Abstract
Background
Knee fractures may lead to post-traumatic knee osteoarthritis and subsequent TKA in some patients. However, absolute risk estimates and risk factors for TKA in patients with knee fractures compared with those of the general population remain largely unknown. Such knowledge would help establish the treatment burden and direct patient counseling after a knee fracture is sustained.
Questions/purposes
(1) What is the short-term risk of TKA after knee fracture? (2) What is the long-term risk of TKA after knee fracture? (3) What are the risk factors for TKA in patients with knee fractures?
Methods
A nationwide 20-year, matched-case comparison cohort study of prospectively collected data from the Danish National Patient Registry included all patients at least 15 years old with International Classification of Diseases, 10th revision codes DS724, DS820, or DS821 (knee fractures) on the date their knee fracture was registered. Each patient with a knee fracture was matched (by sex and age) to five people without knee fractures from the general Danish population on the date the knee fracture patient’s knee fracture was registered (population controls). Patients with knee fractures and people in the population control group were followed from the date the knee fracture patient’s knee fracture was registered to the date of TKA, amputation, knee fusion, emigration, death, or end of follow-up in April 2018. TKA risks for patients with knee fractures versus those for population controls and TKA risk factors in patients with knee fractures were estimated using hazard ratios (HRs) with 95% CIs. A total of 48,791 patients with knee fractures (median age 58 years [interquartile range 41-73]; 58% were female) were matched to 263,593 people in the population control group.
Results
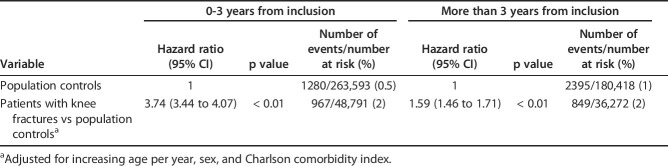
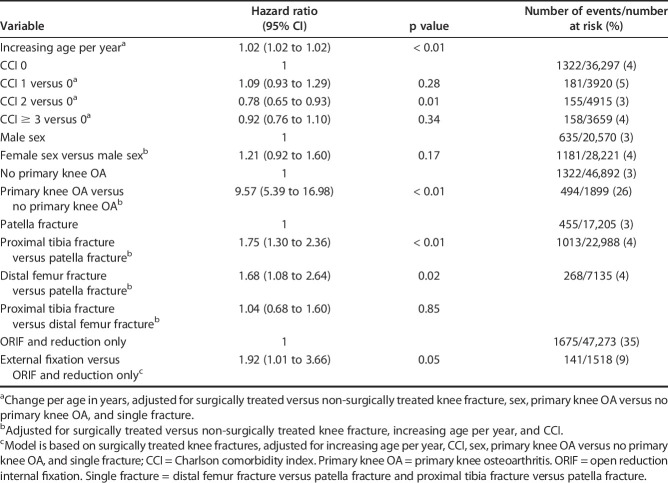
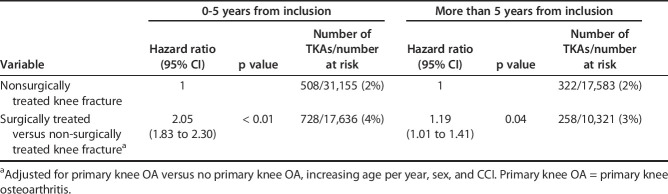
The HR for TKA in patients with knee fractures compared with population controls was 3.74 (95% CI 3.44 to 4.07; p < 0.01) in the first 3 years after knee fracture. Among knee fracture patients, the risk of undergoing TKA was 2% (967 of 48,791) compared with 0.5% (1280 of 263,593) of people in the population control group. After the first 3 years, the HR was 1.59 (95% CI 1.46 to 1.71) and the number of patients with knee fractures with TKA events divided by the number at risk was 2% (849 of 36,272), compared with 1% (2395 of 180,418) of population controls. During the 20-year study period, 4% of patients with knee fractures underwent TKA compared with 1% of population controls. Risk factors for TKA in patients with knee fractures were: primary knee osteoarthritis (OA) versus no primary knee OA (HR 9.57 [95% CI 5.39 to 16.98]), surgical treatment with external fixation versus open reduction and internal fixation and reduction only (HR 1.92 [95 % CI 1.01 to 3.66]), proximal tibia fracture versus patellar fracture (HR 1.75 [95 % CI 1.30 to 2.36]), and distal femur fracture versus patellar fracture (HR 1.68 [95 % CI 1.08 to 2.64]). Surgical treatment of knee fractures was also a risk factor for TKA. The HRs for TKA in patients with knee fractures who were surgically treated versus those who were treated non-surgically were 2.05 (95% CI 1.83 to 2.30) in the first 5 years after knee fracture and 1.19 (95% CI 1.01 to 1.41) after 5 years.
Conclusions
Patients with knee fractures have a 3.7 times greater risk of TKA in the first 3 years after knee fracture, and the risk remains 1.6 times greater after 3 years and throughout their lifetimes. Primary knee OA, surgical treatment of knee fractures, external fixation, proximal tibia fractures, and distal femur fractures are TKA risk factors. These risk estimates and risk factors highlight the treatment burden of knee fractures, building a foundation for future studies to further counsel patients on their risk of undergoing TKA based on patient-, fracture-, and treatment-specific factors.
Level of Evidence
Level III, prognostic study.
Introduction
Knee injuries play a part in the rising rates of TKA procedures, which cannot be explained by increases in population size, longevity, and obesity rates alone [14]. Fractures of the distal femur, proximal tibia, and patella represent a substantial proportion of these injuries (incidence rate in the United States: 9 per 100,000 per year) [10], and often result in lower functional outcomes [1, 3, 13, 27], lower work performance [23, 27], lower health-related quality of life [13, 23, 27], and post-traumatic knee osteoarthritis (OA) [7, 13, 16, 17, 20, 24, 26] with subsequent TKA in some patients [7, 17, 24, 26]. To date, secondary TKA for post-traumatic OA after knee fracture has had less successful results compared with primary TKA for primary knee OA in terms of functional outcomes [15, 26], complication rates [8, 26], reoperations [8, 20], and survival rates [15].
Actual risk estimates of [12, 29] and risk factors for [29] TKA in patients with knee fractures compared with those of the general population remain largely unknown. Such knowledge would help establish the treatment burden and direct patient counseling after a patient sustains a knee fracture.
Therefore, in this study, we asked: (1) What is the short-term risk of TKA after knee fracture? (2) What is the long-term risk of TKA after knee fracture? (3) What are the risk factors for TKA in patients with knee fractures?
Patients and Methods
Study Design and Setting
The study was designed as a nationwide, matched-case comparison cohort study of prospectively collected data from the following population-based data sources: the Danish Civil Registration System [21] and the Danish National Patient Registry [22], which covers the entire population of Denmark of approximately 5.7 million residents [25]. The study was approved by the Danish Data Protection Agency, record number REG-085-2017. No institutional review board approval was needed because the study is a registry study of prospectively collected data. The study was conducted according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines [28].
Participants
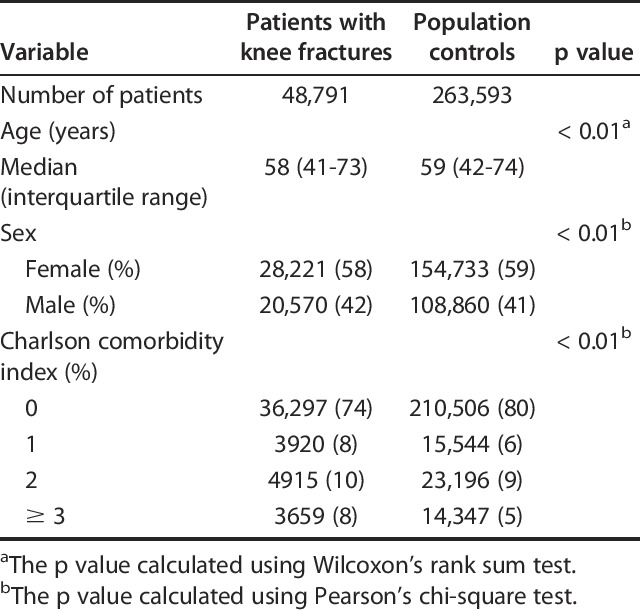
We used the World Health Organization’s 10th revision of International Classification of Diseases (ICD-10) [31] to identify the study population in the Danish National Patient Registry. The study population consisted of all patients at least 15 years old registered in the Danish National Patient Registry from January 1, 1998 to April 30, 2018, with hospital encounters with ICD-10 codes DS724, DS820, or DS821 (knee fractures), with or without subsequent knee surgery codes (see Supplemental Digital Content 1, http://links.lww.com/CORR/A286). Only 3% of knee fracture patients were registered with multiple knee fractures, making the comparison with patients with only one knee fracture and the interpretation of different multiple fractures imprecise; consequently, they were removed from the analysis. Each patient with a knee fracture was matched according to sex and age (same birth year) with five people from the general Danish population without a knee fracture on the date the knee fracture patient’s injury was registered (population controls). Patients with knee fractures and participants in the population control group were followed from the date the patient’s knee fracture was registered to the date of TKA, amputation, knee fusion, emigration, death, or end of follow-up on April 30, 2018. A total of 48,791 patients with knee fractures (median age 58 years [interquartile range 41-73]; 58% were female) were matched to 263,593 population controls (median age 59 [42-74]; 59% were female) (Table 1). For participants in both groups, the mean observation period to TKA was 7 years.
Table 1.
Demographic data of patients with knee fractures and population controls
Description of Experiment, Treatment, or Surgery
Because a unique Danish Civil Personal Register number is assigned to individuals at birth or at immigration, an unambiguous individual-level link between clinical and administrative databases is possible [21]. The Danish Civil Registration System contains complete information on date of birth, sex, residency, and immigration and is updated daily with an individual’s vital status. Every person legally residing in Denmark is registered in the database. The Danish National Patient Registry contains information on all public hospital admissions and emergency department visits. Reporting to the Danish National Patient Registry is mandatory and is used for reimbursement by public and private hospitals [22]. However, private hospitals do not treat patients with knee fractures, and private-paid TKA is rare. The Danish National Patient Registry contains information on date of admission, Civil Personal Register number, age, sex, ICD-10 classification [31], and the Danish version of the Nordic Medico-Statistical Committee Classification of Surgical Procedures (NOMESCO classification) [18].
Variables, Outcome Measures, Data Sources, and Bias
The current NOMESCO classification [18] was implemented in 1996; therefore, we excluded all years before 1996 to reduce surgery code bias. We also excluded years 1996 and 1997 to exclude a potential backlog of already prevalent knee fractures in patients with hospital follow-up. We used the updated version of the Charlson comorbidity index [2, 19] to evaluate comorbidities in patients with knee fractures and population controls. The Charlson comorbidity index could not be calculated in 19% of population controls because they lacked hospital admissions or were not registered with diagnoses used to calculate the Charlson comorbidity index. For these patients, the value was thus set at 0. Primary knee OA was defined as pre-existing knee OA registered at the time of knee fracture (see Supplemental Digital Content 1, http://links.lww.com/CORR/A286). Surgical treatment was divided into external fixation, open reduction internal fixation (ORIF), and reduction. External fixation, ORIF, and reduction procedures were defined by the index procedure, and because we did not have access to medical records, the true proportion of conversions from external fixation to ORIF was unknown. Consequently, to avoid inaccurate assumptions, patients registered with external fixation were allocated to the external fixation group.
Statistical Analysis, Study Size
Descriptive measures are presented as the median and interquartile range or as frequencies and percentages. Based on QQ-plots, the data did not follow a normal distribution, thus we calculated the p value for age in patients with knee fractures and population controls using the Wilcoxon’s rank sum test. We calculated the p value for sex and Charlson comorbidity index in patients with knee fractures and population controls using Pearson’s chi-square test. To answer the first and second research questions, we analyzed the short-term and long-term risk of TKA for patients with knee fractures versus that of population controls with Cox proportional hazard models. Amputation, knee fusion, emigration, and death were considered competing events for TKA, and risk times were therefore censored at these events. Based on an evaluation of the Schoenfeld residuals, the proportional hazard assumption was not satisfied for comparing patients with knee fractures to population controls for the 20-year follow-up; when considering the relationship between knee fracture patients and population controls, the hazard ratio (HR), did not appear to be constant across all 20 years. Because the Cox proportional hazards model assumes this constant HR, this model did not fit our data. The model was therefore split into two separate models, the first fitted to the first 3 years of follow-up, with all non-event observations censured at 3 years; and the second model following observations from 3 years onward. Patients with knee fractures and patients in the population control group were only included in the second model if they did not have any event within the first 3 years, and if they had a follow-up interval of 3 years or longer. Evaluation of the Schoenfeld residuals suggested the proportional hazard could be assumed in these models, that is, a constant HR could be assumed within each model. Estimates from the models are presented as HRs with 95% CIs and p values. Adjusted HRs for patients with knee fractures versus patients in the population control are presented and interpreted for both models. To answer the third research question, when evaluating risk factors for TKA in patients with knee fractures, we could assume proportionality for the entire follow-up period; therefore, risk factors were estimated from a model for the entire 20-year study period. To further answer the third research question, we analyzed the risk factor of TKA in individuals with surgically treated knee fractures versus non-surgically treated fractures with a similar Cox proportional hazards model. A similar issue with the proportionality assumption was present in the model comparing patients with knee fractures to population controls; thus, we used two separate models: the first in the first 5 years after knee fracture and the second from 5 years onward. All analyses were performed in in the statistical software R 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria). A p value < 0.05 was considered statistically significant.
Results
What Is the Short-term Risk of TKA After Knee Fracture?
Patients who sustained knee fractures were 3.7 times more likely to undergo TKA within 3 years than patients in the comparable control group (Fig. 1). After adjusting for increasing age per year, sex, and Charlson comorbidity index, the HR for TKA in individuals with knee fractures versus patients in the population control group was 3.74 (95% CI 3.44 to 4.07; p < 0.01) in the first 3 years after knee fracture (Table 2). Within the first 3 years after knee fracture, 2% of patients (967 of 48,791) with knee fractures underwent TKA compared with 0.5% of patients (1280 of 263,593) in the control population.
Fig. 1.
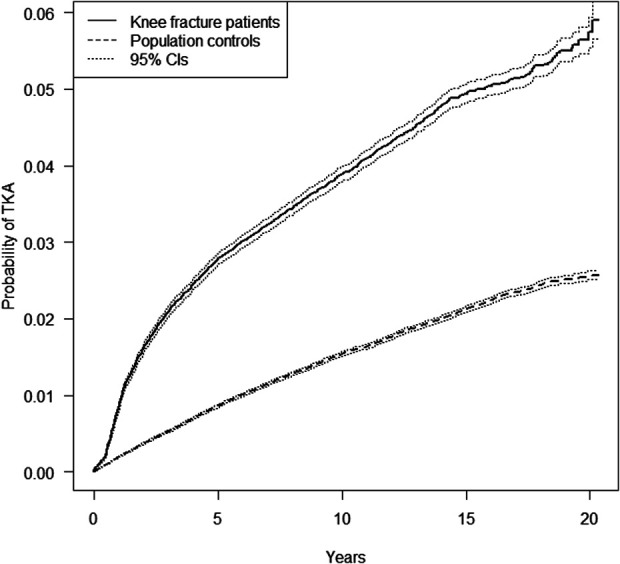
This graph shows the cumulative incidence of TKA probability in patients with knee fractures and patients in the population control group during the 20-year study period with 95% CIs.
Table 2.
Cox proportional hazards model with short-term and long-term hazard ratios for TKA in patients with knee fractures versus population controls
What Is the Long-term Risk of TKA After Knee Fracture?
Patients with knee fractures were 1.6 times more likely to undergo TKA at 3 years or more after their injury than the comparable patients in the control population (Fig. 1). After adjusting for increasing age per year, sex, and Charlson comorbidity index, the HR for TKA in individuals with knee fractures versus population controls was 1.59 (95% CI 1.46 to 1.71; p < 0.01) after the first 3 years after knee fracture (Table 2). After the first 3 years after knee fracture, 2% (849 of 36,272) of patients with knee fractures underwent TKA compared with 1% of patients (2395 of 180,418) in the control population (Table 2). During the 20-year period, 4% (1816 of 48,791) of patients with knee fractures underwent TKA compared with 1% (3675 of 263,593) among patients in the population control group.
What Are the Risk Factors of TKA in Patients with Knee Fractures?
When examining independent risk factors, we found that primary knee OA, surgical treatment of knee fracture, external fixation, proximal tibia fracture, and distal femur fracture were all risk factors for treatment with TKA in patients with knee fractures during the 20-year period (Table 3). After adjusting for surgically treated versus non-surgically treated knee fractures, increasing age per year, and Charlson comorbidity index, the HR for TKA in individuals with primary knee OA and knee fracture versus patients with no primary knee OA and knee fracture was 9.57 (95% CI 5.39 to 16.98; p < 0.01) during the 20-year period (Table 3). During the 20-year period, 26% (494 of 1899) of patients with knee fractures and primary knee OA underwent TKA compared with 3% (1322 of 46,892) of patients with knee fractures and no primary knee OA (Table 3). After adjusting for surgically treated versus non-surgically treated knee fractures, increasing age per year, and Charlson comorbidity index, the HR for TKA in individuals with proximal tibia fractures versus patella fractures was 1.75 (95% CI 1.30 to 2.36; p < 0.01) during the 20-year period (Table 3). During the 20-year period, 4% (1013 of 22,988) of patients with proximal tibia fractures underwent TKA compared with 3% (455 of 17,205) of patients with patella fractures (Table 3). After adjusting for surgically treated versus non-surgically treated knee fractures, increasing age per year, and Charlson comorbidity index, the HR for TKA in individuals with distal femur fracture versus patella fracture was 1.68 (95% CI 1.08 to 2.64; p = 0.02) during the 20-year period (Table 3). During the 20-year period, 4% (268 of 7135) of patients with distal femur fracture underwent TKA (Table 3). The HR of TKA and female versus male sex was 1.21 (95% CI 0.92 to 1.60; p = 0.17) during the 20-year period (Table 3). During the 20-year period, 4% (1181 of 28,221) of female patients with knee fractures underwent TKA, and 3% (635 of 20,570) of male patients with knee fractures underwent TKA (Table 3). The HR of TKA with increasing age per year in patients with knee fractures was 1.02 (95% CI 1.02 to 1.02; p < 0.01) during the 20-year period (Table 3). After adjusting for increasing age per year, Charlson comorbidity index, sex, primary knee OA versus no primary knee OA, and single fracture (distal femur fracture versus patella fracture and proximal tibia fracture versus patella fracture), the HR of TKA and surgical treatment with external fixation versus ORIF and reduction only was 1.92 (95% CI 1.01 to 3.66; p = 0.05) during the 20-year period (Table 3). During the 20-year period, 9% (141 of 1518) of patients with knee fractures were treated with external fixation compared with 35% (1675 of 47,273) of patients with knee fractures treated with ORIF and reduction only. After adjusting for primary knee OA versus no primary knee OA, increasing age per year, sex, and Charlson comorbidity index, the HR of TKA in patients with knee fractures treated surgically versus that of patients treated non-surgically was also a risk factor in the first 5 years (HR 2.05 [95% CI 1.83 to 2.30]; p < 0.01) as well as after 5 years (HR 1.19 [95% CI 1.01 to 1.41]; p = 0.04) (Table 4). In the first 5 years after knee fracture, 4% (728 of 17,636) of patients with surgically treated knee fracture underwent TKA compared with 2% (508 of 31,155) of patients with knee fractures who were treated non-surgically (Table 4). After the first 5 years after knee fracture, 3% (258 of 10,321) of patients with knee fracture treated surgically underwent TKA while 2% (322 of 17,583) of patients with knee fractures treated non-surgically underwent TKA (Table 4).
Table 3.
Cox proportional hazards model with hazard ratios for risk factors for TKA in patients with knee fractures during the 20-year study period
Table 4.
Cox proportional hazards model with hazard ratios for TKA in surgically treated versus non-surgically treated knee fractures
Discussion
Background and Rationale
Knee injuries play a part in the rising rates of TKA procedures, which cannot be explained by increases in population size, longevity, and obesity rates alone [14]. Fractures of the distal femur, proximal tibia, and patella represent a substantial proportion of these injuries [10], often resulting in lower functional outcome [1, 3, 13, 27], lower work performance [23, 27], lower health-related quality of life [13, 23, 27], and post-traumatic knee osteoarthritis [7, 13, 16, 17, 20, 24, 26] with subsequent TKA in some patients [7, 17, 24, 26]. To date, secondary TKA for post-traumatic OA after knee fracture has been shown to have less successful results compared with primary TKA for primary knee OA in terms of functional outcome [15, 26], complication rates [8, 26], reoperations [8, 20], and survival rates [15]. Actual risk estimates of [12, 29] and risk factors for [29] TKA in patients with knee fractures compared with those of the general population remain largely unknown. Such knowledge would help establish the treatment burden and direct patient counseling after a patient sustains a knee fracture. We found that patients with knee fractures have a 3.7 times greater risk of TKA in the first 3 years after knee fracture, and the risk remains 1.6 times greater after 3 years and throughout their lifetimes. We found several independent risk factors that increased the chances of undergoing TKA over and above the risks posed by a history of knee fracture, including primary knee OA, surgical treatment of knee fractures, external fixation, proximal tibia fracture, and distal femur fracture.
This study has a number of limitations: First, there are the well-known limitations of administrative data, with potential incorrect use of diagnosis codes and incomplete registration of surgery codes. Second, there are no specific surgery codes for conversion of surgery to treat knee fractures to TKA, and because the study is a registry study, we did not have access to medical records. However, data in the Danish National Patient Registry are high quality, and the highest positive predictive value is found in orthopaedic diagnoses [22]. Third, laterality of knee fracture, TKA, amputation, and knee fusion were insufficiently registered in the Danish National Patient Registry and thus could not be used, possibly producing overestimations or underestimations of procedure rates as procedures could have been performed on the contralateral knee. Fourth, data on fracture severity, that is, ABC extensions of ICD-10 codes, and injury severity, such as trauma type, were incompletely registered; only a small percentage of the study population was registered with ABC extensions and trauma type, thus distributions of knee fracture subclassifications and trauma type could not be described [22]. Consequently, it was not possible to, for instance, differentiate between a high-energy comminuted proximal tibia fractures with intra-articular involvement and a low-energy simple fractures of the patella, possibly confounding the risk estimates presented. However, we still believe that this study provides insight into what a knee fracture entails in forms of both short-term and long-term TKA risk. It also provides insight into which general anatomic region of the knee is most vulnerable to undergoing TKA when fractured, including risk estimates of how much primary knee OA, surgical treatment versus non-surgical treatment of knee fracture, and external fixation are associated with TKA risk. Fifth, although a 20-year follow-up for the older proportion of patients in the study population would likely be sufficient, it may not be enough for the younger proportion of patients. Because our population consists of both age groups, we believe we have captured a high proportion of TKA events for the older population but may have captured a smaller proportion of TKA events for the younger population. However, given that we found a higher HR within the first 3 years after knee fracture and a lower HR in the remaining follow-up time, we assume it is unlikely that a HR beyond 20 years would drastically deviate from the long-term HR presented in our study, even for younger patients. In summary, the accumulated data comprised a large, representative nationwide sample during a 20-year study period from a relatively homogenous population, increasing external validity and thus providing results with high validity and generalizability with regards to Scandinavian countries. Of note is that international generalizability of the study results can only be assumed because the potential confounder of TKA accessibility in different healthcare systems could not be accounted for in our data analysis.
What Is the Short-term Risk of TKA After Knee Fracture?
We found that within the first 3 years after injury, patients with a knee fracture underwent TKA with much greater frequency than the control population. Larsen et al. [12] found an HR for TKA of 3.02 (95% CI 2.26 to 4.03) from 0 to 5 years after patella fracture compared with that of a matched cohort. This is comparable to the HR of 3.74 (95 % CI 3.44 to 4.07) in the first 3 years following knee fracture in our study. The results of Larsen et al. [12] can only be roughly compared with ours because they included only patellar fractures in patients from a single region in Denmark; however, their study described similar risk trends as our study, in which the critical TKA risk can be seen in the first few years after knee fracture.
What Is the Long-term Risk of TKA After Knee Fracture?
We found that the increased risk of subsequently undergoing TKA remained even after 3 years and in the long term, with a substantially higher proportion of patients with a history of knee fracture undergoing TKA surgery than patients in the matched control group, suggesting that the risk of secondary TKA for posttraumatic OA, pain, reduced function, and other complications after knee fracture is lifelong. Larsen et al. [12], found an HR for TKA of 1.56 [95% CI 1.17 to 2.07] at 5 to 10 years after patella fracture compared with that of a matched cohort. Because of differences in study design as discussed above, this can to some extent be compared with our results (HR 1.59 [95 % CI 1.46 to 1.71] after the first 3 years after knee fracture). Wasserstein et al. [29] compared the HR for TKA in patients with ORIF-treated tibial plateau fractures with that of a matched cohort without ORIF-treated tibial plateau fractures. During the 14-year study period, the comorbidity-adjusted HR for TKA in ORIF-treated tibial plateau fractures was 5.29 (95% CI 4.58 to 6.11), whereas in our study, the increasing age per year-, sex-, and Charlson comorbidity index-adjusted HR for TKA in patients with knee fractures versus that of population controls was 1.59 (95% CI 1.46 to 1.71) after the first 3 years and in the long-term. A total of 7% of patients with ORIF-treated tibial plateau fractures and 2% of patients in the matched cohort underwent TKA after 10 years in the study by Wasserstein et al. [29]. During the 20-year period in our study, 4% of patients with knee fractures and 1% of matched population controls underwent TKA, while 4% of patients with proximal tibia fracture underwent TKA. The variance in results might be explained by differences in knee fracture types, treatment types, comorbidity measures (use of aggregated diagnosis groups versus Charlson comorbidity index), data sources, inclusion and exclusion criteria, group matching criteria, coding systems, populations and length of the study period.
What Are the Risk Factors of TKA in Patients with Knee Fractures?
We found several independent risk factors that increased the chances of undergoing TKA over and above the risks posed by a history of knee fracture. Wasserstein et al. [29] found an HR of 1.25 (p = 0.029) for female sex versus male sex in patients with ORIF-treated tibial plateau fractures during their 14-year study period compared with a female sex versus male sex and knee fracture HR of 1.21 (p = 0.17) during our 20-year study of patients with knee fractures (Table 3). In their study, increasing age per year had an HR of 1.03 (p < 0.01) [29], which is comparable to the results of our study (HR 1.02; p < 0.01) (Table 3). Our results showed an association between external fixation versus ORIF and reduction only, with an HR for TKA of 1.92 (p = 0.05), and Wasserstein et al. [29] calculated an HR of 1.56 (p < 0.20) in preoperative external fixation in patients with ORIF-treated tibial plateau fractures. The studies are only partly comparable as Wasserstein et al. [29] studied conversion surgery in tibial plateau fractures whereas we studied external fixation, ORIF, and reduction index procedures. In other studies, TKA was found to be more prevalent in females and those with increasing age [9], and knee fractures were more prevalent in females and in those with increasing age [4, 5, 6, 11, 30]. Our HRs of 1.21 and 1.02 in patients with knee fractures mimic these findings, although the HR for female sex versus male sex was no different in our study (p = 0.17) and the increased HR for increasing age per year was only 1.02 in our study. TKA for primary knee OA is a well-established procedure; hence, the high HR in patients with knee fractures and primary knee OA is unsurprising. However, the HR of 9.57 provides insight into the level of hazard involved. The high HRs for TKA in patients with knee fractures that were surgically treated versus those that were non-surgically treated (2.05 in the first 5 years and 1.19 after 5 years) in our study indicate that because most surgically treated knee fractures are more complex than non-surgically treated knee fractures, the higher HR for TKA in patients with surgically treated knee fractures is to be expected. The high HRs for TKA in patients with knee fractures with the above-mentioned risk factors illustrate the importance of focusing research on further defining patient-, fracture-, and treatment-specific risk factors during the initial and long-term treatment of knee fractures. Focus should be placed on proximal tibia fractures because our 20-year study showed that proximal tibia fracture had the highest HR for TKA (1.75).
We found that patients with knee fractures have a 3.7 times greater risk of TKA in the first 3 years after knee fracture, and the risk remains 1.6 times greater after 3 years and throughout their lifetimes. Primary knee OA, surgical treatment of knee fractures, external fixation, proximal tibia fractures, and distal femur fractures are risk factors of TKA. This is important because these risk estimates and risk factors highlight the treatment burden of knee fractures, building a foundation for future studies to further counsel patients on their risk of undergoing TKA based on patient-, fracture-, and treatment-specific factors.
Acknowledgments
We thank Thomas Kallemose MSc, for statistical guidance.
Footnotes
The institution of one or more of the authors (VV) has received, during the study period, funding from the Foundation of P. Carl Petersen (grant number 17085); Danish Rheumatism Association (grant number R155-A4838); Research Unit Næstved, Slagelse, and Ringsted Hospitals, Denmark (grant number 06-04-17 and grant number 25-11-16); Region Zealand Health and Medical Science Research Foundation at Production, Research, and Innovation, Naestved, Slagelse, and Ringsted Hospitals, Denmark (grant number 180886); Data and Development Support, Region Zealand, Denmark (grant number 13-000835); Næstved, Slagelse, and Ringsted Hospitals’ Research Fund, Denmark (grant number 1-10-18); the Graduate School of Health and Medical Sciences, University of Copenhagen (grant number 732404); and Clinical Orthopaedic Research Hvidovre, Hvidovre Hospital (grant number 18-11-2018).
Each author certifies that he or she has no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery in Slagelse Hospital, Slagelse, Denmark.
References
- 1.Ahearn N, Oppy A, Halliday R, Rowett-Harris J, Morris SA, Chesser TJ, Livingstone JA. The outcome following fixation of bicondylar tibial plateau fractures. Bone Joint J . 2014;96 B:956–962. [DOI] [PubMed] [Google Scholar]
- 2.Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol . 2010;11:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canadian Orthopaedic Trauma Society, McKee MD. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. J Bone Joint Surg Am . 2006;88:2613–2623. [DOI] [PubMed] [Google Scholar]
- 4.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–697. [DOI] [PubMed] [Google Scholar]
- 5.Court-Brown CM, Clement ND, Duckworth AD, Aitken S, Biant LC, McQueen MM. The spectrum of fractures in the elderly. Bone Joint J . 2014;96 B:366–372. [DOI] [PubMed] [Google Scholar]
- 6.Elsoe R, Larsen P, Nielsen NPH, Swenne J, Rasmussen S, Ostgaard SE. Population-based epidemiology of tibial plateau fractures. Orthopedics. 2015;38:e780-786. [DOI] [PubMed] [Google Scholar]
- 7.Houdek MT, Watts CD, Shannon SF, Wagner ER, Sems SA, Sierra RJ. Posttraumatic total knee arthroplasty continues to have worse outcome than total knee arthroplasty for osteoarthritis. J Arthroplasty. 2016;31:118–123. [DOI] [PubMed] [Google Scholar]
- 8.Kester BS, Minhas S V, Vigdorchik JM, Schwarzkopf R. Total knee arthroplasty for posttraumatic osteoarthritis: Is it time for a new classification? J Arthroplasty. 2016;31:1649–1653. [DOI] [PubMed] [Google Scholar]
- 9.Kremers HM, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am . 2014;97:1386–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lambers K, Ootes D, Ring D. Incidence of patients with lower extremity injuries presenting to US emergency departments by anatomic region, disease category, and age. Clin Orthop Relat Res . 2012;470:284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larsen P, Court-Brown CM, Vedel JO, Vistrup S, Elsoe R. Incidence and epidemiology of patellar fractures. Orthopedics. 2016;39:e1154–e1158. [DOI] [PubMed] [Google Scholar]
- 12.Larsen P, Rathleff MS, Østgaard SE, Johansen MB, Elsøe R. Patellar fractures are associated with an increased risk of total knee arthroplasty. Bone Joint J . 2018;100–B:1477–1481. [DOI] [PubMed] [Google Scholar]
- 13.Lebrun CT, Langford JR, Sagi HC. Functional outcomes after operatively treated patella fractures. J Orthop Trauma. 2012;26:422–426. [DOI] [PubMed] [Google Scholar]
- 14.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am . 2012;94:201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lunebourg A, Parratte S, Gay A, Ollivier M, Garcia-Parra K, Argenson JN. Lower function, quality of life, and survival rate after total knee arthroplasty for posttraumatic arthritis than for primary arthritis. Acta Orthop . 2015;86:189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marczak D, Synder M, Sibiński M, Okoń T, Kowalczewski J. One-stage total knee arthroplasty with pre-existing fracture deformity post-fracture total knee arthroplasty. J Arthroplasty. 2014;29:2104–2108. [DOI] [PubMed] [Google Scholar]
- 17.Mehin R, O’Brien P, Broekhuyse H, Blachut P, Guy P. Endstage arthritis following tibia plateau fractures: Average 10-year follow-up. Can J Surg . 2012;55:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nordic Medico-Statistical Committee. SKS-browseren. Available at: http://medinfo.dk/sks/brows.php. Accessed October 13, 2019.
- 19.Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol . 2011;173:676–682. [DOI] [PubMed] [Google Scholar]
- 20.Saleh H, Yu S, Vigdorchik J, Schwarzkopf R. Total knee arthroplasty for treatment of post-traumatic arthritis: Systematic review. World J Orthop . 2016;7:584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol . 2014;29:541–549. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: A review of content, data quality, and research potential. Clin Epidemiol . 2015;7:449–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sluys KP, Shults J, Richmond TS. Health related quality of life and return to work after minor extremity injuries: A longitudinal study comparing upper versus lower extremity injuries. Injury. 2016;47:824–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Softness KA, Murray RS, Evans BG. Total knee arthroplasty and fractures of the tibial plateau. World J Orthop . 2017;8:107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Statistics Denmark. Den mobile statistikbank. Available at: https://m.statbank.dk/. Accessed October 13, 2019.
- 26.Stevenson I, McMillan TE, Baliga S, Schemitsch EH. Primary and secondary total knee arthroplasty for tibial plateau fractures. J Am Acad Orthop Surg . 2018;26:386–395. [DOI] [PubMed] [Google Scholar]
- 27.van Dreumel RLM, Van Wunnik BPW, Janssen L, Simons PCG, Janzing HMJ. Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46:1608–1612. [DOI] [PubMed] [Google Scholar]
- 28.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg . 2014;12:1495–1499. [DOI] [PubMed] [Google Scholar]
- 29.Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture. J Bone Joint Surg Am . 2014;96:144–150. [DOI] [PubMed] [Google Scholar]
- 30.Wennergren D, Bergdahl C, Ekelund J, Juto H, Sundfeldt M, Möller M. Epidemiology and incidence of tibia fractures in the Swedish Fracture Register. Injury. 2018;49:2068–2074. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization Family of International Classifications. WHO-FIC. Available at: http://www.who.int/classifications/en/. Accessed October 13, 2019.