Abstract
Orbital myositis is a rare manifestation of systemic lupus erythematosus (SLE). Herein, we report a case of orbital myositis in a patient with SLE, along with a literature review. A 45-year-old female patient presented with pain in the right eye, chemosis, proptosis, and limited abduction. Computed tomography of her orbits revealed thickening of her right lateral rectus muscle. She had no other systemic symptoms. There was no elevation in the biomarkers of inflammation or disease activity. She was treated with high-dose steroids, and her symptoms resolved rapidly. It is important to maintain a high index of suspicion for orbital myositis in patients with SLE even when there are no systemic disease activities, such that early treatment can be initiated. It is also important to rule out other mimickers such as orbital cellulitis and thyroid eye disease.
Keywords: Myositis, orbital myositis, systemic lupus erythematosus, discoid lupus erythematosus
Introduction
Ocular manifestations can develop in at least one-third of patients with systemic lupus erythematosus (SLE) and may affect any part of the eye (1). These conditions can be associated with significant morbidity and can be the initial manifestation of SLE (2). The most common ocular complication associated with SLE is keratoconjunctivitis sicca, which typically only results in mild irritation (3). However, conditions that involve the optic nerve (e.g., ischemic optic neuropathy and optic neuritis), retina (e.g., lupus retinopathy), and orbital structures (e.g., orbital vasculitis and orbital myositis) can pose a threat to vision and require early systemic therapy (3–6). Medications used for treating SLE can also cause ocular complications. For example, corticosteroids can cause glaucoma and cataracts, and hydroxychloroquine use can lead to toxic maculopathy.
This article focuses on orbital myositis, a condition that is characterized by the inflammation of extraocular muscles and a rare complication of SLE. Although it does not typically threaten vision and usually responds well to steroids, it can progress to diffuse orbital inflammation and more serious complications such as optic neuritis and ocular ischemia (7, 8). We report a case of a 45-year-old female patient with SLE who presented with acute orbital myositis.
Case Presentation
A 45-year-old Caucasian female presented to our emergency department (ED) with a 2-week history of worsening right eye pain, redness, and swelling. She had received the diagnosis of SLE 4 years ago, and her disease manifestations included polyarthritis, hypocomplementemic urticarial vasculitis, immune thrombocytopenic purpura requiring splenectomy, and pericardial effusion in the context of a non-ST elevated myocardial infarction. She had no other comorbidities. Previous investigations showed positive test results for anti-nuclear antibody (ANA), anti-Smith, anti-SSA, and anti-SSB, but a negative result for anti-dsDNA. She had been treated with azathioprine since her diagnosis 4 years ago and was maintained on 200 mg daily. She had previously trialed hydroxychloroquine but had developed general malaise and was unable to tolerate the medication. Before her presentation to the ED, she was assessed by her rheumatologist and was started on prednisone 5 mg daily a week ago; however, her symptoms continued to worsen. She had no other nonocular symptoms at presentation, although she reported a recent 1-week history of joint swelling and pain in her left knee and right foot that had resolved. On physical examination, she was afebrile, and her vital signs were within normal limits. She had right eye chemosis, injection, and 3-mm right eye proptosis as measured by the Hertel exophthalmometry method. She also reported binocular diplopia consistent with right eye abduction deficit. Her afferent visual function was intact with best-corrected visual acuity of 20/25 in each eye. There was no relative afferent pupillary defect. Color vision testing was intact. There was no evidence of retinal or optic nerve dysfunction. The laboratory investigations revealed a normal complete blood cell count and creatinine. Her anti-dsDNA remained negative, and C3 and C4 were within normal limits. Her C-reactive protein (CRP) was 4 mg/L (reference range: 0–5 mg/L), and creatine kinase (CK) was 27 U/L (reference range: <170 U/L). Test results for anticytoplasmic antibodies (i.e., p-ANCA and c-ANCA) were negative. Her thyroid-stimulating hormone was within the reference range, which suggested against thyroid orbitopathy. There was low suspicion for sarcoidosis, and calcium and angiotensin-converting enzyme levels were within normal limits. Computed tomography (CT) of her orbits revealed thickening of the right lateral rectus muscle and right periorbital soft tissue, including the tendon, with stranding of bordering fat (Figure 1 and 2). A diagnosis of orbital myositis was made on the basis of her clinical presentation and imaging findings. Infectious causes were considered; however, they were deemed less likely given the lack of other infectious symptoms and her recent SLE-like symptoms. She was treated with methylprednisolone 1 g/d for 3 days on the day of her presentation (i.e., 14 days after the onset of symptoms). Over the next 2 to 3 days, her symptoms improved rapidly. She was then continued on prednisone 60 mg/d with a slow taper. Azathioprine was discontinued, followed by a switch to mycophenolate mofetil. A repeat CT scan performed a month later showed resolution of her orbital myositis. She had no recurrence of ocular symptoms over the next 6 months. Written informed consent was obtained from the patient.
Figure 1.
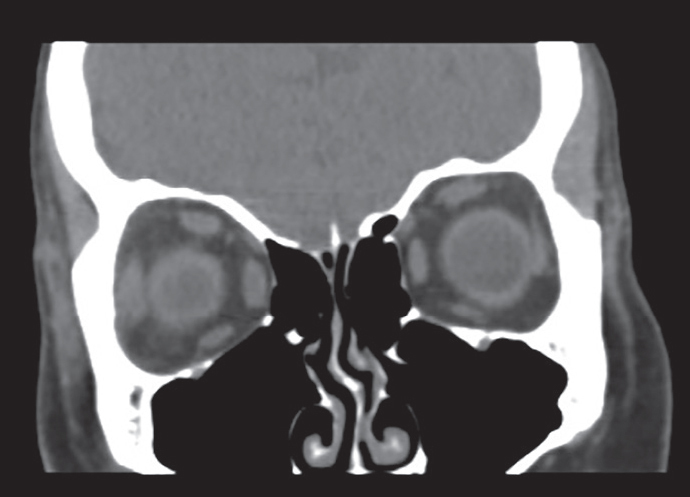
Coronal view of computed tomography (CT) orbits showing thickening of the right lateral rectus muscle and right sided peri-orbital soft tissue with stranding of bordering fat.
Figure 2.

Axial view of computed tomography (CT) orbits showing thickening of the right lateral rectus muscle and right sided peri-orbital soft tissue with stranding of bordering fat.
Discussion
Orbital myositis is associated with many rheumatologic conditions, such as SLE, dermatomyositis, rheumatoid arthritis, sarcoidosis, and granulomatosis with polyangiitis (9, 10). Its pathogenesis is not well understood, but it is likely an immune-mediated process. There are no diagnostic criteria for this condition, and it is largely a diagnosis of exclusion. Enlargement of one or more extraocular muscles can be seen on imaging, and patients usually respond rapidly to high-dose corticosteroids (10). The most common conditions that can mimic orbital myositis are orbital cellulitis and thyroid orbitopathy. Patients with orbital cellulitis typically present with fever and leukocytosis and often have a history of trauma or other head and neck infections (e.g., sinusitis; eyelid, facial, or dental infections). Thyroid eye disease usually has an insidious onset and is associated with eyelid retraction, lid lag, and proptosis. It tends to be tendon sparing on imaging and can be ruled out with thyroid function tests and thyroid antibodies. Other diseases on the differential of orbital myositis include sarcoidosis, vasculitis, arteriovenous malformations, and neoplastic causes (e.g., lymphoma, lymphangioma, metastatic carcinoma, and uveal melanoma) (9, 10). Many of these entities can be distinguished on the basis of radiographic characteristics on ultrasound, CT, and/or magnetic resonance imaging. However, if there is no or incomplete response to steroid therapy, then a biopsy is indicated (9, 10).
To our knowledge, only six cases of orbital myositis in SLE have been reported in the literature (2, 7–9, 11, 12) (see Supplementary Table 1 for details). We also identified two cases of orbital myositis in discoid lupus erythematosus (DLE) (13, 14). All cases presented similarly with eye pain, swelling, proptosis, diplopia, and limitations in extraocular movement. Unilateral and bilateral involvements were both reported. Most did not have other systemic SLE activities but were usually associated with a change in the biomarkers of inflammation and disease activity. However, our patient had normal levels of CRP, CK, anti-dsDNA, C3, and C4. This was also described in the two patients with DLE (13, 14). As such, even when patients present without systemic symptoms or a change in their inflammatory and disease activity biomarkers, a high index of suspicion should be maintained in patients with SLE. Most cases had complete resolution of their ocular symptoms with steroid therapy, with the exception of a case in which the patient had already developed ocular ischemia and vision loss at the time of presentation (8). Hence, early diagnosis and treatment of this condition is crucial.
In conclusion, orbital myositis can present in patients with SLE in the absence of systemic activity or changes in biomarkers of inflammation and disease activity. It can also mimic other common ocular conditions and thus can be a diagnostic challenge. However, when diagnosed and treated promptly, most patients make a complete recovery with no long-term sequelae.
Main Points.
Orbital myositis can mimic common ocular conditions, such as thyroid disease and orbital cellulitis, and thus can be a diagnostic challenge.
Patients with SLE may present with orbital myositis with no other systemic disease activity or elevation in biomarkers of inflammation.
Orbital myositis associated with SLE has excellent response to high-dose steroid therapy when initiated early.
Supplementary Data
Supplementary Table 1.
Summary of published cases of orbital myositis in patients with systemic lupus erythematosus or discoid lupus erythematosus.
| Author | Age (years)/sex | Involved muscles | SLE/DLE diagnosis (duration) | Therapy at time of presentation | Systemic symptoms | Labs | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Case in presentation | 45/F | Right lateral rectus | SLE (4 years) | Azathioprine 200 mg daily, Prednisone 5 mg daily | No | CRP 4 mg/L CK 27 U/L Anti-dsDNA 2.6 IU/mL C3 0.92 g/L C4 0.1 g/L |
Methylprednisolone 1 g IV Methylprednisolone daily × 3 days, prednisone 60 mg (1 mg/kg) daily with slow taper Switch from azathioprine to Cellcept | Symptoms resolved |
| SLE | ||||||||
| Rico et al. (7) | 49/F | Right superior rectus and superior oblique | SLE (10 years) | Azathioprine 50 mg three times a day Prednisone 5 mg daily Belimumab 640 mg IV every 4 weeks | No | Anti-dsDNA 167 IU/mL C3 0.76 g/L C4 0.07 g/L |
Methylprednisolone 1 g by mouth daily × 5 days, then prednisone with slow taper and rituximab | Symptoms resolved |
| Santosa et al. (9) | 38/F | Left lateral rectus | SLE | Methotrexate Prednisolone | No | ESR 102 mm/h CK normal | High-dose IV steroids | Symptoms resolved |
| Stavrou et al. (8) | 73/F | Non-specified | SLE (3 weeks) | Prednisolone 0.8 mg/kg/d | No | Not reported | Topical dexamethasone 0.1% and carteolol 1% Acetazolamide 500 mg by mouth daily Cyclophosphamide 10 mg/kg IV IVIG 0.5 g/kg/d × 3 days | Proptosis and edema resolved but had permanent visual deficit* |
| Serop et al. (2) | 41/F | Right lateral and inferior rectus Left medial rectus | No diagnosis | None | Yes | ESR 27 mm/h Aldolase normal Anti-dsDNA positive |
Prednisolone 64 mg/d Azathioprine 150 mg/d |
Symptoms resolved, with no recurrence within a year |
| Grimson et al. (11) | 39/M | Left lateral and medial rectus Right lateral rectus | SLE (7 years) | Hydroxychloroquine 200 mg daily Quinacrine hydrochloride 50 mg four times a day | Yes | CK 5236 U/L Aldolase high C3 22 g/L C4 3 g/L |
Methylprednisolone 60 mg IV daily, then 40 mg IV twice a day when symptoms persisted, then prednisone 100 mg by mouth daily with slow taper over 3 months | Symptoms resolved |
| Weinstein et al. (12) | 32/F | L superior rectus, left lateral rectus, R medial rectus | SLE | Hydroxychloroquine 250 mg daily Prednisone 5 mg daily | No | ESR 29 mm/h CK <8 mg/100 mL C3 mildly decreased C4 mildly decreased |
Prednisone 80 mg daily × 1 week, then taper over 6 months | Symptoms resolved, with one recurrence within 6 months |
| DLE | ||||||||
| Arrico et al. (13) | 37/F | Left medial rectus | DLE (5 years) | Not reported | No | ESR 20 mm/h CK normal C3 normal C4 normal |
Methylprednisolone 1 g IV daily × three days, then prednisone 20 mg by mouth daily with tapering 5 mg per week | Symptoms resolved with one recurrence within 6 months |
| Kono et al. (14) | 42/F | Bilateral medial and lateral rectus | DLE (10 years) | Mizoribine 50 mg daily | No | CK normal Anti-dsDNA negative C3 normal C4 normal |
Methylprednisolone 1 g IV daily × 3 days, then prednisone 20 mg by mouth daily | Symptoms resolved |
This patient also had ocular ischemia.
SLE: systemic lupus erythematosus; DLE: discoid lupus erythematosus; CRP: C-reactive protein; CK: creatine kinase; ESR: erythrocyte sedimentation rate; F: female; M: male.
Footnotes
Content of this journal is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Informed Consent: Written informed consent was obtained from the patient.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.L., A.J.C.; Design - A.S.R., S.L., A.J.C.; Supervision - A.S.R., S.L.,; Data Collection and/or Processing - A.S.R., S.L., A.J.C.; Analysis and/or Interpretation - A.S.R., S.L., A.J.C.; Literature Search - A.J.C.; Writing Manuscript - A.J.C.; Critical Review - S.L., A.J.C.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Read R. Clinical mini-review: Systemic lupus erythematosus and the eye. Ocul Immunol Inflamm. 2004;12:87–99. doi: 10.1080/09273940490895308. [DOI] [PubMed] [Google Scholar]
- 2.Serop S, Vianna RN, Claeys M, De Laey JJ. Orbital myositis secondary to systemic lupus erythematosus. Acta Ophthalmol. 1994;72:520–23. doi: 10.1111/j.1755-3768.1994.tb02807.x. [DOI] [PubMed] [Google Scholar]
- 3.Sivaraj RR, Durrani OM, Denniston AK, Murray PI, Gordon C. Ocular manifestations of systemic lupus erythematosus. Rheumatology. 2007;46:1757–62. doi: 10.1093/rheumatology/kem173. [DOI] [PubMed] [Google Scholar]
- 4.Shoughy SS, Tabbara KF. Ocular findings in systemic lupus erythematosus. Saudi J Ophthalmol. 2016;30:117–21. doi: 10.1016/j.sjopt.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palejwala NV, Walia HS, Yeh S. Ocular manifestations of systemic lupus erythematosus: A review of the literature. Autoimmune Dis. 2012;2012 doi: 10.1155/2012/290898. 290898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silpa-archa S, Lee JJ, Foster CS. Ocular manifestations in systemic lupus erythematosus. Br J Ophthalmol. 2016;100:135–41. doi: 10.1136/bjophthalmol-2015-306629. [DOI] [PubMed] [Google Scholar]
- 7.Rico M, Diaz-Lopex JB, Pena J, Oliva-Nacarino P. Latent orbital pseudotumor secondary to systemic lupus erythematosus. Clin Case Rep. 2016;4:1065–7. doi: 10.1002/ccr3.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stavrou P, Murray PI, Batta K, Gordon C. Acute ocular ischaemia and orbital inflammation associated with systemic lupus erythematosus. Br J Ophthalmol. 2002;86:474–5. doi: 10.1136/bjo.86.4.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santosa A, Vasoo S. Orbital myositis as manifestation of systemic lupus erythematosus - a case report. Postgrad Med J. 2013;89:59. doi: 10.1136/postgradmedj-2012-130974. [DOI] [PubMed] [Google Scholar]
- 10.Espinoza GM. Orbital inflammatory pseudotumors: Etiology, differential diagnosis, and management. Curr Rheumatol Rep. 2010;12:443–7. doi: 10.1007/s11926-010-0128-8. [DOI] [PubMed] [Google Scholar]
- 11.Grimson BS, Simons KB. Orbital inflammation, myositis and systemic lupus erythematosus. Arch Ophthalmol. 1983;101:736–8. doi: 10.1001/archopht.1983.01040010736006. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein GS, Dresner SC, Slamovits TL, Kennerdell JS. Acute and subacute orbital myositis. Am J Ophthalmol. 1983;96:209–17. doi: 10.1016/S0002-9394(14)77789-X. [DOI] [PubMed] [Google Scholar]
- 13.Arrico L, Abbouda A, Bianchi S, Malagola R. Acute monolateral proptosis and orbital myositis in a patient with discoid lupus erythematosus: A case report. J Med Case Rep. 2014;20:375. doi: 10.1186/1752-1947-8-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kono S, Takashima H, Suzuki D, Terada T, Konishi T, Miyajima H. Orbital myositis associated with discoid lupus erythematosus. Lupus. 2014;23:220–2. doi: 10.1177/0961203313517156. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Summary of published cases of orbital myositis in patients with systemic lupus erythematosus or discoid lupus erythematosus.
| Author | Age (years)/sex | Involved muscles | SLE/DLE diagnosis (duration) | Therapy at time of presentation | Systemic symptoms | Labs | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Case in presentation | 45/F | Right lateral rectus | SLE (4 years) | Azathioprine 200 mg daily, Prednisone 5 mg daily | No | CRP 4 mg/L CK 27 U/L Anti-dsDNA 2.6 IU/mL C3 0.92 g/L C4 0.1 g/L |
Methylprednisolone 1 g IV Methylprednisolone daily × 3 days, prednisone 60 mg (1 mg/kg) daily with slow taper Switch from azathioprine to Cellcept | Symptoms resolved |
| SLE | ||||||||
| Rico et al. (7) | 49/F | Right superior rectus and superior oblique | SLE (10 years) | Azathioprine 50 mg three times a day Prednisone 5 mg daily Belimumab 640 mg IV every 4 weeks | No | Anti-dsDNA 167 IU/mL C3 0.76 g/L C4 0.07 g/L |
Methylprednisolone 1 g by mouth daily × 5 days, then prednisone with slow taper and rituximab | Symptoms resolved |
| Santosa et al. (9) | 38/F | Left lateral rectus | SLE | Methotrexate Prednisolone | No | ESR 102 mm/h CK normal | High-dose IV steroids | Symptoms resolved |
| Stavrou et al. (8) | 73/F | Non-specified | SLE (3 weeks) | Prednisolone 0.8 mg/kg/d | No | Not reported | Topical dexamethasone 0.1% and carteolol 1% Acetazolamide 500 mg by mouth daily Cyclophosphamide 10 mg/kg IV IVIG 0.5 g/kg/d × 3 days | Proptosis and edema resolved but had permanent visual deficit* |
| Serop et al. (2) | 41/F | Right lateral and inferior rectus Left medial rectus | No diagnosis | None | Yes | ESR 27 mm/h Aldolase normal Anti-dsDNA positive |
Prednisolone 64 mg/d Azathioprine 150 mg/d |
Symptoms resolved, with no recurrence within a year |
| Grimson et al. (11) | 39/M | Left lateral and medial rectus Right lateral rectus | SLE (7 years) | Hydroxychloroquine 200 mg daily Quinacrine hydrochloride 50 mg four times a day | Yes | CK 5236 U/L Aldolase high C3 22 g/L C4 3 g/L |
Methylprednisolone 60 mg IV daily, then 40 mg IV twice a day when symptoms persisted, then prednisone 100 mg by mouth daily with slow taper over 3 months | Symptoms resolved |
| Weinstein et al. (12) | 32/F | L superior rectus, left lateral rectus, R medial rectus | SLE | Hydroxychloroquine 250 mg daily Prednisone 5 mg daily | No | ESR 29 mm/h CK <8 mg/100 mL C3 mildly decreased C4 mildly decreased |
Prednisone 80 mg daily × 1 week, then taper over 6 months | Symptoms resolved, with one recurrence within 6 months |
| DLE | ||||||||
| Arrico et al. (13) | 37/F | Left medial rectus | DLE (5 years) | Not reported | No | ESR 20 mm/h CK normal C3 normal C4 normal |
Methylprednisolone 1 g IV daily × three days, then prednisone 20 mg by mouth daily with tapering 5 mg per week | Symptoms resolved with one recurrence within 6 months |
| Kono et al. (14) | 42/F | Bilateral medial and lateral rectus | DLE (10 years) | Mizoribine 50 mg daily | No | CK normal Anti-dsDNA negative C3 normal C4 normal |
Methylprednisolone 1 g IV daily × 3 days, then prednisone 20 mg by mouth daily | Symptoms resolved |
This patient also had ocular ischemia.
SLE: systemic lupus erythematosus; DLE: discoid lupus erythematosus; CRP: C-reactive protein; CK: creatine kinase; ESR: erythrocyte sedimentation rate; F: female; M: male.


