Abstract
Botulinum neurotoxin is widely used for the treatment of central and peripherical neurological conditions. Initially used to treat strabismus, over the years its use has been expanded also to spasticity and other neurological disorders. This review summarizes the evidence from the published literature regarding its effect on neuropathic pain. Almost all investigations were performed using onabotulinum toxin type A (BoNT/A). Most studies provided positive results, even though toxin formulation, dose, dilution, injection techniques, and sites are heterogeneous across studies. Future larger, high-quality, specifically designed clinical trials are warranted to confirm botulinum neurotoxin efficacy in neuropathic pain.
Keywords: botulinum toxin, neuropathic pain, pain treatments, visual analog scale, disability
Introduction
Neuropathic pain (NP) is a pain caused by a lesion or a disease affecting the somatosensory nervous system and encompasses common neurological pain syndromes such as trigeminal neuralgia (TN), postherpetic neuralgia (PHN), diabetic neuropathic pain (DN), and postsurgical neuralgia.
NP is caused by pathological changes involving the peripheral (nerves, plexus, roots, and sensitive ganglia) and the central nervous system (CNS). The pathologies responsible for tissue specific symptoms of NP comprise viral infections (e.g., herpes simplex, varicella zoster, and human immunodeficiency virus), metabolic disorders with mitochondrial dysfunctions (e.g., diabetes), stroke, mechanical injuries to the CNS or peripheral nerves (1, 2), and toxic effects, above all anti-neoplastic compounds (e.g., oxaliplatin, vincristine) (3).
Nociceptor activation is one of the most relevant NP peripheral mechanism, causing abnormal neuronal hyperexcitability, hyperalgesia, and allodynia (4–6).
Nociceptors consist of free nerve endings related to unmyelinated C-fibers and small-myelinated Aδ-fibers; they are activated by different mechanical, thermal, and chemical stimuli and a variety of endogenous substances [e.g., substance P (SP), bradykinin, serotonin, calcitonin gene-related peptide (CGRP), prostaglandins, excitatory amino acids histamine, growth factors, and proinflammatory cytokines] (4–6). Increased nociceptor excitability due to nerve injury causes glutamate-mediated pronociceptive activation and a decrease in inhibitory influences. Primary nociceptive Aδ- and C-fibers terminate at two distinct types of spinal second-order neurons, i.e., spinal neurons projecting to higher neuronal structures, and spinal interneurons modulating synaptic transmission in the dorsal horn where resident microglial activation plays also a key role (7). Glutamate participates in the transmission of nociceptive inputs from the periphery to the brain by binding to α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), N-Methyl-D-Aspartate (NMDA), and metabotrobic (mGluR) receptors. The glutamate pathway mediates basic responses to nociceptive stimuli and contributes to the spinal dorsal horn hyperexcitability, manifesting with synaptic plasticity, and long-term potentiation (6–8).
The activity of second-order neurons is modulated by the descending brainstem inhibitory noradrenergic, serotonergic, and opiatergic pathways, spinal GABAergic and glycine inhibitory inputs, as well as by the cannabinoid system (8–10).
Current pharmacological and non-pharmacological treatment of NP is still unsatisfactory (9, 11, 12). Besides lidocaine, capsaicin, antidepressants, anticonvulsants, and opioids, botulinum toxin (BoNT) has more recently emerged as a promising NP therapeutic strategy (13, 14). The first evidence of BoNT efficacy in NP in humans dates back to 2001 when Freund and Schwartz (15) described seven patients with postherpetic neuralgia (PHN) treated for >6 months with subcutaneous BoNT injections at 38th Interagency Botulism Research Coordinating Committee Meeting (15). Currently, the use of BoNT is considered for NP whenever common pharmacological agents have been ineffective (16).
BoNT is a potent neurotoxin produced by Clostridium botulinum, which blocks acetylcholine release at neuromuscular junctions causing muscle relaxation. The mechanism of action of BoNT in NP is related to the inhibition of the release of neurotransmitters and neuropeptides involved in pain mechanisms and inflammation (substance P, CGRP, glutamate) (16, 17). Moreover, BoNT reduces the activity of the transient receptor potential vanilloid 1 ion channels (TRPV1), involved in the transduction of noxious stimuli (18, 19). Two different BoNT serotypes are used: Botulinumtoxin A (BoNT/A)—encompassing onabotulinumtoxinA (A/Ona, BOTOX® Allergan), abobotulinumtoxinA (A/Abo, Dysport® Ipsen), and incobotulinumtoxinA (A/Inco, Xeomin® Merz)—and Botulinumtoxin B (BoNT/B) i.e., rimabotulinumtoxinB (B/Rima, Myobloc®/Neurobloc® ElanPharmaceuticals). These toxins differ for complexity, purity, potency, dosing, and immunogenicity. Most studies in NP have been conducted using BoNT/A.
The aim of the present paper is to systematically review the evidence on BoNT usefulness in the management of NP, to highlight scientific certainties and doubts, addressing research progresses, and suggesting directions for future investigations.
Materials and Methods
Search Strategy and Criteria for Selecting Articles
We searched the electronic database MEDLINE, PubMed, and the Cochrane Database for published papers and extracted data for (1) pain, (2) neuropathic pain, (3) botox, (4) botulinum toxin, (5) neuralgia, and (6) neuropathy. We considered randomized controlled trials (RCT), open label (OL) studies, retrospective/prospective case-control (CC) studies, case reports (CR), and case-series (CS) on adult patients with neuropathic pain. Our search also included meta-analyses with no language restrictions and all the titles and abstracts identified by the search were evaluated for eligibility (Figure 1).
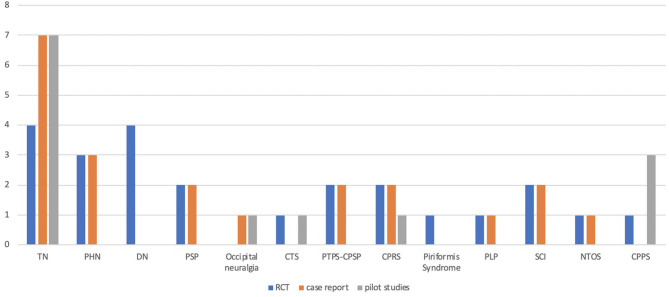
Figure 1.
Studies assessing the efficacy of botulinum toxin in different types of neuropathic pain. TN: trigeminal neuralgia; PHN: post-herpetic neuralgia; DN: diabetic neuropathy; PSP: post-stroke pain; CTS: carpal tunnel syndrome; PTPS: post-thoracotomy pain syndrome; CPSP: chronic post-surgical pain; CPRS: complex regional pain syndrome; PLP: phantom limb pain; SCI: spinal cord injury; NTOS: neurogenic thoracic outlet syndrome; CPPS: Chronic pelvic pain syndrome.
We considered all the articles on human studies providing abstract and full-text published in English language, regardless the year of publication.
We also searched clinical trials on BoNT and NP on www.clinicaltrials.gov.
The search and selection of the articles were made independently by two evaluators (GE, LF) and then discussed with the third author (PB).
Results: BoNT in Neuropathic Pain
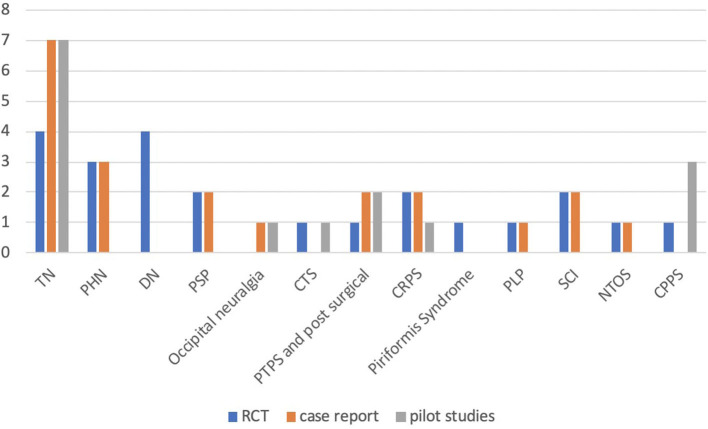
Among the numerous pharmacological studies on BoNT for NP treatment in adults, we identified 22 RCTs, 20 CR, and 10 OL studies including a total of 1,543 patients. Eighteen studies focused on the effect of botulinum toxin in TN, nine in traumatic, compressive and post-surgical causes of NP, six in PHN, five in complex regional pain syndrome (CRPS), four in post-stroke pain (PSP), four in spinal cord injury (SCI), three in painful diabetic neuropathy (PDN), two in occipital neuralgia, two in phantom limb pain (PLP), two in neurogenic thoracic outlet syndrome (NTOS), and four in chronic pelvic pain syndrome (CPPS) (see Figure 2). The search on www.clinicaltrials.gov documented 17 experimental trials: nine completed, four terminated, two ongoing, and one withdrawn. One study actually focused on migraine and was therefore exclude. Complete results are available only for one of the above trials included in our review.
Figure 2.
Studies assessing the efficacy of botulinum toxin in different types of neuropathic pain. TN: trigeminal neuralgia; PHN: post-herpetic neuralgia; DN: diabetic neuropathy; PSP: post-stroke pain; occipital neuralgia; CTS: carpal tunnel syndrome; PTPS: post-thoracotomy pain syndrome; post-surgical pain; CRPS: complex regional pain syndrome; PLP: phantom limb pain; SCI: spinal cord injury; NTOS: neurogenic thoracic outlet syndrome; CPPS: Chronic pelvic pain syndrome.
Trigeminal Neuralgia
TN is the most common and disabling cranial neuralgia in adults and is characterized by a unilateral, abrupt, brief electric shock-like pain, limited to the distribution of one or more divisions of the trigeminal nerve, typically triggered by innocuous stimuli (20). TN is etiologically classified as idiopathic (without any reliable organic substrate), classic (due to a neurovascular conflict between an anomalous vessel and the trigeminal root close to its entry into the pons), and secondary (due to major neurologic diseases, such as multiple sclerosis or tumors at the cerebellopontine angle) (21).
Indisputably, carbamazepine (400–1,200 mg/day) and oxcarbazepine (900–1,800 mg/ day) represent the first-choice TN medical treatment (22). However, even though they are effective in 80% of patients, their clinical benefit may decrease over time and their use is frequently associated to significant side effects (drowsiness, nausea, dizziness, ataxia, hyponatremia, and liver enzymes elevation) (23). Neurosurgical procedures (such as microvascular decompression and radio-surgical treatment)—considered for refractory cases—induce clinical benefit in almost 60–90% of cases but may be followed by complications or pain recurrence (23, 24).
Diverse investigations provided encouraging data on the efficacy of onabotulinum toxin type A (BoNT/A) in reducing pain severity and attack frequency in TN (25, 26). It's worth mentioning, however, that these studies are quite heterogeneous in terms of BoNT/A dose, dilution, route of administration, number/sites of injection and needle type used and include CR (n = 7) (27–33), OL studies (n = 8) (34–41), and RCTs (n = 4) (42–45) (Table 1).
Table 1.
Studies on the use of botulinum toxin in TN.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (27) | Case report | na | na | 1 | IM | Botulinum toxin type A-Botox® | 16 × 8 | VAS reduction score from 82 (baseline) to 45 | - |
| (28) | Case report | na | na | 1 | IM | Botulinum toxin type-A | 7.5 × 2 | More than 90% relief over 2 months with consequent analgesic overuse cessation. | - |
| (29) | Case report | na | na | 1 | SC | Botulinum toxin type A-Botox® | 100 | Complete pain relief at the right external nasal region on the second day after the injection. Partial relief at the mental region. Recurrence after 5 months | Facial paralysis |
| (31) | Case report | na | na | 1 | ID, SC | Onabotulinumtoxin type A | 100 | Improvement after 15 days followed by total pain relief. Pain disappearance at month 28 | Local injection site swelling and slight distal eye- brow ptosis |
| (32) | Case report | na | na | 2 | SM | Onabotulinum toxin A-Botox® | 100 | Case 1: after 3 months, VAS score reduction from 5 to 2; Case 2: after 3 months, VAS score reduction from 10 to 3. | Dryness in the injection area, facial asymmetry |
| (33) | Case report | na | na | 1 | First treatment: SM, IM | Botulinum toxin type A- HengLi® Botox, Lanzhou, Gansu, China | 50 | VAS score reduction from 5–8 to 3–5 after 1 week; pain free after 2 weeks | None |
| (34) | OL | s | na | 8 | SC | Onabotulinum toxin A-Botox® | 100 | VAS score reduction | None |
| (35) | OL | s | na | 13 | SC | Botulinum-A neurotoxin | NS | Significant pain reduction at day 10, symptom free at day 20, > 50% reduction in preventive medication, multiple medications reverted to monotherapy | None |
| (36) | OL | s | na | 20 | SC | Botulinum toxin type A-Botox® | 20–50 | Significant reduction in VAS score (8.83 to 4.08) and in n° of paroxysms (from 23.42 to 8.67). | - |
| (37) | OL | s | na | 15 | SC | BoNT/A | 50 | Significant reduction in VAS score and attack frequency at 1 week, 1 month, and 6 months after injection (P = 0.001). 7 patients became pain free | Transient paresis of the buccal branch of the facial nerve in 3 patients |
| (38) | OL | s | na | 88 | SC | Botulinum toxin type A- HengLi® Botox, Lanzhou, Gansu, China | 25–170 | Effective <1st month in 81 pts and at 2nd month in all subjects. The therapeutic effect decreased after the 3rd month | Local swelling at injection in 3 pts, facial paralysis in 10 pts |
| (39) | OL | s | na | 100 | ID, SM | Botulinum toxin type A- HengLi® Botox, Lanzhou, Gansu, China | 70–140 | Significant VAS score reduction; comparable efficacy and side effects between single and repeated doses. | “Mild, moderate side effects” |
| (40) | OL | s | na | 27 | Maxillary and mandibular root | Onabotulinum toxin A-Botox® | 100 | At month 6 significant reduction in VAS score (from 9.7 to 1.6) and attack frequency (from 217.7 to 55.15); 44.4% of the patients were pain-free | “Mild, moderate side effects |
| (41) | OL | s | na | 43 | ID, SM | Botulinum toxin type A- HengLi® Botox, Lanzhou, Gansu, China | 30–200 | Significant VAS score reduction: in older patients from 8.5 to 4.5 after 1 month, in younger patients from 8.0 to 5.0 | Whole-body mild discomfort, left eye ptosis + slight oral deviation/drooling (2 pts); facial paralysis (2 pts) |
| (42) | RCT | d | Placebo | 42 | ID, SM | BoNT/A | 75 | Significant reduction in VAS score and attack frequency after 2 weeks | Facial asymmetry, facial oedema |
| (44) | RCT | d | Placebo | 36 | SM, IM | Botulinum toxin type A-Botox® | 50 | Significant VAS score reduction after 2 months (p = 0.07) and after 3 months (p = 0.01) | Hematoma, slight facial asymmetry |
| (43) | RCT | s | Placebo | 20 | SM, IM | Botulinum toxin type A-Botox® | 40–60 | Significant reduction in VAS score and number of weekly acute medications and increase in QoL functioning scale | Transient facial asymmetry, hematoma, itching and pain at the site of injection |
| (45) | RCT | d | Placebo | 84 | ID, SM | BoNT/A | 25 or 75 | No difference in short term efficacy with low or high dose | Transient facial asymmetry, oedema at the site of injection |
ITN, idiopathic trigeminal neuralgia; TN, trigeminal neuralgia; s, single blind arm; d, double blind; na, not applicable; *term as originally reported in the study; U, units; IM, intramuscular; SC, subcutaneous; ID, intradermal; SM, submucosal; RCT, randomized controlled trials; OL, open label; BoTN/A, onabotulinum toxin type A; VAS, visual analog scale; -, not reported.
In one RCT, 42 patients affected by classical TN were randomized to multiple intradermal and/or submucosal injections of BoNT/A 75U (22 pts) or saline (20 pts) in the skin and/or mucosa of affected pain areas. BoNT/A significantly reduced pain intensity at week 2 and pain attack frequency at week 1 compared to the placebo (68.2 vs. 15.0%; p < 0.01), showing sustained efficacy and good tolerability (42).
BoNT/A (100 U) has been demonstrated to be effective also in intractable TN in a randomized, single-blinded, placebo-controlled study on 20 patients, significantly reducing pain intensity (6.5 vs. 0.3; p < 0.0001) and acute medication intake and increasing quality of life (QoL) functioning scale at week 12. Each point injection, detected using a “follow the pain” method, received BoNT/A (5 U) or 0.1 ml placebo subcutaneously. In patients with mandibular root involvement, a larger toxin dose was injected posteriorly in the masseter to avoid undesired cosmetic effects (43).
Similarly, BoNT/A (50 U) outperformed placebo in pain severity reduction at 3 months post-dosing (VAS 4.75 vs. 6.94; p = 0.01) in a RCT on 36 patients (20 randomized to active and 16 to placebo) affected by idiopathic TN. Injections were delivered subcutaneously in the affected area and also in the masseter muscle in patients with the involvement of the third branch of the trigeminal nerve (44).
The efficacy of BoNT/A in the treatment of classical TN is not dose-dependent. Zang et al. (45) randomized 84 patients to placebo (n = 28), BoNT/A 25U (n = 27), or BoNT/A 75U (n = 29) and found that both toxin doses were equally significantly more effective than placebo in reducing VAS scores as early as week 1, showing higher response rates at week 8 (70.4 and 86.2%, respectively, vs. 32.1%; p < 0.017). The proportion of patients reporting their pain symptoms as “much improved” or “very much improved” at Patient Global Impression of Change was comparable at both 25U (66.7%) and 75U (75.9%) doses and clearly superior to placebo (32.1%).
A recent meta-analysis of 4 RCTs (42–45) including 178 patients (BoNT/A: 99; placebo: 79) revealed a significant superiority of BoNT/A in reducing pain intensity as measured by VAS total score (RR 2.87, p < 0.0001) and frequency of attacks (p < 0.0001), documenting a benefit duration up to 3 months and mild–moderate and self-limiting adverse events (46). BoNT/A proved effective also in TN persisting after microvascular decompression surgery (29), in symptomatic TN due to exostosis in Meckel's cave (33) and in refractory ITN (40).
To sum up, BoNT/A may represent a useful therapeutic tool in the clinical management of TN. However, the low quality of evidence has led the recent European Academy of Neurology guidelines to limit the use of BoNT/A to a medium-term treatment “in some selected cases” (Table 1) (47).
Post-herpetic Neuralgia
Herpes zoster results from reactivation of varicella zoster virus which lies dormant in sensory dorsal roots, cranial nerves, and autonomic ganglia. It presents as a painful maculopapular or vesicular rash in a dermatomal distribution, most commonly in thoracic and cranial distributions. The PHN is its most common complication, occurring in 10–50% of patients (48), and it can persist for weeks or years after regression of the rash, impairing patients' quality of life (49).
BoNT/A may represent an effective therapeutic option for PHN. Some case-reports documented the efficacy of the toxin in patients with PHN refractory to conventional treatments in term of VAS score reduction at a mean dose of 100 U, with an analgesic effect duration ranging from 52 to 64 days and a good tolerability (50–52).
The encouraging results of this small series have been confirmed by three RCTs and a recent meta-analysis. In one RCT with active comparator, 60 patients affected by PHN in different cutaneous areas were randomized to receive BoNT/A (20 pts), lidocaine (20 pts), or placebo (20 pts). The volumes of administration varied according to the area of tactile allodynia, but fewer than 40 mL volumes (200 units for the maximum BoNT/A dose) were used. BoNT/A reduced pain more effectively than both lidocaine and placebo at day 7 and after 3 months compared to baseline (p < 0.01). The improvement of sleep time in the BoNT/A group was also significantly greater compared with the other groups (P < 0.01) (52, 53).
A long-lasting BoNT/A therapeutic effect has been confirmed in a RCT on 30 adults with PHN in which only the 13 subjects randomized to BoNT/A achieved a >50% reduction in VAS score (NNT=1.2, 95% CI, 2–1; ARR=0.87, 95% CI, 055–096; P < 0.001). Notably, BoNT/A improvement in pain and sleep scores persisted for 16 weeks (54).
In a RCT on 68 patients affected by a miscellany of diverse peripheral neuropathic pain syndromes (post-traumatic or postsurgical pain, polyneuropathy, postherpetic neuralgia), 34 subjects were randomized to receive two subcutaneous administrations of BoNT/A (up to 300 U) or placebo, 12 weeks apart. Two successive BoNT/A administrations significantly decreased (p < 0.0001) the mean pain intensity over 24 weeks after the first treatment administration compared with placebo. The study, which included six subjects with PHN, confirmed the role of BoNT/A in reducing pain severity, evidencing that it was particularly efficacious in participants with preserved nociceptive input. Moreover, the authors suggested that at least two administrations of BoNT/A might be necessary in non-responders before deciding to withdrawing the treatment (55).
Despite BoNT/A efficacy in both chronic TN and PHN (56), herpes zoster has been described as a complication of BoNT/A administration in a 72-year-old woman affected by chronic migraine who developed ophthalmicus herpes zoster 5 days after treatment, probably due to local stress reaction following tissue injury inducing VZV reactivation (57).
In conclusion, the efficacy and safety of BoNT/A in the treatment of PHN is supported by scientific evidence (Table 2), but studies on larger populations are needed.
Table 2.
Studies on the use of botulinum toxin in PHN.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (50) | Case report | Na | na | 1 | SC | Botulinum toxin type A- HengLi® Botox, Lanzhou, Gansu, China | 100 | VAS score reduction from 10 to 1 after 2 days, lasting 52 days | - |
| (51) | Case report | na | na | 1 | ID | BoNT/A | - | VAS score reduction lasting 2 months | - |
| (52) | Case report | na | na | 3 | SC | Botulinum toxin type A-Botox® | 100 | VAS score reduction from 8.3 to 2 after 2 weeks | Temporary erythema |
| (53) | RCT | d | Placebo | 60 (20 treated) | SC | BoNT/A | 200 | Significant reduction of overall symptoms severity (pain, opioid use, sleep interference); marked improvement in quality of life. | - |
| (54) | RCT | d | Placebo | 30 (15 treated) | SC | BoNT/A | 200 | Significant reduction in VAS and sleep scores at week 2; the effect lasted 16 weeks. | Pain during injections |
| (55) | RCT | d | Placebo | 6 | SC | Botulinum toxin type A-Botox® | up to 60 × 5 | Significant VAS score reduction | - |
PHN, post-herpetic neuralga; RCT, randomized controlled trials; s, single blind arm; d, double blind; na, not applicable; IM, intramuscular; SC, subcutaneous; ID, intradermal; SM, submucosal; *term as originally reported in the study; BoTN/A, onabotulinum toxin type A; U, units; VAS, visual analog scale; -, not reported.
Diabetic Neuropathy
DN is a common debilitating complication of diabetes. About a third of patients develop painful diabetic neuropathy (PDN) (58, 59). As current pharmacological treatments are not always effective, BoNT/A has been investigated for pain control in PDN in some RTCs.
Intradermal BoNT/A administration in 18 patients (50 U in the dorsum of the foot for a total of 12 sites at the dose of 4 U for each injection point) induced a significant reduction in VAS score at weeks 1, 4, 8, and 12 compared to placebo with a reduction of VAS ≥3 within 3 months after injection in 44% of patients receiving the active drug. A transient sleep quality improvement was also described (60). Using the same study protocol, Chen et al. (61) reported that BoNT/A may also be beneficial in reducing tactile and mechanical pain threshold in PDN (61). Intradermal BoNT/A at the dose of 8–10 U per injection site (total dose = 100 U) induced a significant (p = 0.05) reduction in neuropathic pain scale (NPS) scores for all items—except cold sensation—in VAS (p = 0.01) and DN4 scores (p < 0.05) compared to placebo in a study performed on 40 patients affected by PDN aged <70 years. One third of patients in the treatment group showed bilateral pain reduction 3 weeks after injection (62).
The use of BoNT/A in DN is promising although the studies are scarce and carried out on small populations (60–63). Larger RTCs are needed.
Post-stroke Pain (PSP)
PSP is a heterogeneous clinical entity caused by neuropathic and nociceptive mechanisms, which affects from 10 to 70% of patients with stroke and includes central PSP, pain related to spasticity, muscle-skeletal pain, complex regional pain syndrome, and post-stroke headache (64, 65).
PSP is one of the factors contributing to patients' disability and interferes with daily activities, sleep, walking, physiotherapy, greatly affecting their quality of life.
The efficacy of BoNT/A in central PSP control has been investigated (Table 3) (66–69). A prospective RCT performed on 37 patients failed to demonstrate any BoNT/A efficacy on PSP (68). Conversely, a larger RCT on post-stroke spasticity on 273 patients—mostly complaining of PSP (74.3%)—randomized to BoNT/A plus standard care showed a significantly greater reduction in pain and in pain interference with work (p < 0.05) compared to patients treated with placebo plus standard care (Table 4) (69).
Table 3.
Studies on the use of botulinum toxin in DN.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (60) | RCT | d | Placebo | 20 | ID | Botulinum toxin type A | 50 | Significant VAS reduction (P < 0.05) | Local skin infection |
| (61) | RCT | d | Placebo | 20 | ID | Onabotulinum toxin A | 50 | Significant decrease in tactile threshold and pain threshold (P < 0.05) | - |
| (62) | RCT | d | Placebo | 40 | ID | Botulinum toxin type A-Dysport®-Ipsen, UK | 100 | Reduction in NPS (P = 0.05) and DN4 scores (P < 0.05). Pain freedom in 30% of patients (p = 0.01) | - |
DN, diabetics neuropathy; RCT, randomized controlled trials; d, double; ID, intradermal; *term as originally reported in the study; U, units; VAS, visual analog scale; NPS, neuropathy pain scale; -, not reported.
Table 4.
Studies on the use of botulinum toxin in PSP.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (67) | Case report | na | na | 1 | IM | Onabotulinum toxin type A-Botox® | 25, 75, and 100 | Pain reduction after 2 days; spasticity improvement after 1 week | - |
| (66) | Case report | na | na | 2 | IM | Botulinum toxin type A | 200 | NRS reduction for more than 3 months | - |
| (69) | RCT | d | Placebo+SC | 273 (139 BoNT/A + SC vs. 134 Placebo + SC) | IM | Onabotulinum toxin type A-Botox® | As needed | Reduction in VAS and pain interference with work (P < 0.05) | - |
| (69) | RCT | d | Placebo | 37 (21 BoNT/A vs. 16 Placebo) | IM | Onabotulinum toxin type A-Botox® | 140, 200 | No significant differences between the groups found for any of the daily pain ratings | - |
PSP, Post-stroke pain; RCT, randomized controlled trials; d, double; na, not applicable; SC, Standard care; IM, intramuscular; *term as originally reported in the study; U, units; VAS, visual analog scale; -, not reported.
The usefulness of BoNT/A in the management of PSP deserves to be investigated in further ad hoc designed RTCs.
Occipital Neuralgia
Occipital neuralgia is a unilateral or bilateral radiating pain in the posterior part of the scalp in the distribution of the greater, lesser, and/or third occipital nerves (20). The causes of occipital neuralgia include irritation or injury to the divisions of the occipital nerve, its focal entrapment and myofascial spasm. Persistent occipital neuralgia can produce severe headaches that are difficult to control by conservative or surgical approaches. The occipital nerve blocks using BoNT/A at the dose of 50 U for each block provided a meaningful reduction in pain intensity and disability in five out of six patients in patients who had failed prior oral therapies or traditional nerve blocks in a case series study (70). BoNT/A, at the same dose, improved the sharp/shooting type of pain associated with occipital neuralgia in a pilot study on six patients, inducing also a significant improvement of headache-specific quality of life (p = 0.0315) (Table 5) (71).
Table 5.
Studies on the use of botulinum toxin in Occipital Neuralgia.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (70) | Cases series | na | na | 6 | Occipital nerve block | Onabotulinum toxin type A-Botox® | 100 (50 for each block) | Significant reduction in pain VAS scores and improvement in PDI | - |
| (71) | PS | s | na | 6 | Occipital nerve block | Onabotulinum toxin type A-Botox® | 100 for each block | Improvement in the sharp/shooting type of pain most commonly associated with occipital neuralgia | - |
PS, prospective study; s, single; na, not applicable; ID, intradermal; *term as originally reported in the study; U, units; VAS, visual analog scale; PDI, pain disability index; -, not reported.
Carpal Tunnel Syndrome (CTS)
ARCT with botulinum toxin type B (BoNT/B) in 20 outpatients affected by CTS did not confirm the positive findings reported in an open label trial on five women (Table 6) (72, 73).
Table 6.
Studies on the use of botulinum toxin in CTS.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (72) | PS | s | na | 5 | Intracarpal | Botulinum toxin type A- Dysport®, Beaufour Ipsen, UK | 60 | Not superior to placebo (p = 0.2) | Local weakness and discomfort |
| (73) | RCT | d | placebo | 20 | Intracarpal | Botulinum toxin type B | 30 for sides | Not superior to placebo | - |
CTS, carpal tunnel syndrome; PS, prospective study; RCT, randomized controlled trials; s, single; d, double; na, not applicable; *term as originally reported in the study; U, units; -, not reported.
Post-thoracotomy Pain Syndrome (PTPS) and Chronic Post-surgical Pain
PTPS is a traumatic neuropathy that can affect as many as 50% of patients undergoing thoracotomy, is often refractory to conservative management and may require multiple analgesics for adequate pain control. BoNT/A may represent an alternative or adjunct treatment to improve symptom management in patients with PTPS (Table 7) (79). Two case reports documented the efficacy of BoNT/A (total dose: 50–100 U, along the scar) in inducing a significant and prolonged pain reduction in patients affected by PTPS with multiple prior therapeutic failures (74, 75).
Table 7.
Studies on the use of botulinum toxin in post-surgical syndrome.
| References | Cause of pain | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|---|
| (74) | Post-thoracotomy | Case report | na | na | 1 | SC | Onabotulinum toxin type A-Botox® | 2.5 for site | 50% VAS score improvement, sustained up to week 12 | - |
| (75) | Post-thoracotomy | Case report | na | na | 1 | SC | Botulinum toxin type A | 50 | Significant reduction of pain at day 4 sustained up to month 4 | - |
| (76) | Post-surgical and post radiation therapy | PS | s | na | 25 | IM, SC | Incobotulinum toxin A | 100 | Significant improvement in VAS score and patients satisfaction | 2 skin reactions |
| (77) | Post-mastectomy | RCT | d | Placebo | 30 | IM | Onabotulinum toxin type A-Botox® | 40 for each pectoralis | Significant pain reduction in VAS score (p < .05) | - |
| (78) | Post-mastectomy | RS | na | Controls | 48 | IM | Botulinum toxin type A | 100 | Significant reduction pain in postoperative (p < 0.0001), during initial (P = 1.6 × 10(6)) and final expansion (p = 0.009) | - |
PS, prospective study; RCT, randomized controlled trials; RS, retrospective study; s, single; d, double; na, not applicable; SC, subcutaneous; IM, intramuscular; *term as originally reported in the study; U, units; VAS, visual analog scale; NRS, numeric rating scale; -, not reported.
The prevalence of chronic post-surgical pain in cancer patients ranges from 20 to 70% according to different studies. Chronic post-surgical pain pathophysiology is likely to include both peripheral and sensitization mechanisms (80, 81).
A prospective study on 48 post-mastectomy patients demonstrated that BoNT/A (100 U) administration in the pectoralis major, serratus anterior, and rectus abdominis muscle followed by immediate insertion of tissue expander leads to a significant reduction of post-operative pain (p < 0.0001) and pain during both initial and final expansion (p = 0.009), greater volume of expansion per session (p = 0.010), reduced number of expansion sessions (p = 0.025), and lower narcotic use compared to standard procedures (p= 0.012) (78).
Similarly, a prospective RCT evaluating BoNT/A in expander-based breast reconstruction (40 U into the pectoralis major muscle), demonstrated a reduction in the use of oxycodone (p < 0.0001) and diazepam (p < 0.0001) and an increase in the expansion volume per visit in the active group compared to placebo (p < 0.05) (77).
BoNT/A (doses up to 100 U, intramuscularly or subcutaneously) proved effective in reducing pain and improving quality of life in eight out of 12 female cancer patients who had surgery or radiation for local cancer and failed >2 analgesic treatments (76) (Table 7).
Complex Regional Pain Syndrome (CRPS)
CRPS is characterized by disabling chronic-relapsing burning pain, vasomotor changes, and occasionally trophic or motor function changes (82).
BoNT/A administration in muscular trigger points was reported to be effective in CRPS (83) but this finding was not confirmed in a larger prospective RCT on 14 individuals delivering BoNT/A into the allodynic skin areas (84). Caroll et al. randomly treated nine patients with refractory CRPS using standard lumbar sympathetic block (LSB) with bupivacaine (0.5%) or LSB with bupivacaine (0.5%) + BoNT/A (75 U) and found a significantly lower rate of pain return (p < 0.02) and greater reduction in pain intensity (p < 0.0001) in those receiving BoNT/A compared with local anesthetic alone (85).
In a retrospective, uncontrolled study, the EMG-guided administration of 100 U of BoNT/A (10–20 U per pain site) to 37 patients with severe local pain at baseline induced a significant pain reduction (mean pain score from 8.2 to 4.5; p < 0.001) in almost all individuals (97%) (86). Lumbar sympathetic block with levobupivacaine 0.25% 5 mL plus botulinum toxin type B 5,000 IU under fluoroscopic guidance was associated, 2 months later, to a meaningful reduction of pain intensity, allodynia, Leeds assessment of neuropathic symptoms, skin coldness and discoloration, and tissue swelling (87). The studies are summarized in Table 8.
Table 8.
Studies on the use of botulinum toxin in CRPS.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (87) | Case report | na | na | 2 | Lumbar sympathetic block | Botulinum toxin type B-Myobloc®, Solstice Neurosciences, USA | 5,000 | Reduction in VAS score and CRPS symptoms | Nausea and vomiting (1 pt) |
| (83) | Cases series | na | na | 2 | IM | Botulinum toxin type A | 20 for site (total 200) | Reduced pain and distal allodynia | - |
| (86) | RS | na | na | 37 | IM | Botulinum toxin type A | 100 | Pain reduction in 97% of patients | Transient neck drop (1 pt) |
| (84) | RCT + OL | d | Placebo | 8+6 | ID, SC | Onabotulinum toxin type A-Botox® | 40–200 | Ineffective | Poorly tolerated |
| (85) | RCT | d | 0.5% bupivacaine | 9 | Sympathetic block | Botulinum toxin type A | 75 | Longer duration of pain reduction (71 vs. 10 days; p < 0.02). Significant VAS core reduction (p < 0.0001) | Nausea and vomiting (1 pt |
CRPS, Complex regional pain syndrome; RCT, randomized controlled trials; RS, retrospective study; OL, Open label; d, double; na, not applicable; SC, subcutaneous; IM, intramuscular; ID, intradermal; *term as originally reported in the study; U, units; VAS, visual analog scale; -, not reported.
Piriformis Syndrome
Piriformis syndrome is caused by the entrapment of the sciatic nerve by the piriformis muscle and accounts to up 8% of sciatic pain. The diagnosis of piriformis syndrome is sometimes challenging due to clinical overlap with low back and buttock pain. A single RCT on 56 patients treated with physical therapy and allocated to BoNT/A A (300 U) or placebo revealed a more marked reduction in VAS score, compared with placebo, at 2, 4, 6, 8, 10, and 12 weeks post-injection (P < 0.0001) (Table 9) (88).
Table 9.
Studies on the use of botulinum toxin in Piriformis syndrome.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (88) | RCT | d | Placebo | 56 | IM | Incobotulinum toxin type A | 300 | Significant VAS score reduction at weeks 2,4,6,8, and 12 post-injection (p < 0.0001) | Injection site pain, stiff neck, wobbly neck, flu-like symptoms |
RCT, randomized controlled trials; d, double; *term as originally reported in the study; U, units; VAS, visual analog scale; -, not reported.
Phantom Limb Pain (PLP)
The long-term treatment of PLP using BoNT/A administration (4 × 25 U, quarterly) in the stump muscles of a lower limb amputee led to almost complete pain freedom (89).
A prospective RCT on 14 patients randomized to receive BoNT/A (250–300 U) or lidocaine plus depomedrol at the focal tender point demonstrated that both treatments were equally effective in PLP relief (Table 10) (90).
Table 10.
Studies on the use of botulinum toxin in PLP.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (90) | Case report | na | na | 1 | IM | Onabotulinum toxin type A-Botox® | 100 (4 injections performed every 3 months) | Almost complete pain-freedom | - |
| (89) | RCT | d | Lidocaine/Depomedrol | 14 | IM/cutaneous/SC | Onabotulinum toxin type A-Botox® | 50 for sides | Not superior to placebo | - |
PLP, Phantom Limb Pain; RCT, randomized controlled trials; d, double; na, not applicable; *term as originally reported in the study; IM, intramuscular; SC, subcutaneous; U, units; -, not reported.
Spinal Cord Injury (SCI)
Pain often complicates SCI. Neuropathic pain after SCI is generally severe, refractory to treatment and persistent over time, reducing quality of life and interfering with cognitive, emotional, and physical functioning. Its prevalence rate ranges between 75 and 81% (91, 92).
A few case reports described a notable VAS score improvement of SCI-related neuropathic pain and allodynia using BoNT/A at a dose ranging from 80 to 200 U, documenting also a quite rapid onset of the clinical benefit and a long-lasting effect (>3 months) (93, 94). These promising findings were confirmed by two RCTs. BoNT/A (200 U) subcutaneous administration into the painful area proved effective in a trial on 40 patients affected by SCI-associated neuropathic pain, exhibiting a statistically significant decrease in VAS at weeks 4 and 8 compared to the placebo group (95). Similar results were reported by another study including 44 patients which documented a greater efficacy of BoNT/A over placebo in decreasing the VAS score after weeks 4 and 8 post treatments (p < 0.01) and in improving quality of life (Table 11) (96).
Table 11.
Studies on the use of botulinum toxin in SCI.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (94) | Case report | na | na | 1 | SC | Botulinum toxin type A | 10 | VAS decreased from 96 to 23 | - |
| (93) | Case report | na | na | 2 | SC | Onabotulinum toxin type A-Botox® | 20 | Significant VAS score reduction for > 3 months | - |
| (95) | RCT | d | Placebo | 40 | SC | Botulinum toxin type A- BTX-A Meditoxin Medytox, Seoul, South Korea | 200 | Significant VAS score reduction at week 4 (p < 0.0001) and at week 8 (p = 0.0012). | - |
| (96) | RCT | d | Placebo | 44 | SC | Botulinum toxin type A- HengLi Botox, Lanzhou, Gansu, China | 200 | Significant VAS score reduction at week 4 and week 8 of treatment (p < 0.01) | - |
SCI, spinal cord injury; RCT, randomized controlled trials; d, double; na, not applicable; SC, subcutaneous; *term as originally reported in the study; U, units; VAS, visual analog scale; -, not reported.
Neurogenic Thoracic Outlet Syndrome (NTOS)
NTOS is a complex entity characterized by different neurovascular signs and symptoms involving the upper limb due to a compression of the brachial plexus trunks or cords, including nerves which comes from the C5-T1 spinal levels. According to some studies, BoNT may be useful to reduce NTOS symptoms in those patients who did not benefit from physical therapy (97–99) (Table 12).
Table 12.
Studies on the use of botulinum toxin in NTOS.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (98) | Case report | na | na | 1 | IM | Botulinum toxin type A | 30 | Symptomatic relief | - |
| (99) | RCT | d | Placebo | 38 | IM | Botulinum toxin type A | 75 | VAS scores did not result in clinically or statistically significant improvements in pain (P = 0.36). | - |
NTOS, neurogenic thoracic outlet syndrome; RCT, randomized controlled trials; d, double; na, not applicable; IM, intramuscular; *term as originally reported in the study; U, units; VAS, visual analog scale; -, not reported.
Chronic Pelvic Pain Syndrome (CPPS)
CPPS is defined as “a chronic pain and inflammation in the pelvic organs lasting >6 months” (100). Its treatment includes behavioral interventions, physical therapy, medications, nerve blocks, neurostimulation techniques, surgical interventions, and alternative therapies. BoNT/A has also been considered in a multimodal treatment plan in selected cases, being able to act on the pelvic peripheral nerves through different mechanisms. Some studies have reported encouraging results as regards VAS score reduction (101–104) (Table 13).
Table 13.
Studies on the use of botulinum toxin in CPPS.
| References | Study type | Blinding | Comparator | Pts n° | Injection route/site | Toxin type* | Dose (U) | Major findings | AEs |
|---|---|---|---|---|---|---|---|---|---|
| (101) | Pilot study | na | na | 12 | IM | Botulinum toxin type A Botox® | 40 | VAS and Quality of life scores significantly improved (p = 0.01) | Influenza-like symptoms (2 pts) |
| (102) | Pilot study | na | na | 29 | IM | Botulinum toxin type A | 100 | Partial response rate on the GRA (p = 0.0002). Significant reduction in CPSI pain subdomain score (p = 0.05) | - |
| (103) | RCT | d | Placebo | 60 | Transurethral intraprostatic | Botulinum neurotoxin type A | 100 | Significant VAS score decrease and significant improvement in QoL scores (p < 0.05) | - |
| (104) | PS | na | na | 43 | Transurethral intraprostatic | Onabotulinum toxin type A | VAS −79 and −27.4% at 3 and 12 months (p < 0.0001) | - |
CPPS, chronic pelvic pain syndrome; RCT, randomized controlled trials; PS, prospective study; d, double; na, not applicable; IM, intramuscular; *term as originally reported in the study; U, units; GRA, Global Response Assessment; CPSI, Chronic Prostatitis Symptom Index; VAS, visual analog scale; -, not reported.
Conclusions
The majority of the studies were performed using BoNT/A, two studies using BoNT/B. VAS score reduction was the primary endpoint in all the studies. A positive effect of BoNT/A on NP was documented in 19 out of 21 RCT studies. The only RCT performed with BoNT/B provided negative results. Negative results emerged in two RCTs, (one in PSP and one in CTS) (69, 73) while one RCT in CRPS was stopped due to low tolerability (84). The positive effects of BoNT/A on NP started after 4–8 weeks [after 1 week in TN (34, 35, 39)] and persisted up to 6 months after treatment (34, 37–42, 45, 60, 62, 68, 70, 71, 89, 90, 94). The duration of BoNT/A benefit was dependent on toxin dose, injection site, number and depth of injections in NP (40, 41) but not in TN (34, 37–42, 45). The effect of BoNT/B, associated with levobupivacaine, was positive only in two case reports (87); negative effect of BoNT/B was observed in a pilot studies on 20 patients (73).
In all the studies, BoNT/A had been used as a second line treatment in patients who had had previous pharmacological therapeutic failures. Prior unresponsiveness to standard of care did not affect patient's responsivity to BoNT/A. The overall tolerability of BoNT/A in the different clinical setting was good, and adverse events were usually transient and mild. No safety concerns emerged. The treatment of the face for trigeminal neuralgia or post-herpetic neuralgia was burdened by a greater number of side effects compared to limb or thorax districts due to potential facial asymmetry induced by the muscle relaxant effect of BoNT/A.
NP is a chronic, highly disabling condition caused by a lesion or disease of the somatosensory nervous system which affects from 1.5 to 6.9% of individuals aged 50–64 years (10, 11).
There is a stringent need for innovative and alternative NP treatments because the current standard of care—including antidepressants, anticonvulsants, opioids, topical capsaicin, and lidocaine as well as non-pharmacological approaches—is still unsatisfactory due to the low responder rate (<30% of patients), the frequency and severity of adverse events (encompassing dizziness, ataxia, nausea, vomiting, somnolence, and cutaneous rash), and the relevant proportion of patients with treatment discontinuation (30–50%) (11, 13).
Botulinum toxin could represent a promising therapeutic tool for NP for its documented efficacy and tolerability in a wide range of NP conditions. BoNT/A is the toxin most extensively studied, having being investigated in 21 RCTs. BoNT/A seems helpful in particular in TN, PHN, PDN, occipital neuralgia, post-surgical pain and in SCI-related pain. However, the quality of evidence is low overall due to the paucity of RCT in some NP types, the small number of patients studied and methodological heterogeneities. One major limitation is the use of different toxin serotypes and preparations which hampers the comparison of studies' results. Most studies specified the use of the common BoNT/A brand (Botox®) (27, 29, 32, 34, 36, 40, 43, 44, 52, 55, 67–71, 74, 77, 84, 89, 90, 93, 101) or other BoNT/A compounds (e.g., HengLi®, Meditoxin®, Disport®) (33, 38, 39, 41, 50, 62, 72, 94, 96), but, in many cases, no specification of the BoNT/A serotype was provided (27, 31, 35, 37, 42, 47, 51, 53, 54, 60, 61, 66, 75, 78, 83, 85, 86, 94, 102–104). Furthermore, two studies were performed with botulinum toxin type B (73, 87) and two with incobotulinum toxin type A (76, 88).
No major safety issue emerged in the studies reported in the present review. Adverse events were rated as mild or moderate and included local skin reaction (swelling), pain at the injection site, muscles weakness, flu symptoms, nausea, and vomiting. However, there is a need for a specific evaluation of this aspect in human trials as, at present, only data on experimental animal models have been provided (105, 106).
The cost of the toxin and the need of specific injection expertise may represent a restriction for its widespread use.
Bearing in mind these limitations, we deem that the use of botulinum toxin should be carefully considered in patients with NP not responsive to current standard of care and to avoid undesired adverse events and safety concerns. BoNT could also reduce the use of surgical or invasive procedures, often applied in patients refractory to common therapeutic strategies.
Larger and specifically designed RCTs are awaited to confirm efficacy and tolerability of BoNT and also to provide standardized treatment models for the different types of NP, systematically specifying serotypes, doses, treatment sites, and the depth and number of injections. Future researches are also expected to ascertain the proportion of patients developing anti-toxin antibodies during prolonged treatment, evaluate the risk of systemic effects after local delivery and appraise the safety of the botulinum toxin in the elderly and in fragile individuals.
Author Contributions
GE and LF equally contributed to the review of the literature and to the draft of the article. PB contributed to the draft and revision of the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
GE has received travel grants and honoraria from Eli-Lilly, Novartis, and New Penta. LF has received travel grants and honoraria from TEVA, Eli-Lilly, and Novartis. PB has received travel grants or research support and honoraria or both for lecturing and being a consultant and scientific advisor for Merck, Lusofarmaco, Bayer, TEVA, Novartis, Eli-Lilly, Visufarma, and Assosalute.
Acknowledgments
The English language in the manuscript was edited by Silvia Riondino.
Footnotes
Funding. This work was partially supported by the Italian Ministry of Health (institutional funding ricerca corrente).
References
- 1.Jensen TS, Finnerup NB. Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. Lancet Neurol. (2014) 13:924–35. 10.1016/S1474-4422(14)70102-4 [DOI] [PubMed] [Google Scholar]
- 2.Cohen SP, Mao J. Neuropathic pain: mechanisms and their clinical implications. BMJ. (2014) 348:f7656. 10.1136/bmj.f7656 [DOI] [PubMed] [Google Scholar]
- 3.Staff NP, Grisold A, Grisold W, Windebank AJ. Chemotherapy-induced peripheral neuropathy: a current review. Ann Neurol. (2017) 81:772–81. 10.1002/ana.24951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nickel FT, Seifert F, Lanz S, Maihöfner C. Mechanisms of neuropathic pain. Eur Neuropsycho pharmacol. (2012) 22:81–91. 10.1016/j.euroneuro.2011.05.005 [DOI] [PubMed] [Google Scholar]
- 5.Julius D, Basbaum AI. Molecular mechanisms of nociception. Nature. (2001) 413:203–10. 10.1038/35093019 [DOI] [PubMed] [Google Scholar]
- 6.Yan YY, Li CY, Zhou L, Ao LY, Fang WR, Li YM. Research progress of mechanisms and drug therapy for neuropathic pain. Life Sci. (2017) 190:68–77. 10.1016/j.lfs.2017.09.033 [DOI] [PubMed] [Google Scholar]
- 7.Tsuda M, Inoue K, Salter MW. Neuropathic pain and spinal microglia: a big problem from molecules in “small” glia. Trends Neurosci. (2005) 28:101–7. 10.1016/j.tins.2004.12.002 [DOI] [PubMed] [Google Scholar]
- 8.Shinder V, Grovin-Lippmann R, Cohen S, Belenky M, Ilin P, Fried K, et al. Structural basis of sympathetic-sensory coupling in rat and human dorsal root ganglia following peripheral nerve injury. J Neurocytol. (1999) 28:743–61. 10.1023/A:1007090105840 [DOI] [PubMed] [Google Scholar]
- 9.Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. (2010) 9:807–19 10.1016/S1474-4422(10)70143-5 [DOI] [PubMed] [Google Scholar]
- 10.Sałata K, Gryzłob B, Kuligc K. Experimental drugs for neuropathic pain. Current Neuropharmacol. (2018) 16:1193–209. 10.2174/1570159X16666180510151241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dosenovic S, JelicicKadic A, Miljanovic M, Biocic M, Boric K, Cavar M, et al. Interventions for neuropathic pain: an overview of systematic reviews. Anesth Analg. (2017) 125:643–52. 10.1213/ANE.0000000000001998 [DOI] [PubMed] [Google Scholar]
- 12.Kerstman E, Ahn S, Battu S, Tariq S, Grabois M. Neuropathic pain. Handb Clin Neurol. (2013) 110:175–87. 10.1016/B978-0-444-52901-5.00015-0 [DOI] [PubMed] [Google Scholar]
- 13.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. (2015) 14:162–73. 10.1016/S1474-4422(14)70251-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meng F, Peng K, Yang JP, Ji FH, Xia F, Meng XW. Botulinum toxin-a for the treatment of neuralgia: a systematic review and meta-analysis. J Pain Research. (2018) 11:2343–51. 10.2147/JPR.S168650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freund B, Schwartz M. Subcutaneous BTX-A in the Treatment of Neuropathic Pain: A Pilot Study. Presented at the 38th Interagency Botulism Research Coordinating Committee Meeting, Easton, MD: (2001). p. 19:2001. [Google Scholar]
- 16.Marinelli S, Vacca V, Ricordy R, Uggenti C, Tata AM, Luvisetto S, et al. The analgesic effect on neuropathic pain of retrogradely transported botulinum neurotoxin A involves Schwann cells and astrocytes. PLoS ONE. (2012) 7:e47977. 10.1371/journal.pone.0047977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bach-Rojecky L, Dominis M, Lackovic Z. Lack of anti-in?ammatory effects of botulinum toxin A in experimental models of in?ammation. Fundam Clin. Pharmacol. (2008) 22:503–9. 10.1111/j.1472-8206.2008.00615.x [DOI] [PubMed] [Google Scholar]
- 18.Meng J, Ovsepian SV, Wang J, Pickering M, Sasse A, Aoki KR, et al. Activation of TRPV1 mediates calcitonin gene-related peptide release, which excites trigeminal sensory neurons and is attenuated by a retargeted botulinum toxin with anti-nociceptive potential. J Neurosci. (2009) 29:4981–92. 10.1523/JNEUROSCI.5490-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Francisco GE, Tan H, Green M. Do botulinum toxins have a role in the management of neuropathic pain? a focused review. Am J Phys Med Rehabil. (2012) 91:899–909. 10.1097/PHM.0b013e31825a134b [DOI] [PubMed] [Google Scholar]
- 20.Headache Classification Committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. (2018) 38:1-211 10.1177/0333102417738202 [DOI] [PubMed] [Google Scholar]
- 21.Scholz J, Finnerup NB, Attal N, Aziz Q, Baron R, Bennett MI, et al. Classification Committee of the Neuropathic Pain Special Interest Group (NeuPSIG). The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain. (2019) 160:53–9. 10.1097/j.pain.0000000000001365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. American Academy of Neurology Society; European Federation of Neurological Society. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. (2008) 15:1013–28. 10.1111/j.1468-1331.2008.02185.x [DOI] [PubMed] [Google Scholar]
- 23.Cheshire WP. Trigeminal neuralgia. Curr Pain Headache Rep. (2007) 11:69–74. 10.1007/s11916-007-0025-7 [DOI] [PubMed] [Google Scholar]
- 24.Gubian A, Rosahl SK. Meta-analysis on safety and efficacy of microsurgical and radiosurgical treatment of trigeminal neuralgia. World Neurosurg. (2017) 103:757–67. 10.1016/j.wneu.2017.04.085 [DOI] [PubMed] [Google Scholar]
- 25.Spina A, Mortini P, Alemanno F, Houdayer E, Iannaccone S. Trigeminal neuralgia: toward a multimodal approach. World Neurosurg. (2017) 103:220–30. 10.1016/j.wneu.2017.03.126 [DOI] [PubMed] [Google Scholar]
- 26.Cruccu G, Truini A. Refractory trigeminal neuralgia. Non-surgical treatment options. CNS Drugs. (2013) 27:91–6. 10.1007/s40263-012-0023-0 [DOI] [PubMed] [Google Scholar]
- 27.Allam N, Brasil-Neto JP, Brown G, Tomaz C. Injections of botulinum toxin type a produce pain alleviation in intractable trigeminal neuralgia. Clin J Pain. (2005) 21:182–4. 10.1097/00002508-200503000-00010 [DOI] [PubMed] [Google Scholar]
- 28.Volcy M, Tepper SJ, Rapoport AM, Sheftell FD, Bigal ME. Botulinum toxin A for the treatment of greater occipital neuralgia and trigeminal neuralgia: a case report with pathophysiological considerations. Cephalalgia. (2006) 26:336–40. 10.1111/j.1468-2982.2005.00959.x [DOI] [PubMed] [Google Scholar]
- 29.Ngeow WC, Nair R. Injection of botulinum toxin type A (BOTOX) into trigger zone of trigeminal neuralgia as a means to control pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2010) 109:e47–50. 10.1016/j.tripleo.2009.03.021 [DOI] [PubMed] [Google Scholar]
- 30.Xu Y, Zhang Q, Mao C, Hu W, Zhou X, Luo W. Evaluation of therapeutic effectiveness and safety of botulinum toxin type A in the treatment of idiopathic trigeminal neuralgia in patients older than 70 years. Zhonghua Yi XueZaZhi. (2015) 95:1994–6. 10.3760/cma.j.issn.0376-2491.2015.25.007 [DOI] [PubMed] [Google Scholar]
- 31.Lunde HM, Torkildsen Ø, Bø L, Bertelsen AK. Botulinum toxin as monotherapy in symptomatic trigeminal neuralgia headache. J Head Face Pain. (2016) 56:1035–9. 10.1111/head.12791 [DOI] [PubMed] [Google Scholar]
- 32.Herrero Babiloni A, Kapos FP, Nixdorf DR. Intraoral administration of botulinum toxin for trigeminal neuropathic pain. Oral Surg Oral Med Oral Pathol Oral Radiol. (2016) 121:e148–53. 10.1016/j.oooo.2016.03.013 [DOI] [PubMed] [Google Scholar]
- 33.Wu C, Xie N, Liu H, Zhang H, Zhang L, Lian Y. A new target for the treatment of trigeminal neuralgia with botulinum toxin type A. Neurol Sci. (2018) 39:599–602. 10.1007/s10072-017-3171-7 [DOI] [PubMed] [Google Scholar]
- 34.Türk Bör, ü Ü, Ilhan S, Alp R, Sur H. Botulinum toxin and intractable trigeminal neuralgia. Clin Neuropharmacol. (2005) 28:161–2. 10.1097/01.wnf.0000172497.24770.b0 [DOI] [PubMed] [Google Scholar]
- 35.Piovesan EJ, Teive HG, Kowacs PA, Della Coletta MV, Werneck LC, Silberstein SD. An open study of botulinum-A toxin treatment of trigeminal neuralgia. Neurology. (2005) 25:65:1306–8. 10.1212/01.wnl.0000180940.98815.74 [DOI] [PubMed] [Google Scholar]
- 36.Zúñiga C, Díaz S, Piedimonte F, Micheli F. Beneficial effects of botulinum toxin type A in trigeminal neuralgia. Arq Neuropsiquiatr. (2008) 66:500–3. 10.1590/S0004-282X2008000400012 [DOI] [PubMed] [Google Scholar]
- 37.Bohluli B, Motamedi MH, Bagheri SC., Bayat M, Lassemi E, Navi F, et al. Use of botulinum toxin A for drug-refractory trigeminal neuralgia: preliminary report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2011) 111:47–50. 10.1016/j.tripleo.2010.04.043 [DOI] [PubMed] [Google Scholar]
- 38.Li S, Lian YJ, Chen Y, Zhang HF, Ma YQ, He CH, et al. Therapeutic effect of Botulinum toxin-A in 88 patients with trigeminal neuralgia with 14-month follow-up. J Headache Pain. (2014) 22:15:43. 10.1186/1129-2377-15-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang H, Lian Y, Xie N, Chen C, Zheng Y. Single-dose botulinum toxin type a compared with repeated-dose for treatment of trigeminal neuralgia: a pilot study. J Headache Pain. (2017) 18:81. 10.1186/s10194-017-0793-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Türk Börü Ü, Duman A, Bölük C, CoşkunDuman S, Taşdemir M. Botulinum toxin in the treatment of trigeminal neuralgia: 6-Month follow-up. Medicine. (2017) 96:e8133. 10.1097/MD.0000000000008133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu J, Xu YY, Zhang QL, Luo WF. Efficacy and safety of botulinum toxin type A in treating patients of advanced age with idiopathic trigeminal neuralgia. Pain Res Manag. (2018) 2018:7365148. 10.1155/2018/7365148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu CJ, Lian YJ, Zheng YK, Zhang HF, Chen Y, Xie NC, et al. Botulinum toxin type A for the treatment of trigeminal neuralgia: results from a randomized, double-blind, placebo-controlled trial. Cephalalgia. (2012) 32:443–50. 10.1177/0333102412441721 [DOI] [PubMed] [Google Scholar]
- 43.Shehata HS, El-Tamawy MS, Shalaby NM, Ramzy G. Botulinum toxin-type A: could it be an effective treatment option in intractable trigeminal neuralgia? J Headache Pain. (2013) 14:92. 10.1186/1129-2377-14-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zúñiga C, Piedimonte F, Díaz S, Micheli F. Acute treatment of trigeminal neuralgia with onabotulinum toxin A. Clin Neuropharmacol. (2013) 36:146–50. 10.1097/WNF.0b013e31829cb60e [DOI] [PubMed] [Google Scholar]
- 45.Zhang H, Lian Y, Ma Y, Chen Y, He C, Xie N, et al. Two doses of botulinum toxin type A for the treatment of trigeminal neuralgia: observation of therapeutic effect from a randomized, double-blind, placebo-controlled trial. J Headache Pain. (2014) 15:65. 10.1186/1129-2377-15-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morra ME, Elgebaly A, Elmaraezy A, Khalil AM, Altibi AM, Vu TL, et al. Therapeutic efficacy and safety of botulinum toxin A therapy in trigeminal neuralgia: a systematic review and meta-analysis of randomized controlled trials. J Headache Pain. (2016) 17:63. 10.1186/s10194-016-0651-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bendtsen L, Zakrzewska JM, Abbott J, Braschinsky M, Di Stefano G, Donnet A, et al. European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol. (2019) 26:831–49. 10.1111/ene.13950 [DOI] [PubMed] [Google Scholar]
- 48.Yawn BP, Gilden D. The global epidemiology of herpes zoster. Neurology. (2013) 81:928–30. 10.1212/WNL.0b013e3182a3516e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oster G, Harding G, Dukes E, Edelsberg J, Cleary PD. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: Results from a population-based survey. J Pain. (2005) 6:356–63. 10.1016/j.jpain.2005.01.359 [DOI] [PubMed] [Google Scholar]
- 50.Liu HT, Tsai SK, Kao MC, Hu JS. Botulinum toxin A relieved neuropathic pain in a case of post-herpetic neuralgia. Pain Med. (2006) 7:89–91. 10.1111/j.1526-4637.2006.00100.x [DOI] [PubMed] [Google Scholar]
- 51.Ruiz Heute C, Bermejo P. Botulinum toxin type A in the treatment of neuropathic pain in a case of postherpetic neuralgia. Neurologia. (2008) 23:259–62. [PubMed] [Google Scholar]
- 52.Sotiriou E, Apalla Z, Panagiotidou D, Ioannidis D. Severe post-herpetic neuralgia successfully treated with botulinum toxin A: three case reports. Acta Derm Venereol. (2009) 89:214–5. 10.2340/00015555-0609 [DOI] [PubMed] [Google Scholar]
- 53.Xiao L, Mackey S, Hui H, Xong D, Zhang Q, Zhang D. Subcutaneous injection of botulinum toxin a is beneficial in postherpetic neuralgia. Pain Med. (2010) 11:1827–33. 10.1111/j.1526-4637.2010.01003.x [DOI] [PubMed] [Google Scholar]
- 54.Apalla Z, Sotiriou E, Lallas A, Lazaridou E, Ioannides D. Botulinum toxin A in postherpetic neuralgia: a parallel, randomized, double-blind, single-dose, placebo-controlled trial. Clin J Pain. (2013) 29:857–64. 10.1097/AJP.0b013e31827a72d2 [DOI] [PubMed] [Google Scholar]
- 55.Attal N, de Andrade DC, Adam F, Ranoux D, Teixeira MJ, Galhardoni R, et al. Safety and efficacy of repeated injections of botulinum toxin A in peripheral neuropathic pain (BOTNEP): a randomised, double-blind, placebo-controlled trial. Lancet Neurol. (2016) 15:555–65. 10.1016/S1474-4422(16)00017-X [DOI] [PubMed] [Google Scholar]
- 56.Shackleton T, Ram S, Black M, Ryder J, Clark GT, Enciso R. The efficacy of botulinum toxin for the treatment of trigeminal and postherpetic neuralgia: a systematic review with meta-analyses. Oral Surg Oral Med Oral Pathol Oral Radiol. (2016) 122:61–71. 10.1016/j.oooo.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 57.Gadient PM, Smith JH, Ryan SJ. Herpes zoster ophthalmicus following onabotulinumtoxin A administration for chronic migraine: a case report and literature review. Cephalalgia. (2015) 35:443–8. 10.1177/0333102414544974 [DOI] [PubMed] [Google Scholar]
- 58.Guariguata L. By the numbers: new estimates from the IDF diabetes atlas update for 2012. Diabetes Res Clin Pract. (2012) 98:524–5. 10.1016/j.diabres.2012.11.006 [DOI] [PubMed] [Google Scholar]
- 59.Abbot CA, Malik RA, Van Ross ER, Kulkarmi J, Boulton AJ. Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the UK. Diabetes Care. (2011) 34:2220–4. 10.2337/dc11-1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yuan RY, Sheu JJ, Yu JM, Chen WT, Tseng IJ, Chang HH, et al. Botulinum toxin for diabetic neuropathic pain: a randomized double-blind crossover trial. Neurology. (2009) 72:1473–8. 10.1212/01.wnl.0000345968.05959.cf [DOI] [PubMed] [Google Scholar]
- 61.Chen WT, Yuan RY, Chiang SC, Sheu JJ, Yu JM, Tseng J, et al. Onabotulinum toxin A improves tactile and mechanical pain perception in painful diabetic polyneuropathy. Clin J Pain. (2013) 29:639–43. 10.1097/AJP.0b013e318255c132 [DOI] [PubMed] [Google Scholar]
- 62.Ghasemi M, Ansari M, Basiri K, Shaigannejad V. The effects of intradermal botulinum toxin type A injections on pain symptoms of patients with diabetic neuropathy. J Res Med Sci. (2014) 19:106–111. [PMC free article] [PubMed] [Google Scholar]
- 63.Lakhan SE, Velasco DN, Tepper D. Botulinum toxin-A for painful diabetic neuropathy: a meta-analysis. Pain Med. (2015) 16:1773–80. 10.1111/pme.12728 [DOI] [PubMed] [Google Scholar]
- 64.Jönsson AC, Lindgren I, Hallström B, Norrving B, Lindgren A. Prevalence and intensity of pain after stroke: a population-based study focusing on patients perspectives. J Neurol Neurosurg Psychiatry. (2006) 77:590–5. 10.1136/jnnp.2005.079145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Harrison RA, Field TS. Post stroke pain: identification, assessment, and therapy. Cerebrovasc Dis. (2015) 39:190–201. 10.1159/000375397 [DOI] [PubMed] [Google Scholar]
- 66.Camoes-Barbosa A, Neves AF. The analgesic effect of a botulinum and incobotulinum toxins type A in central poststroke pain: two case reports PM R. (2016) 8:384–7. 10.1016/j.pmrj.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 67.Shippen C, Bavikatte G, Mackarel D. The benefit of botulinum toxin A in the management of central post stroke pain: a case report. J Neurol Stroke. (2017) 6:218 10.15406/jnsk.2017.06.00218 [DOI] [Google Scholar]
- 68.Marciniak CM, Harvey RL, Gagnon CM, Duraski SA, Denby FA, McCarty S, et al. Does botulinum toxintype a decrease pain and lessen disability in hemiplegic survivors of stroke with shoulder pain and spasticity? Am J Phys Med Rehabil. (2012) 91:1007–19. 10.1097/PHM.0b013e31826ecb02 [DOI] [PubMed] [Google Scholar]
- 69.Wissel J, Ganapathy V, Ward AB, Borg J, Ertzgaard P, Herrmann C, at al. Onabotulinum toxin A improves pain in patients with post-stroke spasticity: Findings from a randomized, double-blind, placebo-controlled trial. J Pain Symptom Manag. (2016) 52:17–26. 10.1016/j.jpainsymman.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 70.Kapural L, Stillman M, Kapural M, McIntyre P, Guirgius M, Mekhail N. Botulinum toxin occipital nerve block for the treatment of severe occipital neuralgia: a case series. Pain Pract. (2007) 7:337–40. 10.1111/j.1533-2500.2007.00150.x [DOI] [PubMed] [Google Scholar]
- 71.Taylor M, Silva S, Cottrell C. Botulinum toxin type A in the treatment of occipital neuralgia: a pilot study. Headache. (2008) 48:1476–81. 10.1111/j.1526-4610.2008.01089.x [DOI] [PubMed] [Google Scholar]
- 72.Tsai CP, Liu CY, Lin KP, Wang KC. Efficacy of botulinum toxin type A in the relief of carpal tunnel syndrome: a preliminary experience. Clin Drug Investig. (2006) 26:511–5. 10.2165/00044011-200626090-00004 [DOI] [PubMed] [Google Scholar]
- 73.Breuer B, Sperber K, Wallenstein S, Kiprovski K, Calapa A, Snow B, et al. Clinically significant placebo analgesic response in a pilot trial of botulinum B in patients with hand pain and carpel tunnel syndrome. Pain Med. (2006) 7:16–24. 10.1111/j.1526-4637.2006.00084.x [DOI] [PubMed] [Google Scholar]
- 74.Fabregat G, Asensio-Samper JM, Palmisani S, Villanueva-Pérez VL, De Andrés J. Subcutaneous botulinum toxin for chronic post-thoracotomy pain. Pain Pract. (2013) 13:231–4. 10.1111/j.1533-2500.2012.00569.x [DOI] [PubMed] [Google Scholar]
- 75.Rashid S, Fields AR, Baumrucker SJ. Subcutaneous botulinum toxin injection for post-thoracotomy pain syndrome in palliative care: a case report. Am J Hosp Palliat Care. (2018) 35:511–3. 10.1177/1049909117716460 [DOI] [PubMed] [Google Scholar]
- 76.Rostami R, Mittal SO, Radmand R, Jabbari B. Incobotulinum toxin-A improves post-surgical and post-radiation pain in cancer patients. Toxins. (2016) 8:22. 10.3390/toxins8010022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gabriel A, Champaneria MC, Maxwell GP. The efficacy of botulinum toxinA in post-mastectomy breast reconstruction: a pilot study. Aesthet Surg J. (2015) 35:402–9. 10.1093/asj/sjv040 [DOI] [PubMed] [Google Scholar]
- 78.Layeeque R, Hochberg J, Siegel E, Kunkel K, Kepple J, Henry-Tillman RS, et al. Botulinum Toxin infiltration for pain control after mastectomy and expander reconstruction. Ann Surg. (2004) 240:608–13. 10.1097/01.sla.0000141156.56314.1f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Karmakar MK, Ho AM. Posthoracotomy pain syndrome. Thorac Surg Clin. (2004) 14:345–52. 10.1016/S1547-4127(04)00022-2 [DOI] [PubMed] [Google Scholar]
- 80.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: Risk factors and prevention. Lancet. (2006) 367:1618–25. 10.1016/S0140-6736(06)68700-X [DOI] [PubMed] [Google Scholar]
- 81.Bruce J, Thornton AJ, Powell R, Johnston M, Wells M, Heys SD, et al. Psychological, surgical, and sociodemographic predictors of pain outcomes after breast cancer surgery: a population-based cohort study. Pain. (2014) 155:232–43. 10.1016/j.pain.2013.09.028 [DOI] [PubMed] [Google Scholar]
- 82.Raja SN, Grabow TS. Complex regional pain syndrome I (reflex sympathetic dystrophy). Anesthesiology. (2002) 96:1254–60. 10.1097/00000542-200205000-00031 [DOI] [PubMed] [Google Scholar]
- 83.Safarpour D, Jabbari B. Botulinum toxin a (Botox) for treatment of proximal myofascial pain in complex regional pain syndrome: two cases. Pain Med. (2010) 11:1415–8. 10.1111/j.1526-4637.2010.00929.x [DOI] [PubMed] [Google Scholar]
- 84.Safarpour D, Salardini A, Richardson D, Jabbari B. Botulinum toxin A for treatment of allodynia of complex regional pain syndrome: a pilot study. Pain Med. (2010) 11:1411–4. 10.1111/j.1526-4637.2010.00897.x [DOI] [PubMed] [Google Scholar]
- 85.Caroll I, Clark D, Mackey S. Sympathetic block with botulinum toxin to treat complex regional pain syndrome. Ann Neurol. (2009) 65:348–51. 10.1002/ana.21601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kharkar S, Ambady P, Venkatesh Y, Schwartzman J. Intramuscular botulinum toxin in complex regional pain syndrome: case series and literature review. Pain Phys. (2011) 14:419–24. [PubMed] [Google Scholar]
- 87.Choi E, Cho CW, Kim HY, Lee PB, Nahm FS. Lumbar sympathetic block with botulinum toxin type B for complex regional pain syndrome: a case study. Pain Phys. (2015) 18:911–6. [PubMed] [Google Scholar]
- 88.Fishman LM, Wilkins AN, Rosner B. Electrophysiologically identified piriformis syndrome is successfully treated with incobotulinum toxin a and physical therapy. Muscle Nerve. (2017) 56:258–63. 10.1002/mus.25504 [DOI] [PubMed] [Google Scholar]
- 89.Wu H, Sultana R, Taylor BK, Szabo A. A prospective randomized double-blinded pilot study to examine the effect of botulinum toxin type A injection vs. Lidocaine/Depomedrol injection on residual and phantom limb pain. Clin J Pain. (2012) 28:108–12. 10.1097/AJP.0b013e3182264fe9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kern U, Martin C, Scheicher S, Müller H. Long-term treatment of phantom and stump pain with Botulinum toxin type A over 12 months. A first clinical observation. Nervenarzt. (2004) 75:336–40. 10.1007/s00115-003-1657-4 [DOI] [PubMed] [Google Scholar]
- 91.Siddall PJ, Loeser JD. Pain following spinal cord injury. Spinal Cord. (2001) 39:63–73. 10.1038/sj.sc.3101116 [DOI] [PubMed] [Google Scholar]
- 92.Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. (2003) 103:249–57. 10.1016/S0304-3959(02)00452-9 [DOI] [PubMed] [Google Scholar]
- 93.Jabbari B, Maher N, Difazio MP. Botulinum toxin A improved burning pain and allodynia in two patients with spinal cord pathology. Pain Med. (2003) 4:206–10. 10.1046/j.1526-4637.2003.03013.x [DOI] [PubMed] [Google Scholar]
- 94.Han ZA, Song DH, Chung ME. Effect of subcutaneous injection of botulinum toxin A on spinal cord injury-associated neuropathic pain. Spinal Cord. (2014) 52:S5–6. 10.1038/sc.2014.43 [DOI] [PubMed] [Google Scholar]
- 95.Han ZA, Song DH, Oh HM, Chung ME. Botulinum toxin type A for neuropathic pain in patients with spinal cord injury. Ann Neurol. (2016) 79:569–78. 10.1002/ana.24605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li G, Lv CA, Tian L, Jin LJ, Sun P, Zhao W. A randomized controlled trial of botulinum toxin A for treating neuropathic pain in patients with spinal cord injury. Medicine. (2017) 96:e6919. 10.1097/MD.0000000000006919 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 97.Foley JM, Finlayson H, Travlos A. A review of thoracic outlet syndrome and the possible role of botulinum toxin in the treatment of this syndrome. Toxins. (2012) 4:1223–35. 10.3390/toxins4111223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rahman A, Hamid A, Inozemtsev K, Nam A. Thoracic outlet syndrome treated with injecting botulinum toxin into middle scalene muscle and pectoral muscle interfascial planes: a case report. A Pract. (2019) 12:235–7. 10.1213/XAA.0000000000000894 [DOI] [PubMed] [Google Scholar]
- 99.Finlayson HC, O'Connor RJ, Brasher PM, Travlos A. Botulinum toxin injection for management of thoracic outlet syndrome: a double-blind, randomized, controlled trial. Pain. (2011) 152:2023–8. 10.1016/j.pain.2011.04.027 [DOI] [PubMed] [Google Scholar]
- 100.Chen CL, Meng E. Can botulinum toxin A play a role in treatment of chronic pelvic pain syndrome in female patients? clinical and animal evidence. Toxins. (2020) 12:110. 10.3390/toxins12020110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jarvis SK, Abbott JA, Lenart MB, Steensma A, Vancaillie TG. Pilot study of botulinum toxin type A in the treatment of chronic pelvic pain associated with spasm of the levator ani muscles. Aust N Z J Obstet Gynaecol. (2004) 44:46–50. 10.1111/j.1479-828X.2004.00163.x [DOI] [PubMed] [Google Scholar]
- 102.Gottsch HP, Yang CC, Berger RE. A pilot study of botulinum toxin A for male chronic pelvic pain syndrome. Scand J Urol Nephrol. (2011) 45:72–6. 10.3109/00365599.2010.529820 [DOI] [PubMed] [Google Scholar]
- 103.Falahatkar S, Shahab E, Gholamjani Moghaddam K, Kazemnezhad E. Transurethral intraprostatic injection of botulinum neurotoxin type A for the treatment of chronic prostatitis/chronic pelvic pain syndrome: results of a prospective pilot double-blind and randomized placebo-controlled study. BJU Inàt. (2015) 116:641–9. 10.1111/bju.12951 [DOI] [PubMed] [Google Scholar]
- 104.Abdel-Meguid TA, Mosli HA, Farsi H, Alsayyad A, Tayib A, Sait M, Abdelsalam A. Treatment of refractory category III nonbacterial chronic prostatitis/chronic pelvic pain syndrome with intraprostatic injection of onabotulinumtoxinA: a prospective controlled study. Can J Urol. (2018) 25:9273–80. [PubMed] [Google Scholar]
- 105.Aoki KR. A comparison of the safety margins of botulinum neurotoxin serotypes A, B, and F in mice. Toxicon. (2001) 39:1815–20. 10.1016/S0041-0101(01)00101-5 [DOI] [PubMed] [Google Scholar]
- 106.Torii Y, Sasaki M, Shin MC, Akaike N, Kaji R. Comparison of efficacy and toxicity between botulinum toxin subtypes A1 and A2 in cynomolgus macaques. Toxicon. (2018) 153:114–9. 10.1016/j.toxicon.2018.08.017 [DOI] [PubMed] [Google Scholar]