Abstract
EUS-guided gallbladder drainage (EUS-GBD) is gradually emerging as an option for patients with cholecystitis. A stent-bridged endoscopic intervention in the gallbladder (GB) has been proposed. The formation of a fistulous tract after EUS-GBD facilitates the entry of the endoscope inside the GB to perform endoscopic lithotomy and polypectomy, which is an efficient and safe procedure. However, the technical aspects of this procedure in order to optimize the success rate have only been scarcely discussed. This paper discusses the EUS-GBD prepared for per-oral cholecystolithotomy, the stent indwelling time, the procedure, the devices of per-oral cholecystolithotomy and the follow-up. The recently published literature on this topic is also updated in this review.
Keywords: Cholecystolithotomy, EUS, gallbladder drainage
INTRODUCTION
EUS-guided gallbladder drainage (EUS-GBD) is a promising and novel method to treat acute cholecystitis in high-risk surgical patients.[1,2,3,4] The technical and clinical success rates for EUS-GBD are reported to be more than 95%, with minor adverse events in <10% of the cases.[5,6] However, after EUS-GBD, most of the patients are followed with a “wait-and-see” strategy until clinical symptoms or stent-related adverse events develop.[7] For gallstones and gallbladder (GB) polys, further steps can be employed based on the drainage technique.
The path created by the stent can also serve as a conduit for a subsequent gallstone removal procedure.[8,9] This minimally invasive technique can preserve the GBs that still have an adequate function. Furthermore, this GB-preserving cholecystolithotomy method facilitated by EUS and the metal stents might have more advantages in comparison to previous percutaneous or laparoscopic GB-preserving cholecystolithotomy methods.[10,11]
However, the technical aspects of the procedure have been scarcely discussed. This paper the technical aspects of EUS-based cholecystolithotomy while providing an update of the recently published literature on the topic.
METHODS
This review first provides a brief summary of endoscopic cholecystolithotomy technique, which is based on the EUS-GBD. Then, this review is focused on the techniques for endoscopic cholecystolithotomy, which is presently very limited in the literature. We have searched PubMed using the following singular and combined search terms: <endoscopic ultrasound>; <gallbladder>; <drainage>; <gallstones>; <cholecystoscopy>; <Cholecystolithotomy>; <lumen-apposing metal stents>; <polyp-resection>; <cholecystitis>. Also, we have provided a discussion based on the experience from the tertiary endoscopic center.
RESULTS
The EUS-guided gallbladder drainage technique
The EUS-GBD technique started in 2007 when the double pigtail plastic stents or nasocystic drainage tube was used for the drainage. The EUS-GBD technique has undergone continuous improvement through the use of plastic stents, self-expandable metal stents, and a lumen apposing metal stent (LAMS); these continuous improvements have increased the success rate.[12] The LAMSs can keep the target object closely opposed to the gastrointestinal (GI) wall. However, the stenting procedure is technically challenging and time consuming. Then, the LAMS with an electro-cautery enhanced delivery system (ECE-LAMS) was introduced and it significantly shortened the operation time.
The studies that refer to the learning curve of EUS-GBD indicate that endoscopists that have performed EUS-GBD are expected to achieve a reduction in the procedure time over successive cases. In terms of the efficiency, the procedure requires 41 min with a learning rate of 19 cases.[13] However, the results were drawn from highly experienced and specialized endoscopists in the tertiary centers. For those who have limited experience with interventional EUS, they may require hands-on training with ex vivo or animal models followed by a standard protocol.[14]
On the other hand, dedicated auxiliary devices can enhance the safety of EUS-GBD that are still in need before introducing the technique effectively and safely to the wider endoscopic society. In an animal study, Zhang et al.[15] reported that the retrievable anchor (RA) delivered by the fine-needle aspiration needle could replace the guidewire. It is preplaced in the GB before the stent insertion, which would hold the GB close to the duodenal wall and it stabilizes the GB when introducing the stent. It is believed that the RA has several advantages. First, the anchored GB is more stable for the stent to target. Second, bile leakage may also be reduced because the puncture site is pressed by the duodenal wall. Third, in the stent release process, pulling the GB can make the internal space larger, which is more conducive to reducing the probability of the stenting failure. Of note, these anchors are nondamaging to the GB, and they are retrievable. This method heightens the probability of success by ensuring a simpler and safer procedure. Operator confidence is boosted as well.
Per-oral cholecystoscopy followed by EUS-guided gallbladder drainage
The fistula created between the GI tract and the GB enables the exploration inside the GB by the endoscope per-orally, which is also termed as peroral cholecystoscopy.[16,17] The applications include: GB mucosa detection (i.e., magnifying endoscopy observation, electronic staining, and confocal endomicroscopy examination),[18] EUS evaluation, removing gallstones, lithotripsy of gallstones,[19] and polyp-resection.[20] From these, gallstone removal is the most reported therapy [Table 1].
Table 1.
Endoscopic cholecystolithotomy
| Author | Year | Cases | Spot for the drainage | Stents type | Stents diameter | Indwelling time | Stone clearance | Spontaneous stone clearance | |
|---|---|---|---|---|---|---|---|---|---|
| Stomach | Duodenum | ||||||||
| Itoi et al.[21] | 2014 | 1 | 1 | N | Cold AXIOS | 15 mm | 14 days | 1/1 | N |
| Ge et al.[22] | 2016 | 7 | 4 | 3 | Microtech stent | 10/35 mm | 9 days | 7/7 | N |
| Larghi et al.[19] | 2016 | 1 | 1 | N | Hot AXIOS | 15/10 mm | N | 1/1 | N |
| Chan et al.[18] | 2017 | 25 | 6 | 19 | Cold/hot AXIOS | 15/10 mm | 1-3 month(s) | 22/25 | 14/25 |
N: Not reported.
How to perform endoscopic cholecystolithotomy
Which stent used in EUS-guided gallbladder drainage can facilitate further endoscopic access?
LAMPs with an antimigration design are usually applied in the EUS-GBD, which are equipped with a “cold” or “hot” deliver system.[23] The hot stents equipped with a cautery tipped delivery system can complete the procedure with a single-step without the tract dilation with cystotome or other dilators. This includes the HOT AXIOS stent (15 mm × 10 mm or 10 mm × 10 mm diameter, Boston Scientific, Marlborough, Massachusetts, United States) and the Microtech stent (10 mm × 35 mm length, Nan Jing Co. Ltd., China). The “cold” stents include the BONA-AL stent (10 mm × 4–7 cm in length with 22 mm external flares, Standard Sci Tech Inc., Seoul, Korea) and the SPAXUS stent (10 mm × 10 mm, and 10 mm × 16 mm, Niti-S, Taewoong Medical, Korea). The overall adverse effect (AE) rate of LAMS in EUS-GBD was 13%, which includes an early AE of 6.5% and a delayed AE of 8%.[24] When deploying the LAMS, the stent-release-within-scope-channel technique was used to avoid the displacement.[25]
What is the superior spot for the drainage: The antrum or the duodenum?
First, it should be noted that a transduodenal approach is optimal for gallstone removal in comparison to the transgastric path. If a transgastric path were chosen for the puncture, food impaction would occur in the GB that would be difficult to remove and it might have a potential risk of contaminating the bile duct system.[26]
Besides, a small stone could pass through the LAMPS spontaneously when the transduodenal approach is applied. More than 10% of the cases were found with no stone residuals a couple of days after the drainage.
In a study by Chan et al.,[18] food residue was found in two patients, and an attempt to prevent food entry into the GB was made by inserting pigtail stents through the LAMS, which also failed. Similar food impaction was also reported by Ge et al. presently, there is no effective method to prevent food impaction in the GB. As a result, drainage of the GB via the duodenum has been advocated.
When should gallstone removal be performed or does GB exploration occur after EUS-guided gallbladder drainage (the stent’s indwelling time)?
In most reported studies, the indication for EUS-GBD is to treat acute cholecystitis in high-risk surgical patients.[27] The stents should remain in place as long as possible.[28] In a study by Choi et al.,[29] the median stent patency was 190 days (15–1185 days) and 458 days (151–1185 days) for the patients who were alive at the end of the study end, and the rate of late AEs was 7%.
If the EUS-GBD was followed by a gallstone removal procedure, the path created by the stent should serve as a temperate conduit for it. The prolonged stent indwelling time after relieving the cholecystitis symptoms may not benefit per-oral cholecystoscopy. The stent should remain until the mature fistula was formed, then the endoscope could enter the GB. The rate of stent-related AEs may increase with the prolonged indwelling time. In a study by Chen,[18] LAMS covered with granulation tissue was found in one patient, which caused the failure of a subsequent gallstone removal. The stent’s indwelling time in this study was 1–3 months. In a study by Kamata et al.,[6] the metal stents were removed 4 weeks after placement in order to avoid stent migration and the recurrence of cholecystitis due to food impaction. In another study by Ligresti et al.,[30] they reported that the longer stent indwelling time resulted in a buried stent and it was rescued with the LAMS-in-LAMS technique. It seems that the indwelling time is longer than 4 weeks, which may increase the risk of a stent-related AE.
The endoscopic cholecystolithotomy should be performed as soon as the symptom of cholecystitis is improved and the mature fistula is formed. In addition, the stent should be removed immediately after the successful stone removal. As reported in our previous study,[22] the following endoscopic cholecystolithotomy was usually performed around 14 days after the EUS-GBD. On the other hand, a shorter time with <10 days of duration may not be enough for the formation of the fistulous tract and this can increase the risk of fistula rupture during the cholecystolithotomy procedure. A stent indwelling time that is <10 days may not be safe to perform peroral cholecystoscopy. However, the minimum stent indwelling time for the mature fistula formation and to facilitate the stone removal procedure with an endoscope needs to be further verified.
Procedure of stone removal
When a fistula is formed between the GI tract and the GB after cholecystostomy with ECE-LAMS, per-oral cholecystoscopy can be performed. The endoscope (e.g., gastroscope, transnasal gastroscope, or ultraslim endoscope) was advanced into the GB via the fistula formed by the stent. A stone basket was inserted into the GB to retrieve the stones [Figure 1]. The stone retrieval basket was withdrawn from the GB, and the stones were discharged into the GI tract. Water flushing may be helpful for the stone grasping procedure. After several deployments of the basket to remove the stones, an endoscope was introduced into the GB to check for any remaining stones. If the LAMS was mal-deployed and it prohibited the entry of the endoscope into the GB, or occasionally gallstones were hidden behind the large flange of the stent, the LAMS could be removed before advancing the endoscope. If necessary, the fistula could be dilated by a balloon catheter, which can subsequently facilitate the insertion of an endoscope or extract gallstones with a larger diameter.
Figure 1.

A stone basket was inserted into the GB to retrieve the stones
The device used for cholecystolithotomy
The device used for cholecystolithotomy has long been used in ERCP procedures. This is similar to holmium laser lithotripsy (SlimLine SIS GI holmium laser fiber; lumenis) for larger gallstones, fiber-optic cholangioscopy (SpyGlass, Boston Scientific), Roth net (US Endoscopy, Mentor, Ohio, USA), and a stone retrieval basket (22Q; Olympus Medical, Tokyo, Japan). Foreign body net could also be used to grasp the scattered small stones [Figure 2]. Most of these devices are designed for stone-grasping movements in a tubular lumen such as the bile duct. For example, the protruding structure at the distal end of the basket was not efficient for the GB and it may easily injure the GB mucosa while grasping for a stone within the GB. Thus, modification of the basket is necessitated so it fits into a spherical lumen.
Figure 2.

A net was inserted to retrieve the small stones near the neck of the G
How to guarantee stone removal without any residuals?
Cystic duct radiography is an important procedure to rule out a residual stone in the structure of the cystic duct [Figure 3]. However, injection of a contrast agent into the cystic duct with an ERCP catheter is not easy because of the existence of the Heister valve. In our experience, a lithotomy balloon can be helpful when injecting a contrast agent. There are two ways to perform cystic duct radiography. First, the balloon can be placed at the neck of the GB, and the air-filled balloon can block the proximal opening of the cystic duct, which can facilitate the contrast agent injection with pressure. Second, the balloon can be completely filled with air while within the GB and then be withdrawn until the fistula is blocked. The injected contrast agent fills the GB and goes into the cystic duct.
Figure 3.
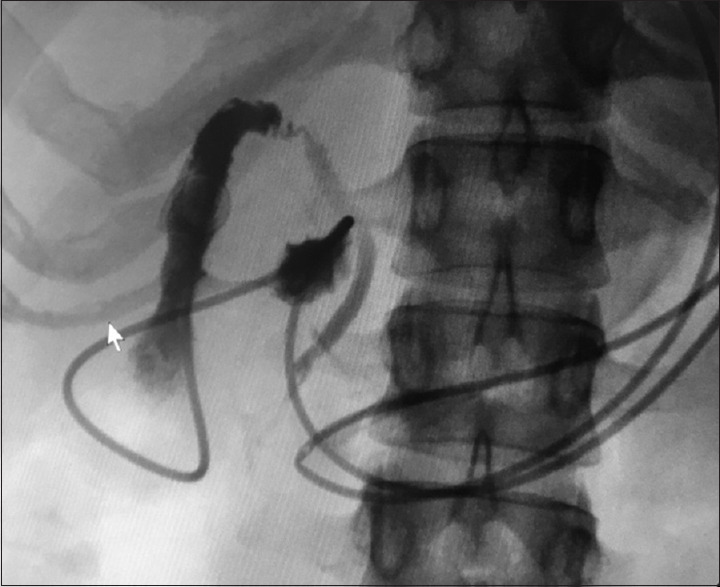
Cystic duct radiography to rule out a residual stone in the structure of the cystic duct
Follow-up after endoscopic cholecystolithotomy
The standard protocol for the follow-up after endoscopic cholecystolithotomy has not been established yet. In light of the previous experiences, we may suggest a normal diet should be resumed 48 h after the stent removal; regular ursodeoxycholic acid should be taken orally for at least 6 months; regular US examination should be performed at 1, 3, 6, and 12 months after the treatment in the 1st year and every 12 months thereafter. These procedures can be followed and verified in further studies.
CONCLUSION
After nearly 10 years of development, EUS-GBD appears to be an attractive alternative for managing acute cholecystitis in high-risk patients. The formation of a fistulous tract after EUS-GBD facilitates the entry of the endoscope inside the GB to perform endoscopic lithotomy and polypectomy, which is an efficient and safe procedure. This technique needs to be further verified by conducting long-term multicenter prospective studies.
Financial support and sponsorship
National Natural Science Foundation of China (grant no. 81770655); China Postdoctoral Science Foundation (grant no. 2019M661174).
Conflicts of interest
Siyu Sun is a Consultant of Vedkang Company and Nanjing Microtech Company.
REFERENCES
- 1.Chaudhary S, Sun S. Endoscopic ultrasound-guided gallbladder drainage: Redefines the boundaries. Endosc Ultrasound. 2016;5:281–3. doi: 10.4103/2303-9027.191605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakai Y, Isayama H, Matsubara S, et al. Conversion of transpapillary drainage to endoscopic ultrasound-guided hepaticogastrostomy and gallbladder drainage in a case of malignant biliary obstruction with recurrent cholangitis and cholecystitis (with videos) Endosc Ultrasound. 2017;6:205–7. doi: 10.4103/2303-9027.208172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dollhopf M, Larghi A, Will U, et al. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc. 2017;86:636–43. doi: 10.1016/j.gie.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 4.Small AJ, Irani S. EUS-guided gallbladder drainage vs. percutaneous gallbladder drainage. Endosc Ultrasound. 2018;7:89–92. doi: 10.4103/eus.eus_8_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peñas-Herrero I, de la Serna-Higuera C, Perez-Miranda M. Endoscopic ultrasound-guided gallbladder drainage for the management of acute cholecystitis (with video) J Hepatobiliary Pancreat Sci. 2015;22:35–43. doi: 10.1002/jhbp.182. [DOI] [PubMed] [Google Scholar]
- 6.Kamata K, Takenaka M, Kitano M, et al. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis: Long-term outcomes after removal of a self-expandable metal stent. World J Gastroenterol. 2017;23:661–7. doi: 10.3748/wjg.v23.i4.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed O, Ogura T, Eldahrouty A, et al. Endoscopic ultrasound-guided gallbladder drainage: Results of long-term follow-up. Saudi J Gastroenterol. 2018;24:183–8. doi: 10.4103/sjg.SJG_506_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ge N, Wang S, Wang S, et al. Endoscopic ultrasound-assisted cholecystogastrostomy by a novel fully covered metal stent for the treatment of gallbladder stones. Endosc Ultrasound. 2015;4:152–5. doi: 10.4103/2303-9027.156749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ge N, Wang Z, Sun S, et al. EUS assisted transmural cholecystogastrostomy fistula creation as a bridge for endoscopic internal gallbladder therapy using a novel fully covered metal stent. BMC Gastroenterol. 2014;14:164. doi: 10.1186/1471-230X-14-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teoh AY, Serna C, Penas I, et al. Endoscopic ultrasound-guided gallbladder drainage reduces adverse events compared with percutaneous cholecystostomy in patients who are unfit for cholecystectomy. Endoscopy. 2017;49:130–8. doi: 10.1055/s-0042-119036. [DOI] [PubMed] [Google Scholar]
- 11.Tyberg A, Saumoy M, Sequeiros EV, et al. EUS-guided versus percutaneous gallbladder drainage: Isn’t it time to convert? J Clin Gastroenterol. 2016;52:79–84. doi: 10.1097/MCG.0000000000000786. [DOI] [PubMed] [Google Scholar]
- 12.James TW, Baron TH. EUS-guided gallbladder drainage: A review of current practices and procedures. Endosc Ultrasound. 2019;8:S28–34. doi: 10.4103/eus.eus_41_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tyberg A, Jha K, Shah S, et al. EUS-guided gallbladder drainage: A learning curve modified by technical progress. Endosc Int Open. 2020;8:E92–6. doi: 10.1055/a-1005-6602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teoh AY. EUS-guided gallbladder drainage: Is it so easy? Endosc Int Open. 2020;8:E97–8. doi: 10.1055/a-1036-6337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang K, Sun S, Guo J, et al. Retrievable puncture anchor traction method for EUS-guided gallbladder drainage: A porcine study. Gastrointest Endosc. 2018;88:957–63. doi: 10.1016/j.gie.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Itoi T, Tsuchiya T, Sofuni A, et al. Development of EUS-guided gallbladder drainage and current indications. Endosc Ultrasound. 2018;7:76–8. doi: 10.4103/eus.eus_4_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan JH, Teoh AY. The development of peroral cholecystoscopy and advanced gallbladder interventions. Endosc Ultrasound. 2018;7:85–8. doi: 10.4103/eus.eus_7_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan SM, Teoh AY, Yip HC, et al. Feasibility of per-oral cholecystoscopy and advanced gallbladder interventions after EUS-guided gallbladder stenting (with video) Gastrointest Endosc. 2017;85:1225–32. doi: 10.1016/j.gie.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 19.Larghi A, Rimbas M, Attili F, et al. Endoscopic holmium laser lithotripsy of symptomatic gallstones through a lumen-apposing self-expandable metal stent. Am J Gastroenterol. 2016;111:1516. doi: 10.1038/ajg.2016.258. [DOI] [PubMed] [Google Scholar]
- 20.Tian L, Yang Y, Xiao D, et al. Resection of gallbladder polyps following endoscopic ultrasound-guided cholecystoduodenostomy using a lumen-apposing metal stent. Endoscopy. 2018;50:E307–8. doi: 10.1055/a-0631-7970. [DOI] [PubMed] [Google Scholar]
- 21.Itoi T, Itokawa F, Tsuchiya T, et al. Transgastric large gallstone extraction through a lumen-apposing metal stent in a patient with acute cholecystitis. Gastrointest Endosc. 2014;79:547. doi: 10.1016/j.gie.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 22.Ge N, Sun S, Sun S, et al. Endoscopic ultrasound-assisted transmural cholecystoduodenostomy or cholecystogastrostomy as a bridge for per-oral cholecystoscopy therapy using double-flanged fully covered metal stent. BMC Gastroenterol. 2016;16:9. doi: 10.1186/s12876-016-0420-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leung Ki EL, Napoleon B. EUS-specific stents: Available designs and probable lacunae. Endosc Ultrasound. 2019;8:S17–27. doi: 10.4103/eus.eus_50_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohan BP, Asokkumar R, Shakhatreh M, et al. Adverse events with lumen-apposing metal stents in endoscopic gallbladder drainage: A systematic review and meta-analysis. Endosc Ultrasound. 2019;8:241–8. doi: 10.4103/eus.eus_63_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogura T, Okuda A, Miyano A, et al. Stent release within scope channel technique to prevent stent migration during EUS-guided hepaticogastrostomy (with video) Endosc Ultrasound. 2018;7:67–8. doi: 10.4103/eus.eus_57_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perez-Miranda M. Technical considerations in EUS-guided gallbladder drainage. Endosc Ultrasound. 2018;7:79–82. doi: 10.4103/eus.eus_5_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adler DG. EUS-guided gallbladder drainage: Current status and future prospects. Endosc Ultrasound. 2018;7:1–3. doi: 10.4103/eus.eus_3_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saumoy M, Novikov A, Kahaleh M. Long-term outcomes after EUS-guided gallbladder drainage. Endosc Ultrasound. 2018;7:97–101. doi: 10.4103/eus.eus_9_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choi JH, Lee SS, Choi JH, et al. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014;46:656–61. doi: 10.1055/s-0034-1365720. [DOI] [PubMed] [Google Scholar]
- 30.Ligresti D, Cipolletta F, Amata M, et al. Buried lumen-apposing metal stent (LAMS) following endoscopic ultrasound-guided gallbladder drainage: The LAMS-in-LAMS rescue treatment. Endoscopy. 2018;50:822–3. doi: 10.1055/a-0624-2050. [DOI] [PubMed] [Google Scholar]


