Abstract
Lung cancer is the leading cause of cancer death worldwide and the third most common cancer following breast and prostate.1 As expected, the primary factor leading to lung cancer is tobacco smoke, and as smoking rates have declined, we have also seen an overall decline in lung cancer rates.2 Despite the general reduction in lung cancer rates, the rate of lung cancer in non-smokers has been noted to be increasing.3–8
Introduction
With the overall rates of lung cancer and tobacco smoking declining, the evaluation of lung cancer in non-smokers has become of clinical interest. Several studies have suggested that lung cancer in non-smokers is different from both a biologic and epidemiologic perspective such that it should be looked at as a completely distinct entity.9 When discussing lung cancer in non-smokers, the term “non-smoker” or “never smoker” classically refers to individuals who have smoked less than 100 cigarettes in their lives. In terms of the type of cancer, non-smokers are mainly afflicted with non-small cell lung cancer, predominantly adenocarcinoma. Due to the exceedingly low rates of small cell lung cancer in non-smokers, this will not be addressed further here.10 In this article we will review the epidemiology, risk factors and treatments for lung cancer in nonsmokers.
Epidemiology
Worldwide, 15–20 percent of men with lung cancer are non-smokers while over 50 percent of women with lung cancer are non-smokers.11 This demographic has some significant geographic differences as lung cancer in non-smoking women in Asia comprises approximately 60–80 percent of the cases of lung cancer.12 In a study performed in the United States, roughly 19 percent of women with lung cancer were non-smokers, and only 9 percent of men with lung cancer were non-smokers.13 As this data has shown, lung cancer in non-smokers tends to be more common in females (Table 1).
Table 1.
Lung Cancer – Smokers vs Non-Smokers
| Lung cancer | ||
|---|---|---|
| Smokers | Non-Smokers | |
| Age at diagnosis | 66 years | 67 years |
| Sex predominance | Male | Female |
| Most common subtype | Adenocarcinoma (65%) | Adenocarcinoma (93%) |
| Time to seek medical care | 2 months | 3 months |
| EGFR mutations | 8% | 36% |
| ALK mutations | 4% | 26% |
| Stage IV at diagnosis | 49% | 62% |
Data taken from:
Margarida Dias, Rita Linhas, Sérgio Campainha, Sara Conde & Ana Barroso(2017) Lung cancer in never-smokers – what are the differences?, Acta Oncologica, 56:7, 931–935
Along with this data, there have been several studies to suggest the rates of lung cancer in non-smokers is overall increasing.3–8 The evidence on mortality rates among non-smokers versus smokers with lung cancer has been conflicting. Some studies have suggested lower mortality rates in the non-smoking population.14 Despite this, other studies have indicated no significant difference or even a possible increase in mortality.5 One finding that has been consistent is that despite non-smoking women more frequently being diagnosed with lung cancer, they do have an overall decreased mortality when compared to men.24 This data is similar in the smoking population as well, as women have been known to live longer than men with lung cancer.15 The age at which lung cancer is diagnosed in non-smokers has classically been considered to be a younger population. Recent studies looking at the age of diagnosis have refuted this clam as the majority of non-smokers with lung cancer were diagnosed at an older age as compared to smokers.16
Risk Factors
There have been several suspected risk factors for lung cancer in non-smokers, but none are known to be directly causative at this time. Several of the proposed essential risk factors will be discussed.
Age
Age at diagnosis for lung cancer in non-smokers has classically been considered to be a younger person’s disease. Several studies have refuted this claim, showing that increasing age is a common predisposing factor.16–17 The increased risk with age is felt to be due to the duration of exposure to potential carcinogens throughout one’s life (e.g., secondhand cigarette smoke, radon gas).
Secondhand Smoke
Secondhand smoke has been implicated in the development of lung cancer in non-smokers.25 Multiple studies have suggested that 15–35 percent of lung cancer in non-smokers is due to secondhand smoke exposure.18 Importantly, there is also an increased risk for those non-smokers that have a spouse that is a smoker. In a meta-analysis that included 55 studies, it was found that women who were married to a smoker had a 27% increase in risk of lung cancer.19
Environmental Exposures
Several studies have also linked environmental exposures to lung cancer — some known exposures including asbestos, chromium, and arsenic.21 There have also been studies linking indoor and outdoor air pollution to the development of lung cancer.20 Asbestos exposure that is complicated by intestinal fibrosis or asbestosis is noted to lead to increased lung cancer rates. In one study, it was noted that asbestos exposure alone lead to a six-fold increase in relative risk of developing lung cancer, while asbestos exposure and smoking lead to a 59-fold increase. 22
In developing countries, chronic exposure to cooking fumes from burning wood or frying has been linked to an increased rate of lung cancer in non-smokers. 20 This problem is most evident in developing countries where women are primarily in charge of cooking duties and can spend hours each day cooking amongst open flames. This exposure is thought to be the cause of some of the disproportionate lung cancer rates within this population.20 Additionally, animal dung/feces can be dried and used as fuel, which when inhaled can also lead to increased risk of cancer and reactive airway disease.
Radon
Another potential risk factor is radon. Radon is a decay product of uranium-238, as well as radium-226, and possesses the capability of damaging respiratory epithelium via emissions of alpha particles. Radon is known to be present in soil, rock, and groundwater and due to this, it can accumulate in homes. Although controversial, exposure to radon within homes may play a role in the development of lung cancer in non-smokers. 23 There is a known increased risk of lung cancer among uranium miners which is felt to be due to radon exposure. The increased radon exposure in this group has more clearly linked the exposure to lung cancer.24 In a meta-analysis of 13 studies, there was a reported a direct relationship between the level of radon detected in homes and the risk of developing lung cancer; based on this information the authors estimated that radon exposure might be responsible for up to 2 percent of lung cancer deaths in Europe.25
Genetic Factors
Lung cancer in non-smokers is felt to have a genetic predisposition as many studies have shown that those with a family history of lung cancer are at increased risk.26 To further illustrate this importance, in one case-control study that looked at over 2,400 relatives of 316 cases of lung cancer in non-smokers, there was a 25 percent increased risk of any cancer among the first degree relatives. There was also an increased risk of early onset (age less than 50 years) lung cancer among the relatives who smoked.27 While this study does not directly link a history of lung cancer in non-smokers to future generations developing lung cancer, it does show the importance of genetic factors leading to the development of cancer as well as the risk involved when genetically susceptible individuals partake in smoking. There are specific germline mutations that have been identified in families with high rates of lung cancer in non-smokers. The most prominent of these is the germline mutation in the epidermal growth factor receptor (EGFR).28 The identification of this mutation has led to specific advances in targeted treatment for individuals with this mutation, which is seen mainly in non-smokers with lung cancer.29
Lung Disease
Another important risk factor for the development of lung cancer in non-smokers is underlying lung disease. Lung disease can be due to many different factors which range from pre-existing disease or from chemotherapy and radiation.26 The extent of this risk is not truly known as the majority of lung disease is related to smoking. Also, when looking at pulmonary fibrosis, studies also suggest there is some increased risk related directly to the disease.27
Oncogenic Viruses
Several viruses have been implicated in the development of cancer. Some of these include Epstein-bar virus (EBV), human papillomavirus (HPV), and Hepatitis B and C. Of these, HPV has known associations with head and neck cancers as well as potential implications in lung cancer.28 Despite these potential implications, a meta-analysis on the role of HPV and the development of lung cancer in non-smokers was inconclusive.29
Estrogens
It has been postulated that estrogens and other female hormones could be leading to the increased risk of lung cancer in non-smokers.11 It has also been noted that many of the non-small cell lung cancers express an estrogen receptor, and expression of this receptor is more common in lung cancer seen in non-smokers as compared to smokers.30
Biologic Differences
There are several differences in lung cancer between smokers and non-smokers; some of these include pathologic differences as well as molecular differences.
Pathologic Differences
Non-small cell lung cancer, mainly adenocarcinoma, is more common in non-smokers and light smokers, as well as former smokers. For heavy smokers, squamous cell carcinoma and small cell lung cancer are seen more commonly.31
Molecular Differences
With advances in the understanding of the molecular biology of cancer there have been found substantial differences between lung cancer in smokers versus non-smokers. Several studies have suggested that lung cancer in non-smokers is different enough from a biologic and epidemiologic perspective to be looked at as a completely different entity.9
Many different mutations have been found. The most common include the epidermal growth factor receptor (EGFR), Kirsten rat sarcoma viral oncogene homolog (KRAS) mutation and anaplastic lymphoma kinase (ALK) gene rearrangement. Due to these known mutations, there has been a significant effort in attempts to find “driver” mutations in non-small cell lung cancer. Driver mutations are those mutations that appear to be leading to or “driving” a particular cancer. The National Cancer Institute’s lung cancer mutation consortium presented data at the American Society of Clinical Oncology annual meeting on the evaluation of 800 patients with non-small cell lung cancer and showed that 25 percent had KRAS mutations, 23 percent had EGFR mutations, and 6 percent had ALK rearrangements.32
Further data has shown that mutations in EGFR are more common in lung cancer of non-smokers compared to smokers.33 Studies on the KRAS mutation have demonstrated that the mutation occurs at approximately the same rate in smokers as well as non-smokers with lung cancer, but the mutations are different with more transition mutations occurring in non-smokers compared to transversion mutations occurring is smokers.34
Lung Cancer Screening in Non-Smokers
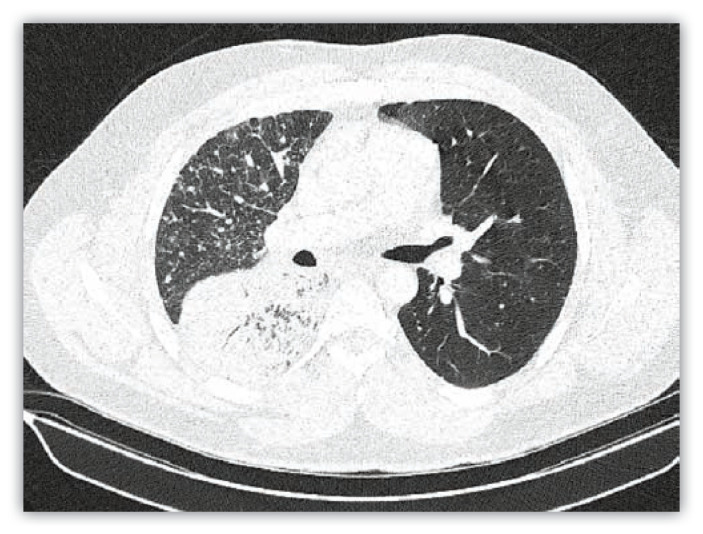
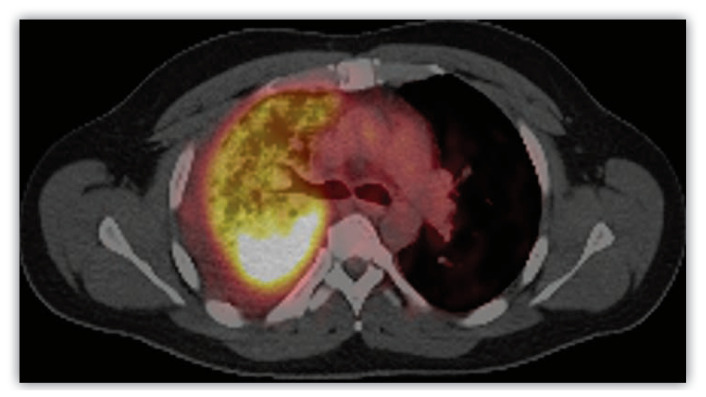
Currently, there are no guidelines to recommend lung cancer screening in non-smokers. Symptoms of lung cancer are often nonspecific and include no symptoms to cough, dyspnea, weight loss, and loss of appetite. More specific symptoms do include chest pain and hemoptysis but these can be shared by many different diseases. Even in the setting of multiple symptoms there are still no guidelines to recommend screening for lung cancer in non-smokers. Current guidelines do recommend lung cancer screening in those 55–79 years of age with at least 30 pack year smoking, who are current smokers or have quit smoking in the past 15 years. In this setting, a screening low dose chest CT is appropriate. Despite there being no guidelines to recommend lung cancer screening in non-smokers, those with increased risk based on family history or other risk factors should be closely monitored for the development of symptoms that would warrant further testing (Figures 1 and 2).
Figure 1.
Atypical radiographic appearance of adenocarcinoma of the lung on CT imaging.
Figure 2.
Atypical radiographic appearance of adenocarcinoma of the lung on PET imaging.
Treatment
Non-smokers with lung cancer do not appear to respond better to standard treatment or have a better prognosis than smokers. Some studies have shown improved outcomes while others have not.35 Despite this, there have been some newly developed targeted treatments that have shown promise in lung cancer due to specific genetic mutations. One such class is the EGFR tyrosine kinase inhibitors which include erlotinib, gefitinib, afatinib, and osimertinib. Studies involving these medications have suggested improved response rates and survival in non-smokers over smokers. The improved response rates are felt to be driven by the fact that this mutation is seen more commonly in non-smokers than smokers and that regardless of smoking status patients with these mutations have improved outcomes with these medications.36
Summary
Non-smokers are those who have smoked less than 100-lifetime cigarettes. Lung cancer in non-smokers is almost exclusively non-small cell lung cancer, with adenocarcinoma being the most common type. Non-smoking women are more likely to get lung cancer than non-smoking men. Regardless of smoking status, women with lung cancer tend to outlive men with lung cancer. It has classically been taught that lung cancer in non-smokers occurs at a younger age, but current data does not seem to suggest this. There are several risk factors for the development of lung cancer in non-smokers and some of these include; age, secondhand smoke, cooking fumes, radon, environmental exposures, genetic factors, underlying lung disease, oncogenic viruses, and estrogens. There are many different genetic mutations seen in non-small cell lung cancer. Some of the most frequently occurring in non-smokers include EGFR mutations, KRAS mutations, and ALK rearrangements. With the discovery of specific genetic mutations, there has been the development of particular treatment targets to these mutations which have shown promise in the treatment of lung cancer.
Footnotes
Sarah Dubin, MD, MPH, and Daniel Griffin, DO, practice Pulmonary and Critical Care medicine in the Truman Medical Center Health Sciences District, Kansas City, Missouri.
Disclosure
None reported.
References
- 1.U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (1999–2015) U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; Jun, 2018. www.cdc.gov/cancer/dataviz. [Google Scholar]
- 2.Giovino GA. Epidemiology of tobacco use in the United states. Oncogene. 2002;21:7326. doi: 10.1038/sj.onc.1205808. [DOI] [PubMed] [Google Scholar]
- 3.Boffetta P, Järvholm B, Brennan P, Nyrén O. Incidence of lung cancer in a large cohort of non-smoking men from Sweden. Int J Cancer. 2001;94:591. doi: 10.1002/ijc.1507. [DOI] [PubMed] [Google Scholar]
- 4.Zell JA, Ou SH, Ziogas A, Anton-Culver H. Epidemiology of bronchioloalveolar carcinoma: improvement in survival after release of the 1999 WHO classification of lung tumors. J Clin Oncol. 23:8396. doi: 10.1200/JCO.2005.03.0312. [DOI] [PubMed] [Google Scholar]
- 5.Peto R, Darby S, Deo H, et al. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000;321:323. doi: 10.1136/bmj.321.7257.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cufari ME, Proli C, De Sousa P, et al. Increasing frequency of non-smoking lung cancer: Presentation of patients with early disease to a tertiary institution in the UK. Eur J Cancer. 2017;84:55. doi: 10.1016/j.ejca.2017.06.031. [DOI] [PubMed] [Google Scholar]
- 7.Thun MJ, Hannan LM, Adams-Campbell LL, et al. Lung cancer occurrence in never-smokers: an analysis of 13 cohorts and 22 cancer registry studies. PLoS Med. 2008;5:e185. doi: 10.1371/journal.pmed.0050185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pelosof L, Ahn C, Gao A, et al. Proportion of Never-Smoker Non-Small Cell Lung Cancer Patients at Three Diverse Institutions. J Natl Cancer Inst. 2017;109 doi: 10.1093/jnci/djw295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yano T, Miura N, Takenaka T, et al. Never-smoking nonsmall cell lung cancer as a separate entity: clinicopathologic features and survival. Cancer. 2008;113:1012. doi: 10.1002/cncr.23679. [DOI] [PubMed] [Google Scholar]
- 10.Kurahara Y, Kawaguchi T, Tachibana K, et al. Small-cell lung cancer in never-smokers: a case series with information on family history of cancer and environmental tobacco smoke. Clin Lung Cancer. 2012;13:75. doi: 10.1016/j.cllc.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 12.Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers--a different disease. Nat Rev Cancer. 2007;7:778. doi: 10.1038/nrc2190. [DOI] [PubMed] [Google Scholar]
- 13.Wakelee HA, Chang ET, Gomez SL, et al. Lung cancer incidence in never smokers. J Clin Oncol. 2007;25:472. doi: 10.1200/JCO.2006.07.2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawaguchi T, Matsumura A, Fukai S, et al. Japanese ethnicity compared with Caucasian ethnicity and never-smoking status are independent favorable prognostic factors for overall survival in non-small cell lung cancer: a collaborative epidemiologic study of the National Hospital Organization Study Group for Lung Cancer (NHSGLC) in Japan and a Southern California Regional Cancer Registry databases. J Thorac Oncol. 2010;5:1001. doi: 10.1097/JTO.0b013e3181e2f607. [DOI] [PubMed] [Google Scholar]
- 15.Donington JS, Le QT, Wakelee HA. Lung cancer in women: exploring sex differences in susceptibility, biology, and therapeutic response. Clin Lung Cancer. 2006;8:22. doi: 10.3816/CLC.2006.n.029. [DOI] [PubMed] [Google Scholar]
- 16.Dias Margarida, Linhas Rita, Campainha Sérgio, Conde Sara, Barroso Ana. Lung cancer in never-smokers – what are the differences? Acta Oncologica. 2017;56(7):931–935. doi: 10.1080/0284186X.2017.1287944. [DOI] [PubMed] [Google Scholar]
- 17.Thun MJ, Henley SJ, Burns D, Jemal A, Shanks TG, Calle EE. Lung cancer death rates in lifelong nonsmokers. Journal of the National Cancer Institute. 2006;98(10):691–699. doi: 10.1093/jnci/djj187. [DOI] [PubMed] [Google Scholar]
- 18.Nyberg F, Agudo A, Boffetta P, et al. A European validation study of smoking and environmental tobacco smoke exposure in nonsmoking lung cancer cases and controls. Cancer Causes Control. 1998;9:173. doi: 10.1023/a:1008882227444. [DOI] [PubMed] [Google Scholar]
- 19.Wu A. Carcinogenic effects. In: Shopland DR, Zeise L, Dunn A, editors. Health Effects of Exposure to Environmental Tobacco Smoke. National Cancer Institute; Bethesda, MD: 1999. [Google Scholar]
- 20.Taylor R, Najafi F, Dobson A. Meta-analysis of studies of passive smoking and lung cancer: effects of study type and continent. Int J Epidemiol. 2007;36:1048. doi: 10.1093/ije/dym158. [DOI] [PubMed] [Google Scholar]
- 21.Yu IT, Chiu YL, Au JS, Wong TW, Tang JL. Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmoking women. Cancer Research. 2006;66(9):4961–4967. doi: 10.1158/0008-5472.CAN-05-2932. [DOI] [PubMed] [Google Scholar]
- 22.Hammond EC, Selikoff IJ, Seidman H. ASBESTOS EXPOSURE, CIGARETTE SMOKING AND DEATH RATES*. Annals of the New York Academy of Sciences. 1979;330:473–790. doi: 10.1111/j.1749-6632.1979.tb18749.x. [DOI] [PubMed] [Google Scholar]
- 23.Sandler DP, Weinberg CR, Shore DL, et al. Indoor radon and lung cancer risk in Connecticut and utah. J Toxicol Environ Health A. 2006;69:633. doi: 10.1080/15287390500261117. [DOI] [PubMed] [Google Scholar]
- 24.Leuraud K, Schnelzer M, Tomasek L, et al. Radon, smoking and lung cancer risk: results of a joint analysis of three European case-control studies among uranium miners. Radiat Res. 2011;176:375. doi: 10.1667/rr2377.1. [DOI] [PubMed] [Google Scholar]
- 25.Darby S, Hill D, Auvinen A, et al. Radon in homes and risk of lung cancer: collaborative analysis of individual data from 13 European case-control studies. BMJ. 2005;330(7485):223. doi: 10.1136/bmj.38308.477650.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alberg AJ, Brock MV, Samet JM. Epidemiology of lung cancer: looking to the future. J Clin Oncol. 2005;23:3175. doi: 10.1200/JCO.2005.10.462. [DOI] [PubMed] [Google Scholar]
- 27.Brenner DR, Hung RJ, Tsao MS, et al. Lung cancer risk in never-smokers: a population based case-control study of epidemiologic risk factors. BMC Cancer. 2010;10:285. doi: 10.1186/1471-2407-10-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gorlova OY, Weng SF, Zhang Y, et al. Aggregation of cancer among relatives of never smoking lung cancer patients. Int J Cancer. 2007;121:111. doi: 10.1002/ijc.22615. [DOI] [PubMed] [Google Scholar]
- 29.Ohtsuka K, Ohnishi H, Kurai D, et al. Familial lung adenocarcinoma caused by the EGFR V843I germ-line mutation. J Clin Oncol. 2011;29:e191. doi: 10.1200/JCO.2010.31.4492. [DOI] [PubMed] [Google Scholar]
- 30.Kawaguchi T, Koh Y, Ando M, et al. Prospective Analysis of Oncogenic Driver Mutations and Environmental Factors: Japan Molecular Epidemiology for Lung Cancer Study. J Clin Oncol. 2016;34:2247. doi: 10.1200/JCO.2015.64.2322. [DOI] [PubMed] [Google Scholar]
- 31.Travis LB, Gospodarowicz M, Curtis RE, et al. Lung cancer following chemotherapy and radiotherapy for Hodgkin’s disease. J Natl Cancer Inst. 2002;94:182. doi: 10.1093/jnci/94.3.182. [DOI] [PubMed] [Google Scholar]
- 32.Littman AJ, Thornquist MD, White E, et al. Prior lung disease and risk of lung cancer in a large prospective study. Cancer Causes Control. 2004;15:819. doi: 10.1023/B:CACO.0000043432.71626.45. [DOI] [PubMed] [Google Scholar]
- 33.Wells C, Mannino DM. Pulmonary fibrosis and lung cancer in the United States: analysis of the multiple cause of death mortality data, 1979 through 1991. South Med J. 1996;89:505. doi: 10.1097/00007611-199605000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Ciotti M, Giuliani L, Ambrogi V, et al. Detection and expression of human papillomavirus oncogenes in non-small cell lung cancer. Oncol Rep. 2006;16:183. [PubMed] [Google Scholar]
- 35.Hasegawa Y, Ando M, Kubo A, et al. Human papilloma virus in non-small cell lung cancer in never smokers: a systematic review of the literature. Lung Cancer. 2014;83:8. doi: 10.1016/j.lungcan.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Mollerup S, Jørgensen K, Berge G, Haugen A. Expression of estrogen receptors alpha and beta in human lung tissue and cell lines. Lung Cancer. 2002;37:153. doi: 10.1016/s0169-5002(02)00039-9. [DOI] [PubMed] [Google Scholar]