Abstract
Background
Home care service (HCS) for sick children is a complex healthcare service, which can be organised in various models. Despite the possibility to support family everyday life, the accessibility and utilisation may still be limited. The aim of this study was to (i) determine characteristics in referrals to county‐based HCS, (ii) determine characteristics of referred children and (iii) assess acceptability of parents and children in county‐based HCS.
Methods
Data on characteristics of referrals and referred children were collected from medical records of children 0–17 years of age, referred to eight HCS units during 2015–2018. Data on parental and child overall experience, satisfaction of, safety with, and preference for care, were collected from parents by a questionnaire. Descriptive and comparative statistics were used to analyse the data.
Results
Three hundred and fifty‐five referrals led to one or more periods of HCS for 171 children in various ages with a wide range of illnesses. Children with cancer (30%) composed the largest group and administration of intravenous antibiotics accounted for 56% of the care tasks. Seven per cent of the referrals were to palliative home care. Thirty‐eight referrals of 34 children were refused. There was an uneven distribution of the indication for referral, acceptance rate and diagnoses of children among HCS units. Parents reported their and their child's experience with the HCS visit as highly positive and preferred home care to hospital care in over 96% of the HCS in 212 visits.
Conclusion
County‐based HCS constitutes a supplement to hospital care for sick children with various illnesses through different stages of acute and long‐term illness and at end of life, with high levels of acceptability. Few referrals and variation in referral characteristics and acceptance rate of referrals between HCS units led to unequal and inequitable accessibility and utilisation of HCS.
Keywords: home care service, paediatric, preference for care, referral, satisfaction with care, utilisation
Introduction
Home care service (HCS), as a substitute and supplement for care in hospital, can support family life 1, 2, 3 in the strained period of time that illness in a child may impose 4 and is advocated in international 5, 6 and national policy documents 7, 8. Models of HCS for sick children vary internationally and within countries 9, 10, 11, 12, 13. There are two main models of HCS, one being hospital‐based and the other community‐based service 13, 14. In Sweden, both hospital‐based and community‐based HCS are used, and when based in the community, it can be organised either by the municipality or by the county 7.
Despite the last decades of increased HCS for children with acute or chronic illnesses 11, 15 and for paediatric palliative care (PPC) and end‐of‐life care needs 16, the accessibility 12 and utilisation may still be limited 13, 17, 18. Lack of awareness of HCS or reluctance among physicians to refer from paediatric departments to HCS has been identified as barriers to the use of HCS 9, 13. Studies show how utilisation of HCS is unevenly distributed among children with different diagnoses or conditions, family economy 10, ethnicity and location of home 9.
Home care service may be feasible for sick children in terms of medical safety and family acceptability 14 and families often prefer HCS to care at the hospital during illness 3, 11, 19, 20, 21, 22. However, HCS may also pose challenges for parents such as differing experiences of having responsibility for care tasks 23 and healthcare professionals experience and expertise in paediatric care may have impact on family feelings of safety and satisfaction with care 1, 19, 24, 25. Further, studies have shown that healthcare professionals, who lack experience in paediatric care, may feel uncomfortable with providing care for children in their home 26, 27.
The evidence base is still limited and strengths and challenges in different models of HCS for children with various conditions, diagnoses and ages need to be thoroughly investigated 12, 13. Studies are also required to identify accessibility, utilisation and acceptability 9, 11, 12, 13, 28. In two previous studies, we have described a county‐based HCS for adults and children. Families with ill children experienced the provision of HCS as a possibility to strengthen family life and health 1, and the HCS healthcare professionals experienced it as challenging but rewarding 26 to care for sick children. The aim of this study was (i) to determine characteristics in referrals to county‐based HCS, (ii) to determine characteristics of referred children and (iii) to assess acceptability of parents and children in county‐based HCS.
Methods
Setting
The study was performed in the southern county of Sweden with a population of approximately 1.3 million, of whom 300 000 are children 0–18 years of age29 including a total of 64 paediatric (0–18 years) deaths every year. One university hospital and two local hospitals provide paediatric inpatient care with altogether 13 000 inpatient admissions yearly, supplemented by extensive care at several out‐patient departments. HCS for children was limited until 2013 when the county council decided to include all inhabitants, regardless of age, condition and stage of illness, in the provision of county‐based HCS. Multi‐professional teams with limited training in and experience of paediatric care 26, organised in eight units around the county, provide HCS with a 24‐hour nursing and physician service available for both adults and children. HCS is provided as various specified care tasks (SCT), such as administering intravenous antibiotics or pain medication or as PPC.
Study population
We assessed all children 0–17 years of age, who were referred to HCS during a 3‐year period from April 2015 to March 2018 to determine characteristics of referrals and referred children. We identified 355 referrals of 203 children, of which 304 referrals resulted in the provision of HCS to 171 children.
Parents to the 171 children provided with HCS were eligible to assess acceptability of HCS if they resided in the county and were able to read Swedish. At one of the first home visits, the HSC healthcare professionals asked parents if they wanted information about the study. Parents to 50 children agreed to be contacted and one or two parents to 48 children were given oral and written information by the first author (CC). Seventy parents to 36 children (one parent was a single legal guardian and one parent lived abroad) and one 15‐year‐old child returned written informed consent by mail of which parents to 23 children returned questionnaires (Fig. 1).
Figure 1.
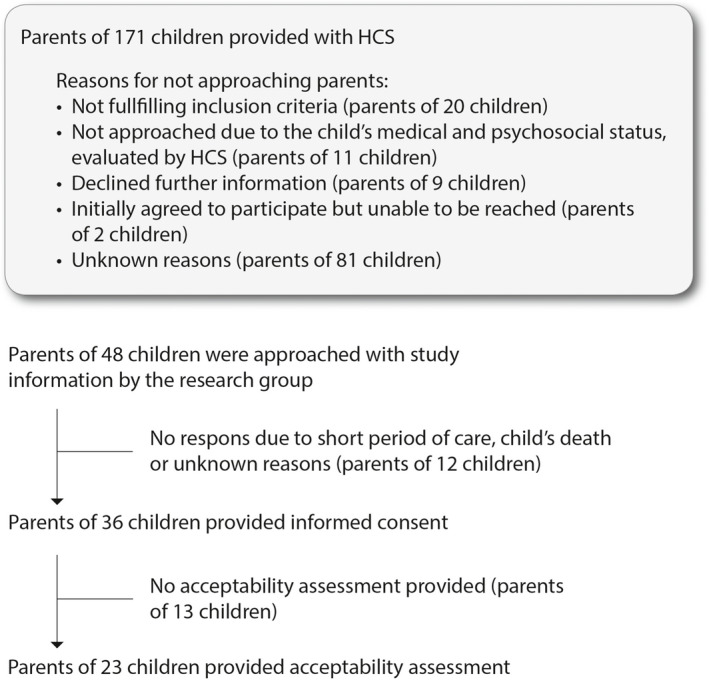
Flow chart of data inclusion for acceptability assessment.
Data collection and outcome measures
Data to determine characteristics of referrals to HCS and referred children were collected from the children's medical records by CC. Data on age, sex, diagnoses, indication for referral, source of referral, distance from the child's home to nearest inpatient paediatric department, child being dead at the time of data collection, time from referral to first day of HCS, reason for denial of referral, reasons for premature discharge from HCS, information on preferred and actual time from referral to first day with HCS, duration of HCS provided (number of days) and number of HCS visits were extracted and transferred to a designated form.
Data to assess parental and child, by proxy, acceptability of HCS, were collected by a questionnaire after each day of HCS visit 28. Parents were instructed to score their overall experience of HCS, how secure they felt, and how satisfied they were with the HCS visit by a five‐point scale ranging from not at all to very much. Parents were also instructed to rate their perception of their child's overall experience, how secure they felt, and how satisfied they were with the HCS visit, and parents finally scored their family's preference for future care as yes or no to HCS. The questionnaire had extra space to write comments in free text. Parents were asked to fulfil one questionnaire per day of HCS visit and return the questionnaires by postal mail. The original questionnaire was tested for face‐validity and cognitive interviews by healthcare professionals and five parents and was deemed simple to understand and complete, in a study of HCS in paediatric oncology patients in Denmark 19. Two of the authors (CC, HH), who are bilingual in Danish and Swedish translated the questionnaire forward and back, emphasising conceptual translation and natural language (30). The Swedish version was tested for face validity in a group of researchers in paediatric nursing. Data were coded with the use of a code key and transformed into SPSS data files.
Analysis
Descriptive statistics were calculated and expressed as frequencies (percentage (%)) for nominal and ordinal data and as median (interquartile range (IQR)) (minimum‐maximum) for quantitative data. Comparative analysis was calculated to explore the differences between units regarding (i) indication of referrals to PPC and the most commonly reported indication for referral, (ii) acceptance rate of referrals and (iii) diagnosis on children who were provided with HCS. Fisher's exact test was used and p < 0.05 was considered as significant. The two lowest ratings in the five‐point questionnaire were merged, as were the two highest. IBM SPSS Statistics 23 Windows (IBM Corporation, Armonk, NY, USA) was used for statistical analyses.
A quantitative content analysis was performed to systematically categorise the free text comments in the questionnaire assessing parents’ and children's acceptability. Each comment was assigned to one or more category according to content. Each category was labelled and the number of times a category was involved in a comment was summarised 31. The analysis was performed by the first author and verified by a second author (KL). Adjustments on single comments were made until full consensus was obtained.
Ethical considerations
The study was approved by the Regional Ethical Review Board (Dnr 2014/818) and the Institutional Review Board at Skane University Hospital (181‐17) and was carried out in accordance with the Helsinki Declaration 32.
Results
Characteristics of referrals
The number of referrals to each of the 203 children varied from 1 to 14. Most referrals n = 333 (93.7%) concerned SCT and the most frequently requested SCT (70%) was intravenous administration of antibiotics, parental nutrition and blood transfusions. A minority n = 22 (6.3%) of referrals concerned PPC. Seventeen children died during the study period and a majority n = 9 (52%) of the referrals concerning these children were not to PPC but various forms of SCT such as blood sample n = 9 (22%) and intravenous antibiotics n = 5 (13%). The major sources of referrals were physicians in somatic paediatric hospital departments (Table 1). Thirty‐eight referrals of children with various illnesses and in various need of HCS were rejected by HCS. The most common reason for HCS to reject a referral was that the care task was defined as a care task not fit for HCS n = 12 (32%) or being too resource intensive n = 10 (26%). Thirteen accepted referrals were cancelled before HCS was provided because of changes in the child's illness leading to either readmission to hospital or because the requested SCT was no longer needed. The number of referrals was lower during the first year of data inclusion than during the next 2 years while the number of children provided with HCS was relatively stable (Fig. 2). The time from referral to first day of HCS was generally short, with a median of less than 24 hours but with outliers of over 100 days (Table 2). When the time from referral to the first day of care was more than 24 hours, it was often reported in the response to referral to be due to difficulties by HCS to decide whether to accept the child for care or not, limited resources at the time of referral, or the need to plan care in advance. Total number of referrals to a HCS unit varied from 5 to 86. There were significant differences between units regarding indication for referral to PPC (p = 0.001) and for the most common SCT, intravenous antibiotics (p < 0.001). There was also a significant difference between the HCS units in acceptance rate (p = 0.001).
Table 1.
Characteristics of referrals to Home care Service, HCS
| Characteristics | Referrals | Referrals leading to HCS | Rejected referrals |
|---|---|---|---|
| Child's age (n; (%)) | n = 355 | n = 304 | n = 38 |
| 0–1 years | 67 (18.9) | 54 (17.7) | 8 (21.0) |
| 2–5 years | 99 (27.9) | 84 (27.6) | 13 (34.2) |
| 6–12 years | 119 (33.5) | 106 (34.9) | 10 (26.3) |
| 13–17 years | 70 (19.7) | 60 (19.8) | 7 (18.4) |
| (Median [IQR] (min‐max)) | 6.0 [2.5–11.0] (0.1–18) | 6.3 [2.5–11.0] (0.1–18) | 5.0 [1.8–11.0] (0.1–18) |
| Sex (n; (%)) | n = 355 | n = 304 | n = 38 |
| Female | 171 (48.2) | 144 (47.4) | 23 (60.5) |
| Diagnosis (n; (%)) | n = 355 | n = 304 | n = 38 |
| Circulatory illness | 11 (3.1) | 8 (2.6) | 2 (5.3) |
| Cystic fibrosis | 32 (9.0) | 32 (10.5) | 0 |
| Digestive illness | 22 (6.2) | 18 (5.9) | 2 (5.3) |
| Hepato‐nephrological | 36 (10.1) | 33 (10.9) | 3 (7.9) |
| Lyme decease | 29 (8.2) | 29 (9.5) | 0 |
| Multiple | 20 (5.6) | 11 (3.6) | 6 (15.8) |
| Neoplasm | 107 (30.1) | 99 (32.6) | 3 (7.9) |
| Neuro‐muscular illness | 52 (14.6) | 38 (12.5) | 12 (31.6) |
| Othera | 46 (13.0) | 36 (11.8) | 10 (26.2) |
| Indication for referral to HCS (n; (%)) | n = 355 | n = 301 | n = 38 |
| Palliative care | 22 (6.3) | 17 (5.6)* | 3 (7.9) |
| Special care task | |||
| Administration of blood transfusion | 6 (1.7) | 4 (1.3) | 1 (2.6) |
| Administration of intravenous antibioticb | 198 (56.7) | 177 (58.6) | 17 (44.7) |
| Blood sample | 21 (6.0) | 19 (6.3) | 2 (5.3) |
| Total parental nutrition | 21 (6.0) | 19 (6.3) | 1 (2.6) |
| Other intra venous medication | 23 (6.5) | 21 (7.0) | 3 (7.9 |
| Other medicationc | 22 (6.2) | 13 (4.3) | 3 (7.9) |
| Other care taskd | 37 (10.6) | 30 (9.9) | 8 (21.1) |
| Source of referral (n; (%)) | n = 353 | n = 304 | n = 38 |
| Local hospital east | 121 (34.3) | 115 (37.8) | 5 (13.2) |
| Local hospital west | 19 (5.4) | 17 (5.6) | 2 (5.3) |
| University hospital | |||
| Paediatric Oncology department | 67 (19.0) | 58 (19.1) | 4 (10.4) |
| Paediatric Neurology department | 18 (5.1) | 12 (3.9) | 5 (13.2) |
| Paediatric Surgery department | 6 (1.7) | 6 (2.0) | 0 |
| Paediatric Cardiology department | 6 (1.7) | 2 (0.7) | 2 (5.3) |
| Other paediatric departments | 99 (28.0) | 78 (25.7) | 17 (44.7) |
| Othere | 17 (4.8) | 16 (5.2) | 3 (7.9) |
Arthritis, haemato‐immunologic, infection, orthopaedic, respiratory and other (0.9–3.2%).
Ten different antibiotics were administered in either peripheral venous catheters or central venous accesses
Other intravenous drugs for example albumin or antiviral treatment, sub cutaneous or nasal infusion.
Supervision and support to parents during education, assessment of a care‐related situation
Psychiatric departments and a rehabilitation centre.
Figure 2.
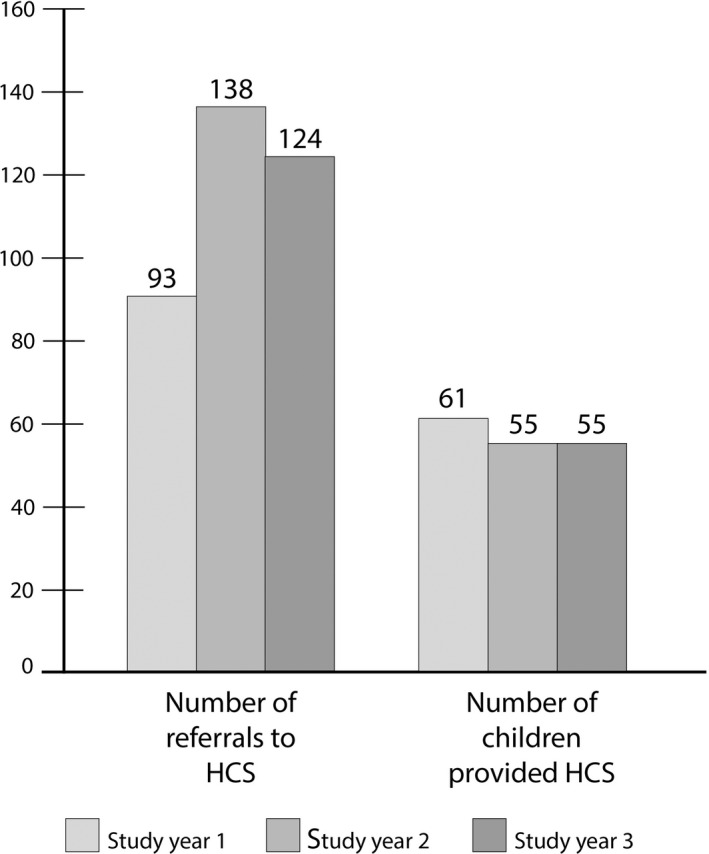
Number of referrals to HCS and of children provided HCS.
Table 2.
Characteristics of children who were, and were not, provided with Home care Service, HCS, children with parents participating in acceptability assessment
| Characteristics | Provided HCS | Rejected HCS | Participants in the acceptability assessment |
|---|---|---|---|
| Child's age at first referral | n = 171 | n = 34 | n = 23 |
| (median, [IQR] (min‐max)) | 5.5 [2.5–9.0] (0.1–18) | 5.0 [1.9–11.3] (0.1–18) | 6.0 [1.5–10.0] (0.5–16) |
| Sex (n (%)) | n = 171 | n = 34 | n = 23 |
| Female | 78 (45.6) | 18 (52.9) | 9 (39.1%) |
| Diagnosis (n (%)) | n = 171 | n = 34 | n = 23 |
| Arthritis | 2 (1.2) | 1 (2.9) | 1 (4.3) |
| Circulatory illness | 8 (4.7) | 2 (5.7) | 2 (8.7) |
| Cystic fibroses | 11 (6.4) | 0 | 0 |
| Digestive illness | 10 (5.8) | 3 (8.8) | 1 (4.3) |
| Haemato‐immunologic illness | 4 (2.3) | 1 (2.9) | 0 |
| Hepato‐nephrological | 12 (7.0) | 3 (8.8) | 3 (13.0) |
| Infection | 9 (5.3) | 3 (8.8) | 1 (4.3) |
| Lyme decease | 29 (17.0) | 0 | 3 (13.0) |
| Multiple illnesses | 7 (4.1) | 4 (11.8) | 0 |
| Neoplasm | 43 (25.1) | 3 (8.8) | 10 (43.5) |
| Neuro‐muscular illness | 22 (12.9) | 10 (29.4) | 1 (4.3) |
| Orthopaedic | 6 (3.5) | 0 | 0 |
| Respiratory illness | 5 (2.9) | 1 (2.9) | 1 (4.3) |
| Other | 3 (1.8) | 3 (8.8) | 0 |
| Duration of ongoing care | n = 162 | n = 21 | |
| Days (median [IQR] (min‐max)) | 7.0 [4.0–10.0] (1–514) | – | 8 [5–19] (1–282) |
| HCS visits nurse | n = 160 | n = 22 | |
| median [IQR] (min‐max)) | 8 [5–14] (1–137) | – | 13 [7–26] (1–123) |
| HCS visits physician | n = 12 | n = 4 | |
| median [IQR] (min‐max)) | 5 [1–9] (1–28) | – | 5[2–22.5] (1–28) |
| Distance from family residence to nearest paediatric inpatient department (km) (n (%)) | n = 166 | n = 33 | n = 23 |
| <20 | 94 (55.0) | 16 (47.1) | 11 (47.8) |
| 20–50 | 58 (33.9) | 11 (32.4) | 10 (43.5) |
| >50 | 14 (8.2) | 6 (17.6) | 2 (8.7) |
| Dead at end of data inclusion (n (%)) | n = 168 | n = 30 | n = 23 |
| Yes | 18 (10.1) | 2 (6.6) | 4 (17.4) |
Characteristics of referred children and the HCS provided for them
There were variations in age, diagnoses, conditions and residence, with a preponderance of younger children, children with cancer or Lyme disease and families living < 50 km from the nearest paediatric department among referred children. The numbers of days HCS was ongoing and the number of visits each child was provided, varied highly (Table 2) between and within diagnoses. Most visits were provided by nurses who were registered for 3337 (95%) of all HCS visits. Other healthcare professionals made occasional home visits alone or together with a nurse, primarily for the children in PPC. The children who were referred to PPC had primarily oncological n = 12 (85%) illness. There was a significant difference (p < 0.001) in distribution of children with Lyme disease among HCS units but not for children with oncological or neuro‐muscular illness.
Parent's and children's acceptability of HCS
Parents to 23 children rated overall experience, satisfaction, feeling of safety and preference for care after 212 HCS visits. Parents from two families contributed with 50% of the questionnaires and each of the other families contributed with 1–14 questionnaires. Parents reported child overall experience, satisfaction and feeling of safety generally as high, although lower than parental rates and more often with missing data (Table 3). In 209 of the 212 questionnaires, parents stated a preference for HCS rather than for hospital care. Comments in free text were made in 124 questionnaires, which constituted seven categories. The number of times a comment was assigned to the category is presented within parentheses. ‘Description of reasons for the HCS‐visit’(97), ‘Description of HCS healthcare professionals’(46), ‘Motivation to the rating of the HCS visit in the questionnaire’(26), ‘Reflections on HCS healthcare professional's personality’(21), ‘Description of the child's condition during the visit’(20), ‘Experience of the HCS visit’(20), ‘Outcome of the HCS visit’(12), and ‘Other’(3). Citations from each category are presented in Table 4.
Table 3.
Parent's and children's acceptability of Home Care Service, HCS visits
| Parents | Children | |
|---|---|---|
| Overall experience with HCS (n (%)) | n = 211 | n = 94 |
| Not good or less good | 2 (0.9) | 3 (1.4) |
| Good | 7 (3.3) | 37 (17.5) |
| Very good or excellent | 202 (95.8) | 154 (72.7) |
| Satisfaction with HCS (n (%)) | n = 212 | n = 94 |
| Very unsatisfied or unsatisfied | 0 (0) | 2 (1.0) |
| Neither satisfied nor unsatisfied | 5 (2.4) | 35 (16.5) |
| Very satisfied or satisfied | 207 (97.6) | 157 (74.1) |
| Feeling of safety during HCS (n (%)) | n = 212 | n = 202 |
| Feeling very unsafe or unsafe | 0 (0) | 2 (1.0) |
| Neither feeling safe nor unsafe | 7 (3.3) | 37 (19.1) |
| Feeling safe or very safe | 205 (96.7) | 163 (79.4) |
n = number of questionnaires providing a response.
Table 4.
Categories with citation
| Categories | Citations |
|---|---|
| Description of reasons for HCS visit | Thursday check‐up |
| Needle placed into porth a’ cath for bloodtransfusion | |
| A catheter was inserted | |
| Description of HCS healthcare professionals | Nurse and physician came |
| Visit from occupational therapist | |
| Motivation to the rating of the visit in the questionnaire | Having a blood sample taken in your finger is never fun but it would not have been better at the hospital |
| Being only three month, he can't have much of an opinion | |
| Absolutely yes/to further HCS/after these days of HCS | |
| Reflections on HCS HP's personality | Staff was fantastic |
| Physician was new and nice | |
| A besserwisser kind | |
| Description of the child's condition during the visit | In deep pain today |
| X is now less aware of what is going on around her | |
| Our child was asleep during the visit | |
| Experience of the HCS visit | Nice and calm visit where we could discuss medication, feelings and so on |
| The idea is good but it is difficult to overview which treatment that is actually given to the child | |
| Outcome of the HCS visit | The time at home is highly valued by everyone |
| The worry we/the parents/had, disappeared | |
| Other comments | Reflections or episodes not related to the HCS visit |
Discussion
This study indicates infrequent and possibly unequal accessibility and utilisation for children of county‐based HCS organised to provide for both adults and children but high levels of acceptability for children in different stages of illness, including end of life. This knowledge is important when implementing a new healthcare service such as county‐based HCS to ensure equality in care for all inhabitants. The findings show that a highly heterogeneous group of children was referred and provided with various care tasks by HCS. The number of children referred to HCS was limited during the study period. When the study opened for inclusion in 2015, most of the HCS units had recently started to provide HCS for children. A small number of referrals and variations in referrals could thus be due to limited knowledge among paediatricians about whom and how to refer, which has previously been acknowledged 9, 13. Although the number of children who were provided HCS during the study period was unchanged, the number of referrals was higher during the two last years. This could indicate that the children who were provided with HCS more often were referred to more than one period of, or more than one indication for, HCS than during year one. Studies, with larger number of referrals and referred children, would be needed to study changes in usage of HCS further. Both the limited number of referrals, and the difference in which children were referred to, and provided with HCS, throughout the county, affects accessibility and is a barrier to equal care based on children's and families’ needs.
Children referred to PPC constituted a small group of patients and almost half of the children who died during the study period were referred to SCT rather than PPC. A reason for this may be perceived barriers for paediatricians 33, 34 and parents 16, 35 to recognise needs of PPC for children. Home care is regarded as part of PPC 6 and children with life‐limiting or life‐threatening illness and with palliative care needs benefit from home care throughout the trajectory of illness 6, 36, 37. However, we found that a relatively high number of children who were rejected had multiple (11.8%) or neuro‐muscular illnesses (20%). This limits utilisation of HCS to a group of children with complex nursing care needs, shown in other studies to consume frequent healthcare 9, 38 and to have well‐known positive psycho‐social effects of HCS 1, 3. These findings may indicate that it might be difficult to identify and describe the special nursing care needs of children with multiple illnesses. Competence in Child Centred Care 39 may thus be important during the referral process to secure both a child perspective, and a child's perspective in the referral and in HCS. One reason to reject a referral might be the fear of lacking knowledge due to limited training and experience in HCS for children which previously has been identified among HCS healthcare professionals not trained in paediatric care 1, 26, 27. Another possible barrier to accessibility and utilisation may be that it was physicians that referred children to HCS and physicians that managed the referrals at the HCS units, although 95% of the care tasks were provided by nurses. Still, limited available resources were one of the most commonly reported reason for rejecting a referral and could explain the difference in acceptance rate of referrals between HCS units that were identified. Regardless of reason, the uneven acceptance rate constitutes yet another barrier for equal accessibility and utilisation of HCS.
Some referrals concerned support to parents with a new care task they were to perform for their children. Such support has been shown to help parents bridge the vulnerable period of time families may face during the transition from the hospital to their home 40, 41, 42, 43. To provide support and assist parents during this transition places great demands on HCS healthcare professionals, who may feel less experienced in these skills and insecure about the task imposed on them 26, 27, 44 and cooperation with paediatric departments gives important support 26, 27. Despite possible insecurity among HCS healthcare professionals about providing care for children 26, 27, 44, the present study showed overall high ratings from parents of acceptability with HCS in accordance with parents to children who was provided HCS care by paediatric oncology nurses 28. This is important knowledge and may be due to the positive effects of strengthened family life and health that HCS may impose 1.
Strengths and limitations
This study includes all referrals to HCS in a paediatric population over a 3‐year period supplemented with the families’ own experiences of HCS. Data on referrals were collected from medical records, and to ensure reliability, data were collected using a designated form by the first author and verified by administrative staff when data were ambiguous or missing. Parents of children with acute short‐term illness and progressing life‐limiting illnesses in different ages and sexes are represented in the acceptability assessment. However, the findings can only be generalised with caution as subgroups are small and as the children might differ in other respects relevant to the acceptability of HCS. For example, the acceptability assessment had participants with other background than Swedish, but non‐Swedish‐speaking inhabitants were excluded even though they constitute an increasing part of the Swedish population. As communication has been found important for families’ experience of satisfaction and trust in HCS 1, further studies including families regardless of language skills should be a prioritised area. The limited number of parents who participated in the acceptability assessment could be due to gatekeeping by HCS healthcare professionals, which has been acknowledged in previous research 45. Short periods of care may be further reasons why families were not being approached with study information and why parents did not consent to participation. To minimise the risk of influence from HCS healthcare professionals on parents’ consent or ratings of visits, all contact took place between CC and the family.
The present study confirms that broad implementation of a new healthcare service such as county‐based HCS may carry challenges in terms of limited usage despite high parental acceptability. A strategy for interventions to support the implementation may increase accessibility and utilisation and equalise differences in provision. We are grateful to the administrative staff at Palliativ vård och ASIH, Region Skåne, for contributing with data collection, Helene Jacobsson for statistical support.
Author contributions
All co‐authors have contributed to the manuscript according to requirement of full authorship. CC, IKH, KL, HH involved in study design, CC with supervision of IKH, KL, HH involved in data collecting, CC, IKH, KL, HH performed the analysis, and CC, IKH, KL, HH involved in report writing.
Ethical approval
Regional Ethical Review Board (Dnr 2014/818) and the Institutional Review Board at Skane University Hospital (181‐17).
Funding
The Swedish Childhood Cancer Foundation, Stockholm, Sweden (2014–0064), the Lions Research Foundation, Skane, Sweden (LU20160423), the Jonas Foundation, Lund, Sweden (F2017/468), Region Skane, Sweden (REGSKANE‐725451), and the Mjölkdroppen Foundation, Helsingborg, Sweden (LU20171219).
Scand J Caring Sci; 2019. Accessibility, utilisation and acceptability of a county‐based home care service for sick children in Sweden
References
- 1. Castor C, Landgren K, Hansson H, Hallstrom IK. A possibility for strengthening family life and health: family members’ lived experience when a sick child receives home care in Sweden. Health Soc Care Community 2018; 26: 224–31. [DOI] [PubMed] [Google Scholar]
- 2. Angelhoff C, Edell‐Gustafsson U, Morelius E. Sleep of parents living with a child receiving hospital‐based home care: a phenomenographical study. Nurs Res 2015; 64: 372–80. [DOI] [PubMed] [Google Scholar]
- 3. Eskola K, Bergstraesser E, Zimmermann K, Cignacco E. Maintaining family life balance while facing a child's imminent death‐A mixed methods study. J Adv Nurs 2017: 1–11. [DOI] [PubMed] [Google Scholar]
- 4. Hallstrom I, Elander G. Families’ needs when a child is long‐term ill: a literature review with reference to nursing research. Int J Nurs Pract 2007; 13: 193–200. [DOI] [PubMed] [Google Scholar]
- 5. European Association for Children in Hospital . European Association for Children in Hospital 2015, https://www.each-for-sick-children.org/ (last accessed 21 February 2019).
- 6. Organization WH . WHO Definition of Palliative Care 1998, http://www.who.int/cancer/palliative/definition/en/ (last accessed 21 February 2019).
- 7. National Board of Health and Welfare . Hemsjukvård i förändring – En kartläggning av hemsjukvården i Sverige. Home healthcare in change – A documentation of home healthcare services in Sweden 2008, http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/8800/2008-126-59_200812659.pdf (last accessed 21 February 2019).
- 8. Great Britain. National Audit Office., Great Britain . Department for Children Schools and Families. Financial management in the Department for Children, Schools and Families: report. 2009, TSO, London, 43 p. [Google Scholar]
- 9. Berry JG, Hall M, Dumas H, Simpser E, Whitford K, Wilson KM, O'Neill M, Mittal V, Agrawal R, Dribbon M, Haines CJ, Traul C, Marks M, O'Brien J. Pediatric hospital discharges to home health and postacute facility care: a national study. JAMA Pediatr 2016; 170: 326–33. [DOI] [PubMed] [Google Scholar]
- 10. Delgado E, Barfield RC, Baker JN, Hinds PS, Yang J, Nambayan A, Quintana Y, Kane JR. Availability of palliative care services for children with cancer in economically diverse regions of the world. Eur J Cancer 2010; 46: 2260–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Parab CS, Cooper C, Woolfenden S, Piper SM. Specialist home‐based nursing services for children with acute and chronic illnesses. Cochrane Database Syst Rev 2013; 6: CD004383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Parker G, Spiers G, Cusworth L, Birks Y, Gridley K, Mukherjee S. Care closer to home for children and young people who are ill: developing and testing a model of service delivery and organization. J Adv Nurs 2012; 68: 2034–46. [DOI] [PubMed] [Google Scholar]
- 13. Spiers G, Gridley K, Cusworth L, Mukherjee S, Parker G, Heaton J, Atkin K, Birks Y, Lowson K, Wright D. Understanding care closer to home for ill children and young people. Nurs Child Young People 2012; 24: 29–34. [DOI] [PubMed] [Google Scholar]
- 14. Parker G, Spiers G, Gridley K, Atkin K, Birks Y, Lowson K, Light K. Systematic review of international evidence on the effectiveness and costs of paediatric home care for children and young people who are ill. Child Care Health Dev 2013; 39: 1–19. [DOI] [PubMed] [Google Scholar]
- 15. While AE, Dyson L. Characteristics of paediatric home care provision: the two dominant models in England. Child Care Hlth Dev 2000; 26: 263–75. [DOI] [PubMed] [Google Scholar]
- 16. Vadeboncoeur CM, Splinter WM, Rattray M, Johnston DL, Coulombe L. A paediatric palliative care programme in development: trends in referral and location of death. Arch Dis Child 2010; 95: 686–9. [DOI] [PubMed] [Google Scholar]
- 17. Herbert A, Bradford N, Donovan L, Pedersen LA, Irving H. Development of a state‐wide pediatric palliative care service in Australia: referral and outcomes over two years. J Palliat Med 2014; 17: 288–95. [DOI] [PubMed] [Google Scholar]
- 18. Wentlandt K, Krzyzanowska MK, Swami N, Rodin G, Le LW, Sung L, Zimmermann C. Referral practices of pediatric oncologists to specialized palliative care. Support Care Cancer 2014; 22: 2315–22. [DOI] [PubMed] [Google Scholar]
- 19. Hansson H, Kjaergaard H, Johansen C, Hallstrom I, Christensen J, Madsen M, Schmiegelow K. Hospital‐based home care for children with cancer: feasibility and psychosocial impact on children and their families. Pediatr Blood Cancer 2013; 60: 865–72. [DOI] [PubMed] [Google Scholar]
- 20. Hansson H, Kjaergaard H, Schmiegelow K, Hallstrom I. Hospital‐based home care for children with cancer: a qualitative exploration of family members’ experiences in Denmark. Eur J Cancer Care (Engl) 2012; 21: 59–66. [DOI] [PubMed] [Google Scholar]
- 21. von Lutzau P, Otto M, Hechler T, Metzing S, Wolfe J, Zernikow B. Children Dying from Cancer: parents’ perspectives on symptoms, quality of life, characteristics of death, and end‐of‐life decisions. J Palliat Care 2012; 28: 274–81. [PubMed] [Google Scholar]
- 22. Kassam A, Skiadaresis J, Alexander S, Wolfe J. Parent and clinician preferences for location of end‐of‐life care: home, hospital or freestanding hospice? Pediatr Blood Cancer 2014; 61: 859–64. [DOI] [PubMed] [Google Scholar]
- 23. Spiers G, Parker G, Gridley K, Atkin K. The psychosocial experience of parents receiving care closer to home for their ill child. Health Soc Care Community 2011; 19: 653–60. [DOI] [PubMed] [Google Scholar]
- 24. Aschenbrenner AP, Winters JM, Belknap RA. Integrative review: parent perspectives on care of their child at the end of life. J Pediatr Nurs 2012; 27: 514–22. [DOI] [PubMed] [Google Scholar]
- 25. Stevens B, McKeever P, Law MP, Booth M, Greenberg M, Daub S, Gafni A, Gammon J, Yamada J, Epstein I. Children receiving chemotherapy at home: perceptions of children and parents. J Pediatr Oncol Nurs 2006; 23: 276–85. [DOI] [PubMed] [Google Scholar]
- 26. Castor C, Hallstrom I, Hansson H, Landgren K. Home care services for sick children: healthcare professionals’ conceptions of challenges and facilitators. J Clin Nurs 2017: 1–10. [DOI] [PubMed] [Google Scholar]
- 27. Samuelson S, Willen C, Bratt EL. New kid on the block? Community nurses’ experiences of caring for sick children at home. J Clin Nurs 2015; 24: 2448–57. [DOI] [PubMed] [Google Scholar]
- 28. Baker JN, Levine DR, Hinds PS, Weaver MS, Cunningham MJ, Johnson L, Anghelescu D, Mandrell B, Gibson DV, Jones B, Wolfe J, Feudtner C, Friebert S, Carter B, Kane JR. Research priorities in pediatric palliative care. J Pediatr 2015; 167(467–70): e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. SCB . Statistics Sweden, http://www.scb.se/be0101-en (last accessed 21 February 2019).
- 30. World Health Organization . 2018, https://www.who.int/substance_abuse/research_tools/translation/en/ (last accessed 21 February 2019).
- 31. Kondracki NL, Wellman NS, Amundson DR. Content analysis: review of methods and their applications in nutrition education. J Nutr Educ Behav 2002; 34: 224–30. [DOI] [PubMed] [Google Scholar]
- 32. World Medical Association . WORLD MEDICAL ASSOCIATION DECLARATION OF HELSINKI. Ethical Principles for Medical Research Involving Human Subjects Helsinki 2013, https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/ (last accessed 21 February 2019). [DOI] [PubMed]
- 33. Twamley K, Craig F, Kelly P, Hollowell DR, Mendoza P, Bluebond‐Langner M. Underlying barriers to referral to paediatric palliative care services: knowledge and attitudes of health care professionals in a paediatric tertiary care centre in the United Kingdom. J Child Health Care 2014; 18: 19–30. [DOI] [PubMed] [Google Scholar]
- 34. Knapp C, Thompson L. Factors associated with perceived barriers to pediatric palliative care: a survey of pediatricians in Florida and California. Palliat Med 2012; 26: 268–74. [DOI] [PubMed] [Google Scholar]
- 35. Kars MC, Grypdonck MH, de Korte‐Verhoef MC, Kamps WA, Meijer‐van den Bergh EM, Verkerk MA, van Delden JJM. Parental experience at the end‐of‐life in children with cancer: ‘preservation’ and ‘letting go’ in relation to loss. Support Care Cancer 2011; 19: 27–35. [DOI] [PubMed] [Google Scholar]
- 36. Levine DR, Johnson LM, Snyder A, Wiser RK, Gibson D, Kane JR, Baker JN. Integrating palliative care in pediatric oncology: evidence for an evolving paradigm for comprehensive cancer care. J Natl Compr Canc Netw 2016; 14: 741–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Weaver MS, Heinze KE, Kelly KP, Wiener L, Casey RL, Bell CJ, Wolfe J, Garee AM, Watson A, Hinds PS. Palliative care as a standard of care in pediatric oncology. Pediatr Blood Cancer 2015; 62(Suppl 5): S829–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ananth P, Melvin P, Feudtner C, Wolfe J, Berry JG. Hospital use in the last year of life for children with life‐threatening complex chronic conditions. Pediatrics 2015; 136: 938–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Coyne I, Hallstrom I, Soderback M. Reframing the focus from a family‐centred to a child‐centred care approach for children's healthcare. J Child Health Care 2016: 1–9. [DOI] [PubMed] [Google Scholar]
- 40. Mizrak B, Deniz AO, Acikgoz A. Anxiety levels of mothers with newborns in a Neonatal Intensive Care Unit in Turkey. Pak J Med Sci 2015; 31: 1176–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Barnard JG, Albright K, Morrato EH, Nowels CT, Benefield EM, Hadley‐Miller NA, Kempe A, Erickson MA. Paediatric spinal fusion surgery and the transition to home‐based care: provider expectations and carer experiences. Health Soc Care Community 2013; 21: 634–43. [DOI] [PubMed] [Google Scholar]
- 42. Manhas KP, Mitchell I. Extremes, uncertainty, and responsibility across boundaries: facets and challenges of the experience of transition to complex, pediatric home care. J Child Health Care 2012; 16: 224–36. [DOI] [PubMed] [Google Scholar]
- 43. Sparud‐Lundin C, Hallstrom I. Parents’ experiences of two different approaches to diabetes care in children newly diagnosed with type 1 diabetes. Qual Health Res 2016; 26: 1331–40. [DOI] [PubMed] [Google Scholar]
- 44. Chong L, Abdullah A. Community palliative care nurses’ challenges and coping strategies on delivering home‐based pediatric palliative care. Am J Hosp Palliat Care 2017; 34: 125–31. [DOI] [PubMed] [Google Scholar]
- 45. Kars MC, van Thiel GJ, van der Graaf R, Moors M, de Graeff A, van Delden JJ. A systematic review of reasons for gatekeeping in palliative care research. Palliat Med 2016; 30: 533–48. [DOI] [PubMed] [Google Scholar]


