Abstract
Universal school health services are expected to offer similar, needs‐based services to all students across schools, service providers and students’ socio‐economic statuses and health needs. This study investigates access to school health nurses in Finland. The objectives were to study the differences in access to school health nurse between service providers, schools, students’ characteristics and school health nurse resources. Access was examined through a nationwide School Health Promotion study, which is a self‐reporting, voluntary and anonymous survey for 8th and 9th graders (15 to 16‐year old, N = 71865). The ethical committee of the National Institute for Health and Welfare has approved procedure for the School Health Promotion study. Data on school health nurse resources and service providers were obtained from the national database (534 schools; 144 service providers). Multilevel logistic regression was used. Of the pupils, 15% of girls and 11% of boys reported difficult access to a school health nurse. The number of adolescents who reported difficult access ranged between service providers (0%–41%) and schools (0%–75%). Students with lower socio‐economic background, poorer well‐being at school, lack of support for studying and greater health needs reported difficult access more often. School health nurse resources were associated with difficult access only among boys, when resources were under the national recommendations. These findings raise concern about equality and unmet health needs in school health services.
Keywords: access, adolescents, school health nurse, school health services, universal health care
Introduction
Adolescence is often considered to be a period of good health. However, about 12% of this age group suffers from chronic conditions and mental health disorders 1. Further, health‐compromising behaviours often begin in adolescence. The processes of physical, mental and sexual maturation in adolescence point out a need for health services tailored for this age 1, 2, 3, 4, 5. World Health Organization's 6 guidance on adolescent‐friendly services emphasises health systems that are responsive to adolescent needs with easy and equal access and appropriate care. The purpose is to reach those who are vulnerable or lack services, without discriminating anyone. Still, the way the health services for adolescents are organised, if these are organised, varies greatly between countries 7, 8, 9, 10.
School health services have the potential to offer easy access for adolescents in their everyday environment 10, 11, and school health nurses are important providers of children's and adolescents’ health services 12. In Finland, school health services are part of universal preventive health care, free of charge for pupils. They are organised by municipal service providers, which means each service provider organises services for one or more schools. Services are available mainly during school hours and are usually located at schools or in primary health care centres close to schools. School health services include regular health examinations, open‐door clinic, acute medical care for minor symptoms or injuries, some specialist care as well as the promotion of well‐being and safety at school 13, 14. For pupils, open‐door clinics offered by school health nurses are important channels to get help with health or well‐being problems 15. These clinics must be organised in a way that pupils can access them when needed, even without an appointment 16. School health nurses also counsel pupils in sexual matters and deliver contraceptives.
Equal access to school health services means that pupils have access to similar services regardless of the school adolescents attend or the municipality in which they live. It also means that those who have more health needs have access to services according to their needs. It is known that in many countries school health services are not equitably reachable or the content and resources of the services vary 17. Also in Finland, there has been variation between service providers in personnel resources which has resulted variation in meeting the recommended number of the health examinations 18, 19.
Less is known how school health services meet the different health needs of pupils. Previous studies have reported that adolescents’ difficulty in accessing health care is connected to the unmet health needs, such as diseases or health‐compromising behaviour 20, 21, or families with low income 20. Ethnicity has been found to have a connection with difficult access to care 22, 23, but results also claim that racial or ethnic differences in access do not exist 21. According to World Health Organizations’ survey, making the access to school health services equal for all groups of young people would improve the relevance of the services to pupils’ health and developmental needs 17.
We study how Finnish adolescents, from ages 14 to 16, perceive the access to school health services, specifically regarding open‐door appointments with nurses. We investigate whether there is variation among municipal service providers or schools in pupils’ self‐reported access to open‐door clinics of school health nurses. Secondly, we study whether those at risk of health and well‐being problems perceive access to school health service more difficult than those without these problems. Access to school health nurses is studied since the primary contact of the pupils regarding any health and well‐being problems would be their school health nurse. School nurses also meet with all pupils for annual health and well‐being examinations, so they are familiar to most pupils and are usually the only staff member in school health and social services who has an open‐door clinic.
Methods
Data and participants
The data were merged from two sources: (1) the School Health Promotion study (SHP) 2013 and (2) the Benchmarking System of Health Promotion Capacity Building (BSHPCB) data collection for comprehensive schools in 2013.
The School Health Promotion (SHP) study monitors 10 to 20‐year‐old's health and well‐being. The study has been conducted nationwide every second year since 1996. Participation is free of charge for pupils, schools and municipalities. All Finnish municipalities with pupils in the 8th and/or 9th grades were invited to the study, and municipals or schools decided on the participation. The data were collected via a voluntary, anonymous classroom survey in March and April in 2013. The nationwide SHP data included 84 per cent (N = 99 478) of all pupils from the 8th and 9th grade. The National Institute for Health and Welfare is responsible for the study, and its ethical committee has approved the procedure 24, 25.
The Benchmarking System of Health Promotion Capacity Building (BSHPCB) is a nationwide benchmarking tool for schools and local governments. Its purpose is to support the managing, planning and evaluating of health promotion activities. Data from comprehensive schools were collected nationwide online in digital form in October/November 2013. The data collection form was addressed to principals of all comprehensive schools, who collected the data in collaboration with a school welfare team. Data were received from 757 of the 949 (80%) schools with grades 7–9 or 1–9. The National Institute for Health and Welfare and the Finnish National Board of Education are responsible for biennially collecting the data used 26.
The data for this study were formed by combining the SHP and the BSHPCB data. The SHP data comprise responses from 8th and 9th graders from lower secondary schools. Respondents who answered less than 50% of the questions, or did not report their gender or grade, were excluded 24. All schools from the BSHPCB data that had not reported the school health nurse resource information described below were excluded (N = 48, 5548 pupils). Information on school type and the number of pupils from the BSHPCB data were used to exclude remaining special schools (N = 37 614 pupils) and schools with less than 10 respondents (N = 29, N = 122 pupils). These were excluded in order to eliminate a possible bias in the school‐level results. The final data included 534 schools (56% of the original schools’ data set) from 144 service providers’ areas, and 71 865 pupils (63% of Finnish 8th and 9th graders).
Measures
Outcome variable
The outcome variable, self‐reported access to a school health nurse, was measured by the question, “If you wanted to visit your school health nurse, physician, social worker or psychologist, how easy would it be to get an appointment? Please give an answer for each item.” The items were presented on a four‐point scale (“Very easy”; “Fairly easy”; “Fairly difficult”; “Very difficult). “Access to school health nurse” was dichotomised as difficult (“Fairly difficult” and “Very difficult”) or easy (“Fairly easy” and “Very easy”).
Predictors
Individual‐level predictors were from the SHP study and indicating common health needs and risks to well‐being based on literature 27, 28. They have been grouped by the adolescents’ socio‐demographic background, school‐related well‐being, health and health behaviours (Table 1). Before analysis, variables were dichotomised (“yes”/”no”) to make scales convergent.
Table 1.
Frequencies of individual‐level variables related to adolescents’ socio‐demographic background, school‐related well‐being and health needs among Finnish 8th and 9th graders (N = 71865)
| Individual‐level variable | Boys (N = 37 648) | Girls (N = 37 200) | ||
|---|---|---|---|---|
| % | N | % | N | |
| Socio‐demographic background | ||||
| Immigrant background | 3.2 | 1129 | 2.2 | 804 |
| Does not live with mother and father | 30.6 | 10471 | 32.4 | 11,521 |
| Parent unemployed | 27.7 | 9595 | 29.3 | 10,500 |
| Parents have no high education | 58.4 | 20790 | 58.4 | 21,187 |
| Discussion difficulties with parents | 6.9 | 2397 | 9.7 | 3,465 |
| School‐related well‐being | ||||
| Academic performance under average | 59.7 | 21047 | 37.6 | 13,541 |
| Lack of support from school for studying | 22.3 | 7730 | 23.2 | 8,238 |
| Lack of support from home for studying | 14.3 | 4941 | 18.1 | 6,408 |
| Health needs | ||||
| Heavy drinking | 12.9 | 4528 | 11.4 | 4,105 |
| Sexual intercourse | 21.6 | 7390 | 22.2 | 7,794 |
| Perceived health moderate or bad | 12.6 | 4464 | 19.0 | 6,884 |
| Daily health complaint | 22.6 | 7500 | 42.1 | 14,591 |
| School burnout | 11.3 | 3986 | 14.3 | 5,167 |
| Bullied weekly | 7.6 | 2674 | 6.3 | 2,284 |
Adolescents’ socio‐demographic backgrounds were described using five dichotomous items. Birth country was measured with the question, “In which country were you and your parents born?” with several alternatives. The variable was dichotomised to “Immigrant background” (adolescents’ birth country other than Finland) and “Others” (birth country Finland). Living conditions were measured by the question, “Who are the adults you live with? Choose the option that best describes your situation”, and the variable was dichotomised as “Does not live with mother and father” (“my mother and my father alternately, my parents don't live together”; “only my mother”; “only my father”; “my father/mother and his/her partner”; “one or more other adults”; “none of the above”) and “Others” (“my mother and my father”).
The employment status of parents was measured with the question, “During the past year, have your parents been unemployed of laid‐off?” and dichotomised as “Parent unemployed” (“one of my parents”; “both parents”) and “Others” (“neither of my parents”). The education of parents was asked about with the question, “What is the highest educational level your parents have achieved?” The items were dichotomised as “Parents have no higher education” (Comprehensive school or primary school; upper secondary school or vocational education institution; occupational studies in addition to upper secondary school or vocational education institution; no education; also, if education was not reported) and “Others” (university, university of applied sciences or other higher education institution).
Adolescents’ relationships with their parents were described by “Discussion difficulties with parents”. The original question was “Can you talk about things that concern you with your parents?” and the alternatives were dichotomised as “Discussion difficulties with parents” (“hardly ever”; “every once and a while”) and “Others” (“fairly often”; “often”). The age and grade of the pupils were not considered in the analysis because of the small amount of variation between respondents; pupils were in 8th or 9th grade and mainly 15–16 years old.
School‐related well‐being was described by three dichotomous items. Academic performance, which was asked by the question, “What was your average grade (all subjects) on your latest school report?” was dichotomised to “Academic performance under average” (alternatives “<6.5”; “6.5–6.9”; “7.0–7.4”; “7.5–7.9”) and “Others” (alternatives “8.0–8.4”; “8.5–8.9”; “9.0–9.4”; “9.5–10.0”). “Lack of support from school for studying” or “Lack of support from home for studying” were originally measured by the question, “If you have difficulties at school or with your school work, how often do you get help? Please give an answer for both items.” with a four‐point scale (“Whenever I need”; “on most occasions”; “rarely”; “hardly ever”) for both “at school” and “at home”. The items were dichotomised as “Lack of support from school/home for studying” (“rarely”; “hardly ever”) and “Others” (“whenever I need”; “on most occasions”).
Adolescents’ health needs were described using six items. General alcohol consumption was one topic explored (“On the whole, how often do you consume alcohol, a half‐bottle of beer or more, for example?”), and evaluated with a scale (“once a week or more often”; “a couple of times a month”; “about once a month”; “not very often”; “I do not consume alcoholic beverages.”). Drinking habits were asked about (“How often do you use alcohol to get heavily drunk?”) and evaluated on a scale (“Once a week or more often”; “About 1 to 2 times a month”; “Not very often; “Never”). These were dichotomised into a sum variable “Heavy drinking” (those who reported in the first question consuming alcohol and in the second question using it to get heavily drunk at least once a month) and “Others” (those who reported consuming alcohol to get heavily drunk less than once a month or did not reported consuming no alcohol at all). Sexual intercourse was measured by the question, “Have you had sexual intercourse?” and dichotomised to “Sexual intercourse” (If they answered yes, they were to respond to the follow‐up question “Yes, on how many occasions? Once; 2 to 4 times; 5 to 9 times; 10 times or more”) and “Others” (“No”).
Health status was measured with the question, “How is your health in general? Is it very good; fairly good; moderate; fairly or very bad?” The responses were dichotomised as “Perceived health moderate or bad” (“Moderate”; “Fairly or very bad”) and “Others” (“Very good”; Fairly good”). Daily health complaints during the previous 6 months were also included in the analysis. Pupils were asked, “In the last six months, have you experienced any of the following symptoms, and how often? Please give an answer for each item: Neck or shoulder pain; lower back pain; abdominal pain; tenseness or anxiety; irritability or bouts of anger; trouble falling asleep, waking up during the night; headache; tiredness or dizziness.” Each item was measured on a four‐point scale (“Seldom or never”; “About once a month”; “About once a week”; “Almost every day”), and responses were dichotomised as “Daily health complaints” (“Almost every day”) and “Others” (“Seldom or never”; “About once a month”; “About once a week”). Those who reported at least one daily health complaint were grouped into the “Daily health complaint” category and the rest to “Others”.
Sum variable “School burnout” was based on the School Burnout Inventory (SBI) 29. Pupils were originally asked, “Have you had any of the following feelings relating to school work? Please give an answer for each item.” The alternatives were “I feel overwhelmed by school work”; “It feels that there is no point in studying” and “I feel inadequate at my studies”. Every alternative was scored (“Hardly ever” and “A few times a month” = 0 points; “A few days a week” = 1 point, “Almost daily” = 2 points). Those who got from 3 to 6 points were grouped into the “School burnout” category, and those receiving less than 3 points were labelled as “Others”.
Bullying was studied by asking a question “How often have you been bullied at school during this semester?” with a four‐point scale (“Several times a week”; “about once a week”; “rarely”; “not at all”). The responses were dichotomised as “Bullied weekly” (“Several times a week”; “About once a week”) and “Others” (“Rarely”; “Not at all”).
School health nurse resources
School health nurse resources were from the BSHPCB data. The original question measured school health nurse resources in monthly working hours or monthly working days. These resources were transformed to person‐years. The figures were proportioned to 100 pupils. The variable describing the school health nurse‐to‐pupil ratio was categorised into the following groups: 0–400 pupils; 401–500 pupils; 501–600 pupils; over 600 pupils/school health nurse. The national recommendation is at most 600 pupils per one full‐time school health nurse 30, which means 20 days or 140.25 hours per month. For example, the local circumstances, adolescents’ need for special support and the availability of a school psychologist and social worker are taken into account when allocating the resources 30.
Design and analyses
Individual‐level variables were first examined with frequencies (Table 1). For further analysis, we used a multilevel logistic regression model because of the data's hierarchical nature; each service provider organised the services at one or more school and each school had multiple pupils. The service providers and schools were included in the model as random effects. Multilevel analysis was used to evaluate pupil and school‐level factors as fixed effects on the self‐reported access, a pupil‐level outcome variable.
Analyses were performed separately for boys and girls due to variation in individual‐level variables. The variables were brought into the model in the following order: 1. Service provider, 2. School, 3. Predictors, including both individual‐level variables and school health nurse resources. The predictors’ associations with difficult access was studied with both bivariate and multivariate analysis. Service providers and schools were included in the analysis to study possible variation within them and to adjust for their random effects. The standard deviation describes their unexplained variation in self‐reported access; the bigger the value, the greater the variation. The marginal and conditional coefficients of determination represent the variance explained after each variable group was included in the model 31. The marginal coefficient of determination describes how the fixed predictors explain the variation in the self‐reported access. The conditional coefficient of determination describes how the whole model explains the same variation. The strength of each predictors’ association with access to a school health nurse is shown in an odds ratio (OR).
The analyses were conducted with R software, version 3.3.1 32, package lme4 33. The marginal and conditional coefficients of determination were calculated with Lefcheck's 34 function rsquared.glmm. The level of significance was set at 0.05.
Results
Equality in access to a school health nurse by service providers and schools
Most adolescents reported that access to a school health nurse was easy (Table 2). Of the pupils, 13% reported that access was rather or very difficult. Girls reported difficult access more often than boys (15% and 11%, respectively).
Table 2.
Access to school health services among Finnish 8th and 9th graders in lower secondary schools (N = 71865)
| Access to school health nurse | Boys (N = 35 580) | Girls (N = 36 285) | All (N = 71 865) |
|---|---|---|---|
| Very easy | 44.6% | 36.8% | 40.7% |
| Rather easy | 44.1% | 48.1% | 46.1% |
| Rather difficult | 8.1% | 12.2% | 10.2% |
| Very difficult | 3.1% | 2.9% | 3.0% |
| 100.0% | 100.0% | 100.0% |
The self‐reported access varied depending on the service provider and school (Figure 1). The proportion of adolescents who reported access to a school health nurse as being difficult ranged between service providers from 0 to 41%. Among schools, the number ranged between 0 and 75%.
Figure 1.
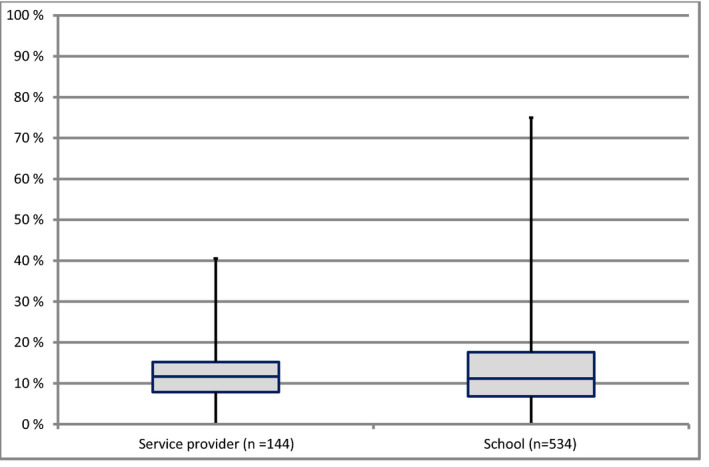
Boxplots representing the amount of adolescents (%) who reported difficult access to school health nurse by service providers (N = 144) and schools (N = 534). Box = 25th and 75th percentiles, line = median, bars = min and max values.
In the model with the service provider as the only predictor, the standard deviation of the random effect was 0.49 for boys and 0.58 for girls. When the school was added to the model, the standard deviation of the random effect on the service provider declined among both boys (0.17) and girls (0.18). The standard deviation of the random effect on the school was higher, 0.68 for boys and 0.87 for girls, implying most of the unexplained variation lay on the school level rather than on the level of the service provider. All selected predictors together had little effect on the standard deviation of the random effects. The variation between service providers slightly increased among boys (SD 0.19) and decreased among girls (SD 0.15), while the variation between schools slightly increased in both models (among boys to 0.72 and among girls to 0.89).
Access to school health nurses and risks to adolescent health and well‐being
The variation between pupils in self‐reported access to a school health nurse was studied further with bivariate and multivariate models. The first model including service providers only explained 7% of boys’ (Table 3) and 9% of girls’ (Table 4) variation in difficult access. After including schools, the model explained 13% of variation among boys and 19% among girls. Second, the individual‐level variables and school health nurse resources explained some of the variation in difficult access between adolescents. After including them, the whole multivariate model explained 20% of boys’ and 23% of girls’ variation in self‐reported access to a school health nurse.
Table 3.
Associations between difficult access to a school health nurse and adolescents’ socio‐demographic background, school‐related well‐being, health needs or school health nurse resources among boys
| Model 1 Service provider | Model 2 School | Bivariate models | Multivariate model | |
|---|---|---|---|---|
| (N = 35 580) | (N = 35 580) | (n = 34 118–35 580) | (N = 29 353) | |
| (Intercept) | 0.11 (0.10–0.12) | 0.11 (0.10–0.12) | 0.06 (0.05–0.07) | |
| School health nurse resources (pupils/school health nurse) | ||||
| Under 400 (ref) | ||||
| 400–500 | 1.15 (0.96–1.38) | 1.18 (0.96–1.45) | ||
| 501–600 | 1.01 (0.82–1.23) | 1.06 (0.84–1.32) | ||
| Over 600 | 1.23 (1.00–1.51) | 1.32 (1.06–1.65) | ||
| Adolescents’ socio‐demographic background | ||||
| Immigrant background (ref: born in Finland) | 2.55 (2.20–2.97) | 1.32 (1.08–1.62) | ||
|
Does not live with mother and father (ref: Lives with mother and father) |
0.81 (0.75–0.87) | 0.91 (0.83–0.99) | ||
|
Parent unemployed (ref: Parent employed) |
1.19 (1.10–1.28) | 1.02 (0.93–1.11) | ||
|
Parents have no higher education (ref: At least one parent has higher education) |
0.97 (0.90–1.04) | 1.06 (0.97–1.15) | ||
|
Discussion difficulties with parents (ref: Can discuss concerns with parents often) |
2.80 (2.53–3.12) | 1.50 (1.31–1.73) | ||
| Adolescents’ School‐related well‐being | ||||
|
Academic performance under average (ref: Academic performance at least average level) |
0.93 (0.87–1.00) | 1.24 (1.14–1.35) | ||
|
Lack of support from school for studying (ref: Support from school for studying at least on most occasions) |
4.47 (4.05–4.92) | 2.64 (2.31–3.02) | ||
|
Lack of support from home for studying (ref: Support from home for studying at least on most occasions) |
2.74 (2.44–3.08) | 1.02 (0.87–1.20) | ||
| Adolescents’ health needs | ||||
|
Heavy drinking at least once a month (ref: Heavy drinking less than once a month or not at all) |
1.91 (1.75–2.09) | 1.11 (0.98–1.25) | ||
|
Sexual intercourse (ref: No sexual intercourse) |
1.79 (1.65–1.93) | 1.26 (1.14–1.39) | ||
|
Perceived health moderate or bad (ref: Perceived health fairly or very good) |
1.97 (1.80–2.15) | 1.29 (1.16–1.44) | ||
|
School burnout (ref: No school burnout) |
3.30 (3.03–3.59) | 1.83 (1.63–2.05) | ||
|
Bullied weekly (ref: Bullying less than weekly or not at all) |
2.41 (2.18–2.67) | 1.42 (1.25–1.62) | ||
|
Daily health complaint (ref: Health complaints less than daily or not at all) |
2.10 (1.95–2.26) | 1.28 (1.17–1.41) | ||
| Coefficient of Determination | ||||
| Marginal R² | 0.000 | 0.000 | 0.0003–0.037 | 0.068 |
| Conditional R² | 0.068 | 0.129 | 0.128–0.164 | 0.202 |
| Random effects Std Dev | ||||
| School (N = 534) | 0.676 | 0.669–0.686 | 0.718 | |
| Service provider (N = 144) | 0.492 | 0.168 | 0.161–0.208 | 0.190 |
Associations presented as odds ratio (95% confidence interval). Models adjusted for service provider and school. Ref = reference group. Significant odds ratios (OR) are presented in bold (p < 0.05).
Table 4.
Associations between difficult access to a school health nurse and adolescents’ socio‐demographic background, school‐related well‐being, health needs or school health nurse resources among girls
| Model 1 Service provider | Model 2 School | Bivariate models | Multivariate model | |
|---|---|---|---|---|
| (N = 36 285) | (N = 36 285) | (n = 35 170–36 285) | (N = 32 165) | |
| (Intercept) | 0.15 (0.13–0.16) | 0.14 (0.12–0.15) | 0.12–0.15 (0.11–0.16) | 0.08 (0.06–0.09) |
| School health nurse resources (pupils/school health nurse) | ||||
| Under 400 (ref) | ||||
| 400–500 | 1.20 (0.96–1.49) | 1.20 (0.96–1.51) | ||
| 501–600 | 1.11 (0.87–1.41) | 1.09 (0.85–1.40) | ||
| Over 600 | 1.22 (0.96–1.55) | 1.18 (0.92–1.52) | ||
| Adolescents’ socio‐demographic background | ||||
|
Immigrant background (ref. group: born in Finland) |
1.44 (1.19–1.73) | 1.25 (1.01–1.55) | ||
|
Does not live with mother and father (ref: Lives with mother and father) |
0.96 (0.90–1.02) | 1.04 (0.97–1.12) | ||
|
Parent unemployed (ref: Parent employed) |
1.07 (1.00–1.15) | 1.00 (0.93–1.07) | ||
|
Parents have no higher education (ref: At least one parent has higher education) |
1.09 (1.02–1.16) | 1.13 (1.06–1.22) | ||
|
Discussion difficulties with parents (ref: Can discuss concerns with parents often) |
1.84 (1.68–2.02) | 1.33 (1.20–1.48) | ||
| Adolescents’ school‐related well‐being | ||||
|
Academic performance under average (ref: Academic performance at least average level) |
1.04 (0.98–1.11) | 1.23 (1.14–1.33) | ||
|
Lack of support from school for studying (ref: Support from school for studying at least on most occasions) |
2.54 (2.28–2.84) | 1.63 (1.43–1.85) | ||
|
Lack of support from home for studying (ref: Support from home for studying at least on most occasions) |
2.09 (1.88–2.32) | 1.29 (1.13–1.46) | ||
| Adolescents’ health needs | ||||
|
Heavy drinking at least once a month (ref. group: Heavy drinking less than once a month or not at all) |
1.38 (1.26–1.51) | 1.07 (0.96–1.19) | ||
|
Sexual intercourse (ref: No sexual intercourse) |
1.25 (1.16–1.34) | 1.08 (0.99–1.17) | ||
|
Perceived health moderate or bad (ref: Perceived health fairly or very good) |
1.59 (1.48–1.70) | 1.21 (1.12–1.32) | ||
|
School burnout (ref: No school burnout) |
1.95 (1.81–2.11) | 1.45 (1.32–1.59) | ||
|
Bullied weekly (ref: Bullying less than weekly or not at all) |
1.47 (1.31–1.65) | 1.01 (0.89–1.15) | ||
|
Daily health complaint (ref: Health complaints less than daily or not at all) |
1.56 (1.47–1.66) | 1.30 (1.21–1.40) | ||
| Coefficient of Determination | ||||
| Marginal R² | 0.000 | 0.000 | 0.00009–0.013 | 0.032 |
| Conditional R² | 0.092 | 0.192 | 0.192–0.206 | 0.225 |
| Random effects Std Dev | ||||
| School (N = 534) | 0.8663 | 0.864–0.875 | 0.8945 | |
| Service provider (N = 144) | 0.5766 | 0.1752 | 0.162–0.199 | 0.1447 |
Associations presented as odds ratio (95% confidence interval). Models adjusted for service provider and school. Ref = reference group. Significant odds ratios (OR) are presented in bold (p < 0.05).
Tables 3 and 4 show the association between difficult access and the fixed predictors. The bivariate models show that many predictors describing adolescents’ backgrounds, well‐being or health needs have association with difficult access. In the multivariate model, when all predictors are taken into account, most of those associations remain.
When looking at background variables, the risk for difficult access was higher among those who had an immigration background or difficulties in discussion with parents, among girls whose parents had no higher education. Among boys, those who lived outside of a nuclear family had a lower risk for difficult access, meaning that boys in nuclear families actually had a higher risk. Parents’ unemployment had no statistically significant connection with perceived access.
Variables related to school‐related well‐being had the strongest association with difficult access. Those who had weaker academic performance or a lack of support from school for studying difficulties were more likely to report difficult access. Among girls, a lack of support from home for studying difficulties had a similar connection.
Adolescents’ health needs were also associated with difficult access. Those whose perceived health was moderate or bad and those who had daily health complaints or school burnout reported difficult access more often than others. Among boys, the odds were higher among those who were bullied on a weekly basis or had experienced sexual intercourse. Heavy drinking was not associated with difficult access.
The association between different school health nurse resources and difficult access was quite low in both the bivariate and multivariate models (Tables 3 and 4). A higher risk for difficult access was found among boys only when resources were under national recommendations, i.e., more than 600 pupils per one school health nurse.
Discussion
According to the results, school health services are well accessible; 87% of adolescents reported access to school health nurses as being easy. Still, 11% of boys and 15% of girls felt access was difficult. The portion of adolescents who perceived difficult access varied from 0% to 41% between service providers and from 0% to 75% between schools. Further analysis showed that many adolescents who had health and well‐being problems perceived access as more difficult. The whole multivariate model explained 20% of variation between boys and 23% of variation between girls.
The variation in difficult access by service providers, schools and adolescents might reflect the previous inequality in school health services 17, 18, 19. Although, as expected, schools explained the variation between individuals more than between service providers, school health resources had an interesting association with difficult access only among boys when the national recommendation was not met. Better resources had no association with access. When considering this result, one should remember that there was no information available on how these resources were allocated. As noted by Telljohann et al. 35, access to school‐based health care in schools with part‐time nurses may not be as adequate as in schools with full‐time nurses. On the other hand, Tylee et al. 28 noted that school health services might be inaccessible for several reasons, even if there were enough resources. According to a recent study, Finnish school health services have the possibility to intervene in children's health issues, but there are problems in entering care, and annual health examinations and their reporting use up a major part of the school health nurse resources 36. Currently, 61% of schools fulfil the national recommendations for school health nurse resources 37. The association between the availability of school health services and the allocation of resources needs further studying.
Finnish adolescents have the right to access school health services when needed 16. Still, our study shows that many factors describing school well‐being or health needs are associated with difficult access. For example, adolescents with daily health complaints or school burnout perceived access to school health services as more difficult. These results are in line with the previous finding that teenagers have health‐related problems, especially mental health needs, which are not necessarily met by current services 5. These results are even more worrying considering that discussion difficulties with parents and the lack of support for studying difficulties were also associated with difficult access. Adolescents need support during physical, mental and sexual maturation 1, 2, 3, 4, 5. Appropriate adolescent‐friendly services with easy and equal access are strongly needed 6, especially when support from home is not guaranteed. The association between health needs and access to school‐based care needs more research.
Our findings showed that access to Finnish universal school health services is not strongly related to socioeconomic status. Parents’ employment rate had no association with difficult access, and parents’ lower education was associated with it only among girls. Still, background was shown to matter; adolescents with an immigrant background had a higher risk for perceiving the access as difficult. According to previous studies, racial or ethnic disparities may exist in health care but not necessarily in school health services 21, 22. It is known that first generation immigrants have more problems in health and well‐being than others 23. Compared to older groups, young immigrants more often have experiences related to insecurity, and school activities may promote their social relationships and strengthen perceived safety 38. Overall, it would be beneficial to study more immigrant adolescents’ experiences of school health services and support their well‐being at school.
Even though many variables related to health complaints or concerns were found to be connected with difficult access, there were some exceptions. Our study found no association between health‐compromising behaviour—in our study heavy drinking—and access to universal school health services. Interestingly, boys with experience of sexual intercourse perceived access to a school health nurse more difficult than girls. In Finland, adolescents can get counselling concerning sexual health and contraceptives from school health services 10. Future research should focus on gender equality in sexual counselling in school health services.
Even though many pupils’ perceived access to school health services easy, difficult access does not tell whether adolescents received help in the end. Our findings raise the concern of unmet health needs. Adolescents may not even seek help if they perceive access as difficult. Equality in access to school health services would improve the services in responding better to pupils’ health and developmental needs 17. According to Borup and Holstein, many adolescents reflect the health dialogue they have with school nurse and follow the advice they get, pupils from lower social classes even more than others 39. School health services, which have the potential to promote pupils’ health and well‐being in their everyday environment, should be developed to be more adolescent‐friendly.
Limitations
This study is based mainly on the School Health Promotion study data, which represents most of Finnish lower secondary schools and 8th and 9th graders. The study is anonymous and voluntary, which increases the reliability. Still some limitations should be considered. There were some non‐responses, mainly when pupils were absent from school or disabled to participate in the survey independently because of a disability or weak knowledge of language 24. Furthermore, pupils from special needs schools and schools that did not provide information on school health nurse resources, and schools that would have had less than 10 pupils in the study, were excluded from this research. Also the dichotomisation of the variables may have caused a loss of some detailed information on how different variables are associated with difficult access. Still, selected predictors described the overall health needs and risk behaviour. Also, since most children in Finland attend public schools, the data represent the whole country and all socio‐economic groups. However, as school health services are organised in several ways 7, 8, 9, 10, our results can mainly be generalised to universal health care systems.
Implications for school nursing practice
School‐related well‐being and overall support from both school and home are associated with perceived access to school health services. This means that when meeting students, school health nurses should put more attention on comprehensive well‐being, including their family situation and school performance, and not only on traditional health matters. Teamwork between teachers and school health nurses could help to identify problems related to school, and contact with parents could help identify home‐related problems. A Finnish innovation, Comprehensive health examination 10, where parents are invited and the teachers’ assessment of a student is requested, would be useful in the school nurse practice.
Open‐door clinics held by school nurses are important for everyday needs for students. Particularly for adolescents, health and well‐being needs, e.g. mental problems or contraception, are often “urgent” because of their developmental phase. When the school health nurse is not on site until the following week, it does not satisfy these needs. New digital online options could be used in addition to necessary open‐door clinic hours.
A majority of students reported access to school health services as easy or fairly easy, but there was a remarkable variation between schools. This raises the question of the allocation of school health nurse resources between schools. Schools are not homogeneous in the socio‐economic structure (e.g. parents’ education, children with special needs), other resources or students’ performance. The educational authorities could allocate the resources so that those schools get more school nurse resources. For many years, the City of Helsinki has used educational policy where school resources are allocated partly according to a need‐based index 40.
Adolescent‐friendly services are supposed to involve adolescents in the planning and monitoring of services 6. As adolescents are probably eager to give their opinions on services and various well‐being needs, routine surveys could give information to help develop access to school health services. This could be organised, even school‐based. Examples of such feedback systems in Finland are the School Health Promotion Study 24, 25, which collects school‐based data nationally every second year, and the Benchmarking System of Health Promotion Capacity Building 26, which also collects school‐based data.
Conclusion
Access to Finnish school health services was mainly reported to be easy. Still, 13% of adolescents reported access as being difficult, and there was variation by service providers and schools even after several factors were adjusted for. Difficult access to a school health nurse was explained by selected variables in 20% of the variation in boys and 23% of the variation in girls. Several variables describing adolescents’ health needs were found to be associated with perceived difficult access to school health nurses. These results might reflect previously found inequality in access to school health services 7, 8, 17. It is crucial to continue the study of the association between school health service resources, for example the amount of open‐door service, and equality in access. Further studies are needed to recognise barriers to school health services in securing adolescent‐friendly services and healthy adulthood.
Author contributions
All authors contributed to the concept and design of the study. VS and HK performed data analyses. HK, VS, TS and AR contributed to drafting of the manuscript. All the authors read, critically reviewed and approved the manuscript.
Acknowledgements
The authors thank all adolescents and principals, who participated in the original surveys. The first author was supported by grants from the Juho Vainio Foundation and the Competitive State Research Financing of the Expert Responsibility Area of Tampere University Hospital (Grant 9P063 and 9T055). The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Scand J Caring Sci; 2019; 33; 165–175 Access to a school health nurse and adolescent health needs in the universal school health service in Finland
References
- 1. Sawyer SM, Drew S, Yeo MS, Britto MT. Adolescents with a chronic condition: challenges living, challenges treating. Lancet 2007; 369: 11481–9. [DOI] [PubMed] [Google Scholar]
- 2. Mokdad AH, Forouzanfar MH, Daoud F, Mokdad AA, Bcheraoui CE, Moradi‐Lakeh M, Kyu HH, Barber RM, Wagner J, Cercy K, Kravitz H, Coggeshall M, Chew A, O'Rourke KF, Steiner C, Tuffaha M, Charara R, Al‐Ghamdi EA, Adi Y, Afifi RA, Alahmadi H, AlBuhairan F, Allen N, AlMazroa M, Al‐Nehmi AA, AlRayess Z, Arora M, Azzopardi P, Barroso C, Basulaiman M, Bhutta ZA, Bonell C, Breinbauer C, Degenhardt L, Denno D, Fang J, Fatusi A, Feigl AB, Kakuma R, Karam N, Kennedy E, Khoja TA, Maalouf F, Obermeyer CM, Mattoo A, McGovern T, Memish ZA, Mensah GA, Patel V, Petroni S, Reavley N, Zertuche DR, Saeedi M, Santelli J, Sawyer SM, Ssewamala F, Taiwo K, Tantawy M, Viner RM, Waldfogel J, Zuñiga MP, Naghavi M, Wang H, Vos T, Lopez AD, Al Rabeeah AA, Patton GC, Murray CJL. Global burden of diseases, injuries, and risk factors for young people's health during 1990‐2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016; 387: 2383–401. [DOI] [PubMed] [Google Scholar]
- 3. Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public‐health challenge. Lancet 2007; 369: 1302–13. [DOI] [PubMed] [Google Scholar]
- 4. Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, Arora M, Azzopardi P, Baldwin W, Bonell C, Kakuma R, Kennedy E, Mahon J, McGovern T, Mokdad AH, Patel V, Petroni S, Reavley N, Taiwo K, Waldfogel J, Wickremarathne D, Barroso C, Bhutta Z, Fatusi AO, Mattoo A, Diers J, Fang J, Ferguson J, Ssewamala F, Viner RM. Our future: a Lancet commission on adolescent health and wellbeing. Lancet 2016; 387: 2423–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Patton GC, Viner R. Pubertal transitions in health. Lancet 2007; 369: 1130–9. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization . Adolescent Friendly Health Services. An agenda for Change. 2002, http://apps.who.int/iris/bitstream/10665/67923/1/WHO_FCH_CAH_02.14.pdf. (last accessed 15 December 2017).
- 7. Baltag V, Levi M. Organizational models of school health services in the WHO European Region. J Health Organ Manag 2013; 6: 733–46. [DOI] [PubMed] [Google Scholar]
- 8. Baltag V, Pachyna A, Hall J. Global overview of school health services: data from 102 countries. Health Behav Policy Rev 2015; 4: 268–83. [Google Scholar]
- 9. Crowley R, Armour‐Marshall J, Wolfe I. Young people's health and health services Chapter seven. European Observatory on Health System and Policies. European Child Health Services and Systems: Lessons without borders (Wolfe I, McKee M. eds), 2013, Open University Press, Maidenhead, 183–96. http://www.euro.who.int/__data/assets/pdf_file/0003/254928/European-Child-Health-Services-and-Systems-Lessons-without-borders.pdf, (last acccessed 15 December 2017). [Google Scholar]
- 10. Rimpelä A, Caan W, Bremberg S, Wiegersma PA, Wolfe I. Schools and the health of children and young people Chapter six. European Observatory on Health System and Policies. European Child Health Services and Systems: lessons without borders (Wolfe I, McKee M. eds), 2013, Open University Press/McGraw‐Hill, Maidenhead, 146–82. http://www.euro.who.int/__data/assets/pdf_file/0003/254928/European-Child-Health-Services-and-Systems-Lessons-without-borders.pdf (last accessed 15 December 2017). [Google Scholar]
- 11. Soleimanpour S, Geierstanger SP, Kaller S, McCarter V, Brindis CD. The Role of School Health Centers in Health Care Access and Client Outcomes. Am J Public Health 2010; 100: 1597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Council on School Health . Role of the school nurse in providing school health services. Pediatrics 2008; 5: 1052–6. [DOI] [PubMed] [Google Scholar]
- 13. Health Care Act 1326/2010. Ministry of Social Affairs and Health, Finland. Finlex, http://www.finlex.fi/en/laki/kaannokset/2010/en20101326.pdf (last accessed 15 December 2017).
- 14. Government Decree 338/2011 on maternity and child health clinic services, school and student health services and preventive oral health services for children and youth. Finlex, http://www.finlex.fi/en/laki/kaannokset/2011/en20110338.pdf, (last accessed 15 December 2017).
- 15. National Institute for Health and Welfare . Terveydenhoitaja (The public health nurse), 2017. https://www.thl.fi/fi/web/lapset-nuoret-ja-perheet/peruspalvelut/opiskeluhuolto/kouluterveydenhuolto/toimijat/terveydenhoitaja (last accessed 15 December 2017).
- 16. Oppilas‐ ja opiskelijahuoltolaki 1287/2013. (Pupil and Student Welfare Act.) Ministry of Social Affairs and Health, Finland. Finlex, http://www.finlex.fi/fi/laki/smur/2013/20131287 (last accessed 15 December 2017).
- 17. WHO Regional Office for Europe . Pairing children with health services. The results of a survey on school health services in the WHO European Region, 2010, www.euro.who.int/__data/assets/pdf_file/0006/112389/E93576.pdf (last accessed 15 December 2017).
- 18. Wiss K, Frantsi‐Lankia M, Pelkonen M, Saaristo V, Ståhl T. Neuvolatoiminta, koulu‐ ja opiskeluterveydenhuolto sekä lasten ja nuorten ehkäisevä suun terveydenhuolto 2014. Asetuksen (338/2011) toimeenpanon seuranta ja valvonta. Ohjaus 21/2014. (Maternity and child health clinics, school and student health care and oral health care for children and young people 2014 – Follow‐up and monitoring of the implementation of the Decree (338/2011) Directions 21/2014.) 2014, National Institute for Health and Welfare, Helsinki, http://urn.fi/URN:ISBN:978-952-302-356-7 (last accessed 15 December 2017).
- 19. Wiss K, Hakamäki P, Hietanen‐Peltola M, Koskinen H, Laitinen K, Manninen M, Saaristo V, Ståhl T. Hyvinvoinnin ja terveyden edistäminen peruskouluissa – TEA 2015. Tilastokatsaus 2/2016. (Promotion of wellbeing and health in comprehensive schools – TEA 2015). 2016, National Institute for Health and Welfare and Finnish National Agency for Education, http://urn.fi/URN:NBN:fi-fe2016051111637 (last accessed 15 December 2017).
- 20. Ford CA, Bearman PS, Moody J. Foregone health care among adolescents. JAMA 1999; 23: 2227–34. [DOI] [PubMed] [Google Scholar]
- 21. Parasuraman SR, Shi L. Differences in access to care among students using school‐based health centers. J Sch Nurs 2015; 4: 291–9. [DOI] [PubMed] [Google Scholar]
- 22. Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: has anything changed over the years? Int J Equity Health 2013; 12: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Matikka A, Luopa P, Kivimäki H, Jokela J, Paananen R. The well‐being of eight‐year and ninth‐year pupils with an immigrant background ‐ School Health Promotion Study 2013. Discussion paper 6/2015. 2015, National Institute for Health and Welfare, Helsinki, http://urn.fi/URN:ISBN:978-952-302-434-2 (last accessed 15 December 2017).
- 24. Luopa P, Kivimäki H, Matikka A, Vilkki S, Jokela J, Laukkarinen E, Paananen R. Nuorten hyvinvointi Suomessa 2000–2013. Kouluterveyskyselyn tulokset. (Wellbeing of adolescents in Finland 2000‐2013. The results of the School Health Promotion study.) Report 25/2014. 2014, The National Institute for Health and Welfare, Helsinki, http://urn.fi/URN:ISBN:978-952-302-280-5 (last accessed 15 December 2017).
- 25. National Institute for Health and Welfare . School Health Promotion study, https://www.thl.fi/fi/web/thlfi-en/research-and-expertwork/population-studies/school-health-promotion-study (last accessed 15 December 2017).
- 26. National Institute for Health and Welfare . TEAviisari, https://www.teaviisari.fi/teaviisari/en/index (last accessed 15 December 2017).
- 27. Konu A, Rimpelä M. Well‐being in schools: a conceptual model. Health Promot Int 2002; 1: 79–87. [DOI] [PubMed] [Google Scholar]
- 28. Tylee A, Haller DM, Graham T, Churchill R, Sanci LA. Youth‐ friendly primary‐ care services: how are we doing and what more needs to be done? Lancet 2007; 9572: 1565–73. [DOI] [PubMed] [Google Scholar]
- 29. Salmela‐Aro K, Kiuru N, Leskinen E, Nurmi J‐E. School‐burnout inventory (SBI). Reliability and validity. Eur J Psychol Assess 2009; 1: 48–57. [Google Scholar]
- 30. Ministry of Social Affairs . Kouluterveydenhuollon laatusuositus. Sosiaali‐ ja terveysministeriön oppaita 2004:8 (Quality Recommendation for School Health Care. Handbooks of the Ministry of Social Affairs and Health 2004:8. 2004, Helsinki, http://urn.fi/URN:NBN:fi-fe201504225962 (last accessed 15 December 2017). [Google Scholar]
- 31. Nakagawa S, Schielzeth A. A general and simple method for obtaining R2 from generalized linear mixed‐effects models. Methods Ecol Evol 2013; 2: 133–42. [Google Scholar]
- 32. R Core Team . R: A Language and Environment for Statistical Computing. 2015, R Foundation for Statistical Computing, Vienna, Austria: http://www.R-project.org (last accessed 15 December 2017). [Google Scholar]
- 33. Bates D, Maechler M, Bolker B, Walker S. Fitting linear mixed‐effects models using lme4. J Stat Softw 2015; 1: 1–48. [Google Scholar]
- 34. Lefcheck JS. PiecewiseSEM: piecewise structural equation modeling in R for ecology, evolution, and systematics. Methods Ecol Evol 2015; 5: 573–9. [Google Scholar]
- 35. Telljohann SK, Price JH, Dake JA, Durgin J. Access to school health services: differences between full‐time and part‐time school nurses. J Sch Nurs 2004; 3: 176–81. [DOI] [PubMed] [Google Scholar]
- 36. National Audit Office of Finland . Lasten mielenterveysongelmien ehkäisy ja hyvinvoinnin tukeminen kouluerveydenhuollossa (Preventing children's mental health problems and supporting their wellbeing through school health care services.) Valtiontalouden tarkastusviraston selvitykset 3/2017. Koskinen M, Hanhinen S and Suni A. 2017, National Audit Office of Finland, Helsinki, http://urn.fi/urn:isbn:isbn%20978-952-499-384-5 (last accessed 15 December 2017).
- 37. Wiss K, Ståhl T, Saaristo V, Kivimäki H, Frantsi‐Lankia M, Rimpelä A. Terveydenhoitajat, lääkärit, psykologit ja kuraattorit peruskouluissa 2008–2015. (Pupil welfare services in Finnish comprehensive schools in 2008‐2015.) Suomen lääkärilehti (Finnish Medical Journal) 2017, 72: 127–31. [Google Scholar]
- 38. Castaneda A, Larja L, Nieminen T, Jokela S, Suvisaari J, Rask S, Koponen P, Koskinen S. Ulkomaalaistaustaisten psyykkinen hyvinvointi, turvallisuus ja osallisuus. Työpaperi 18/2015. Ulkomaista syntyperää olevien työ ja hyvinvointi –tutkimus 2014 (UTH). (Mental health, safety and social inclusion among people of foreign origin. Working paper 18/2015. The 2014 Survey on work and well‐being among people of foreign origin (UTH)). 2015, National Institute for Health and Welfare, Helsinki, http://urn.fi/URN:ISBN:978-952-302-535-6 (last accessed 15 December 2017).
- 39. Borup I, Holstein BE. Social class variations in schoolchildren's self‐reported outcome of the health dialogue with the school health nurse. Scand J Caring Sci 2004; 18: 343–50. [DOI] [PubMed] [Google Scholar]
- 40. Silliman M. Targeted Funding, Immigrant Background, and Educational Outcomes: Evidence from Helsinki's “Positive Discrimination” Policy. VATT Working Papers 91. 2017, VATT Institute for economic research, Helsinki. https://vatt.fi/documents/2956369/4541479/wp91.pdf/d0921f09-baba-4120-a5cd-dc25243da4b6/wp91.pdf.pdf (last accessed 8 August 2018).


