Abstract
Introduction
The purpose of this study was to investigate the resumption of endodontic practices in Hubei Province, China 1 month after the end of the lockdown.
Methods
A Web-based survey was sent to 1069 active endodontic specialists and general dentists who provided endodontic care in Hubei Province from May 7 to May 9, 2020. The survey consisted of 18 questions on demographics, the current situation of endodontic practice for the participants, and concerns regarding contracting or spreading the virus in newly opened endodontic practices.
Results
A total of 322 participants completed the survey. Most respondents (62%) were from Wuhan. Almost 83% of the respondents have resumed their endodontic practice partially or fully. Most respondents in practice (99%) would take measures to screen patients before treatment including paid screening measures. More than 93% of the respondents reported having taken special measures for routine endodontic treatment at this stage, with the most common measure taken being wearing an N95 mask. The rubber dam was recognized as efficient in preventing infection by most respondents. Many respondents were concerned about contracting coronavirus disease 2019 (COVID-19) as a result of routine endodontic practice at this stage, and respondents with more than 11 years of endodontic experience were significantly less concerned about infection compared with those with fewer than 5 years of experience (P < .05).
Conclusions
There is a fear of contracting/spreading COVID-19 among endodontic clinicians, the fear is negatively associated with years of practice, and most clinicians believe that rubber dam isolation can protect them and their patients from COVID-19.
Key Words: COVID-19, endodontic practice, pandemic, resuming, survey
Significance.
The endodontic practices are gradually reopening in the COVID-19 hardest-hit area of China. The practitioners are concerned about the possibility of contracting and spreading the virus.
An epidemic coronavirus disease 2019 (COVID-19) caused by a novel coronavirus (severe acute respiratory syndrome–associated coronavirus 2 [SARS-CoV-2]) infection was first reported in Wuhan, the capital city of Hubei Province in China, at the end of December 20191. Since then, it has rapidly spread to other cities of the province, as well as internationally2, and has been declared by the World Health Organization as a pandemic on March 11, 20203. As of May 9, 2020, the Health Commission of Hubei Province reported 50,334 cumulative cases in the city of Wuhan and 68,129 cumulative cases in Hubei4. Besides transmission by inhalation of virus-laden liquid droplets, close contact with infected persons, and contact with surfaces contaminated with SARS-CoV-2, aerosol transmission has been suggested as an additional method of transmission in confined spaces5. A study has found that SARS-CoV-2 could be detected in the air ≈2–3 m from infected patients6. Several endodontic procedures including high-speed drilling with water spray are aerosol-generating7, and endodontic practice, which requires prolonged close face-to-face contact between patients and operators, is regarded as a high risk for cross infection8. In consideration of the risk that dental treatment may pose during the COVID-19 outbreak, the Hubei Province government suspended regular dental treatments including routine endodontic treatments and allowed only emergency treatments during the peak of the pandemic9.
To block the rapid spread of infection and control the epidemic, China has conducted a series of strict measures including redistributing nationwide resources, shelter-in-place orders, quarantining confirmed cases, and locking down the city of Wuhan on January 23, 202010. The lockdown was found to have delayed the arrival of COVID-19 in other cities by 2.91 days, and control measures including suspending intra-public transport, closing entertainment venues, and banning public gatherings were found to be associated with a reduction in case incidence11. The current daily new COVID-19 cases in China have reached a very low level10. On April 8, 2020, the government declared an end of the lockdown in Wuhan. People’s lives gradually returned to normal, and dental services including endodontic practice have also recently resumed. However, because no antiviral treatment for coronavirus infection or vaccine has been proven to be effective until now12 and to resume gradually and safely, several measures are taken by endodontists and general dentists who provide endodontic treatments in Hubei Province. In addition, public health emergencies may negatively impact the mental health of individuals including medical staff13. Thus, the purpose of this study is to investigate the status of endodontic practice in Hubei Province 1 month after the end of the lockdown in Wuhan and the psychological status of endodontists and dentists who conduct endodontic treatments.
Materials and Methods
Survey Design
Approval of the study was obtained from the Ethics Committee of the Wuhan University School of Stomatology before the investigation (project number: 2020B31). A descriptive, cross-sectional survey was generated by using an online crowdsourcing platform WJX (https://www.wjx.cn), which provides functions equivalent to Amazon Mechanical Turk14. The questionnaire contained 3 sections with a total of 18 questions (Supplementary material). The first section consisted of 5 questions regarding the participants’ demographic information, including age, type of endodontic practice, years of experience, the nature of their healthcare facilities, and location. The second section consisted of 8 questions referring to the current situation of endodontic practice for the participants. The third section consisted of 5 questions that assessed the current concerns of the participants regarding virus spreading in the dental office, as well as their view toward the role of rubber dam in the prevention of cross infection during endodontic treatments. The responders who answered “yes” on Question 14 were regarded as healthcare dental providers who volunteered in medical facilities.
Distribution of the Survey
A list of 1069 active endodontic specialists and general dentists who have provided endodontic care in Hubei Province was obtained from the Endodontic Association of School and Hospital of Stomatology, Wuhan University, and 2 online chat groups for endodontic professionals in Hubei Province on social media software (WeChat)15. The questionnaire was distributed via WeChat15 to all members on the list from May 7 to May 9, 2020, one month after the end of the lockdown in Wuhan on April 8, 2020. The study description and invitations to participate were sent to each member 4–5 times per day. Among the completed surveys, those with an answer time of less than 1 minute or more than 15 minutes were deemed unreliable and were excluded16. All participants were assured of complete anonymity to facilitate collecting unbiased data.
Statistical Methods
Data were exported into Microsoft Excel (Microsoft Corp, Redmond, WA) and analyzed with SPSS 23.0 software (SPSS Inc, Chicago, IL). Descriptive statistics were used for analysis. The χ2 and Fisher exact tests were performed to explore the relation between demographic information of respondents and their recognitions on the change of patient numbers compared with the same period of time last year, as well as the important role that rubber dam plays in preventing cross infection with severe acute respiratory syndrome including COVID-19. Generalized linear model with binary logistic regression was performed to explore the factors associated with concerns for infection. Independent variables included age, type of practice, years of practice, type of healthcare facility, location, and participation in COVID-19–related frontline work. The option “Neither agree nor disagree” in Question 16 was excluded from the multivariate logistic regression. All independent variables were entered into multivariable analyses. A P value <.05 was regarded as significant.
Results
A total of 322 participants completed the survey, representing an overall response rate of 30.12%. The demographic data of the respondents are summarized in Table 1 . The respondents were from 15 cities of Hubei Province, and 200 of them (62.11%) came from Wuhan. Of the 322 respondents, 152 (47.20%) were ≤35 years old, 114 (35.40%) were between 36 and 45 years old, 46 (14.29%) were between 46 and 55 years old, and 10 (3.11%) were ≥56 years old. Among these individuals, 26.40% (n = 85) were endodontists, and 73.60% (n = 237) were general dentists who provide endodontic care. Most respondents (n = 125, 38.82%) were from private dental clinics, followed by public dental hospitals (n = 97, 30.12%) and public general hospitals (n = 90, 27.95%). Seventy respondents (21.74%) worked with COVID-19 patients at designated hospitals, fever clinics, and quarantine sites.
Table 1.
Demographic Information of Respondents
| Frequency (n) | Percent (%) | |
|---|---|---|
| Age (y) | ||
| ≤35 | 152 | 47.20 |
| 36–45 | 114 | 35.40 |
| 46–55 | 46 | 14.29 |
| ≥56 | 10 | 3.11 |
| Type of practitioner | ||
| Endodontist | 85 | 26.40 |
| General dentist | 237 | 73.60 |
| Years of practice | ||
| ≤5 | 88 | 27.33 |
| 6–10 | 94 | 29.19 |
| 11–20 | 92 | 28.57 |
| ≥21 | 48 | 14.91 |
| Type of healthcare facility | ||
| Public dental clinic | 97 | 30.12 |
| Dental department of public hospital | 90 | 27.95 |
| Private dental clinic | 125 | 38.82 |
| Dental department of private hospital | 10 | 3.11 |
| Location | ||
| Wuhan | 200 | 62.11 |
| Other cities in Hubei | 122 | 37.89 |
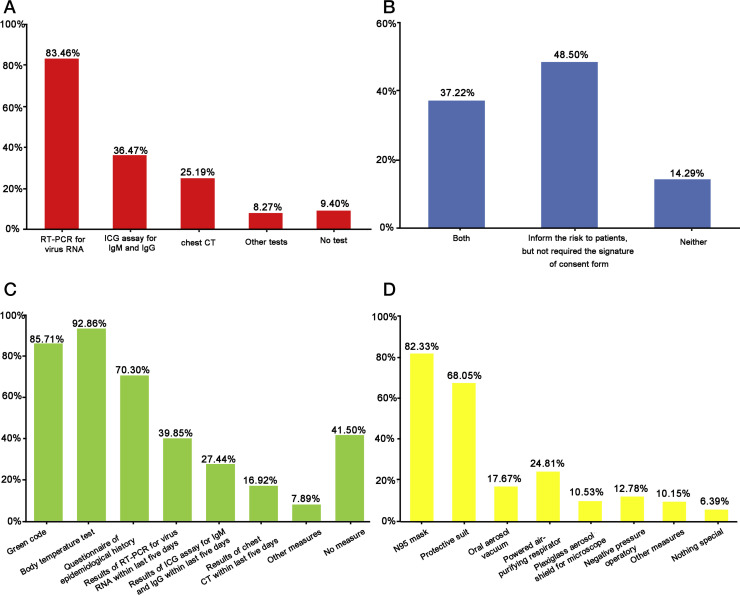
For the current situation of endodontic practice, 82.61% of the respondents (n = 266) had resumed their endodontic practice partially or fully by May 9, 2020. Among respondents who resumed practice, 65.41% of them reported a decrease in the number of patients compared with the same period of time a year ago, especially the responders in Wuhan (Table 2 ), and 90.60% of them (n = 241) have completed COVID-19 tests for themselves to start practicing again. The most common test used was reverse transcriptase polymerase chain reaction (RT-PCR) to detect viral RNA (n = 222, 83.46%) (Fig. 1 A). Most of the respondents (n = 228, 85.72%) would inform patients about the risk of COVID-19 cross infection before endodontic treatment. However, only 37.22% of the respondents (n = 99) required that patients sign an informed consent form (Fig. 1 B). Most of the respondents (n = 262, 98.50%) would take measures to screen patients before treatment, with the most common method being taking body temperature measurements (92.86%), followed by the green code (85.71%) (Supplemental Table S1 for explanation of the green code) (Fig. 1 C). Most respondents have taken paid screening measures (74.44%), including RT-PCR, antibody tests, chest computed tomography (CT) scan, or any other paid screening measures. Only 5.64% of respondents reported uncooperative patients who thought that the paid screening measures were unnecessary. Only 17.29% of respondents reported receiving confirmed or suspected COVID-19 patients who had recovered from COVID-19, confirmed or suspected COVID-19 patients with no symptoms, or patients who have been in close contact with an individual with COVID-19. Besides regular personal protective equipment, 93.61% of the respondents reported having taken special measures for routine endodontic treatment at this stage, with the most common being N95 mask (82.33%), followed by a protective suit (68.05%) (Fig. 1 D).
Table 2.
Chi-Square Tests and Fisher Exact Tests: Influence of the Variables (Age, Type of Practitioner, Years of Practice, Type of Healthcare Facility, and Location) on the Number of Endodontic Patients per Month Compared with That of This Same Period of Time Last Year (Question 7)
| Significant variable | Less (n = 174) | More (n = 60) | Same (n = 32) | P value∗ |
|---|---|---|---|---|
| Location | <.001 | |||
| Wuhan | 127 (77.0) | 27 (16.4) | 11 (6.7) | |
| Other cities in Hubei | 47 (46.5) | 33 (32.7) | 21 (20.8) |
All other variables were not significant.
Figure 1.
Survey results from 266 responders. Graphically illustrated here is the distribution of answers to the questions (A) “What kinds of COVID-19 tests have you completed for yourself to resume practice? (multiple answer question)”; (B) “Did you inform patients of their COVID-19 infection risk and required the signature of informed consent form from patients before endodontic treatment?”; (C) “What kinds of patient screening measures will you take before endodontic treatment at this stage? (multiple answer question)”; (D) “Except standard PPE of gloves, goggles or face shield, mask, and gown, what special measures did you use for routine endodontic treatment? (multiple answer question)”.
According to current concern regarding the possibility of spreading the virus of the participants for endodontic practice, the rubber dam was recognized as an efficient measure for preventing COVID-19 cross infection by most respondents (73.60%), and no significant correlation was observed between the recognition of rubber dam and the demography of the responders (Table 3 ). A total of 225 respondents felt concerned about COVID-19 infection as a result of routine endodontic practice at this stage. Moreover, 198 respondents were concerned about themselves being infected, 196 were concerned about consequently infecting their own families, and 173 were concerned about infecting the patients. No significant differences were observed in concerns about infection depending on age of the dentist, type of endodontic practice, type of healthcare facility, location, and participation in COVID-19–related frontline work (P > .05). Participants with more than 21 years of endodontic experience or 11–20 years of endodontic experience were significantly less concerned about infection compared with those who have practiced for fewer than 5 years (P < .05) (Table 4 ).
Table 3.
Chi-Square Tests and Fisher Exact Tests: Influence of the Variables (Age, Type of Practitioner, Years of Practice, Type of Healthcare Facility, and Location) on the Important Role of Rubber Dam in Preventing Cross Infection with Severe Acute Respiratory Syndrome Including COVID-19 (Question 18)
| Variables | Agree (n = 237) | Do not know (n = 67) | Disagree (n = 18) | P value |
|---|---|---|---|---|
| Age (y) | .087 | |||
| ≤35 | 111 (73.0) | 32 (21.1) | 9 (5.9) | |
| 36–45 | 84 (73.7) | 24 (21.1) | 6 (5.3) | |
| 46–55 | 37 (80.4) | 9 (19.6) | 0 (0.0) | |
| ≥56 | 8 (50.0) | 2 (20.0) | 3 (30.0) | |
| Type of practitioner | .850 | |||
| Endodontist | 64 (75.3) | 16 (18.8) | 5 (5.9) | |
| General dentist | 173 (73.0) | 51 (21.5) | 13 (5.5) | |
| Years of practice | .873 | |||
| ≤5 | 66 (75.0) | 18 (20.5) | 4 (4.5) | |
| 6–10 | 69 (73.4) | 20 (21.3) | 5 (5.3) | |
| 11–20 | 69 (75.0) | 19 (20.7) | 4 (4.3) | |
| ≥21 | 33 (68.8) | 10 (20.8) | 5 (10.4) | |
| Type of healthcare facility | .375 | |||
| Public dental clinic | 76 (78.4) | 17 (17.5) | 4 (4.1) | |
| Dental department of public hospital | 63 (70.0) | 23 (25.6) | 4 (4.4) | |
| Private dental clinic | 91 (72.8) | 26 (20.8) | 8 (6.4) | |
| Dental department of private hospital | 7 (70.0) | 1 (10.0) | 2 (20.0) | |
| Location | .271 | |||
| Wuhan | 153 (76.5) | 36 (18.0) | 11 (5.5) | |
| Other cities in Hubei | 84 (68.9) | 31 (25.4) | 7 (5.7) |
Table 4.
Multivariable Linear Regression: Influence of the Independent Variables (Age, Type of Practitioner, Years of Practice, Type of Healthcare Facility, Location, and Participation in COVID-19 Related Frontline Work) on Concern for Becoming Infected with COVID-19 from Endodontic Practice (Question 16∗)
| Independent variables | Odds ratio | 95% Confidence interval | P value |
|---|---|---|---|
| Age (y) | .051 | ||
| ≤35 | Reference | ||
| 36–45 | 3.07 | (1.32–7.14) | .009 |
| 46–55 | 4.89 | (1.10–21.68) | .037 |
| ≥56 | 4.03 | (0.52–31.26) | .182 |
| Type of practitioner | |||
| Endodontist | Reference | ||
| General dentists | 1.24 | (0.59–2.59) | .566 |
| Years of practice | .035 | ||
| ≤5 | Reference | ||
| 6–10 | 0.68 | (0.32–1.44) | .313 |
| 11–20 | 0.33 | (0.12–0.88) | .027 |
| ≥21 | 0.10 | (0.02–0.50) | .005 |
| Type of healthcare facility | .877 | ||
| Public dental clinic | Reference | ||
| Dental department of public hospital | 0.96 | (0.44–2.13) | .923 |
| Private dental clinic | 1.18 | (0.53–2.66) | .684 |
| Dental department of private hospital | 0.70 | (0.15–3.28) | .647 |
| Location | |||
| Wuhan | Reference | ||
| Other cities in Hubei | 1.08 | (0.60–1.94) | .804 |
| Participation in COVID-19 related frontline work | |||
| Yes | Reference | ||
| No | 0.88 | (0.43–1.81) | .729 |
The bold font indicate the factors with P < .05.
The option B “Neither agree nor disagree” has been excluded from multivariate logistic regression.
Discussion
Although most endodontists and dentists who provide endodontic care have resumed operations since the end of the lockdown, more than half have reported a decrease in the number of patients compared with that of the same period a year ago. In the process of resuming their practice, many dentists including endodontists chose to get tested for COVID-19, with the most common method being RT-PCR. Most respondents would inform patients of the risk of cross infection before endodontic treatment, but only a minority would require that patients sign an informed consent form. Many respondents likely did not require patients to sign an informed consent form out of fear of financial stress as a result of losing patients because patients may end up refusing treatment after reviewing the form.
The diagnosis of COVID-19 is based on clinical features and laboratory tests12. Laboratory tests play an important role in patient screening. Although RT-PCR is widely adopted as a standard method in diagnosing COVID-19, the limitation of this technology is obvious17. Existing PCR methods for detecting SARS-CoV-2 have very good specificity but low sensitivity, meaning that false negatives are common18, and the test is time-consuming, particularly when performed commercially19. The serologic detection method of immunochromatographic (ICG) test for immunoglobulin (Ig) M and IgG antibodies was considered an important supplementary diagnostic approach for SARS-CoV-2–infected patients and could help dentists make a preliminary judgment20. Unlike RT-PCR, assay results could be obtained within 15 minutes with a simple device17. Chest CT scan was also considered to be an important tool for COVID-19 diagnosis with high accuracy19 , 21 and could be used for patients who need urgent dental care. However, its use as a first-line diagnostic tool has been cautioned against by the American College of Radiologists because of its relatively untested specificity22. Recently, a patient with serious dental trauma needing immediate dental treatment was found to be abnormal on chest CT scan imaging in the oral surgery department of one general hospital of Wuhan but tested negative for COVID-19 by a series of diagnostic tests and was eventually excluded of having COVID-19. However, these popular methods are not without limitations. Sharma et al23 suggested using saliva as a noninvasive specimen for the early diagnosis and monitoring of SARS-CoV-2 for endodontists on the basis of previous studies24 , 25.
Several measures have been taken for patient screening, including paid and unpaid measures. Fever was reported to be the most common clinical symptom for patients diagnosed with COVID-1912. Unsurprisingly, taking the body temperature was the most common method of patient screening (92.86%) used by respondents in our study. Another method of screening used by many respondents was green code (85.71%). Green code allows individuals to share their travel history and health status in China via WeChat and Alipay26.
Only 5.64% of the respondents reported uncooperative patients who thought that the paid screening measures used by the dentists or endodontists were unnecessary. Even though the local government has ensured that costs associated with paid screening measures are low enough to allow the general population to afford them and allowed tests such as RT-PCR and ICG to be covered by public medical insurance27, 35.71% of respondents still reported patients who complained about testing costs. Almost one-fifth of the respondents reported receiving confirmed or suspected COVID-19 patients who have recovered after treatment, confirmed or suspected COVID-19 patients with no symptoms, or patients who have been in close contact with an individual with COVID-19, which might result in 93.61% of respondents having taken special protective measures for routine endodontic treatments.
More than half of respondents (69.88%) expressed concerns about becoming infected with COVID-19 as a result of endodontic practice. Outbreaks of infectious diseases, including COVID-19, typically result in widespread fear, anxiety, and a variety of psychological problems16. Some studies have reported on dentists becoming infected through their social contacts9 or dying28; therefore, the risk is legitimate. In this study, only 3 respondents (1.3%) indicated that they were positive on one of the tests, and 2 of them have worked on the frontline during the outbreak. Whether these or dental professionals in other studies became positive as a result of professional exposure is unknown. Nonetheless, professional mental health services should be made available to aid the psychological well-being of the population in highly affected areas including endodontists. Respondents expressed concerns about themselves, their family, and their patients. The importance of rubber dam isolation for helping minimize the production of saliva- and blood-contaminated aerosol or spatter has been emphasized in previous studies7 , 8 and was agreed on by most of the respondents in the present study. No significant difference was observed between endodontists and general dentists on their view toward the role of rubber dam in the prevention of cross infection during endodontic treatments in our study. Because the general dentists surveyed were an intermediary category of dentists with some postgraduate education in and who practiced endodontics, they had similar education background with endodontists.
During the COVID-19 pandemic, the healthcare system was overburdened29, as was the case in Wuhan. Many healthcare workers including dentists and endodontists volunteered to work with COVID-19 patients at designated hospitals, fever clinics, and quarantine sites during the peak of the pandemic30. As of March 24, 2020, the Chinese Stomatological Association31 reported that approximately 288 dentists in Wuhan and 490 dentists in Hubei Province volunteered to work on the frontlines. In our study, 70 respondents (21.74%) admitted having worked on the frontlines. A previous study32 reported that respondents who had worked on the frontlines reported burnout at a lower frequency and were less concerned about being infected than respondents working in wards. The authors proposed that those who worked on the frontlines may have had more experience and knowledge as a result of directly caring for COVID-19 patients, leading to the observed differences in attitudes between the groups. Contrary to those findings, we did not observe such differences in our sample. Instead, a negative correlation was observed between years of practice and concerns about infection. Respondents who have been practicing longer may have felt a greater sense of control associated with more experience. Most of the respondents in this particular study who have been practicing longer are younger than 56. Further studies may be necessary to determine whether the same correlation would be true for older individuals (>65 years old) because old age was widely reported to be associated with a poorer prognosis9.
This study has several limitations. First, the small sample size may produce a clustering effect. Second, although participants were assured of their anonymity, concerns about being identified may have affected their answers32. However, the study found that there is a fear of contracting/spreading COVID-19 among endodontic clinicians, the fear is negatively associated with years of practice, and most clinicians believe that rubber dam isolation can protect them and their patients from COVID-19.
CRediT authorship contribution statement
Jingjing Yu: Data curation, Formal analysis, Funding acquisition, Investigation, Writing – original draft, Revision. Fang Hua: Conceptualization, Data curation, Methodology, Formal analysis, Validation. Ya Shen: Conceptualization, Methodology, Writing – review & editing, Revision. Markus Haapasalo: Validation, Writing – review & editing, Revision. Danchen Qin: Data curation, Formal analysis. Dan Zhao: Conceptualization, Project administration, Resources, Writing – original draft, Supervision, Writing – review & editing, Revision. Bin Peng: Conceptualization, Resources, Validation, Supervision, Writing - review & editing. Ashraf Fouad: Conceptualization, Methodology, Writing – review & editing, Revision.
Acknowledgments
Jingjing Yu and Fang Hua contributed equally to this study.
This work was partly supported by grants from the National Natural Science Foundation of China (grant no. 81901000).
The authors deny any conflicts of interest related to this study.
Footnotes
Supplementary material associated with this article can be found in the online version at www.jendodon.com (10.1016/j.joen.2020.08.001).
Supplementary Material
Supplemental Table S1.
Sample Questionnaire
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The “health code” service–run on the ubiquitous platforms Alipay and WeChat and developed for the Chinese government–give users color-coded designations based on their health status and travel history, and a QR code that can be scanned by authorities. People given a green code are allowed to travel relatively freely.
References
- 1.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang J., Lin G., Zeng J. Challenges of SARS-CoV-2 and lessons learnt from SARS in Guangdong Province, China. J Clin Virol. 2020;126:104341. doi: 10.1016/j.jcv.2020.104341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Coronavirus disease (COVID-19) outbreak situation. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at:
- 4.Health Commission of Hubei Province Epidemic situation of new coronary pneumonia in Hubei Province on May 9, 2020. http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/xxfb/202005/t20200510_2266275.shtml Available at:
- 5.Liu Y., Ning Z., Chen Y. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- 6.Guo Z.D., Wang Z.Y., Zhang S.F. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26:1583–1591. doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samaranayake L.P., Peiris M. Severe acute respiratory syndrome and dentistry: a retrospective view. J Am Dent Assoc. 2004;135:1292–1302. doi: 10.14219/jada.archive.2004.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prati C., Pelliccioni G.A., Sambri V. COVID-19: its impact on dental schools in Italy, clinical problems in endodontic therapy and general considerations. Int Endod J. 2020;53:723–725. doi: 10.1111/iej.13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu J., Zhou J., Yao J. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tian H., Liu Y., Li Y. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiat. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu S.J., Bai X., Fiske S.T. Admired rich or resented rich? how two cultures vary in envy. J Cross Cult Psychol. 2018;49:1114–1143. [Google Scholar]
- 15.Yang Y., Zhou Y., Liu X., Tan J. Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin Oral Invest. 2020;24:1861–1864. doi: 10.1007/s00784-020-03267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu N., Zhang F., Wei C. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiat Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kucirka L.M., Lauer S.A., Laeyendecker O. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Ann Intern Med. 2020:M20–1495. doi: 10.7326/M20-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang S., Peng W., Zhu Y. Recent progress in understanding 2019 novel coronavirus (SARS-CoV-2) associated with human respiratory disease: detection, mechanisms and treatment. Int J Antimicrob Ag. 2020;55:105950. doi: 10.1016/j.ijantimicag.2020.105950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashokka B., Loh M., Tan C.H. Care of the pregnant woman with COVID-19 in labor and delivery: anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am J Obstet Gynecol. 2020;223:66–74. doi: 10.1016/j.ajog.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giudice A., Antonelli A., Bennardo F. To test or not to test? an opportunity to restart dentistry sustainably in “COVID-19 era”. Int Endod J. 2020;53:1020–1021. doi: 10.1111/iej.13324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Z., Shen Y., Wang H. High-resolution computed tomographic imaging disclosing COVID-19 pneumonia: a powerful tool in diagnosis. J Infect. 2020;81:318–356. doi: 10.1016/j.jinf.2020.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu D., Li L., Wu X. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. Am J Roentgenol. 2020;215:127–132. doi: 10.2214/AJR.20.23072. [DOI] [PubMed] [Google Scholar]
- 23.Sharma S., Kumar V., Chawla A., Logani A. Rapid detection of SARS-CoV-2 in saliva: can an endodontist take the lead in point-of-care COVID-19 testing? Int Endod J. 2020;53:1017–1019. doi: 10.1111/iej.13317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.To K.K., Tsang O.T., Yip C.C. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71:841–843. doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabino-Silva R., Jardim A.C.G., Siqueira W.L. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Invest. 2020;24:1619–1621. doi: 10.1007/s00784-020-03248-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kummitha R.K.R. Smart technologies for fighting pandemics: the techno- and human- driven approaches in controlling the virus transmission. Gov Inform Q. 2020:101481. doi: 10.1016/j.giq.2020.101481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Healthcare Security Administration of Hubei Province Hubei: public medical insurance covers COVID-19 tests, including RT-PCR for virus RNA and ICG assay for IgM and IgG. http://ybj.hubei.gov.cn/fbjd/xxgkml/zcwj/gfwj/202005/t20200505_2258711.shtml Available at:
- 28.Ing E.B., Xu Q.A., Salimi A., Torun N. Physician deaths from corona virus (COVID-19) disease. Occupational Medicine. 2020;70:370–374. doi: 10.1093/occmed/kqaa088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ethics Subcommittee of the Council on Ethics, Bylaws, and Judicial Affairs Ethical practice during the COVID-19 pandemic. J Am Dent Assoc. 2020;151:377–378. doi: 10.1016/j.adaj.2020.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feng Z., Cheng Y., Chen J. Chinese medical personnel against the 2019-nCoV. J Infect. 2020;80:578–606. doi: 10.1016/j.jinf.2020.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Data of oral health care personnel who entered Hubei's hot clinics, isolation points and isolation wards. http://www.cndent.com/archives/68391 Available at:
- 32.Wu Y., Wang J., Luo C. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manag. 2020;60:e60–e65. doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]