Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic placed unprecedented pressure on various healthcare systems, including departments that use immunotherapies such as chimeric antigen receptor (CAR) T-cell therapy and immunosuppression therapy in organ transplantation units. The true impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection on immunocompromised CAR T-cell therapy recipients and kidney transplant recipients (KTRs) has not yet been established.
Case presentation
In this report, we compare two patients with severe COVID-19 pneumonia in either the humoral or cell-mediated immunodeficient states. The first patient was a man in his early 30s who was diagnosed with refractory multiple myeloma. He received fully humanized, anti-B-cell maturation antigen, CAR T-cell therapy before 4 months and achieved strict complete remission. He was infected with SARS-CoV-2 starting on January 26, 2019 and gradually progressed to severe pneumonia. Throughout the clinical progression of the disease, SARS-CoV-2 could not be cleared due to his humoral immunodeficient state. During this period of his severe COVID-19 pneumonia, elevated cytotoxic T-cells were observed in this patient’s peripheral blood while elevated plasma levels of interleukin (IL)-2R, IL-6, tumor necrosis factor α, and ferritin were observed in his cytokine profiles. This patient eventually progressed into acute respiratory distress syndrome and recieved non-invasive ventilatory support. He failed to generate specific SARS-CoV-2 antibodies and died of respiratory failure on day 33 (d33). The second patient was a 52-year-old kidney transplant recipient (KTR) who took ciclosporin after renal transplantation for more than 7 years. He confirmed SARS-CoV-2 infection on January 20, 2019 and gradually progressed into severe pneumonia on d16 with a slightly elevated B-cell percentage and normal T-lymphocyte subsets. Viral clearance occurred together with the generation of specific anti-immunoglobulin G-SARS-CoV-2 antibodies after 2 weeks of treatment. He was symptom-free and discharged from the hospital on d42.
Conclusion
We report a CAR T-cell therapy recipient diagnosed with COVID-19 for the first time. His virus clearance failure and life-threating cytokine storm during SARS-CoV-2 infection suggested that any decision to proceed CAR T-cell therapy during COVID-19 pandemics will require extensive discussion of potential risks and benefits. Immunosuppressant treatment based on ciclosporin could be relatively safe for KTRs diagnosed with COVID-19.
Trial registration number
ChiCTR-OPN-1800018137.
Keywords: immunotherapy, adoptive; immunity, humoral; immunity, cellular; receptors, chimeric antigen
Introduction
In December 2019, a cluster of acute respiratory illness, caused by a novel coronavirus pneumonia, occurred in Wuhan, Hubei Province, China.1 It has spread globally and has been declared a pandemic by the WHO.2 This outbreak was confirmed to be caused due to an infection with a novel coronavirus, namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the same family of viruses responsible for severe acute respiratory syndrome (SARS).3 Coronavirus disease 2019 (COVID-19) is a heterogeneous disease population, of which most patients exhibit mild to moderate symptoms, however approximately 15% progress to severe pneumonia, while 5% were eventually admitted to intensive care units (ICU) due to the resultant acute respiratory distress syndrome (ARDS), septic shock and/or multiple organ failure.4 One of the current research focuses is on preventing the progression of this disease into the critical stage in patients suffering from severe pneumonia, since this is what has led to the high mortality associated with this infection.4 Aberrant immune responses, also referred to as a ‘cytokine storm’, is featured in severe SARS-CoV-2 infection, and proposed as being associated with an inferior clinical prognosis, severe ARDS and also lethal multiple organ dysfunction syndrome.5 6 Once patients developed ARDS, more than half of them eventually died.7 It is hypothesized that SARS-CoV-2 infection in immunocompromised patients place them within the high-risk group more likely to encounter severe outcomes from COVID-19. However, COVID-19 patients with underlying hematological malignancies, receiving chimeric antigen receptor (CAR) T-cell therapy, were not yet reported.
CAR T-cell therapy is an innovative form of adoptive cell therapy that has revolutionized the treatment of certain hematological malignancies.8 B-cell maturation antigen (BCMA), a highly plasma cell-selective protein expressed on malignant plasma cells of patients with multiple myeloma (MM), has appeared as a promising antigen to target, using a variety of immunotherapy treatments including CAR T-cells, for MM patients.9 It will likely result in increased acquired deficiencies in humoral immunity and subsequent infections in persons with cancer. Unlike CAR T-cell immunotherapy, the utilization of mycophenolate mofetil with calcineurin inhibitors (ciclosporin and/or tacrolimus) in kidney transplant recipients (KTRs) has led to a significant improvement in graft survival.10 Its molecular mechanism of action has been well defined in T-cells and involved in the inhibition of critical signaling pathways that regulated T-cell activation.11 It was suggested that if these immunocompromised individuals were infected with SARS-CoV-2, it would be more likely for them to progress into the severe or critical disease stages due to their impaired host immunity. However, the role of host immunity in an immunocompromised individual with the SARS-CoV-2 pathogenesis of COVID-19 remains unclear and needs to be evaluated further.
Here we report on two patients with severe COVID-19 pneumonia, who had an underlying deficiency in either humoral (CAR T-cell recipient) or cell-mediated immunity (KTR). The two patients had dramatically different courses of disease, with the first succumbing to pneumonia and cytokine release syndrome, while the second patient went on to recover. The true impact on immunocompromised CAR T-cell recipients and KTRs with SARS-CoV-2 infection has not previously been evaluated. Our findings may contribute to additional information on COVID-19 patients in different immunocompromised states.
Case presentation
This study retrospectively evaluated two cases of COVID-19, hospitalized in Tongji Hospital, Wuhan, China by comparing the demographic, clinical, laboratory, treatment, and outcome data. The diagnosis and illness severity of COVID-19 was re-defined according to the Chinese Management Guidelines for COVID-19 (V.7.0).12 According to the guidelines, the clinical classifications of COVID-19 are as follows. (1) Mild: the clinical symptoms were mild, and there were no imaging features of pneumonia. (2) General: there were fever, respiratory symptoms, as well as imaging features of pneumonia. (3) Severe: meeting any of the following: respiratory distress, respiratory rates ≥30 breaths/min; the oxygen saturation ≤93% at rest state; partial pressure of oxygen in arterial blood (PaO2)/fraction of inspired oxygen (FiO2) ≤300 mm Hg (1 mm Hg=0.133 kPa). (4) Critically ill: meeting any of the following items: respiratory failure needing mechanical ventilation; shock; being complicated with other organ failures needing ICU monitoring and treatment. Case 1 was a patient with refractory MM post-cellular immunotherapy (CAR T-cell therapy). Case 2 was a patient who had undergone a kidney transplantation. The first day of symptom onset has been defined as day 1 (d1).
COVID-19 patient with humoral immunity defect (CAR T-cell recipient)
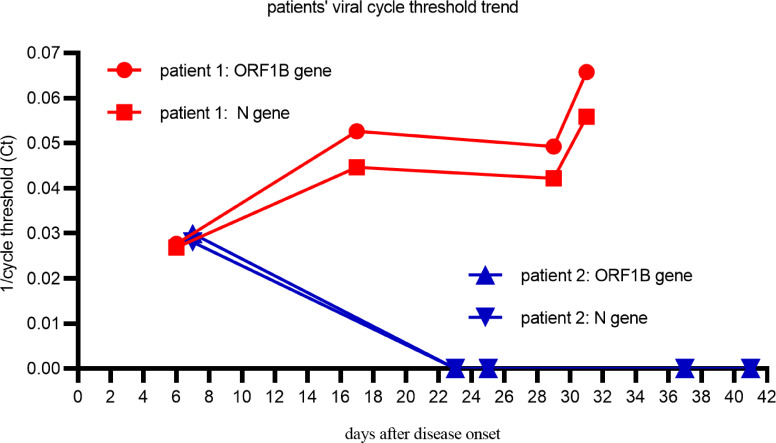
Patient 1 (figure 1A) was a man in his early 30s with a history of refractory MM for more than 2 years. The patient was enrolled in a clinical trial and received fully humanized, anti-BCMA, CAR T-cell therapy in October 2019. He was conditioned with a standard lympho-depleting chemotherapy regimen, consisting of fludarabine (25 mg/m2) and cyclophosphamide (20 mg/kg) for consecutive 3 days. The sequential infusion of anti-BCMA CAR T-cells was performed with a total dosage of 0.5×106 cells/kg of CAR T-cells. He achieved strict complete remission (CR) after 30 days of initial infusion. The patient maintained follow-up and showed continued CR together with the persistence of CAR T-cells (online supplementary figure S1). He was symptom-free and no evidence of other pathogenic infections could be found prior to his SARS-CoV-2 infection. The patient presented to the fever clinic with a dry cough and fever (38.5°C) on January 26, 2019 (d1). He was found to be positive for SARS-CoV-2 nucleic acid on d5 and was immediately hospitalized in isolation. Once hospitalized, he received nasal cannula oxygen therapy (3 L/min) and maintained an oxygen saturation (SpO2) level between 96% and 99% during this therapy. He was prescribed 200 mg Arbidol (umifenovir) three times per day, 500 mg lopinavir/ritonavir two times per day and 400 mg moxifloxacin once per day, however his symptoms were aggravated. His chest CT showed bilateral pulmonary infiltration with consolidation (figure 1B). During the severe pneumonia state, the patient showed elevated levels of interleukin (IL)-2R, IL-6, tumor necrosis factor α (TNF-α), and ferritin in his plasma cytokine profiles (table 1). He also exhibited an absence of B-lymphocytes and elevated cytotoxic T-cells in his peripheral blood (table 1). He was supplemented with 20 g intravenously immunoglobulin (IVIG) for 3 days followed by a once per week regimen of IVIG supplementation. A chest CT on d18 showed prominent progression of the pulmonary infiltration together with consolidation and the patient gradually developed ARDS (figure 1B). He was then transferred to the ICU and given high-flow oxygen therapy (100% concentration, flow rate 60 L/min) with intravenous corticosteroids (methylprednisolone 40–120 mg for 10 days) due to his shortness of breath and hypoxemia. Intravenous administration of 3 g cefoperazone/sulbactam every 12 hours, 400 mg teicoplanin once per day and 200 mg voriconazole every 12 hours was commenced to prevent secondary infections. At this stage, the patient was not able to maintain blood oxygen saturation levels, received biphasic positive airway pressure (BiPAP) ventilation, and refused to undergo mechanical ventilation. Although the elevated IL-6, IL-2R, and TNF-α levels were reduced after the use of methylprednisolone, the ferritin continued to increase (table 1). Multiple repeated swab tests (on d17, d29, and d31) showed a reduced cycle threshold value, suggesting that the high viral load correlated with the clinical progression experienced in this patient (figure 2, online supplementary table S1). The anti-SARS-CoV-2 immunoglobulin G (IgG) and IgM could not be detected in this patient. He eventually died of respiratory failure on d33.
Figure 1.
(A) Timeline of disease course and key clinical information from the first day of swab tests to death (patient 1). (B) Case 1 had chest CT progression on day 18 since the symptom onset. (C) Timeline of disease course and key clinical information from the first day of swab tests to the days of hospitalization charge (patient 2). (D) Case 2 had gradual absorbance of bilateral focal ground glass-like lung lesions with symptoms improvement. CAR T, chimeric antigen receptor T cells; COVID-19, coronavirus disease 2019; iv, intravenous; IL, interleukin; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Table 1.
Summary of clinical and laboratory examination results of two cases with SARS-CoV-2 infection
| Case | 1 | 2 |
| Sex/age | M/in his early 30s | M/52 |
| Primary disease | Multiple myeloma | Chronic kidney disease |
| Prior treatment/date | Anti-BCMA-CAR T 2019/10 |
Kidney transplantation 2013/06 |
| Symptoms onset time | January 26 | January 20 |
| Main symptoms | Fever, dry cough | Fever, sore throat, and dry cough |
| First swab time/results* | January 30 (+) | January 27 (+) |
| CRP at disease onset (mg/L) | 11 | – |
| WBC/LYM at disease onset (×109/L) | 3.14/1.42 | 4.67/0.38 |
| COVID-19 clinical classification† | Moderate to severe to critical | Moderate to severe |
| Cytokine profiles and lymphocyte subsets in severe status | ||
| IL-1β (range: <5.0 pg/mL) | <5.0 | <5.0 |
| IL-2R (range: 223–710 U/mL) | 903 ↑ | 670 |
| IL-6 (range: <7.0 pg/mL) | 87.51 ↑ | 2.82 |
| IL-8 (range: <62 pg/mL) | <5.0 | 12.4 |
| IL-10 (range: <9.1 pg/mL) | <5.0 | <5.0 |
| TNF-α (range: <8.1 pg/mL) | 17.6 ↑ | 6.7 |
| Ferritin (range: 30–400 µg/L) | 10308 ↑ | 2534 ↑ |
| Lymphocyte subsets‡ | ||
| T Lymphocytes (CD3 +CD19−) (range: 27%–51%) |
84.43% ↑ | 65.6% ↑ |
| Helper T cell: CD3 +CD4+ (%) (range: 27%–51%) |
7.74% | 47.37% |
| Cytotoxic T cell: CD3 +CD8+ (%) (range: 15%–44%) |
76.56% ↑ | 16.40% |
| B Lymphocytes (CD3−CD19+) (range: 5%–18%) |
0% ↓ | 24.5% ↑ |
| Anti-SARS-CoV-2-IgG (AU/mL)§ | (−) 0.48 | (+) 41.51 |
| Anti-SARS-CoV-2-IgM (AU/mL)§ | (−) 2.97 | (−) 7.54 |
*RNA was extracted from oropharyngeal swabs of patients using the respiratory sample RNA isolation kit (Xi’an Tianlong Science and Technology Co., China). The reverse-transcription PCR assay (Shanghai Huirui Biotechnology Co., China) of SARS-CoV-2 RNA was conducted to amplify and test two target genes including open reading frame 1ab and nucleocapsid protein. Patients with the cycle threshold value greater than 40 were categorized as positive for the virus.
†Clinical classification is re-defined according to the seventh version of New Coronavirus Pneumonia Prevention and Control Program issued by the Chinese National Health Commission.
‡Lymphocyte subsets in peripheral blood were assessed by flow cytometry.
§Serological detection of anti-SARS-CoV-2-IgG/IgM was performed by chemiluminescence immunoassay kit (YHLO BIOTECH, China); <10.00 AU/mL was categorized as negative results; ≥10.00 AU/mL was categorized as positive results.
BCMA, B-cell maturation antigen; CAR T, chimeric antigen receptor T cells; COVID-19, coronavirus disease 2019; CRP, C-reactive protein; Ig, immunoglobulin; IL, interleukin; LYM, lymphocyte; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TNF-α, tumor necrosis factor α; WBC, white blood cell.
Figure 2.
Patients’ viral cycle threshold trend. Red: patient 1; blue: patient 2.
jitc-2020-000862supp001.pdf (209.7KB, pdf)
COVID-19 patient with cell-mediated immunity defect (KTR)
Patient 2 (figure 1C) was a 52-year-old man with a history of chronic kidney disease for many years. He received a kidney transplantation 7 years ago. After his renal transplant, he was prescribed 50–75 mg ciclosporin, two times per day for 7 years with doses adjusted to attain target trough concentrations; the target trough levels of ciclosporin during the first 3 months were 300–400 ng/mL, with reduction to 250–300 ng/mL until 6 months, 200–250 ng/mL until 1 year and 150–200 ng/mL after 1 year. His serum creatinine and blood urea nitrogen were within the normal ranges. He was asymptomatic with no evidence of other pathogenic infections prior to the SARS-CoV-2 infection. The patient presented to the fever clinic with a fever (38.6°C), sore throat, and dry cough starting on January 20, 2019 (d1). He was diagnosed with general type of COVID-19 on d7. He then received treatment consisting of 200 mg Arbidol (umifenovir), three times per day and 400 mg moxifloxacin once per day for 7 days as per the triage strategy.13 He was admitted to hospital on d12 when he presented with shortness of breath and SpO2 level between 90% and 93%. His chest CT on d13 showed bilateral ground-glass opacities compatible with viral pneumonia (figure 1D). After admission, the patient received nasal cannula oxygen therapy (3–5 L/h). He also received 40 mg intravenous methylprednisolone for 10 days and 3 g cefoperazone/sulbactam every 12 hours. During the severe stage, his plasma cytokine profiles, including IL-1β, IL-2R, IL-8, IL-10, and TNF-α, remained within normal range (table 1). Although initially elevated, IL-6 and ferritin levels gradually decreased after the use of methylprednisolone. Flow cytometry for lymphocyte subsets showed a slightly elevated B-cell percentage, with normal T-lymphocyte subsets. The patient exhibited significant symptom reduction, as well as chest CT improvement (figure 1D) after treatment. Swab tests for SARS-CoV-2 RNA were negative from d23 and remained negative following repeated tests, indicating clearance of the virus (figure 2, online supplementary table S1). The specific anti-SARS-CoV-2 IgG antibodies were detected at the recovery stage (table 1). The patient was symptom-free and discharged from the hospital on d42.
Discussion
Numerous clinical data have shown that patients with COVID-19 develop severe hypoxia and ARDS after 7–10 days of initial diagnosis, and their symptoms may deteriorate quickly in these patients, even when treated in ICU or in other significant life-support treatments.14 The pathogenesis for pathogenic human coronaviruses is often associated with rapid virus replication and elevated proinflammatory cytokine/chemokine responses, resulting in acute lung injury and ARDS.15 Although clinical similarity and the overexuberant inflammatory response was expected when comparing SARS and COVID-19, particularly in severe and fatal cases,5 14 the exact pathogenesis of the severe pneumonia caused by SARS-CoV2 remains unclear. COVID-19 poses increased risk in cancer patients, especially in those who have recently undergone chemotherapy, radiotherapy, or immunotherapy treatments. The dysfunction of the host immune response complicates the clinical course and can lead to the deterioration of COVID-19 patients.
To our knowledge, this is the first report to depict the clinical course of a CAR T-cell therapy recipient with severe COVID-19 pneumonia and it is also the first occasion where the potential mechanisms involved in the severe pneumonia experienced in COVID-19 patients, after CAR T-cell therapy and kidney transplantation, are compared. The studies on these two cases elucidate the potential role of host immunity in critical cases. The treatment of MM has entered into a new era of immunotherapy. Novel immunotherapies, including CAR T-cell therapy, has significantly improved these patients’ outcomes.16 BCMA, selectively expressed in plasma, is highly expressed in MM cells during all stages. Recently, the BCMA CAR T-cell therapies have shown great potential to improve the treatment landscape for refractory MM, for deep and durable responses.16 In our first patient, after CAR T-cell therapy, aplasia of plasma cells and B-cells was accomplished for an extended duration, with the persistence of CAR T-cells (online supplementary figure S1). If the SARS-CoV-2 virus is successful in establishing an infection, successful clearance of the virus requires adaptive immunity. This patient was not able to clear the virus with the usual host immune response and was not able to generate antibodies for SARS-CoV-2, thus demonstrating that a humoral immune response is vital for virus clearance. At a later stage, host inflammatory response becomes a major cause of lung damage and subsequent mortality. Overactivation of T-cells with a high degree of cytotoxicity such as CD8+ T-cells17 and/or macrophages18 in diffuse lung tissues, such as in patient 1, accounts for the severe immune injury in patients with COVID-19. In critically ill patients, the overwhelming inflammation and cytokine-related lung injury may cause rapidly progressive pneumonia.19 In patient 1, elevated plasma IL-6, IL-2R, and TNF-α levels were suppressed by using a corticosteroid. The pathogenesis of the persistently elevated ferritin, which is associated with a higher risk of poor outcome in hospitalized patients with influenza infections,20 has not yet been reported in COVID-19 studies. Pathophysiological mechanism underlying high ferritin levels are not fully understood, though it may be indicative of a potential cytokine storm or results of the activated macrophage system.21 In current clinical practice, the prognosis of COVID-19 patients with a HIV coinfection, thus having a degree of CD4+ T-cell dysfunction, was generally favorable,22 with cases seldom progressing into the critical stage. As for case 2, after kidney transplantation, the long-term oral intake of a calcineurin inhibitor (ciclosporin) inhibits critical signaling pathways that regulate T-cell activation. In the severe state, the lack of cytokine release syndrome in patient 2 is likely tied to global immunosuppression and specific inhibition of T-cell responses. Furthermore, the patient’s humoral immunity, which was supposed to be partially affected by ciclosporin, assisted in early virus clearance. The serology tests, though exhibiting a relatively lower titer than in COVID-19 patients with non-impaired immune function, confirmed our hypothesis.
This small case study has several important clinical implications: first, together with our previous report of fatal HBV reactivation and clearance failure post anti-CD19/22 CAR T-cell therapy,23 we confirmed that the absence of humoral immunity can lead to a fatal virus clearance failure and aberrant T-cell activation. As the global COVID-19 pandemic continues, any decision to proceed with immunotherapy such as CAR T-cell therapy or anti-CD20-targeted therapy will require extensive discussion around the potential risks and benefits.24 Special consideration should be given to the potentially fatal failure of virus clearance after CAR T-cell therapy. On the contrary, our second case, together with a recently published paper, indicated that immunosuppressant treatment, based around ciclosporin, could be safe and effective for KTRs diagnosed with COVID-19.25 Although we cannot draw any definitive conclusion from our observation, this small case study may provide critical clues on the role of host immunity in the aggravation of COVID-19-related respiratory symptoms and should serve as a cautious warning for patients after receiving CAR T-cell therapy in the era of COVID-19.
Acknowledgments
We thank LetPub (www.letpub.com) and Jehane Michael Le Grange for their linguistic assistance during the preparation and revision of this manuscript.
Footnotes
Contributors: JW analyzed the data and wrote the manuscript. FM, JZ, MH, and JZ managed the patients. FM revised the manuscript and was in charge of the final approval of the manuscript. All authors read and approved the final manuscript.
Funding: This work is supported by the National Natural Science Foundation of China (81873427, to Dr. JW).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Medical Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology and in accordance with the Declaration of Helsinki. Written informed consent was obtained from the patients for treatment. The CAR T clinical trial for first patient was registered at www.chictr.org.cn as ChiCTR-OPN-1800018137.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med Overseas Ed 2020;382:727–33. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mahase E. Covid-19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. BMJ 2020;368:m1036. 10.1136/bmj.m1036 [DOI] [PubMed] [Google Scholar]
- 3. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565–74. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stebbing J, Phelan A, Griffin I, et al. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect Dis 2020;20:400–2. 10.1016/S1473-3099(20)30132-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol 2020;20:269–70. 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020. 10.1001/jamainternmed.2020.0994. [Epub ahead of print: 13 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Roex G, Feys T, Beguin Y, et al. Chimeric antigen receptor-T-cell therapy for B-cell hematological malignancies: an update of the pivotal clinical trial data. Pharmaceutics 2020;12:194. 10.3390/pharmaceutics12020194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Perez-Amill L, Suñe G, Antoñana-Vildosola A, et al. Preclinical development of a humanized chimeric antigen receptor against B cell maturation antigen for multiple myeloma. Haematologica 2020:haematol.2019.228577 10.3324/haematol.2019.228577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nakamura K, Oshima S, Maeda M, et al. Replacement of mycophenolate mofetil with a JAK inhibitor, AS2553627, in combination with low-dose tacrolimus, for renal allograft rejection in non-human primates. Int Immunopharmacol 2018;64:201–7. 10.1016/j.intimp.2018.08.029 [DOI] [PubMed] [Google Scholar]
- 11. Rezzani R. Cyclosporine A and adverse effects on organs: histochemical studies. Prog Histochem Cytochem 2004;39:85–128. 10.1016/j.proghi.2004.04.001 [DOI] [PubMed] [Google Scholar]
- 12. China National Health Commission Diagnosis and treatment of pneumonitis caused by new coronavirus (trial version 7). Beijing: China National Health Commission, 2020. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml [Google Scholar]
- 13. Zhang J, Zhou L, Yang Y, et al. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir Med 2020;8:e11–12. 10.1016/S2213-2600(20)30071-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol 2017;39:529–39. 10.1007/s00281-017-0629-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shah N, Chari A, Scott E, et al. B-Cell maturation antigen (BCMA) in multiple myeloma: rationale for targeting and current therapeutic approaches. Leukemia 2020;34:985–1005. 10.1038/s41375-020-0734-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020;8:420–2. 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carsana L, Sonzogni A, Nasr A, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis 2020. 10.1016/S1473-3099(20)30434-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shang L, Zhao J, Hu Y, et al. On the use of corticosteroids for 2019-nCoV pneumonia. The Lancet 2020;395:683–4. 10.1016/S0140-6736(20)30361-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lalueza A, Ayuso B, Arrieta E, et al. Elevation of serum ferritin levels for predicting a poor outcome in hospitalized patients with influenza infection. Clin Microbiol Infect 2020. 10.1016/j.cmi.2020.02.018. [Epub ahead of print: 28 Feb 2020]. [DOI] [PubMed] [Google Scholar]
- 21. Bataille S, Pedinielli N, Bergounioux J-P. Could ferritin help the screening for COVID-19 in hemodialysis patients? Kidney Int 2020;98:235–6. 10.1016/j.kint.2020.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blanco JL, Ambrosioni J, Garcia F, et al. COVID-19 in patients with HIV: clinical case series. Lancet HIV 2020;7:e314–6. 10.1016/S2352-3018(20)30111-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wei J, Zhu X, Mao X, et al. Severe early hepatitis B reactivation in a patient receiving anti-CD19 and anti-CD22 CAR T cells for the treatment of diffuse large B-cell lymphoma. J Immunother Cancer 2019;7:315 10.1186/s40425-019-0790-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bachanova V, Bishop MR, Dahi P, et al. Chimeric antigen receptor T cell therapy during the COVID-19 pandemic. Biol Blood Marrow Transplant 2020;26:1239–46. 10.1016/j.bbmt.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodriguez‐Cubillo B, Moreno de la Higuera MA, Lucena R, et al. Should cyclosporine be useful in renal transplant recipients affected by SARS‐CoV‐2? Am J Transplant. 2020 doi: 10.1111/ajt.16141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2020-000862supp001.pdf (209.7KB, pdf)