Abstract
Background:
The purpose of the present study was to assess the impact of the coronavirus disease 2019 (COVID-19) pandemic on orthopaedic and trauma surgery departments in university hospitals in Germany in order to clarify current challenges.
Methods:
In this cross-sectional study, an online-based anonymous survey was conducted within the Convention of University Professors of Orthopaedic and Trauma Surgery in Germany from April 3 to April 11, 2020. A bipolar 5-point Likert scale (with possible responses of “totally disagree,” “rather disagree,” “neutral,” “rather agree,” and “totally agree”) was applied. Fifty-two (69.3%) of 75 clinic directors participated.
Results:
Communication and cooperation with the government, hospital administration, and other departments during the COVID-19 pandemic were mainly perceived as appropriate. However, only 7 respondents (13.7%) totally agreed or rather agreed with the statement that the authorities are supporters of orthopaedic and trauma surgery departments. Substantial financial and personnel changes in orthopaedic and trauma surgery departments of university hospitals were reported, resulting in an average reduction of 49.4% in operating room capacity and an expected 29.3% loss of revenue. In addition, 14.7% of physicians were reallocated from orthopaedic and trauma surgery to other care-delivery environments.
Conclusions:
Our study demonstrated that the COVID-19 pandemic has had a substantial impact on orthopaedic and trauma surgery departments in German university hospitals. Distinct structural and financial effects were noted. Nevertheless, the present study demonstrates the commitment of our specialty to overcome the pandemic by providing competent personnel as well as close cooperation with the hospital administration and other departments.
Clinical Relevance:
To our knowledge, this is the first Germany-wide survey among the heads of orthopaedic and trauma surgery departments in university hospitals on the impact of the COVID-19 pandemic. The survey results may help to inform system-wide decision-making in Germany, in Europe, and beyond.
In December 2019, an unknown respiratory disease caused by a novel coronavirus, referred to as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported in Hubei province of the People’s Republic of China1,2. This disease was named coronavirus disease 2019 (COVID-19) and leads to fever, coughing, and dyspnea in the context of viral pneumonia3,4. Because of the rapid increase in the numbers of patients infected and deaths caused by COVID-19, the World Health Organization (WHO) classified the situation as a Public Health Emergency of International Concern (PHEIC) in January 20205. Despite drastic measures of containment taken in China, the virus spread throughout the world and the WHO declared it as a pandemic on March 11, 20206,7.
In Germany, the first case was reported on January 27, 20208. In March 2020, because of the increasing number of SARS-CoV-2 infections and associated deaths without the availability of a vaccine or specific drug treatment, the German government decided on far-reaching nationwide containment and mitigation strategies for the entire population, including restrictions such as the closing of restaurants and stores as well as limitations of personal contact9. In order to maximize hospital capacity, personal protective equipment (PPE) for hospital personnel and ventilators for an increasing number of COVID-19 patients were ordered, all elective surgical procedures were postponed, and personnel were shifted to intensive-care units and emergency departments10.
By April 20, 2020, >145,000 people had tested positive for SARS-CoV-2 in Germany and >4,600 people had died of COVID-1911. In the course of these unprecedented medical and social challenges, German university hospitals, as flagships of medical care and research, have also been heavily involved in the fight against the SARS-CoV-2 pandemic. This situation has had an impact not just on the infectious-disease and intensive-care departments providing direct treatment, but on all specialties12. To decrease the economic burden on hospitals and contract physicians in Germany, a law providing additional financing was passed on March 25, 202010. However, persistent hardships include the lack of PPE, SARS-CoV-2 infections of employees, and far-reaching personnel and organizational restructuring in the hospitals. A timeline of key events related to the COVID-19 pandemic worldwide with special emphasis on Germany provides a distinctive overview (Fig. 1).
Fig. 1.
Timeline of key events related to the COVID-19 pandemic worldwide and in Germany.
In order to evaluate the current challenges of orthopaedic and trauma surgery departments in university hospitals given the complex interplay among a wide range of actors (government, health authorities, hospital administration, and other specialties) in an environment that is developing rapidly over time, we initiated a survey among the clinic directors at German university hospitals. The purpose of this survey was to obtain objective data with regard to personnel restructuring and financial changes as well as a baseline assessment for future developments. The aim of the present study was to identify current challenges in order to enable constructive solutions in this crisis of unprecedented dimensions in one of the countries most affected by SARS-CoV-2 worldwide.
Materials and Methods
Study Design and Participants
In this cross-sectional study, an online-based anonymous voluntary survey was conducted within the Convention of University Professors of Orthopaedics and Trauma Surgery in Germany from April 3 to April 11, 2020. This convention is composed of the heads of the orthopaedic and trauma surgery departments of the university hospitals and accordingly represents the leading German orthopaedic and trauma surgeons13. Currently, there are 89 members in the convention, with 14 members being heads of research institutions. Of the remaining 75 leading orthopaedic and trauma surgeons, 52 (69.3%) participated. In Germany, there are 37 university hospitals covering orthopaedic and trauma surgery (Fig. 2). The study protocol was reviewed and approved by the institutional ethics committee (EA1/075/20).
Fig. 2.
Map of the locations of university hospitals in Germany.
Survey
The online survey tool was developed with use of a commercial product (SurveyMonkey Europe UC; https://www.surveymonkey.com). The survey included 39 individual questions and statements in 7 categories (government, health authorities, hospital administration, departments of other specializations, restructuring and pandemic consequences, financial impact, and future prospects) using a combination of a 5-point Likert scale, closed (yes/no) questions, and open-ended questions (see Appendix). The questionnaire was developed in cooperation with the Institute of Psychometry and Health Outcome Research of our university clinic. After a literature review had been performed, the questions were developed by the first and senior authors (H.H., M.P., C.P.) in internal consensus meetings. The questionnaire was revised and approved by external coauthors and the Executive Board of the German Society of Orthopaedics and Trauma Surgery. We used a bipolar 5-point Likert scale; the possible responses were “totally disagree” (corresponding to 1 on the scale), “rather disagree” (corresponding to 2 on the scale), “neutral” (corresponding to 3 on the scale), “rather agree” (corresponding to 4 on the scale), and “totally agree” (corresponding to 5 on the scale).
In the first section (Government; 5 questions) and second section (Health Authorities; 4 questions), respondents were asked to rate the communication and actions taken by the government and authorities in the COVID-19 pandemic on the Likert scale described above. These questions were chosen because governments and authorities have made particularly far-reaching decisions during the pandemic, including those for orthopaedic and trauma surgery. In the third section (Hospital Administration; 8 questions), respondents were asked about cooperation in crisis management, the establishment of protective measures, and the redistribution of personnel. The fourth section (Other Departments; 2 questions) examined cooperation with the other specialist departments in the hospital. These categories were chosen because the restructuring of hospital routine caused by the pandemic has made cooperation with all participants in the hospital particularly important. The fifth section (Restructuring/Pandemic Consequences; 15 questions) and sixth section (Financial Impact; 2 questions) evaluated the impact of the COVID-19 pandemic on orthopaedic and trauma surgery departments. These categories were created because the cancellation of all elective surgical procedures and the reallocation of personnel to the direct care of COVID-19 patients could have a distinct structural influence on the departments. The last section (Future Prospects; 3 questions) allowed respondents to estimate whether the number of orthopaedic surgical procedures will decrease in the future and whether orthopaedic and trauma surgery will emerge weakened from the pandemic.
Statistical Analysis
Data analysis was performed with use of Prism 5 (GraphPad) and Excel 2019 (Microsoft). The means and standard deviations (SDs) of the bipolar 5-point Likert scales and the open questions were calculated.
Results
Government
Thirty-four (65.4%) of the leading orthopaedic and trauma surgeons in Germany totally or rather agreed with the statement that information provided by the government was adequate (mean score, 3.5 ± 1.1). Thirty-seven respondents (71.2%) totally or rather agreed with the general measures taken by the government (mean score, 3.7 ± 1.1) (Fig. 3). Twenty-four respondents (45.2%) totally or rather agreed with the statement that the postponement of elective surgical procedures was an adequate measure of the government, whereas 20 (38.5%) totally or rather disagreed (mean score, 3.1 ± 1.1). Thirty-six respondents (69.2%) totally or rather agreed that they would have preferred more commitments to financial support/protection (mean score, 4.0 ± 1.0).
Fig. 3.
Graphical overview of the responses on section A of the survey (government).
Health Authorities
Thirty-one respondents (60.8%) considered the information policy of the authorities to be totally or rather appropriate (mean score, 3.5 ± 1.1). Nineteen respondents (37.3%) totally or rather perceived the authorities as a competent partner (mean score, 3.2 ± 1.0). Seven respondents (13.7%) totally or rather perceived the authorities to be a supporter of their specialty, whereas 27 (52.9%) totally or rather disagreed (mean score, 2.5 ± 0.99) (Fig. 4). Fourteen respondents (27.5%) totally or rather agreed with the statement that the protective measures taken by the authorities for health care workers were adequate, whereas 28 (54.9%) totally or rather disagreed (mean score, 2.7 ± 1.1).
Fig. 4.
Graphical overview of the responses on section B of the survey (authorities).
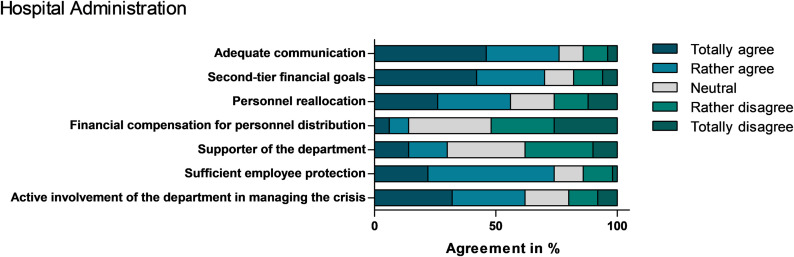
Hospital Administration
Thirty-eight respondents (76.0%) totally or rather perceived communication by the hospital administration to be adequate, whereas 7 (14.0%) totally or rather disagreed with this statement (mean score, 4.0 ± 1.2). Thirty-seven respondents (74.0%) stated that they were totally or rather satisfied with the protective arrangements by the hospital administration for employees (mean score, 3.8 ± 0.99). Thirty-five respondents (70.0%) totally or rather agreed with the statement that the hospital administration explicitly communicated that financial targets were second-tier in the current situation (mean score, 3.9 ± 1.3). Twenty-eight respondents (56.0%) totally or rather agreed that the hospital administration actively controlled the distribution of personnel affiliated with the orthopaedic and trauma surgery departments, including surgeons, nonoperative physicians, physician assistants, and nurses (mean score, 3.4 ± 1.3). Seven respondents (14.0%) totally or rather agreed with the statement that there was financial compensation for reallocation of personnel from the orthopaedic and trauma surgery departments, whereas 26 (52.0%) totally or rather disagreed with this statement (mean score, 2.4 ± 1.1) (Fig. 5).
Fig. 5.
Graphical overview of the responses on section C of the survey (hospital administration).
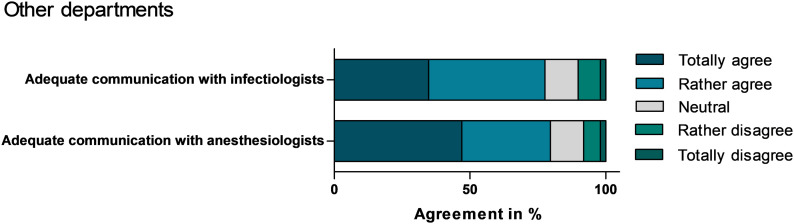
Communication with Other Departments
Thirty-nine respondents (79.6%) totally or rather agreed with the statement that there was appropriate communication with anesthesiology (mean score, 4.2 ± 1.0), whereas 38 respondents (77.6%) totally or rather agreed that there was adequate communication with the infectious-disease department (mean score, 4.0 ± 1.0) (Fig. 6).
Fig. 6.
Graphical overview of the responses on section D of the survey (other departments).
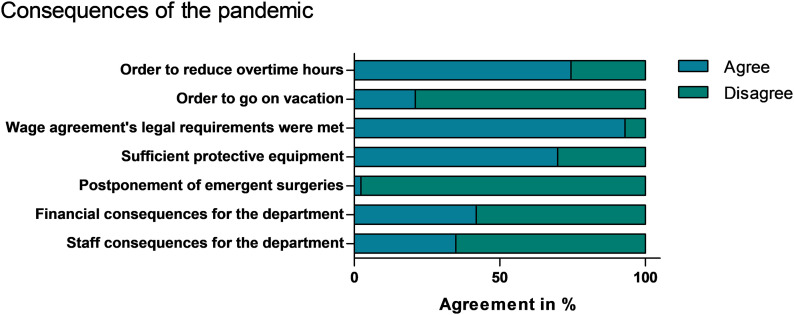
Restructuring and Other Pandemic Consequences
A mean reduction in patient bed capacity of 45.3% ± 20.1% of the orthopaedic and trauma surgery wards was reported. Furthermore, there was a reduction in operating room (OR) capacities by an average of 49.4% ± 20.4% and a reduction in outpatient departments by an average of 72.0% ± 21.1%. On average, 14.7% ± 17.2% of orthopaedic and trauma surgeons were reallocated to other specialties. Several of the departments have delegated personnel to intensive-care units (n = 19) or to specialized COVID-19 wards (n = 18). An average of 2.1% ± 5.8% of the doctors in the departments tested positive for SARS-CoV-2, and an average of 8.6% ± 10.4% of the physicians were in domestic quarantine. Thirty-two (74.4%) of the heads of the departments ordered reduction of accumulated overtime for their employees by means of free time, whereas 9 (20.9%) ordered leave for holidays (Fig. 7). Thirty respondents (69.8%) stated that enough PPE was provided in their hospitals. One university hospital (2.3%) reported on the postponement of emergency surgery.
Fig. 7.
Graphical overview of the responses on section E of the survey (consequences of the pandemic).
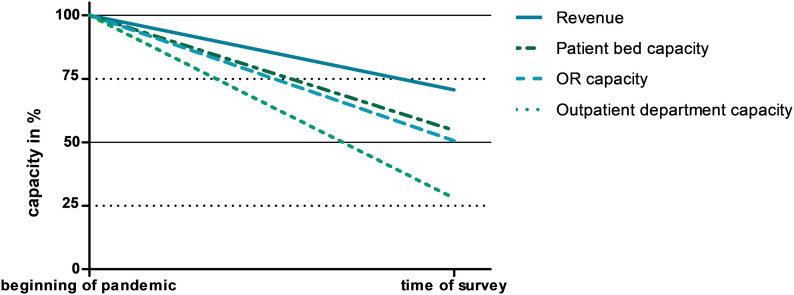
Financial Impact
The average loss of revenue for orthopaedic and trauma surgery departments has so far been estimated to be 29.3% ± 17.9% (Fig. 8). Eighteen clinic directors (41.9%) assumed that not achieving their financial target settings will have financial consequences for their department. Accordingly, 15 respondents (34.9%) reported that that failure to meet financial target settings would have personnel consequences for their department.
Fig. 8.
Line graph showing the impact of the COVID-19 pandemic on hospital performance indicators.
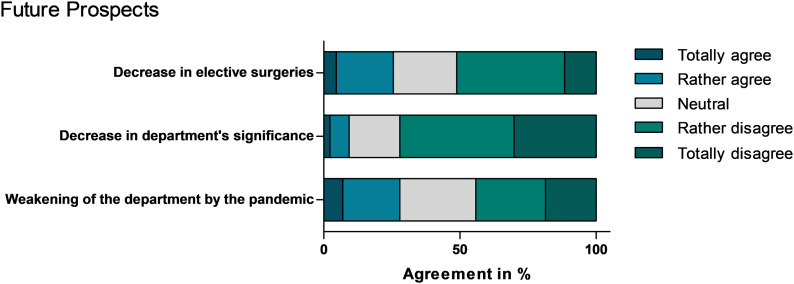
Future Prospects
Eleven respondents (25.6%) totally or rather agreed with the statement that the number of elective surgical procedures will decrease in the future, whereas 22 respondents (51.2%) totally or rather disagreed with that statement (mean score, 2.7 ± 1.1). Thirty-one respondents (72.1%) totally or rather disagreed with the statement that their department would lose its importance in the future (mean score, 2.1 ± 1.0). Twelve respondents (27.9%) totally or rather agreed with the statement that the orthopaedic and trauma surgery departments will be weakened by the COVID-19 pandemic, whereas 19 (44.2%) totally or rather disagreed with that statement (mean score, 2.7 ± 1.2) (Fig. 9).
Fig. 9.
Graphical overview of the responses on section F of the survey (future prospects).
Discussion
Because of the increasing number of SARS-CoV-2 infections and the associated severity of disease progression and deaths, the COVID-19 pandemic is a global challenge for our society and health systems. This challenge not only affects departments that are directly involved in the treatment of COVID-19 patients, but, because of nationwide restrictions and restructuring of the health-care system, it also affects other departments such as orthopaedic and trauma surgery. In order to provide an overview of the current situation in university hospitals in one of the most affected countries in Europe, we conducted this nationwide survey in Germany. In order to generate the most reliable data regarding university clinics, the Convention of University Professors of Orthopaedic and Trauma Surgery was consulted. In total, 37 university hospitals cover orthopaedic and trauma surgery in Germany. Some institutions delegate multiple university professors to the convention. The participation of 52 members of the convention can be considered representative.
The majority of the leading orthopaedic and trauma surgeons in Germany perceived the communication and measures taken by the government as appropriate. This finding is remarkable because political actions have massive financial and structural impact on the departments. On March 12, 2020, the German government asked all clinics to cancel elective surgery, resulting in an estimated average reduction of 49.4% in OR capacity and 29.3% in revenue. Of the 20 most frequently performed operations in Germany, half are trauma surgery and orthopaedic procedures, and, of those, >50% are elective operations such as total joint arthroplasty; the situation is comparable to that in the United States14,15. This cancellation of elective procedures will lead to significant financial losses in almost all orthopaedic and trauma surgery departments. Overall, the departments of orthopaedic and trauma surgery seemed to be adhering to the limitations, regardless of the possibility of dire consequences16. Politicians and hospital managers have conveyed the impression that financial considerations are irrelevant in the fight against the pandemic. This is remarkable in a health-care system that has been focused on cost efficiency for years17.
An estimated 14.7% of physicians were reallocated from orthopaedic and trauma surgery departments to other areas of clinical service, demonstrating the versatility and commitment of the departments to provide support where required. The difference between the distinct reduction in the volume of surgical procedures and the personnel redistribution can be explained by the facts that university hospitals perform other tasks such as teaching and research in addition to patient care and that some personnel capacities were occupied by the restructuring measures. The cooperation with the hospital administration in these times of crisis was assessed positively overall. Interdisciplinary communication also was largely considered to be appropriate, demonstrating the strong cohesion within the university hospitals in facing challenging conditions and reflecting the commitment of the orthopaedic and trauma surgery departments to a common goal.
In contrast, the work of the health authorities was perceived as lacking in terms of protection for health-care workers and support for the departments. This finding may be an indication of the structural deficiencies of the authorities in pandemic control and should be considered and improved for future preparations. Given the fact that the current situation is highly dynamic and circumstances regarding health regulations must be adapted constantly, the lower agreement rate was expected. Another major issue in German hospitals in the beginning of the pandemic was the lack of PPE for health-care workers, such as face masks. There was concern that increased SARS-CoV-2 infections of employees could push the health-care system to its limits and lead to COVID-19-associated deaths of health-care workers, similar to the situations in Italy and Spain, where thousands of health-care workers have become infected and several have died from COVID-1918. In our survey, the majority of the hospitals were able to provide sufficient PPE, but, nevertheless, on average, 2.1% ± 5.8% of the physicians at the university hospital departments for orthopaedic and trauma surgery became infected with SARS-CoV-2.
The orthopaedic and trauma surgery departments have been seriously affected by the COVID-19 pandemic. Because of the massive reduction in operational capacities and the reallocation of personnel, only emergency operations were carried out at most facilities.
The university orthopaedic and trauma surgery departments have stringently implemented the government-mandated measures and have used a considerable portion of their staff and financial resources to fight the COVID-19 pandemic. With regard to the future, most department heads are not expecting a permanent decline in elective operations. The majority of those consulted did not assume that the pandemic will lead to decreased importance of orthopaedic and trauma surgery in general.
The present study had limitations, and the results should be interpreted accordingly. Only German university hospitals were surveyed; therefore, applicability of the results to German hospitals in general and to orthopaedic and trauma surgery departments in other countries is limited. Despite a high response rate, distortion due to nonresponse bias must be taken into account. Because of the rapid development of the pandemic, prior pilot testing was not performed and the lack of psychometric assessment should be considered. As we conducted a nationwide survey, the regional differences of the spread of COVID-19 may lead to distortions in the assessment of the pandemic because areas have been affected to varying degrees. Given that the COVID-19 pandemic is still in its early stages in Germany and is expected to progress further, the present survey provides a first impression of the impact that this pandemic has had on orthopaedic and trauma surgery departments in German university hospitals. The financial losses are only estimated, and the final impact can only be determined when the pandemic ends. In order to assess more accurately the overall effects of the pandemic, there will be follow-up surveys during and beyond the crisis.
Nevertheless, we should continue the stern implementation of measures and constructive cooperation and engagement to help contain the COVID-19 pandemic.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F923).
Supplementary Material
Acknowledgments
Note: The authors thank the Convention of University Professors of Orthopaedic and Trauma Surgery for time and careful participation. We would also like to sincerely thank Professor Günther for his wise and constructive suggestions for improvement. We warmly thank the Institute for Social Medicine, Epidemiology and Health Economics for the consultation.
Footnotes
Matthias Pumberger, MD, and Carsten Perka, MD, contributed equally to this work.
Investigation performed at Charité University Medicine Berlin, Berlin, Germany
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F922).
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020. February 20;382(8):727-1-8 Epub 2020 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020. February 22;395(10224):565-1-8 Epub 2020 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ. A new coronavirus associated with human respiratory disease in China. Nature. 2020. March;579(7798):265-1-8 Epub 2020 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020. March;579(7798):270-1-8 Epub 2020 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. January 23 Accessed 2020 Apr 17 https://www.who.int/news-room/detail/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [Google Scholar]
- 6.Tian H, Liu Y, Li Y, Wu CH, Chen B, Kraemer MUG, Li B, Cai J, Xu B, Yang Q, Wang B, Yang P, Cui Y, Song Y, Zheng P, Wang Q, Bjornstad ON, Yang R, Grenfell BT, Pybus OG, Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020. March 31 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020. March 19;91(1):157-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Der Spiegel. [First SARS-CoV-2 infection in Germany is confirmed.] 2020. January 28 Accessed 2020 Apr 17. German https://www.spiegel.de/wissenschaft/medizin/corona-virus-erster-fall-in-deutschland-bestaetigt-a-19843b8d-8694-451f-baf7-0189d3356f99 [Google Scholar]
- 9.Bundesregierung Die. [German government imposes nationwide exit restrictions.] 2020. Mar 18, https://www.bundesregierung.de/breg-de/themen/coronavirus/ansprache-der-kanzlerin-1732108 Accessed 2020 Apr 17. German. [Google Scholar]
- 10.Bundesministerium für Gesundheit. [Coronavirus SARS-CoV-2: chronicle of previous measures.] 2020. Accessed 2020 Apr 17. German https://www.bundesgesundheitsministerium.de/coronavirus/chronik-coronavirus.html [Google Scholar]
- 11.John Hopkins University Center for Systems Science and Engineering. COVID-19 dashboard. Accessed 2020 Apr 17 https://coronavirus.jhu.edu/map.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang Liang Z, Wang W, Murphy D, Po Hui JH. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. 2020. March 20 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Konvent der Universitätsprofessoren für Orthopädie und Unfallchirurgie (KUOU). https://www.kuou.de/kuou/ [About us.] Accessed 17 Apr 2020. German. [Google Scholar]
- 14.Statistisches Bundesamt. (Destatis). [The 20 most frequent surgeries in 2018 in Germany.] Accessed 17 Apr 2020. German https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/Tabellen/drg-operationen-insgesamt.html [Google Scholar]
- 15.Anoushiravani A, O’Connor C, DiCaprio M, Iorio R. Economic impacts of the COVID-19 crisis: an orthopaedic perspective. J Bone Joint Surg Am. 2020. April 21 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Surgeons. COVID-19: recommendations for management of elective surgical procedures 2020 Mar 13. Accessed 2020 Apr 17 https://www.facs.org/covid-19/clinical-guidance/elective-surgery [Google Scholar]
- 17.Wirtz DC, Stöckle U. Künftige versorgungsstrukturen in Deutschland: gibt es lehren aus der corona-pandemie? Z Orthop Unfall. 2020. April;158(2):163-1-8 Epub 2020 Apr 8. [DOI] [PubMed] [Google Scholar]
- 18.The Guardian 'As if a storm hit': more than 40 Italian health workers have died since crisis began. 2020. March 26 Accessed 2020 Apr 17 https://www.theguardian.com/world/2020/mar/26/as-if-a-storm-hit-33-italian-health-workers-have-died-since-crisis-began [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.