Abstract
Objective
To evaluate cases of insufficiency fractures verified by magnetic resonance imaging (MRI) of the knee, ankle, and foot in patients with rheumatoid arthritis (RA) cared for in our clinic over an 8-year period, to identify possible risk factors, and to test these in a case-control study.
Methods
All patients in the rheumatology clinic with RA were registered prospectively in the database, DANBIO. All MRIs ordered from the clinic were registered and coded according to the anatomical region. We were thus able to retrieve all patients with RA and performed an MRI of the knee or ankle/foot. The patients with fractures constituted the case series, and the patients without fractures constituted the control group.
Results
The RA clinic population comprised 1,624 patients who underwent a total of 70 MRIs. Case series: 39 insufficiency fractures were identified in 32 patients; 93% were women, and the median age was 68 years (range 33–89 years). Half of the patients had a T score >−2.5. The case control group without fractures comprised 38 patients; 74% were women, and the median age was 62 years (range 32–84 years). In the case series, 20 patients experienced later additional episodes of insufficiency fractures in the knee, ankle, or foot.
Conclusion
Insufficiency fractures of the knee, ankle, and foot are a significant cause of pain and long-lasting disability in RA. Recurrent fractures are common. Diagnosis is often delayed and confused with arthritic activity. Conventional radiography and DEXA scan are often normal. Older age, female gender, radiological erosions in hand/wrist, and treatment with methotrexate were all significantly associated with fractures.
Keywords: Rheumatoid arthritis, insufficiency fracture, stress fracture, MRI
Introduction
Rheumatoid arthritis (RA) is a chronic, progressive, systemic inflammatory disease leading to substantial pain, disability, and other morbidities (1). Patients with RA are at an increased risk of osteoporosis and osteoporotic fractures, aggravated by factors such as inactivity or corticosteroid therapy (2–5). The occurrence of spontaneous extremity fractures in RA, including stress and insufficiency fractures, has only occasionally been reported in the medical literature, primarily in the form of case reports or case series (6–14). Published epidemiological studies on the occurrence of fractures in RA are almost entirely based on the use of conventional radiography as the diagnostic imaging modality (2, 15). However, MRI has been shown to be considerably more sensitive in the detection of occult fractures, which commonly can be overlooked under conventional radiography (16). An insufficiency fracture occurs when the mechanical strength of a bone is reduced to the point where it breaks by a given physiological stress that would normally not lead to a fracture in a healthy bone. Reduced bone strength can be typically due to generalized osteopenia in the skeleton as observed in osteoporosis, osteomalacia, or osteogenesis imperfecta, as well as due to localized osteopenia caused by demineralization in a limb due to inactivity (7).
RA patients frequently contact rheumatology clinics due to an increase in their joint pain or emergence of new articular or periarticular pain at a new site, despite their ongoing treatment. Most often, increased arthritis disease activity is the cause of such pain; however, secondary osteoarthritis and joint deformities are other possible causes and therefore should be considered in differential diagnosis. The treatment of joint pain in such patients will usually include joint injections with steroids, adding or increasing the dose of concomitant antirheumatic medications, including nonsteroidal anti-inflammatory drugs and orthoses. Pain in the hips or back is unlikely to be confused with arthritis disease activity because RA predominantly attacks the peripheral joints. However, pain, swelling, and disability caused by insufficiency fractures of the lower extremities may be easily mistaken for rheumatoid synovitis (9). Plain radiographs taken initially may not reveal the fracture (8, 10). Therefore, RA patients, those presenting with local pain in the knee, ankle, or foot, particularly if a single periarticular site is involved and those who also have normal articular findings on ultrasound examination, should be examined with an MRI to confirm or rule out a diagnosis of an insufficiency fracture, irrespective of the absence of a trauma history or the presence of normal findings on conventional radiography.
The aim of this study was to review MRI-verified cases of insufficiency fractures of the knee, ankle, and foot in patients with RA cared for in our clinic over an 8-year period and to identify possible risk factors.
Methods
Study design
The study was designed as a retrospective case-control study based on prospectively registered clinical data.
Patients and setting
The clinic of rheumatology, North Denmark Region Hospital, Hjørring cares for around 1,200 RA patients, and, since 2010, all have been prospectively registered twice a year in the clinical database DANBIO (17). Patients have access to clinical consults “on demand” without waiting times or costs. Treatment of the patients follows national guidelines, which is similar to the European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) guidelines. The treatment costs are almost entirely free of charge for the patients. Ultrasonic scanners are readily available to all physicians in the entire clinic. The C-reactive protein (CRP) and Disease-Activity-Score-28 joints with CRP (DAS28crp) values used were the last values recorded before the estimated fracture date. The body mass index of patients was routinely recorded when ordering an MRI.
The inclusion criteria for both the case series and the controls were an RA diagnosis and a first-time MRI of the knee or ankle/foot in the 8-year period from 2010 to 2017. The only exclusion criterion was evident high-energy fractures initially diagnosed and treated by orthopedic surgeons. The case series patients had a fracture of the distal femur, tibia, fibula, talus, calcaneus, and navicular or metatarsal bones detected with an MRI.
The case-control group comprised the patients without fractures (Figure 1). The control group had the same RA diagnosis and were treated by the same staff and with the same treatment principles. In addition, the indications for MRI were largely similar for both groups of patients (unexplained local pain in the knee, ankle, or foot despite clinical, ultrasonic, and conventional radiographic examinations).
Figure 1.
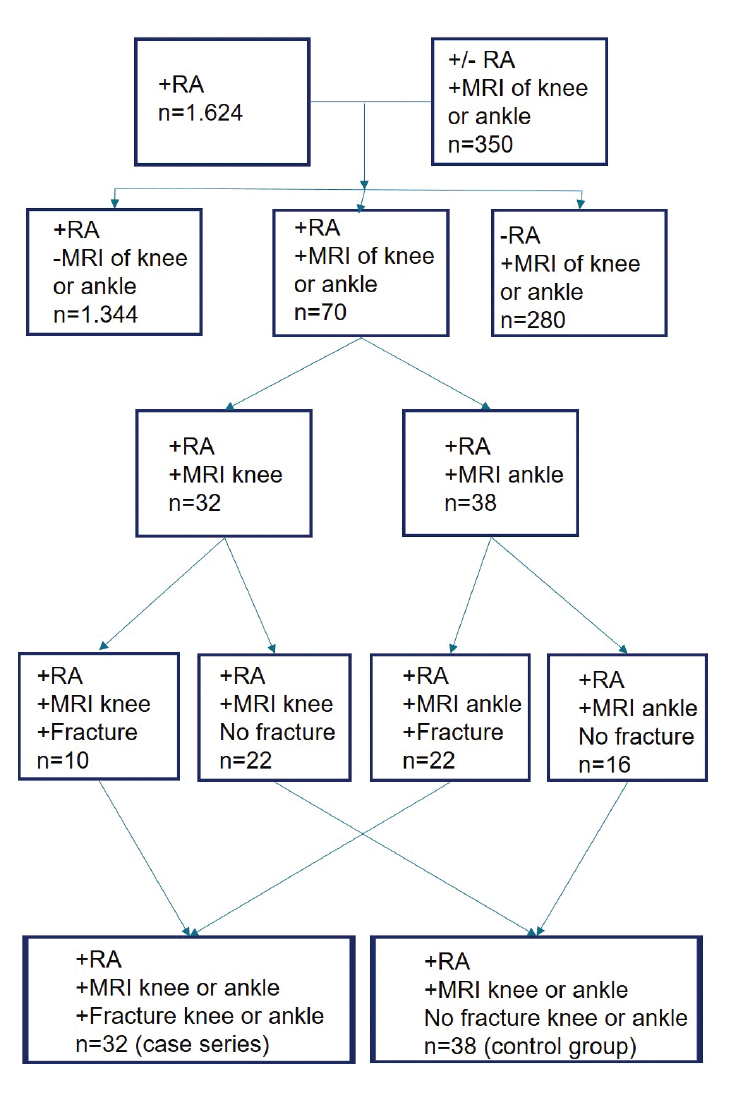
Patient selection for the case series and the case-control group, both with RA and unexplained local pain in the knee, ankle, or foot. In total, 1,624 unique patients with RA were treated in the clinic during 2010–2017. The lower two boxes define the case series and the case-control group. MRI ankle includes foot.
RA: rheumatoid arthritis; MRI: magnetic resonance imaging.
All included patients were unique, that is, if more than one fracture episode occurred in the 8-year period, only the first episode was included.
Statistical analysis
Descriptive statistics of the study populations was presented as medians + quartiles, where data were nonnormally distributed. Test for normality was performed using the Kolmogorov-Smirnoff test for normality. The Mann-Whitney U test was used for comparison of clinical variables and the Fisher’s exact test was performed to test the risk contingency for fractures amongst patients suffering from osteoporosis in comparison with patients not suffering from osteoporosis. P values <0.05 were considered statistically significant. Statistical analysis was carried out after the collection of patient data. After testing for normality, a final decision regarding the remaining statistical testing was done. All statistical analysis was carried out using Graphpad Prism 7.0 (Graphpad; San Diego, CA, USA).
Osteoporosis
DEXA scans examining the lumbar spine and one hip were obtained, and the result was reported as a T score. DEXA scans were not systematically ordered in the clinic, and therefore, T scores were missing for some patients. Some of the patients were referred to DEXA scan by their general practitioner, and others were invited by a local private clinical trial center. The results of these DEXA scans were not always available to us because of incompatibility with the results given on print paper and the hospital’s new electronic patient record IT system. However, we could manage all patients for any prescribed pharmaceutical treatment for osteoporosis.
MRI
Access to MRI was available, with an average waiting time between 2 and 6 weeks. The hospital IT system codes MRI procedures by both anatomical localization and by the requesting clinic. Thus, it is possible to retrieve all MRI scans of the knee and ankle/foot in patients with RA by combining DANBIO and the hospital IT systems. MRIs of the ankle also include MRIs of the foot. After retrieving the patients, both their medical records and MRIs were systematically reviewed.
Ethical considerations
According to the Danish legislation, the registration and publication of data from clinical registries, or quality assurance studies, do not require consent of patients or approval from the Ethics Committees. The study was approved on October 1, 2018 by the North Jutland Region (research registration) with ID number 2018-155.
Results
Description of study population characteristics and fracture incidence rate
A total of 1,624 unique patients with RA received treatment during 2010 to 2017. The selection of patients for the case series and the case-control group is shown in Figure 1. The number of MRIs performed for the knees was 32 with 10 fractures identified, and for the foot/ankle, it was 38 with 22 fractures. The numbers of patients, MRIs performed, and fractures diagnosed for each year are provided in Table 1. The anatomical distribution is shown in Table 2. The case-control study showed several risk factors, which were significantly more common in the case series. Older age, female gender, radiological erosions in hand/wrist, and treatment with methotrexate were all significantly associated with fractures. Other variables that were not associated with fractures included disease duration, positive results for rheumatoid factor or anti-citrullinated protein antibodies (ACPA), erosions in feet, DAS28crp, CRP, smoking, BMI, or use of prednisolone or biologic Disease Modifying Antirheumatic Drug (bDMARD). In the case series, the average age was 68 years, median disease duration was 12 years, and 93% were women. The average DAS28crp was 2.3, that indicates remission. Comparison of the case series and the case-control group is provided in Table 3.
Table 1.
For each year, the total number of RA patients treated in the clinic by the end of each year, the number of MRIs performed, and the number of RA patients with a fracture have been noted. The last two columns display the period in days from onset of symptoms until fracture diagnosis by MRI. Owing to the small number of observations, the delay in days is stated as a range and only the last row as a calculated median.
| Year | RA clinic population | MRI performed | Fracture present | Delay diagnosis in days | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Knee | Ankle/foot | Knee | Ankle/foot | Knee | Ankle/foot | ||
| 2010 | 935 | 3 | 3 | 3 | 2 | 32–214 | 85–241 |
| 2011 | 1,005 | 0 | 4 | 0 | 3 | - | 34–468 |
| 2012 | 1,165 | 5 | 5 | 2 | 4 | 197–249 | 216–948 |
| 2013 | 1,202 | 4 | 4 | 0 | 3 | - | 50–153 |
| 2014 | 1,276 | 3 | 8 | 0 | 4 | - | 30–652 |
| 2015 | 1,352 | 10 | 8 | 3 | 3 | 58–89 | 25–398 |
| 2016 | 1,351 | 3 | 2 | 1 | 0 | 105 | - |
| 2017 | 1,377 | 4 | 4 | 1 | 3 | 18 | 31–60 |
| 2010–2017 | Average 1,208 (of 1,624 unique patients) | 32 | 38 | 10 | 22 | Median 84 | Median 85 |
Table 2.
Anatomical localization of the 39 fractures diagnosed with an MRI in the 32 unique patients (case series). In the cases with recurrent fracture episodes, only the first episode is included.
| Fracture in anatomical region | Knee only | Ankle only | Foot only | Multiple in ankle/foot |
|---|---|---|---|---|
| Distal femur | 1 | - | - | - |
| Proximal tibia | 9 | - | - | - |
| Distal tibia | - | 7 | - | 3 |
| Talus | - | 3 | - | 3 |
| Calcaneus | - | - | 3 | 6 |
| Naviculare/metatarsal | - | - | 3 | 1 |
| Number of fractures | 10 | 10 | 6 | 13 |
| Number of patients | 10 | 10 | 6 | 6 |
Table 3.
Characteristics of the 70 unique patients with RA who had an MRI of the knee or ankle/foot during 2010–2017.
| Variable | Fracture (case series) | No fracture (case-control group) | p |
|---|---|---|---|
| No. of patients | 32 | 38 | - |
| Age (years) | 68.5 (33–89) | 62.5 (32–84) | 0.011 |
| RA duration (years) | 12 (0–45) | 10 (0–33) | NS |
| Gender (No. of females/No. of males) | 30/2 | 28/10 | <0.0001 |
| Anatomy MRI (knee, ankle/foot) | Knee: 10 Ankle: 22 | Knee: 23 Ankle: 15 | - |
| IgM RF, pos/neg/unknown | 25/7/0 | 29/9/0 | NS |
| Anti-CCP, pos/neg/unknown | 18/12/2 | 21/16/1 | NS |
| Erosion upper extremity, +/− | 17/15 | 11/27 | 0.04 |
| Erosion lower extremity, +/− | 16/16 | 11/27 | NS |
| DAS28crp, median (range) | 2.3 (1.6–6.6) | 2.8 (1.3–6.1) | NS |
| CRP (mg/L) | 3 (1–46) | 5 (1–64) | NS |
| MTX treatment, +/− | 31/1 | 29/9 | 0.014 |
| MTX treatment duration years | 6 (0–20) | 5 (0–20) | NS |
| bDMARD, +/− | 4/28 | 1/37 | NS |
| Smoking, yes/stopped/never | 9/10/13 | 11/8/19 | NS |
| BMI (kg/m2), median (range) | 24.5 (18–41) | 27 (20–36) | NS |
NS denotes no statistical difference between groups.
The estimated average annual minimum fracture incidence rate over the study period was 3.31 per 1000 years (32/(935+1005+1165+ 1202+1276+1352+1351+1377 person years)). Only the first fracture episode was included in these incidence calculations, despite 20 patients suffering at least one more episode in the study period.
Clinical and radiological manifestations
The patients with fractures presented symptoms of slight, sudden onset pain in the knee, ankle/foot without any relevant trauma. The onset of fracture symptoms was well described in all the patients’ medical records.
MRI was performed at a median of 84 days (18–948) after the estimated fracture date and with the same delay for knees and ankles/feet. Among the 32 patients with fractures, 26 patients had antecedent conventional radiography, which could not detect the fracture (Figure 2). Despite conventional radiography initially being reported without fracture, three of them later gave evidence of a visible fracture when reviewed after the MRI had detected a fracture. Six patients with fractures were not examined by conventional radiography before MRI. One included a patient with a distal tibia fracture referred to, and registered as, MRI, but who instead had a CT scan because of a metal implant.
Figure 2. a, b.
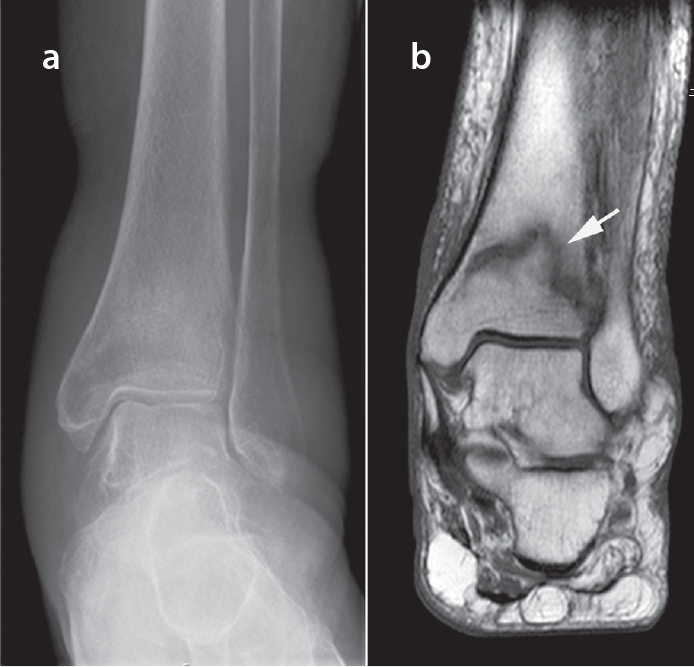
Conventional radiography July 2011 (a). MRI (T1) August 2011 (b). Only on MRI, the distal tibia insufficiency fracture is clearly visible.
Among the 32 patients with fractures, 16 patients were treated with at least one intra-articular steroid injection in the fractured joint before the fracture was diagnosed by MRI. Four of the 16 patients had two injections and one patient even had four.
The patients’ fractures were treated conservatively with an immobilization plaster for several weeks. Twenty of the 32 patients with a fracture episode experienced at least one additional fracture episode in the knee or ankle/foot within the 8-year study period.
Risk factors of insufficiency fractures
The case-control study showed several risk factors, which were significantly more common in the case series. Older age, female gender, radiological erosions in hand/wrist, and treatment with methotrexate were all significantly associated with fractures. Other variables that were not associated with fractures included disease duration, positive results for rheumatoid factor or ACPA, erosions in feet, DAS28crp, CRP, smoking, BMI, and use of prednisolone or bDMARD.
Osteoporosis (T score <−2.5) as measured by DEXA scans was compared between cases and controls and showed a statistically significant difference between the groups (Table 4). Patients with insufficiency fractures had significantly lower T score values than the controls. Additionally, a diagnosis of osteoporosis was found to be statistically significant related to the occurrence of insufficiency fractures in our study population (p=0.027, Fisher test of contingency).
Table 4.
Number of patients with, or without, fracture with presence, or absence, of osteoporosis. DEXA scan results were not available for 15 patients. Osteoporosis was defined as a DEXA scan result <−2.5.
| Result of DEXA scans | Fracture (case series) | No fracture (case-control group) | p |
|---|---|---|---|
| Osteoporosis present | 15 (12 in treatment) | 5 (5 in treatment) | 0.027 (Fisher’s exact test) |
| No osteoporosis | 15 | 20 | |
| DEXA T score, median (range) | −2.48 (−4.13 to 0.50) | −1.42 (−5.0 to 0.54) | 0.0047 (Mann-Whitney Test) |
| No DEXA scan available | 2 | 13 | - |
| Use of prednisolone, actual/ever/never | 7/26/6 | 5/23/14 | NS |
| Osteoporosis treatment, yes/no | 12/3 | 5/1 | NS |
| Osteoporosis treatment duration (years) | 3 (0–8) | 3 (0–11) | NS |
Discussion
In this study, we demonstrate that new-onset knee or ankle/foot pain in patients with RA is frequently due to insufficiency fractures only visible on MRI scans. Most patients experienced significant delays in diagnosis and fracture treatment, resulting in long-term pain and disability. Twenty of the 32 patients (62%) experienced at least one additional fracture episode in the knee or ankle/foot in the 8-year study period. The minimum incidence rate of a first-time insufficiency fracture in the knee or ankle/foot was 3.31/1000 RA patients/year.
Additionally, we found an increased risk of fracture in female patients, in older patients, and in patients with erosions of hand and wrist, in patients treated with methotrexate, and in patients with osteoporosis. In contrast, several other traditionally acknowledged risk factors could not be associated with fractures.
Despite that osteoporosis was statistically and significantly associated with insufficiency fractures in our study, only half of the patients with fractures had osteoporosis. These findings support both routine screening for osteoporosis in patients with RA and scrutiny for the diagnosis of fracture even if osteoporosis is absent.
The use of the unique patients’ ID system and the twice-a-year complete database registration coverage in a stable patient population ensured that no patient information was lost to follow-up. To date, the published case series of insufficiency fractures in patients with RA is very limited in number and principally based on conventional radiography without any long-term follow-up. The criteria used for making the case-control group reflect the clinical situation presented to the rheumatologist when examining a patient with RA with local pain in the knee or ankle/foot.
Our study has some limitations, mostly with respect to underestimation of the true number of fractures. We did not retrieve fractures seen on conventional radiography and which were therefore not examined by MRI. The case series comprised 39 fractures in 32 unique patients, and only the first episode was included. If all the fractures had been included, including the later fracture episodes, the fracture incidence rate would have increased significantly. Our review of original MRI radiological reports excluded the possibility of false positives, but false negatives (failure to report a fracture) may exist (10, 11). MRI capacity is frequently limited; clinicians therefore try to limit the number of referrals, and this reluctance may explain the high “hit rate” of 46% with a fracture. The number of our patients with an MRI-incompatible metal is low, this tends to underestimate the number of fractures detectable only by MRI. The uneven numbers (range 4–18) of MRIs performed by year may indicate the staff’s shifting awareness of insufficiency fractures. Furthermore, it is possible that the true fracture incidence is higher because RA patients with a new onset of knee or ankle pain, and a normal conventional radiography or DEXA scan, are less likely to be referred to an MRI examination. The missing DEXA scans for the control group may weaken the statistical significance. Finally, we cannot exclude asymptomatic cases, or unwillingness to report symptoms, although it seems unlikely from a clinical point of view and from a viewpoint of easy access to free care in the clinic.
The anatomical sites of the insufficiency fractures in our case series, their clinical presentations, and the effects on the patients are similar to those seen in other, but smaller studies (8, 13). Consistent with a previously unreported finding, we have shown that insufficiency fractures are commonly a recurrent problem because 62% of the patients experienced at least one more subsequent insufficiency fractures, either in the same place or elsewhere in the knees or ankles/feet.
A study from 1995 to 1999 examined 33 patients with inflammatory joint disease and insufficiency fractures (14). For 26 patients, the fractures were located in, or below, the knee and mostly in the metatarsal bones. MRI was only used for some selected cases with calcaneal pain. The patients were generally significantly younger, with an average age of 44 years. However, the description of the clinical presentations of fractures corresponds well with our findings.
An epidemiological study examined the incident first-time fractures in 1008 female patients with RA in an 8-year period from 1994 to 2001 (2). By conventional radiography, 82 fractures were diagnosed, of which 15 were in, or distal to, the knee and 26 in the spine. The relative risk of any incident first-time fracture for patients with RA was 1.43 (95% CI 0.98–2.09) compared to the general population.
A retrospective study of 2,250 patients with RA from 1990 to 1999 found 18 patients with stress fractures, of which 11 were in the knee, ankle, or foot (8). The fractures were diagnosed using conventional radiography and, in one patient, using isotope bone scan. The delay of diagnosis was a median of 4 (range 1–12) weeks. Ongoing, and high-dose, treatment with corticosteroids was more common in patients with fractures than that in controls. Osteoporosis was not found to be a risk factor. Clinical presentation of fractures and delays in diagnosis correspond to our findings.
A study prospectively examined 209 patients with RA for possible fractures in a 1-year period with four scheduled examinations by an orthopedic surgeon who frequently used either conventional radiography, CT, MRI, or bone scans (13). Most patients were in current long-term treatment with corticosteroids, but no other treatments were explained. They found five cases with insufficiency fractures in the knee or ankle/foot. This number is significantly higher than expected from our study and probably explained by patients with a more severe disease, a high prevalence of previous joint surgery, and careful search for even minor pain problems indicating a fracture.
The inclusion criteria we used for both the case series and the control group may explain why our findings differ from those of other studies. We consequently used first-time MRI for diagnosis and did not use any other types of radiography. We selected our control group to most accurately mimic the clinical presentation of patients with RA with insufficiency fractures consulting a rheumatologist.
Knees, ankles, and feet are weight-bearing joints and commonly deformed in RA. These conditions, together with the increased incidence of reduced bone strength in patients with RA, are some of the possible risk factors for insufficiency fractures or stress fractures. Corticosteroid treatment may predispose such patients to insufficiency fractures rather than disease-specific factors such as RA disease activity or duration, a suggestion supported by others (8–12). However, stress fractures in RA were also reported before the introduction of corticosteroid treatment (18). We may also speculate whether patients with RA have localized reduced bone mass around their joints corresponding to the halisteresis around joints commonly observed by conventional radiography.
Some studies have suggested a causal relationship between insufficiency fractures and the use of methotrexate (19, 20), while others have not been able to find such a correlation (15). Our case-control study found that treatment with methotrexate was significantly associated with fractures but not with the duration of the treatment. This might support the belief that there is a causal relationship. However, in our clinical experience, we have not seen this type of fracture in patients treated with methotrexate for other common joint diseases, e.g., psoriatic arthritis.
Insufficiency fractures in knees, ankles, or feet are not uncommon and are most likely even found to be more frequent if the physicians are more aware of the diagnosis and clinical presentation. Hopefully, more awareness can lead to fewer delays in the diagnosis and avoidance of potential harmful treatments.
We do not fully understand why patients with RA suffer from unusual fractures. Osteoporosis is a risk factor, but half of the patients with fractures had no osteoporosis. We do not know an effective way to prevent these fractures, and especially one to avoid the high rate of subsequent insufficiency fractures in knees, ankles, and feet. Different types of osteoporosis medication work differently in different anatomical regions (spine, hip, radius, and tibia). We therefore do not know what type of medicine will be effective after a fracture in the knee or ankle/foot to prevent new fractures (21). Treatment of, and rehabilitation after, these fractures is complex, e.g., difficulties in using crutches and wheelchairs because of hand or wrist problems. The necessary period for no weight load during plastering is not clear and the time for definite fracture healing is difficult to ascertain. All the above-mentioned unanswered questions call for more research.
In conclusion, a diagnosis of insufficiency fracture should be considered in elderly female patients with RA who present with unexplained lower extremity joint pain and MRI should be performed even if the initial conventional radiographs and DEXA scans are normal.
Main Points.
Lower extremity insufficiency fractures in patients with rheumatoid arthritis are common.
Most patients will encounter new or recurrent fractures within a few years.
Fracture diagnoses are often delayed and only visible after MRI.
Elderly female patients are at particular risk.
MRI is recommended even if conventional radiography and DEXA scans are normal.
Footnotes
Content of this journal is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Ethics Committee Approval: No ethical approval was needed in Denmark for this type of study. Instead the study has been approved by the local data protection agency, North Denmark Region Research Administration. (Approval Date: October 1, 2018; Approval Number: 2018-155).
Informed Consent: Written informed consent was not obtained due to the nature of the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.Y., S.K.F., C.R.; Design - A.Y., S.K.F., C.R.; Supervision - A.Y., S.K.F., C.R.; Materials - A.Y., S.K.F., C.R.; Data Collection and/or Processing - A.Y., S.K.F., C.R.; Analysis and/or Interpretation - A.Y., S.K.F., C.R.; Literature Search - A.Y., S.K.F., C.R.; Writing Manuscript - A.Y., S.K.F., C.R.; Critical Review - A.Y., S.K.F., C.R.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Michaud K, Wolfe F. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007;21:885–906. doi: 10.1016/j.berh.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Brennan SL, Toomey L, Kotowicz MA, Henry MJ, Griffiths H, Pasco JA. Rheumatoid arthritis and incident fracture in women: A case-control study. BMC Musculoskelet Disord. 2014;15:13. doi: 10.1186/1471-2474-15-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SY, Schneeweiss S, Liu J, Daniel GW, Chang CL, Garneau K, et al. Risk of osteoporotic fracture in a large population-based cohort of patients with rheumatoid arthritis. Arthritis Res Ther. 2010;12:R154. doi: 10.1186/ar3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Resnick D, Cone R. Pathological fractures in rheumatoid arthritis. RadioGraphics. 1984;4:549–62. doi: 10.1148/radiographics.4.3.549. [DOI] [Google Scholar]
- 5.Hauser B, Riches PL, Wilson JF, Horne AE, Ralston SH. Prevalence and clinical prediction of osteoporosis in a contemporary cohort of patients with rheumatoid arthritis. Rheumatology. 2014;53:1759–66. doi: 10.1093/rheumatology/keu162. [DOI] [PubMed] [Google Scholar]
- 6.Spina A, Clemente A, Vancini C, Fejzo M, Campioni P. Spontaneous talar and calcaneal fracture in rheumatoid arthritis: A case report. J Radiol Case Rep. 2011;5:15–23. doi: 10.3941/jrcr.v5i7.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pentecost RL, Murray RA, Brindley HH. Fatigue, insufficiency, and pathologic fractures. JAMA. 1964;187:1001–4. doi: 10.1001/jama.1964.03060260029006. [DOI] [PubMed] [Google Scholar]
- 8.Kay L, Holland T, Platt P. Stress fractures in rheumatoid arthritis: A case series and case-control study. Ann Rheum Dis. 2004;63:1690–2. doi: 10.1136/ard.2003.010322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fam AG, Shuckett R, McGillivray DC, Little AH. Stress fractures in rheumatoid arthritis. J Rheumatol. 1983;10:722–6. [PubMed] [Google Scholar]
- 10.Schneider R, Kaye JJ. Insufficiency and stress fractures of the long bones occurring in patients with rheumatoid arthritis. Radiology. 1975;116:595–9. doi: 10.1148/116.3.595. [DOI] [PubMed] [Google Scholar]
- 11.Dreher R, Buttgereit F, Demary W, Görtz B, Hein G, Kern P, et al. Insufficiency fractures in rheumatology. Case report and overview. Z Rheumatol. 2006;65:417–23. doi: 10.1007/s00393-006-0089-5. [DOI] [PubMed] [Google Scholar]
- 12.Elkayam O, Paran D, Flusser G, Wigler I, Yaron M, Caspi D. Insufficiency fractures in rheumatic patients: Misdiagnosis and underlying characteristics. Clin Exp Rheumatol. 2000;18:369–74. [PubMed] [Google Scholar]
- 13.Nampei A, Hashimoto J, Koynagi J, Ono T, Hashimoto H, Tsumaki N, et al. Characteristics of fracture and related factors in patients with rheumatoid arthritis. Modern Rheumatol. 2008;18(2):170–6. doi: 10.3109/s10165-008-0032-5. [DOI] [PubMed] [Google Scholar]
- 14.Mäenpää HM, Soini I, Lehto MUK, Belt EA. Insufficiency fractures in patients with chronic inflammatory joint diseases. Clin Exp Rheum. 2002;20:77–9. [PubMed] [Google Scholar]
- 15.Vestergaard P, Rejnmark L, Mosekilde L. Methotrexate, azathioprine, cyclosporine, and risk of fracture. Calcif Tissue Int. 2006;79:69–75. doi: 10.1007/s00223-006-0060-0. [DOI] [PubMed] [Google Scholar]
- 16.Sankey RA, Turner J, Lee J, Healy J, Gibbons CE. The use of MRI to detect occult fractures of the proximal femur: A study of 102 consecutive cases over a ten-year period. J Bone Joint Surg Br. 2009;91:1064–8. doi: 10.1302/0301-620X.91B8.21959. [DOI] [PubMed] [Google Scholar]
- 17.Ibfelt EH, Sørensen J, Jensen DV, Dreyer L, Schiøttz-Christensen B, Thygesen PH, et al. Validity and completeness of rheumatoid arthritis diagnoses in the nationwide DANBIO clinical register and the Danish National Patient Registry. Clin Epidemiol. 2017;9:627–32. doi: 10.2147/CLEP.S141438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boer GJ. Fractures in chronic arthritis. Ann Rheum Dis. 1941;2:269–73. doi: 10.1136/ard.2.4.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schapira D, Scharf Y. Insufficiency fracture of the distal tibia mimicking arthritis in a rheumatoid arthritis patient. The possible role of methotrexate treatment. Clinical Exp Rheumatol. 1995;31:130–1. [PubMed] [Google Scholar]
- 20.Van der Bijl AE, Zijlstra TR, Engelage AH, Posthuma BJ, van Veen GJ. [Three patients with a fracture during methotrexate use, possibly due to methotrexate osteopathy]. Ned Tijdschr Geneeskd. 2008;152:2357–60. [PubMed] [Google Scholar]
- 21.Lems WF, Dreinhöfer KE, Bischoff-Ferrari H, Blauth M, Czerwinski E, Silva JAP, et al. EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis. 2017;76:802–10. doi: 10.1136/annrheumdis-2016-210289. [DOI] [PubMed] [Google Scholar]


