Abstract
Introduction
In March 2020, the WHO released a Global Research Roadmap in an effort to coordinate and accelerate the global research response to combat COVID-19 based on deliberations of 400 experts across the world. Three months on, the disease and our understanding have both evolved significantly. As we now tackle a pandemic in very different contexts and with increased knowledge, we sought to build on the work of the WHO to gain a more current and global perspective on these initial priorities.
Methods
We undertook a mixed methods study seeking the views of the global research community to (1) assess which of the early WHO roadmap priorities are still most pressing; (2) understand whether they are still valid in different settings, regions or countries; and (3) identify any new emerging priorities.
Results
Thematic analysis of the significant body of combined data shows the WHO roadmap is globally relevant; however, new important priorities have emerged, in particular, pertinent to low and lower middle-income countries (less resourced countries), where health systems are under significant competing pressures. We also found a shift from prioritising vaccine and therapeutic development towards a focus on assessing the effectiveness, risks, benefits and trust in the variety of public health interventions and measures. Our findings also provide insight into temporal nature of these research priorities, highlighting the urgency of research that can only be undertaken within the period of virus transmission, as well as other important research questions but which can be answered outside the transmission period. Both types of studies are key to help combat this pandemic but also importantly to ensure we are better prepared for the future.
Conclusion
We hope these findings will help guide decision-making across the broad research system including the multilateral partners, research funders, public health practitioners, clinicians and civil society.
Keywords: public health, other infection, disease, disorder, or injury, other study design
Key questions.
What is already known?
The WHO produced a roadmap that sets out the research priorities following a meeting in February, just before COVID-19 was declared a pandemic. Now, at this point in the evolution of this novel disease across the world, and almost 6 months later, it is important to assess whether these priorities remain and if research teams in all countries across the globe agree that these are the most important questions that need to be tackled within their healthcare setting and communities, both to mitigate this outbreak and to learn for next time.
What are the new findings?
Over 3000 healthcare workers and researchers contributed to this research and their data tell us that across the globe there has been a shift in priorities and new questions have emerged, particularly from low-resourced settings. For example, there is a strong call for evidence on the relative effectiveness and optimal implementation of public health interventions in varied global settings, for social science studies to guide how to gain public trust and mitigate myths, to understand the impact on already present diseases within communities and to explore the ethics of research within a pandemic.
What do the new findings imply?
The WHO roadmap is globally relevant; however, our findings also provide insight into the temporal nature of these research priorities, highlighting the urgency of research that can only be undertaken within the period of virus transmission, as well as other important research questions but which can be answered outside the transmission period. Both types of studies are key to help combat this pandemic but also importantly to ensure we are better prepared for the future.
Introduction
COVID-19 was declared a public health emergency of international concern on 30 January 20201 and then a global pandemic on 11 March 2020.2 The WHO published their Global Research Roadmap3 on 12 March 2020, within the context of the situation and the epicentre of infection at that time. The Roadmap was built on deliberations of the Global Research Forum, whereby over 400 participants from different sectors across the world identified three to four immediate research priorities for the following 3 months across each of nine themes.
Now, in June 2020, we see the evolution of this pandemic at different points across the globe. We know from our previous experience with Ebola and other outbreaks4 5 that it is essential to embed research into the response to an outbreak, and that there is a finite and unknown window where these questions can be answered. COVID-19 is an unprecedented situation and therefore we must take every opportunity to undertake all the possible research that funding and capabilities allow; and high-quality studies should happen everywhere there are cases in order to maximise the evidence generated and ensure that the resulting data and findings are globally applicable. Therefore, it is important to assess now, what are the most key remaining global health questions that need to be addressed, both to ensure this pandemic can be halted and to learn for future outbreaks of this pathogen or another.
This research intentionally builds from the WHO roadmap, with the aim of strengthening the global health research response effort already aligned to this, rather than generating a completely new set of priorities. Using broad consultative workshops, we have identified additional considerations beyond the WHO roadmap scope in order to broaden the current global research priorities at this point in time to tackle the COVID-19 pandemic and to help learn for any future outbreaks.
Methods
An online multilanguage survey was developed where ranking questions were coupled with open-ended questions. This was based on a previous survey led by the African Academy of Science (AAS) that was undertaken in March 2020 to assess how well the WHO priorities were applicable to Africa.6 Here, we worked from the AAS survey so we could now assess whether the findings remained relevant across the globe, and if they had changed over time. Seventy-three potential priorities (41 from the original WHO document and 32 generated as part the AAS survey and consultations) were arranged under the nine topic headings used in the WHO Research Roadmap. Participants ranked their top three options for both short-term and long-term priorities (18 total ranking questions). Free text boxes were provided under each of the broad topics, where participants were asked to list any research priority they felt was not included in the options provided. Recognising that this survey inherently focused respondents on the existing WHO priority framework, we expanded our consultation through workshops to enable broader discussions of research priorities.
After the survey closed, a virtual workshop was held on the fifth of June to seek wider global comment and discussion on the survey findings and to discuss current priorities and unmet research areas beyond the scope of the existing WHO priority framework. We conducted 10 further open access workshops with research teams and health workers across the globe, led by the The Global Health Network (TGHN) COVID-19 Research Implementation and Knowledge Hub between 14 April and 12 June 2020. These workshop meetings were recorded with permission of participants, and comments and questions captured. A thematic content analysis methodology was developed to report the findings of each.7 Here, we applied this to the cumulative data of all 11 workshops to add to the survey data and better address the question: what are the current global research priorities during the COVID-19 pandemic?
Quantitative data analysis methods
Responses from the survey were downloaded in Excel format, all data were fully anonymised, password protected and access restricted to the study team. Descriptive analyses were undertaken within Excel to provide a ranking score for each research priority for immediate and longer term, as per the survey. Priorities ranked as first were given a score of 3, those ranked second were given a score of 2 and those ranked third were given a score of 1. This analysis was conducted within the category headings from the WHO roadmap and included both the original WHO priorities and new priorities suggested in the AAS report. Therefore, these data show us how responders currently rank the priorities set within the WHO roadmap and the AAS report. The data were split for comparison between the global researcher responses and those originating from less-resourced settings. Within the less-resourced setting category, we include low and lower middle-income countries as defined by the World Bank.
Qualitative data analysis method
The aim of the open-ended survey was to determine whether there are new priorities that were not included in the original WHO roadmap or the AAS survey findings. These written comments were imported into NVivo qualitative data analysis package and we undertook a pragmatic thematic content analysis. Analysing the data from the workshops allowed a further open consideration of current research priorities as this step expanded beyond the limitation that the survey had of asking questions within the framework of the WHO roadmap. Following the methodology established after the first workshop,7 we compiled a dataset by transcribing the spoken and written comments from each workshop. A coding framework was generated through an inductive and then deductive approach, following the same categories used in the survey.
Patient and public involvement
The participants in this study were The Global Health Research and Healthcare community and the very aim was to give them a voice in the requirement to assess whether the right research questions are being tackled in COVID-19. We made ongoing open calls through social media for contributions to surveys and the workshops were open access on TGHN and also on Facebook. The research question was set to address prior lack of engagement with the wider, global community, and the design was based on ongoing engagement with this community and our understanding of how to most effectively engage and gain their involvement. The study was entirely open throughout all the steps and the time taken to complete the survey and taking part in the workshops was made clear to participants.
Results
In total, 1528 individuals completed the online survey and 2559 attended the workshops, from across 137 countries, ensuring representation from all of the WHO regions (African region=612 (40%); American region=279 (18%); Eastern Mediterranean region=32 (2%); European region=460 (30%); South East Asia region=87 (6%); Western Pacific region=58 (4%)). Participants were most commonly employed in academia (47%), hospitals (14%), research organisations (11%) and non-government organisations (10%).
Current global ranking of the WHO roadmap priorities
The survey results (table 1) show how priorities were ranked across the immediate and longer term within the WHO categories. We present these globally, along with a subgroup analysis of less-resourced countries, to understand whether there are differences in priorities for less-resourced countries.
Table 1.
Survey results: top three research priorities from the WHO roadmap categories showing less-resourced countries as a subset of the global responses
| Priority | Immediate | Longer term | |||
| Global (n=1528) | Less-resourced countries (n=694) | Global (n=1528) | Less-resourced countries (n=694) | ||
| Virus natural history, transmission and diagnostics | 1 | Support work to develop cheaper, faster easier to use in field antigen tests (for virus detection) | Support development of diagnostics products to improve clinical processes | ||
| 2 | Support development of diagnostics products to improve clinical processes | Development of cheaper, faster easier to use in field antigen tests (for virus detection) | |||
| 3 | Support work to develop cheaper, faster, easier-to-use in field antibody tests (for determining exposure) | Characterise immunity (naturally acquired, population and vaccine-induced, including mucosal immunity) | Support work to develop cheaper, faster easier to use in field antibody test tests (for determining exposure) | ||
| Animal and environmental research on the virus origin, and management measures at the human–animal interface | 1 | Improve understanding of socioeconomic and behavioural risk factors for spillover and transmission between animals and humans | Identify animal source and route of transmission (hosts, any evidence of continued spillover to humans and transmission between animals and humans) | ||
| 2 | Identify animal source and route of transmission (hosts, any evidence of continued spillover to humans and transmission between animals and humans) | Improve understanding of socioeconomic and behavioural risk factors for spillover and transmission between animals and humans | |||
| 3 | Design and test suitable risk reduction strategies at the human–animal–environment interface | ||||
| Epidemiological studies | 1 | Describe transmission dynamics of COVID-19 and understand spread of disease nationally, regionally and globally | |||
| 2 | Describe disease severity and susceptibility to facilitate effective clinical and public health response to COVID-19— identify groups at high risk of severe infection | Establish suitable cohorts and prospectively collect longitudinal laboratory and outcome data | |||
| 3 | Perform rapid population cross-sectional surveys to establish extent of virus transmission using standardised sampling framework | Describe disease severity and susceptibility to facilitate effective clinical and public health response to COVID-19—identify groups at high risk of severe infection | Perform rapid population cross-sectional surveys to establish extent of virus transmission using standardised sampling framework | ||
| Clinical management | 1 | Determine interventions that improve the clinical outcome of COVID-19-infected patients | Define the natural history of COVID-19 infection through careful standardised and comprehensive clinical and laboratory description of cases | ||
| 2 | Determine optimal clinical practice strategies to improve the processes of care (eg, develop criteria for early diagnosis, when to discharge, when to use adjuvant therapies for patients and contacts) | Determine interventions that improve the clinical outcome of COVID-19-infected patients | |||
| 3 | Develop protocols for management of severe disease in the absence of intensive care facilities | Define the natural history of COVID-19 infection through careful standardised and comprehensive clinical and laboratory description of cases | Determine optimal clinical practice strategies to improve the processes of care (eg, develop criteria for early diagnosis, when to discharge, when to use adjuvant therapies for patients and contacts) | ||
| Infection prevention and control, including healthcare workers’ protection | 1 | Understand the effectiveness of movement control strategies to prevent secondary transmission in healthcare and community settings | |||
| 2 | Optimise the effectiveness of PPE and its use in reducing the risk of transmission in healthcare and community settings | Research to support health systems strengthening and building of resilience post the outbreak | Optimise the effectiveness of PPE and its use in reducing the risk of transmission in healthcare and community settings | ||
| 3 | Develop new PPE approaches using local materials and manufacturing processes | Optimise the effectiveness of PPE and its use in reducing the risk of transmission in healthcare and community settings | Develop new PPE approaches using local materials and manufacturing processes | ||
| Candidate therapeutics R&D | 1 | Develop mechanisms to support coordinated collaboration to implement clinical trials for evaluation of safety/efficacy of therapeutics. | Identification of existing candidates for clinical evaluation in addition to the ones already prioritised | Develop mechanisms to support coordinated collaboration to implement clinical trials for evaluation of safety/efficacy of therapeutics. | Support basic science to identify new drug targets |
| 2 | Support basic science to identify new drug targets | Identification of existing candidates for clinical evaluation in addition to the ones already prioritised | |||
| 3 | Identification of existing candidates for clinical evaluation in addition to the ones already prioritised | Develop mechanisms to support coordinated collaboration to implement clinical trials for evaluation of safety/efficacy of therapeutics | Support basic science to identify new drug targets | Develop mechanisms to support coordinated collaboration to implement clinical trials for evaluation of safety/efficacy of therapeutics | |
| Candidate vaccines R&D | 1 | Develop a multicountry Master Protocol for phase IIb/phase 3 vaccine evaluation to determine whether candidate vaccines are safe and effective before widespread distribution | Capacity development for basic science and preclinical development of new vaccines | ||
| 2 | Capacity development for basic science and preclinical development of new vaccines | Develop a multicountry Master Protocol for phase IIb/phase III vaccine evaluation to determine whether candidate vaccines are safe and effective before widespread distribution | |||
| 3 | Identification of candidates for clinical evaluation in addition to the ones already prioritised. | ||||
| Ethics considerations for research | 1 | Identify key knowledge gaps and research priorities in relation to ethical issues arising out of proposed restrictive public health measures (eg, quarantine, isolation, cordon sanitaire) | |||
| 2 | Define a research governance framework that enables effective and ethical collaboration between multiple stakeholders, including WHO, the global research community, subject matter experts, public health officials, funders and ethicists | ||||
| 3 | Establish processes for speeding up ethical review of COVID-19-related research proposals | Sustained education, access and capacity building to facilitate effective cross-working and collaboration across the research thematic areas | |||
| Social sciences in the outbreak response | 1 | Investigate ways of ensuring transparency of information flow and mitigating false information spread by various mechanisms | Ensure that knowledge is produced according to local, national and regional needs | ||
| 2 | Ensure that knowledge is produced according to local, national and regional needs | Promote the prioritisation of knowledge needs according to epidemic dynamics | |||
| 3 | Examine optimal ways of communicating about potential interventions in high-density low socioeconomic status urban settings | ||||
PPE, personal protective equipment.
The ranking of these priorities broadly indicates what researchers feel to be the most important research areas from the WHO roadmap at this point within this pandemic. The qualitative data from the survey and the workshops then provide further insight to guide where emphasis should be placed and where completely new priorities are relevant, particularly in low-resourced nations.
The qualitative data analysis from the survey, workshops and working groups supported the existing WHO roadmap and highlights where greater research emphasis is needed at this later point in the pandemic. However, most importantly new broader priorities have also come through from this study (table 2).
Table 2.
Existing priorities now requiring greater research emphasis and new priorities not in the WHO roadmap or AAS list (all data from participants working in less-resourced countries apart from those priorities asterisked which originated from participants working in higher income countries)
| Existing priorities now requiring greater research emphasis | |
| Infection recurrence | |
| Understanding infections and outcomes in vulnerable populations including children, persons living with disabilities, ethnic groups | |
| Relationship between repeated viral exposure and disease severity (in frontline workers)** | |
| The effects of the disease on pregnant women | |
| Effective use of PPE for frontline healthcare workers (emphasis on nurses) | |
| Health systems research and strengthening to mitigate impact of COVID-19 on capacity | |
| Understanding zoonotic leap between human and animals | |
| The impact of redirecting resources and public health interventions towards COVID-19 on other disease burdens | |
| Adherence to and trust in public health interventions such as quarantine and social distancing | |
| Evaluation of public health interventions in varied settings | |
| Public health messaging and addressing myths and mistrust | |
| Engaging relevant stakeholders (including religious leaders) in research to enhance community sensitisation, adherence to public health measures, detection and surveillance | |
| Effective and feasible ways of community engagement during lockdowns and social distancing. | |
| New priorities | |
| Virus natural history, transmission and diagnostics | Improved diagnostic tools for safer sample collection, faster and easier assays |
| Epidemiological studies | Examine relationships to other lung diseases. The impact of improved WASH practices on WASH-related infections diseases. Long-term health impacts and complications of contracting COVID-19—with emphasis on children/those with comorbidities. |
| Clinical management | Clinical guidelines for post-hospitalisation home management and community rehabilitation. Palliative care for COVID-19 patients. Vitamin D levels in COVID-19 severity.** |
| Candidate therapeutics R&D | Investigate the potential role of natural/traditional remedies. What would the target therapeutic be with our new knowledge. Evaluate therapeutics in the community in early infection. |
| Candidate vaccines R&D | Innovative vaccine delivery modalities |
| Ethical considerations for research | Ethical considerations for resource allocation to LMICs. Ethical considerations of recruiting final year medical/nursing students. |
| Social sciences in the outbreak response | Understanding COVID-19 in the contexts of conflict, civil war and refugee situations. Examine the effects of the pandemic on the participation of the public in democratic processes. |
| Infection prevention and control | How to ensure effective social distancing in public spaces and congregate settings post lockdown** |
| The environmental impact of the response to COVID-19 | Determine the impact of: Public Health Interventions on the environment (including air pollution and carbon dioxide emissions)
|
| Preparing for the next pandemic | Ensure effective measures including community surveillance and animal screening techniques are in place to rapidly identify emerging zoonotic diseases. Evaluation of governmental policies and lessons learnt in preparation for the next pandemic. |
| Cross-cutting | The use of technology in various aspects of pandemic response. Assess effective ways of conducting cross-disciplinary research. |
All data from low-income countries apart from the three priorities marked as ** which are only from participants from high-income countries.
LMICs, low-and-middle-income countries; PPE, personal protective equipment.
Discussion
These data suggest that that original WHO COVID-19 Research Roadmap remains broadly globally applicable. Here, we also show which research questions require the most emphasis and also that potential new priorities have emerged that were not within the initial roadmap.
Some newly suggested priorities reflect the progress of the pandemic and acquisition of knowledge as to where the gaps lie; notably research in children, pregnancy, long-term health impacts of the disease and that there is a strong call for research that assesses the effectiveness of public health measures put into place across the globe to reduce transmission of this virus. These were alongside a demand for greater social science research to determine public perception, and better ways to change behaviours and build trust (including a need for social sciences to cross-cut the other more biomedical priorities). We also identified a range of new priorities relating to addressing COVID-19 in lower resource settings, where multiple pressures including ongoing endemic infectious diseases and other comorbidities are competing within the health and policy systems for limited resources. These pressures have led to emphasis on cheaper and field applicable tools and research and health capacity strengthening.
The need for further studies to evaluate public health measures and studies on other potential interventions as they arise were ranked highly by the survey respondents and workshop participants. These studies must be undertaken as quickly as possible, in highly varied social contexts, if we are to gain evidence now on just how effective measures such as lockdown, handwashing and social distancing are on reducing transmission and to understand the relative risks and benefits. The need for social science research and mixed methods came through very strongly, with an emphasis on determining how to gain trust and successfully deliver public health messages. This needs evidence-based community engagement strategies; tested and evaluated everywhere.
Limitations of our approach include the fact that we built the questions to align with the original WHO broad priority headings, this would have inherently focused the survey respondents around the largely biomedical focus of these priorities and this meant that some headings (eg, the animal human interface) had relatively few suggested priorities, while others (eg, social sciences in the outbreak response) had much larger numbers. We also retained the original order of priorities from the WHO Research Roadmap and the AAS survey and this may have influenced the ranking given by respondents. The workshops however were open and purposefully invited researchers to make whatever comments they wanted in regard to where current research priorities lie, beyond the scope of the WHO Research Roadmap. Therefore, taken together, we suggest that these data support the importance of the WHO Research Roadmap approach and highlight where funders and researcher should be placing emphasis as well as identifying potential new areas that should be tackled within this pandemic.
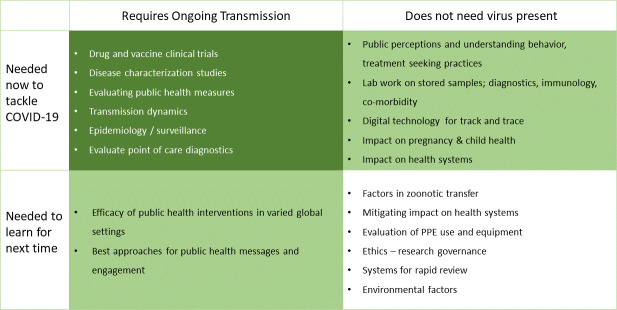
Consideration of both immediate and long-term priorities is important to address this specific pandemic and to better prepare for the future. There are studies that need ongoing transmission, at a high enough rate to answer the question they set. These might be essential for this pandemic, for example, clinical trials to determine the efficacy of drugs or vaccines, or address questions to guide future outbreaks, such as evaluating the effectiveness of public health interventions. Other studies do not need circulating virus and could still guide the effort to address COVID-19 or might help for future pandemics. Figure 1 shows these four situations and gives examples.
Figure 1.
Priority assessment matrix for research within the COVID-19 pandemic. PPE, personal protective equipment.
Consideration of these findings in the context of where we are now with the global shifting and evolution of the pandemic requires both research teams and funders to ensure research across all these key areas within this finite window. This complements ongoing work by the UK Collaborative on Development Research and Global Research Collaboration for Infectious Disease Preparedness to map research funding against the WHO roadmap priorities to enable funders and researchers identify gaps and opportunities, and inform future research investments or coordination needs.8
Finally, we want to highlight both the importance of fully involving the global research community in priority settingand the ongoing need to review priorities where knowledge and practice is advancing rapidly. We recognise that these efforts need to be complemented by further research priority scoping work, beyond the global health focus to further strengthen cross-disciplinary efforts. Here, we have shown that the global health research community supports the recommendations of the WHO Research Roadmap, but that important new priorities have emerged both due to the transition through the pandemic and consideration of differing global epidemiological, health system, policy and research contexts.
Acknowledgments
We acknowledge and thank all survey and workshop participants for their contributions.
Footnotes
Handling editor: Seye Abimbola
Twitter: @thogoto
Contributors: KM, CA, WM, JMA and MA developed the original survey with input from MT; all the authors then contributed to further developing and delivering this global version with oversight from TL. AN and TL guided this analysis along with ADLHG, NC, EA with support from ZA-R and JP. The workshops were delivered by TL and NFdC, with support from ZA-R and JP. TL led the drafting with AN and MT, PP and KM were closely involved throughout and contributed to the draft and review. The other authors contributed significantly and equally in conducting the study and analysing the data. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. TL is responsible for the overall content as guarantor.
Funding: The Global Health Network is supported by a grant from the Bill and Melinda Gates Foundation (https://www.gatesfoundation.org/ Grant number: OPP1169808). The COVID-19 Knowledge hub is supported by a grant from UK Research and Innovation (https://www.ukri.org/ Grant number: MC_PC_19073). AN & MT are employees of UKCDR, which receives funds from BEIS, DHSC, DFID, UKRI and Wellcome for its core activities. No other specific funding supported this work. The funders played no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All researchers are independent from funders, and all authors, external and internal, had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Ethics approval: This research was limited to seeking the views of healthcare professionals and research staff; patients and the wider community were not involved. Therefore, this research would be considered 'minimal risk' and does not come under the definition of research involving human subjects. However, this work does still fall with our research methodology and remit for the protocol that is approved by the University of Oxford Research Ethics Committee (OxTREC) protocol number OxTREC 541-18.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository. All the data from this study will be openly available on the Global Health Network.
Author note: The results from the survey were shared with the community through the ‘research priorities’ workshop and the reports from each workshop are being shared on the platform. The wider, cumulative report is being shared online and the release of that will also be widely disseminated. One of our core aims with this research is to make these findings as widely known as possible so that the prioritise that this work highlights translates to studies undertaken by this same community.
References
- 1. World Health Organization Who director-general's statement on IHR emergency Committee on novel coronavirus (2019-nCoV). Available: https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov)
- 2. World Health Organization Who director-general's opening remarks at the media briefing on COVID-19, 2020. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 [Accessed 11 Jun 2020].
- 3. World Health Organization A coordinated global research roadmap: 2019 novel coronavirus Geneva. Available: https://www.who.int/blueprint/priority-diseases/key-action/Coronavirus_Roadmap_V9.pdf?ua=1 [Accessed 11 Jun 2020].
- 4. Lang T. Ebola: embed research in outbreak response. Nature 2015;524:29–31. 10.1038/524029a [DOI] [PubMed] [Google Scholar]
- 5. Piot P, Soka MJ, Spencer J. Emergent threats: lessons learnt from Ebola. Int Health 2019;11:334–7. 10.1093/inthealth/ihz062 [DOI] [PubMed] [Google Scholar]
- 6. The African Academy of Sciences Research and Development goals for COVID-19 in Africa - The African Academy of Sciences Priority Setting Exercise. Available: https://www.aasciences.africa/sites/default/files/2020-04/Research%20and%20Development%20Goals%20for%20COVID-19%20in%20Africa.pdf [Accessed 11 Jun 2020].
- 7. Tibenderana J, Alia J, Hamade P, et al. Malaria and COVID-19: a rapid determination of unknowns and call for research, 2020. [Google Scholar]
- 8. The UK Collaborative on Development Research COVID-19 Research Project Tracker by UKCDR & GloPID-R, 2020. https://www.ukcdr.org.uk/funding-landscape/covid-19-research-project-tracker/ [Google Scholar]