VT) | Assessment of CROM |
| Sarig-Bahat et al. (2009) |
|
Healthy adults | N = 30 | Unspecified | i-glasses HRV Pro (I-o Display Systems, Menlo Park, CA), Virtual Realities HMD (Virtual Realities, Wintersville, OH), and Fastrak electromagnetic tracking system (Polhemus, Colchester, VT) | Assessment of CROM |
| Sarig-Bahat et al. (2010) |
|
Chronic neck pain | N = 67 (n = 25 symptomatic adults, n = 42 asymptomatic adults) | Unspecified | i-glasses HRV Pro (I-o Display Systems, Menlo Park, CA), Virtual Realities HMD (Virtual Realities, Wintersville, OH), and Fastrak electromagnetic tracking system (Polhemus, Colchester, VT) | Assessment of CROM |
| Parkinson’s Disease | ||||||
| Arias et al. (2012) |
|
PD | N = 36 (n = 12 PD, n = 12 healthy younger adults, 12 older adults) | Unspecified | Vuzix iWear VR920 glasses (Vuzix, Rochester, NY) | Assessment of fine motor movements |
| Congenital Limb Deficiency | ||||||
| Kurzynski et al. (2017) |
|
Congenital limb difference | N = 2 (n = 1 congenital limb difference, n = 1 healthy control) | Unspecified; experienced instructor in a lab | Visual Studio development environment and XNA framework (Microsoft, Redmond, WA) with Sony HMZ-T1 headset (Sony, Tokyo, Japan) | HMD–VR-based motor imagery training |
Note. BCI = brain–computer interface; CROM = cervical range of motion; FES = functional electrical stimulation; HMD = head-mounted display; PD = Parkinson’s disease; RCT = randomized controlled trial; SCI = spinal cord injury; VR = virtual reality.
The included studies used both experimental and nonexperimental designs. The majority (n = 17) did not specify the profession of the provider who carried out the intervention; the intervention in 2 studies was carried out by physical therapists, in 1 study by a medical doctor, and in 1 study by an athletic trainer. Clinical populations targeted in these studies included stroke (n = 7), spinal cord injury (SCI; n = 2), disorders of the vestibular system (n = 3), impaired balance (n = 1), cervical range of motion (ROM) impairments (n = 3), Parkinson’s disease (n = 1), and congenital limb deficiency (n = 1); some balance studies examined healthy adults (n = 3). The most common uses of HMD–VR were for upper extremity rehabilitation (n = 4), vestibular training (n = 4), and gait and balance rehabilitation (n = 5). The assessment and intervention uses of HMD–VR are summarized for each clinical population in the sections that follow.
Assessment and Intervention for Stroke
Seven studies examined the use of HMD–VR in stroke rehabilitation. Four studies addressed upper extremity rehabilitation using HMD–VR-based immersive game training. In a Level III quasi-experimental study, Huang and colleagues (2018) found that HMD–VR games such as flying a spaceship and cooking in a virtual kitchen increased upper extremity strength and ROM in subacute stroke survivors. Similarly, in a Level II prospective RCT, participants with stroke receiving virtual upper extremity training exercises demonstrated increased ROM and less compensatory trunk movement in a reaching task than those who received training in a traditional physical environment (Subramanian et al., 2007).
A Level III nonrandomized trial examined precision of movement, endpoint movement velocity, and endpoint trajectory during a reaching task of participants with stroke who received repetitive task-based training using HMD–VR compared with a two-dimensional screen projection system (Subramanian & Levin, 2011). Participants’ movements were slower and less precise in the HMD–VR condition than in the screen condition; however, participants with moderate to severe hemiparesis moved their arm more quickly in the HMD–VR condition, suggesting the possible utility of this tool for this specific patient population (Subramanian & Levin, 2011). The final upper extremity study examined HMD–VR in conjunction with a combined brain–computer interface (BCI) and functional electrical stimulation (FES) system to focus on repeated flexion and extension of the hand and fingers (Lupu et al., 2018). In this Level III quasi-experimental study, the BCI–FES system effectively allowed participants to receive real-time feedback on performance and corrections to the exercise program from a virtual therapist (Lupu et al., 2018).
One study explored the use of HMD–VR for poststroke gait rehabilitation. This Level II pretest–posttest RCT study evaluated the effect of optic flow modulation in HMD–VR on functional recovery of gait and balance with 30 participants (Kang et al., 2012). To circumvent participants’ challenges with poor proprioceptive feedback after stroke, the researchers used HMD–VR to provide participants with optic flow information about the direction and speed of their gait and thus improve their ability to maintain postural stability, gait, and balance. Participants in the optic flow group who wore the HMD–VR during treadmill walking demonstrated the greatest improvement in Timed Up and Go tests and the greatest increase in gait velocity (Kang et al., 2012). Both Lupu et al. (2018) and Kang et al. (2012) found that the use of HMD–VR resulted in improved participant motivation and increased concentration during the rehabilitation process; motivation and concentration are often limited given the challenging and repetitive nature of rehabilitation tasks.
Finally, 2 small-sample Level III studies examined the use of VR to assess visuospatial neglect, traditionally assessed through a brief, cursory bedside examination or standardized pencil-and-paper test, such as the cancellation test (Gauthier et al., 1989) or the line bisection task (Schenkenberg et al., 1980). In 1 study, participants with stroke demonstrated a more inefficient, trial-and-error search pattern to locate a visual stimulus in the virtual environment compared with healthy control participants (Jannink et al., 2009). Detecting aberrations in typical search patterns provides a means for measuring unilateral neglect that may be more sensitive than standard pencil-and-paper methods (Jannink et al., 2009). In the second trial, an HMD–VR system was used to assess visuospatial neglect through various visual search tasks in a virtual town, including locating a swing set in the town center and locating and counting 13 bus stops on both the left and right sides along a walking path (Peskine et al., 2011). The use of HMD–VR in this study isolated the visual system, allowing for the testing of neglect deficits in a controlled yet realistic manner without challenging participants’ motor impairments or causing physical fatigue (Peskine et al., 2011).
Intervention for Spinal Cord Injury
Two studies investigated the use of HMD–VR in interventions for people with SCI. In a Level VI qualitative study, participants with SCI and clinicians trialed the use of VR for power wheelchair training, and the results suggested that, for people with a recent SCI, an HMD–VR program could be especially helpful in reducing anxiety before trying a new wheelchair (Nunnerley et al., 2017). Participants also noted the capacity of the HMD–VR to transport the user outside the “rehabilitation bubble,” providing experience in a realistic environment to better prepare them for transition to the community (Nunnerley et al., 2017, p. 419).
A Level II randomized comparative trial compared HMD–VR to a traditional three-screen display for using a driving simulator (Carlozzi et al., 2013). Although no significant differences were found, participants using HMD–VR had a greater number of off-road collisions and longer stopping latencies indicative of more hesitancy or increased head movements (Carlozzi et al., 2013). These 2 studies, although limited, provide an impetus for continued examination of HMD–VR use for people with SCI, but appropriate applications and assessment or intervention protocols require substantially more exploration.
Assessment and Intervention for Vestibular Impairment and Balance
Three studies explored the use of HMD–VR for the assessment and treatment of vestibular impairment, traditionally assessed by caloric and rotational tests (Yardley et al., 1999). A Level IV pilot study matched vertigo symptoms to a specific frequency displayed in the HMD–VR for participants with chronic vertigo (Zalewski-Zaragoza & Viirre, 2003). The researchers concluded that HMD–VR can reasonably simulate vertigo and can be used in evaluation of people with low frequency vertigo (≤1.0 Hz). In a Level II RCT, Micarelli and colleagues (2017) explored using an HMD–VR-based game for people with unilateral vestibular hypofunction, a condition characterized by a reduction of at least 25% in responsivity of the peripheral vestibular system to bithermal air or caloric testing (Hall et al., 2016). Compared with control participants who received traditional vestibular rehabilitation, participants using home-based HMD–VR showed greater improvements in vestibulo–ocular reflex responsivity and balance (p < .001; Micarelli et al., 2017). At a 1-yr follow-up, improvements in these outcomes were maintained at a higher level by the HMD–VR group compared with the conventional rehabilitation group (p < .001; Viziano et al., 2018).
Four studies examined the use of HMD–VR to assess balance in older adults and healthy participants across various age ranges. In a Level III pilot study with older adults at risk for falls, the use of HMD–VR to track the influence of visual perturbations on balance was found to be a comparable alternative to a traditional assessment using a force plate, with the added benefit of portability making HMD–VR highly suitable for assessing balance in busy clinics or hospital rooms with limited space (Saldana et al., 2017). Two Level IV studies provided preliminary data to support HMD–VR as a clinical tool for assessing balance. The first study found HMD–VR to be a feasible and reliable means for measuring postural control (Lubetzky et al., 2018), and the second study concluded that a smartphone-based HMD–VR application produced a standardized assessment of postural stability in a clinical setting with concurrent validation with the Balance Error Scoring System and center-of-pressure measurements (Rausch et al., 2018). Finally, in a small-sample Level IV study, Tossavainen and colleagues (2001) provided visual perturbations using HMD–VR to create a loss of balance in participants to assess the impact of alcohol consumption on balance. Although the specific focus of this study on alcohol consumption may limit its clinical relevance to occupational therapy, it provides further validation for the use of HMD–VR to induce postural instability as a way of safely assessing balance across a variety of diagnostic conditions.
Assessment for Cervical Range of Motion
No gold standard exists for assessing cervical ROM. Sarig-Bahat and colleagues (2009, 2010, 2015) conducted 3 studies investigating the use of HMD–VR as an option for enhancing clinical assessment of cervical ROM and provided foundational support for the feasibility, reliability, and validity of this use of HMD–VR. One of their studies, a Level II nonrandomized comparative trial, demonstrated that HMD–VR was able to differentiate significantly reduced ROM in a chronic cervical pain group compared with a healthy control group (p < .05; Sarig-Bahat et al., 2010). In addition, results of the authors’ 2 Level III repeated-measures studies suggested that use of HMD–VR increased motivation and engagement, which may have positively affected both assessment and intervention for their participants with cervical pain and limited ROM (Sarig-Bahat et al., 2009, 2015).
Assessment for Parkinson’s Disease
HMD–VR was used in 1 Level III nonrandomized controlled trial to assess manual dexterity in people with Parkinson’s disease. The study compared performance on a finger-tapping test among healthy young adults, healthy older adults, and people with Parkinson’s disease and found that HMD–VR was able to detect slower, less rhythmic movements in the Parkinson’s group compared with the healthy control groups (Arias et al., 2012). Arias and colleagues (2012) suggested that HMD–VR could be a suitable and reliable tool for the evaluation of parkinsonian motor movements.
Intervention for Congenital Limb Deficiency
A Level IV single case–control study used HMD–VR in motor imagery training with both visual and sensory feedback to improve voluntary control over transplanted extremities for a participant with bilateral upper limb congenital transverse deficiency (Kurzynski et al., 2017). The computer-aided training system included a virtual hand that the user saw in an HMD–VR headset combined with haptic feedback on the user’s residual limb to stimulate the visual and sensory cortex as a means of improving motor function. Results showed that the motor imagery task in HMD–VR was related to improved motor planning for reaching and grasping (Kurzynski et al., 2017). Although preliminary, these results demonstrate the potential role of HMD–VR in rehabilitative interventions for people with congenital limb differences.
Discussion
In this scoping review, we sought to understand how HMD–VR has been used in physical rehabilitation contexts, identify implications for occupational therapy practice, and discern gaps in the current literature to guide future research. The studies identified in this review demonstrate initial support for HMD–VR as a tool for both assessment and intervention in adult physical rehabilitation for a variety of patient populations. On the whole, the authors of these studies reported success with use of VR in rehabilitation, noting added benefits of HMD–VR as a low-cost, portable tool that increases patient motivation and engagement in rehabilitative activities. However, the level of evidence of most studies was relatively weak, and larger studies with better control conditions are needed.
Overall, HMD–VR was used across a range of populations with a variety of needs commonly addressed by occupational therapists. A key benefit of HMD–VR was providing simulated environments for assessment or intervention that closely resembled real-world environments. However, unlike real-world environments, the simulated environments were safe and controlled, making it easier for patients to practice complex skills such as cooking, without the actual risks of cooking such as cuts or burns or dropping fragile items, and driving, without the actual risks of being on the road. In addition, assessments of balance and neglect using HMD–VR showed a quality comparable to that of standard assessments. In some assessments, such as for visual neglect and motor performance in patients with Parkinson’s disease, the HMD–VR measurements were more accurate than other measures and could detect more subtle impairments.
The findings of this scoping review suggest that HMD–VR can be a safe, portable means for assessment in a variety of settings. Thus, although most included studies were conducted in a laboratory environment with researcher supervision, the use of HMD–VR to provide complex assessment and training in a safe environment could be easily translated to clinic- and home-based therapies. Future studies could build on these studies by exploring the use of HMD–VR applications in clinical settings and home-based training and as a component of telerehabilitation. Notably, although many of the earlier studies used expensive HMD–VR devices that are no longer commercially available, some of the more recent studies used commercially available and low-cost devices, such as the Google Cardboard (Google, Mountain View, CA), which retails online for $15 (but requires a smartphone), or the Oculus Rift, which retails online for several hundred dollars, depending on the model and technical specifications. The accessibility of these devices should help make future studies using HMD–VR with larger populations more feasible.
A key component of the interventions identified by this scoping review was increased patient motivation and engagement in rehabilitation tasks using HMD–VR. Supporting patients’ motivation to participate actively in therapy can be especially useful when conventional interventions, such as repetitive task-based training, become boring. The included studies suggest that HMD–VR can improve on standard assessment and training by engaging patients in the immersive environment. In addition, these studies reported, little, if any, discomfort (e.g., as measured using the Simulator Sickness Questionnaire; Kennedy et al., 1993) with use of HMD–VR. In studies using HMD–VR for standing or balance tasks with the supervision of study personnel, no adverse events were noted (e.g., falls, overexertion). Thus, HMD–VR may enable some patients to experience greater enjoyment and motivation during therapy with few risks or side effects, suggesting that HMD–VR can be a low-risk, fun adjunct to therapy.
Although the literature indicates that VR is a feasible intervention for use in physical rehabilitation, none of the studies listed occupational therapy practitioners as the primary intervention provider. More recently published studies (i.e., after 2008–2018) using HMD–VR included occupational therapists, including studies on HMD–VR-based BCIs for stroke rehabilitation (e.g., Vourvopoulos et al., 2019). Occupational therapy practitioners are distinctly positioned to engage in future evaluation of HMD–VR uses because of their expertise in many of the areas reported in this review, including assessment of ROM, neglect, and fall risk and intervention to improve strength, balance, and motor control. Moreover, VR can enable occupational therapy practitioners to help patients safely engage in valued occupations that can facilitate changes in client factors such as body function, body structure, values, beliefs, and skills (AOTA, 2014). Proffitt and colleagues (2019) emphasized that occupational therapy practitioners have expertise in adapting technologies to the unique abilities of people with disabilities and thus are prime candidates to incorporate VR technology into therapy.
To further substantiate VR as a useful tool in rehabilitation, higher quality studies with larger sample sizes are needed. Most of the studies described in this review provide Level III evidence (i.e., from participants not randomized into groups), limiting the impact of the findings (Melnyk & Fineout-Overholt, 2011). The average sample size of included studies was 23.75 ± 17.60, and future research would benefit from larger samples. In addition, study protocols varied widely in terms of treatment dosage, length of treatment, and methods for incorporating HMD–VR. The development of manualized protocols for VR-based rehabilitation would strengthen these interventions and allow for study replication.
Implications for Occupational Therapy Practice
This scoping review offers the following implications for occupational therapy practice:
HMD–VR is a commercially available, relatively inexpensive tool that can be used in rehabilitation with adult patients across the lifespan.
HMD–VR can be used appropriately in assessment and intervention for patients with a variety of diagnoses.
Acknowledgments
David Saldana, Meghan Neureither, and Allie Schmiesing contributed equally to this article. This research was funded by the American Heart Association (16IRG26960017), the U.S. Army Research Office (W911NNF-14-D-0005), and the National Institutes of Health (K01HD091283). We thank Jennifer Dinalo for guidance and facilitation through this process and Ashley Hvidt for assistance.
Appendix A. Database Details and Search Strategies
Database Names: Ovid Medline® Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid Medline® Daily, Ovid Medline®
Database Vendor: Wolters Kluwer
Database Coverage: 1946–present
Date Last Searched: July 25, 2018
((exp Virtual Reality/ OR exp Virtual Reality Exposure Therapy/ OR virtual.af OR VR.af OR VRs.af OR VRaaS.af)
AND
(exp Head Protective Devices/ OR exp Computers, Handheld/ OR head mount* OR helmet OR helmets OR headset OR headsets OR “head set” OR “head sets” OR HMD OR OHMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windows OR microsoft OR merge OR zeiss OR razer OR sentics OR immerse OR glyph OR smartphone OR smartphones OR “smart phone” OR “smart phones” OR iphone OR iphones OR android).af)
OR
((oculus rift).af OR (google cardboard).af OR hololens.af OR “holo lens”.af OR (HTC vive).af OR (samsung gear).af OR (gear VR).af OR daydream.af OR “mixed reality”.af OR “leap motion”.af OR (vr one).af OR osvr.af)
Database Names: Embase & Embase Classic
Database Vendor: Elsevier
Database Coverage: 1947–present
Date Last Searched: July 25, 2018
((‘virtual reality’/exp OR ‘virtual reality exposure therapy’/exp OR ‘virtual reality simulator’/exp OR ‘virtual reality modeling language’/exp OR virtual OR VR OR VRs OR Vraas)
AND
(‘helmet’/exp OR ‘mobile phone’/exp OR (head AND mount*) OR helmet OR helmets OR headset OR headsets OR ‘head set’ OR ‘head sets’ OR HMD OR OHMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windows OR microsoft OR merge OR zeiss OR razer OR sentics OR immerse OR glyph OR smartphone OR smartphones OR ‘smart phone’ OR ‘smart phones’ OR iphone OR iphones OR android))
OR
((oculus AND rift) OR (google AND cardboard) OR hololens OR ‘holo lens’ OR ‘HTC vive’ OR (samsung AND gear) OR (gear AND VR) OR daydream OR ‘mixed reality’ OR ‘leap motion’ OR ‘vr one’ OR osvr)
Database Names: Cochrane Library
Database Vendor: Wiley
Database Coverage: Cochrane Reviews (Issue 7 of 12, July 2018)
Cochrane Trials (Issue 7 of 12, July 2018)
Date Last Searched: July 25, 2018
(([mh “Virtual Reality”] OR [mh “Virtual Reality Exposure Therapy”] OR virtual OR VR OR VR OR VRaaS)
AND
([mh “Head Protective Devices”] OR [mh “Computers, Handheld”] OR head mount* OR helmet OR helmets OR headset OR headsets OR “head set” OR “head sets” OR HMD OR OHMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windows OR microsoft OR merge OR zeiss OR razer OR sentics OR immerse OR glyph OR smartphone OR smartphones OR “smart phone” OR “smart phones” OR iphone OR iphones OR android))
OR
(oculus rift OR google cardboard OR hololens OR “holo lens” OR HTC vive OR samsung gear) OR gear VR OR daydream OR “mixed reality” OR “leap motion” OR vr one OR osvr)
Database Names: CINAHL Complete
Database Vendor: EBSCO
Database Coverage: 1937–present
Date Last Searched: July 25, 2018
((MH “Virtual Reality+” OR MH “Virtual Reality Exposure Therapy” OR MH “VRML” OR virtual OR VR OR VRs OR VRaaS)
AND
(MH “Head Protective Devices” OR MH “Computers, Hand-Held+” OR head mount* OR helmet OR headset OR “head set” OR “head sets” OR HMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windows OR microsoft OR merge OR zeiss OR immerse OR glyph OR smartphone OR “smart phone” OR “smart phones” OR iphone OR android))
OR
(oculus rift OR google cardboard OR hololens OR HTC vive OR samsung gear OR gear VR OR daydream OR “mixed reality” OR “leap motion” OR “vr one”)
Database Names: Web of Science
Database Vendor: Clarivate Analytics
Database Coverage: 1800–present
Date Last Searched: July 25, 2018
(((virtual NEAR/8 reality) OR VR OR VRs OR VRaaS)
AND
((head NEAR/8 mount*) OR helmet OR headset OR “head set” OR “head sets” OR HMD OR OHMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windows OR microsoft OR merge OR zeiss OR razer OR sentics OR immerse OR glyph OR daydream OR “mixed reality” OR “leap motion” OR smartphone OR smartphones OR “smart phone” OR “smart phones” OR iphone OR iphones OR android))
OR
((oculus NEAR/8 rift) OR google cardboard OR hololens OR “holo lens” OR HTC vive OR samsung gear OR gear VR OR “vr one” OR osvr)
Database Names: PsycINFO
Database Vendor: ProQuest
Database Coverage: 1800–present
Date Last Searched: July 25, 2018
((Exact(“virtual reality”) OR Exact(“virtual reality explosure therapy”) OR virtual OR VR OR VRs)
AND
(Exact(“head protective devices” OR “smartphone” OR “computers, handheld”) OR head mount* OR helmet OR headset OR “head set” OR HMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windows OR microsoft OR merge OR zeiss OR razer OR sentics OR immerse OR glyph OR daydream OR “mixed reality” OR smartphone OR smartphones OR “smart phone” OR “smart phones” OR iphone OR iphones OR android))
OR
(oculus rift OR google cardboard OR hololens OR HTC vive OR samsung gear OR gear VR OR “mixed reality” OR “leap motion” OR “vr one”)
Database Names: ERIC
Database Vendor: ProQuest
Database Coverage: 1966–present
Date Last Searched: July 25, 2018
((esu.Exact(“Virtual Reality”) OR virtual OR VR OR VRs)
AND
(Exact(“Handheld Devices”) OR head mount* OR helmet OR headset OR “head set” OR HMD OR htc OR oculus OR sony OR playstation OR samsung OR google OR intel OR windwos OR microsoft OR merge OR zeiss OR razer OR sentics OR immerse OR glyph OR daydream OR “mixed reality” OR smartphone OR smartphones OR “smart phone” OR “smart phones” OR iphone OR iphones OR android))
OR
(oculus rift OR google cardboard OR hololens OR gear VR)
Footnotes
Indicates studies that were included in the scoping review.
Contributor Information
David Saldana, David Saldana, MA, OTR/L, is Occupational Therapist, Beverly Hospital, Montebello, CA. At the time of the research, he was Student, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles..
Meghan Neureither, Meghan Neureither, OTD, OTR/L, is Occupational Therapist, Riverside Community Hospital, Riverside, CA. At the time of the research, she was Student, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles..
Allie Schmiesing, Allie Schmiesing, OTD, OTR/L, is Occupational Therapist, Stanford Hospital, Palo Alto, CA. At the time of the research, she was Student, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles..
Esther Jahng, Esther Jahng, MA, OTR/L, is Student, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles..
Lynn Kysh, Lynn Kysh, MS, is Clinical and Research Librarian, Institute for Nursing and Interprofessional Research, Children’s Hospital of Los Angeles, Los Angeles, CA..
Shawn C. Roll, Shawn C. Roll, PhD, OTR/L, RMSKS, FAOTA, FAIUM, is Associate Professor, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles.
Sook-Lei Liew, Sook-Lei Liew, PhD, OTR/L, is Assistant Professor, Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles; sliew@usc.edu.
References
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. 10.5014/ajot.2014.682006 [DOI] [PubMed] [Google Scholar]
- *Arias P., Robles-García V., Sanmartín G., Flores J., & Cudeiro J. (2012). Virtual reality as a tool for evaluation of repetitive rhythmic movements in the elderly and Parkinson’s disease patients. PLoS ONE, 7(1), e30021. 10.1371/journal.pone.0030021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H., & O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Bramer W. M., Giustini D., de Jonge G. B., Holland L., & Bekhuis T. (2016). De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association, 104, 240–243. 10.3163/1536-5050.104.3.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Carlozzi N., Gade V., Rizzo A., & Tulsky D. (2013). Using virtual reality driving simulators in persons with spinal cord injury: Three screen display versus head mounted display. Disability and Rehabilitation: Assistive Technology, 8, 176–180. 10.3109/17483107.2012.699990 [DOI] [PubMed] [Google Scholar]
- Gauthier L., Dehaut F., & Joanette Y. (1989). The Bells Test: A quantitative and qualitative test for visual neglect. International Journal of Clinical Neuropsychology, 11, 49–54. [Google Scholar]
- Hall C. D., Herdman S. J., Whitney S. L., Cass S. P., Clendaniel R. A., Fife T. D., . . . Woodhouse S. N. (2016). Vestibular rehabilitation for peripheral vestibular hypofunction: An evidence-based clinical practice guideline. Journal of Neurologic Physical Therapy, 40, 124–155. 10.1097/NPT.0000000000000120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson A., Korner-Bitensky N., & Levin M. (2007). Virtual reality in stroke rehabilitation: A systematic review of its effectiveness for upper limb motor recovery. Topics in Stroke Rehabilitation, 14, 52–61. 10.1310/tsr1402-52 [DOI] [PubMed] [Google Scholar]
- *Huang X., Naghdy F., Du H., Naghdy G., & Murray G (2018). Design of adaptive control and virtual reality–based fine hand motion rehabilitation system and its effects in subacute stroke patients. Computer Methods in Biomechanics and Biomedical Engineering: Imaging and Visualization, 6, 678–686. 10.1080/21681163.2017.1343687 [DOI] [Google Scholar]
- *Jannink M. J. A., Aznar M., de Kort A. C., van de Vis W., Veltink P., & van der Kooij H. (2009). Assessment of visuospatial neglect in stroke patients using virtual reality: A pilot study. International Journal of Rehabilitation Research, 32, 280–286. 10.1097/MRR.0b013e3283013b1c [DOI] [PubMed] [Google Scholar]
- Juliano J. M., Spicer R. P., Vourvopoulos A., Lefebvre S., Jann K., Ard T., . . . Liew S.-L. (2020). Embodiment is related to better performance on a brain–computer interface in immersive virtual reality: A pilot study. Sensors, 20, 1204 10.3390/s20041204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kang H. K., Kim Y., Chung Y., & Hwang S. (2012). Effects of treadmill training with optic flow on balance and gait in individuals following stroke: Randomized controlled trials. Clinical Rehabilitation, 26, 246–255. 10.1177/0269215511419383 [DOI] [PubMed] [Google Scholar]
- Kennedy R. S., Lane N. E., Berbaum K. S., & Lilienthal M. G. (1993). Simulator Sickness Questionnaire: An enhanced method for quantifying simulator sickness. International Journal of Aviation Psychology, 3, 203–220. 10.1207/s15327108ijap0303_3 [DOI] [Google Scholar]
- *Kurzynski M., Jaskolska A., Marusiak J., Wolczowski A., Bierut P., Szumowski L., . . . Kisiel-Sajewicz K. (2017). Computer-aided training sensorimotor cortex functions in humans before the upper limb transplantation using virtual reality and sensory feedback. Computers in Biology and Medicine, 87, 311–321. 10.1016/j.compbiomed.2017.06.010 [DOI] [PubMed] [Google Scholar]
- Laver K. E., Lange B., George S., Deutsch J. E., Saposnik G., & Crotty M. (2017). Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews, 2017, CD008349 10.1002/14651858.CD008349.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., & O’Brien K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, 69 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lubetzky A. V., Kary E. E., Harel D., Hujsak B., & Perlin K. (2018). Feasibility and reliability of a virtual reality Oculus platform to measure sensory integration for postural control in young adults. Physiotherapy Theory and Practice, 34, 935–950. 10.1080/09593985.2018.1431344 [DOI] [PubMed] [Google Scholar]
- *Lupu R. G., Irimia D. C., Ungureanu F., Poboroniuc M. S., & Moldoveanu A. (2018). BCI and FES based therapy for stroke rehabilitation using VR facilities. Wireless Communications and Mobile Computing , 2018, 4798359 10.1155/2018/4798359 [DOI] [Google Scholar]
- Melnyk B. M., & Fineout-Overholt E. (2011). Evidence-based practice in nursing and healthcare: A guide to best practice. Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- *Micarelli A., Viziano A., Augimeri I., Micarelli D., & Alessandrini M. (2017). Three-dimensional head-mounted gaming task procedure maximizes effects of vestibular rehabilitation in unilateral vestibular hypofunction: A randomized controlled pilot trial. International Journal of Rehabilitation Research, 40, 325–332. 10.1097/MRR.0000000000000244 [DOI] [PubMed] [Google Scholar]
- *Nunnerley J., Gupta S., Snell D., & King M. (2017). Training wheelchair navigation in immersive virtual environments for patients with spinal cord injury—End-user input to design an effective system. Disability and Rehabilitation: Assistive Technology, 12, 417–423. 10.1080/17483107.2016.1176259 [DOI] [PubMed] [Google Scholar]
- *Peskine A., Rosso C., Galland A., Caron E., Canet P., Jouvent R., & Pradat-Diehl P. (2011). Virtual reality navigation and visuospatial neglect after stroke [Abstract]. Cerebrovascular Diseases, 31(Suppl. 2), 193 10.1159/000329448 [DOI] [Google Scholar]
- Proffitt R., Schwartz J. K., Foreman M., & Smith R. O. (2019). Role of occupational therapy practitioners in mass market technology research and development. American Journal of Occupational Therapy, 73, 7301347010 10.5014/ajot.2019.028167 [DOI] [PubMed] [Google Scholar]
- Rausch M., Simon J. E., Starkey C., & Grooms D. R (2018). Smartphone virtual reality to increase clinical balance assessment responsiveness. Physical Therapy in Sport, 32, 207–211. 10.1016/j.ptsp.2018.05.017 [DOI] [PubMed] [Google Scholar]
- Rizzo A. A., Buckwalter J. G., & Neumann U. (1997). Virtual reality and cognitive rehabilitation: A brief review of the future. Journal of Head Trauma Rehabilitation, 12, 1–15. 10.1097/00001199-199712000-00002 [DOI] [Google Scholar]
- *Saldana S. J., Marsh A. P., Rejeski W. J., Haberl J. K., Wu P., Rosenthal S., & Ip E. H. (2017). Assessing balance through the use of a low-cost head-mounted display in older adults: A pilot study. Clinical Interventions in Aging, 12, 1363–1370. 10.2147/CIA.S141251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sarig Bahat H., Takasaki H., Chen X., Bet-Or Y., & Treleaven J. (2015). Cervical kinematic training with and without interactive VR training for chronic neck pain—A randomized clinical trial. Manual Therapy, 20, 68–78. 10.1016/j.math.2014.06.008 [DOI] [PubMed] [Google Scholar]
- *Sarig-Bahat H., Weiss P. L., & Laufer Y. (2009). Cervical motion assessment using virtual reality. Spine, 34, 1018–1024. 10.1097/BRS.0b013e31819b3254 [DOI] [PubMed] [Google Scholar]
- *Sarig-Bahat H., Weiss P. L., & Laufer Y. (2010). Neck pain assessment in a virtual environment. Spine, 35, E105–E112. 10.1097/BRS.0b013e3181b79358 [DOI] [PubMed] [Google Scholar]
- Schenkenberg T., Bradford D. C., & Ajax E. T. (1980). Line bisection and unilateral visual neglect in patients with neurologic impairment. Neurology, 30, 509–517. 10.1212/WNL.30.5.509 [DOI] [PubMed] [Google Scholar]
- Sherman W. R., & Craig A. B. (2002). Understanding virtual reality: Interface, application, and design. Burlington, MA: Morgan Kaufmann. [Google Scholar]
- *Subramanian S., Knaut L. A., Beaudoin C., & Levin M. F. (2007). Enhanced feedback during training in virtual versus real world environments. In 2007 Virtual Rehabilitation, Venice, Italy (pp. 8–13). Piscataway, NJ: IEEE 10.1109/ICVR.2007.4362121 [DOI] [Google Scholar]
- *Subramanian S. K., & Levin M. F. (2011). Viewing medium affects arm motor performance in 3D virtual environments. Journal of Neuroengineering and Rehabilitation, 8, 36 10.1186/1743-0003-8-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tossavainen T., Juhola M., Aalto H., Toppila E., Pyykkö I., Honkavaara P., . . . Laakso J. (2001). Postural control as assessed with virtual reality. Acta Oto-Laryngologica, 121(545), 53–56. 10.1080/000164801750388117 [DOI] [PubMed] [Google Scholar]
- Tricco A. C., Lillie E., Zarin W., O’Brien K. K., Colquhoun H., Levac D., . . . Straus S. E. (2018). PRISMA extension for scoping reviews (PRISMA–ScR): Checklist and explanation. Annals of Internal Medicine, 169, 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- *Viziano A., Micarelli A., Augimeri I., Micarelli D., & Alessandrini M. (2018). Long-term effects of vestibular rehabilitation and head-mounted gaming task procedure in unilateral vestibular hypofunction: A 12-month follow-up of a randomized controlled trial. Clinical Rehabilitation, 33, 24–33. 10.1177/0269215518788598 [DOI] [PubMed] [Google Scholar]
- Vourvopoulos A., Pardo O. M., Lefebvre S., Neureither M., Saldana D., Jahng E., & Liew S.-L. (2019). Effects of a brain–computer interface with virtual reality (VR) neurofeedback: A pilot study in chronic stroke patients. Frontiers in Human Neuroscience, 13, 210 10.3389/fnhum.2019.00210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson P. N., Foreman N., & Stanton D. (1997). Virtual reality, disability and rehabilitation. Disability and Rehabilitation, 19, 213–220. 10.3109/09638289709166530 [DOI] [PubMed] [Google Scholar]
- Yardley L., Gardner M., Lavie N., & Gresty M. (1999). Attentional demands of perception of passive self-motion in darkness. Neuropsychologia, 37, 1293–1301. 10.1016/S0028-3932(99)00024-X [DOI] [PubMed] [Google Scholar]
- *Zalewski-Zaragoza R. A., & Viirre E. S. (2003). Quantitative measurement of vertigo frequency: Preliminary results. Journal of Vestibular Research, 13, 53–56. [PubMed] [Google Scholar]