Abstract
This article highlights major findings from the 2019 Emergency/Trauma/Transport Nursing Workforce Survey, which was developed to profile today's emergency nurses and help identify specific resources necessary to ensure a sufficient, well-prepared, and well-supported future workforce.
Figure.

No caption available.
Nurses working across the emergency spectrum—in adult, mixed, and pediatric EDs, in trauma centers, on scene, and during transport—deliver critical care in dynamic, high-stakes, and high-stress environments. Because emergency/trauma/transport nurses serve on the frontline of healthcare, they must respond expertly and confidently with no room for error, often when seconds count and detecting subtle signs or changes can have major implications. Ensuring that these nurses possess the highest levels of clinical knowledge and expertise and supporting their continued competence, preparedness, well-being, and ability to be compassionate as they respond to the unique needs of every emergent patient and situation are vital concerns of the healthcare community and consumers.
Previous studies have described the characteristics of the entire US nursing workforce, and researchers and professional nursing organizations have examined specific emergency nursing issues and trends.1-3 However, to our knowledge, no research had been conducted to describe the characteristics of the emergency nursing workforce across the spectrum of emergency care. In 2018, the Board of Certification for Emergency Nursing (BCEN) formed a research partnership with the MedEvac Foundation International, Emergency Nurses Association (ENA), Society of Trauma Nurses (STN), and Air & Surface Transport Nurses Association (ASTNA). The partnership commissioned the Human Resources Research Organization (HumRRO) to conduct a comprehensive study of the emergency nursing workforce, including an in-depth look at the emergency, trauma, and transport specialties.
In this article, we highlight major findings from the 2019 Emergency/Trauma/Transport Nursing Workforce Survey (ETTS), which was developed to profile today's emergency nursing workforce and help identify specific resources necessary to ensure a sufficient, well-prepared, and well-supported future workforce.
Methods
We conducted a descriptive study of the emergency/trauma/transport nursing workforce using two data sources: an extract of data for emergency/trauma nurses from the 2017 National Nursing Workforce Survey (NNWS)4 provided by the National Council of State Boards of Nursing and the custom-designed ETTS, which included items developed specifically for this study and items from the NNWS. (View the survey instrument and other bonus content by visiting www.nursingmanagement.com and clicking on the Online Exclusives tab.) The inclusion of NNWS items in the ETTS allowed us to evaluate the representativeness of our sample of respondents and directly compare ETTS results with those for the entire nursing workforce. NNWS data provide population-level estimates.
The ETTS included 60 questions that had either been previously developed or were developed to address the research questions.1,5 The study was reviewed and approved by the Institutional Review Board at HumRRO. Following publicity about the survey by the research sponsors, HumRRO emailed the custom survey to 157,608 individuals identified in the BCEN, ENA, STN, and ASTNA databases. Because some of the organizational databases didn't include RN status for every individual, selection for RN status occurred via the survey instrument. Participants took the survey between January 25 and February 18, 2019, and completed a consent statement before taking the survey. Responses were stored on a secure server. A total of 7,089 individuals began the survey. Before calculating descriptive statistics and correlations, we cleaned the data to include only responses from actively employed RNs working in emergency, trauma, or transport nursing settings. In total, 4,702 individuals met the inclusion criteria. Where NNWS and ETTS shared common questions, we compared the results across surveys.
Results
Workforce profile
Based on self-reported specialty and work setting, 73.8% of ETTS respondents identify as emergency nurses, 11.5% as trauma nurses, and 14.7% as transport nurses. Overall, workforce profile demographics are similar across the three specialties. Based on survey responses for those answering the demographics questions, the largest proportions of the emergency/trauma/transport nursing workforce are 30 to 39 years old (33.5%), female (78.8%), and White (87.4%). Survey results suggest that emergency/trauma/transport nurses are younger than the general nursing population. Specifically, ETTS data indicate that the average age is 43.6, the median age is 42, and 31.7% of emergency/trauma/transport nurses are 50+ years old. Similarly, the NNWS data for emergency/trauma nurses suggest that the mean age is 41.6, the median age is 40, and 37.9% of emergency/trauma nurses are 50+ years old. However, the NNWS data for the general nursing population suggest that the average age is 50, the median age is 53, and 50.9% of nurses are 50+ years old. (See online bonus content.)
The gender of ETTS respondents is 78.8% female and 21.1% male compared with 90.9% female and 9.1% male in the overall NNWS data. Notably, ETTS data indicate that the female-to-male ratio for transport nurses is approximately 3:2 versus 4:1 for trauma nurses and nearly 5:1 for emergency nurses. The racial and ethnic diversity of ETTS respondents generally mirrors the NNWS data. Nurses responding to the ETTS represent all 50 states, as well as Washington, D.C., American Samoa, Puerto Rico, and the US Virgin Islands, with 42.6% reporting their main work setting as urban, 31.7% suburban, and 22.8% rural. The geographic distribution of ETTS respondents is generally representative of the NNWS data for emergency/trauma nurses.
Workforce qualifications
Licensure, education, tenure, and professional credentials. Of the ETTS respondents, 6.4% indicate that they're advanced practice registered nurses (APRNs). Similarly, 5.9% of respondents from the NNWS emergency/trauma nurse data are APRNs, whereas 9.9% of nurses in the full NNWS data set are APRNs. Among emergency/trauma/transport nurses, 60.4% report having a bachelor's degree as their highest level of nursing education versus 51.0% for NNWS emergency/trauma nurses and 45.2% for all nurses. (See Figure 1.) For 16.3% of emergency/trauma/transport nurses, a master's degree is the highest level of nursing education as compared with 12.9% for NNWS emergency/trauma nurses and 17.1% for all nurses. Considering emergency/trauma/transport nursing tenure by specialty, emergency nurses obtained their RN more recently (14.7 years) on average than trauma nurses (17.0 years) or transport nurses (17.2 years) but also report the longest tenure within their specialty (11.6 years) as compared with trauma nurses (10.6 years) and transport nurses (9.9 years).
Figure 1:
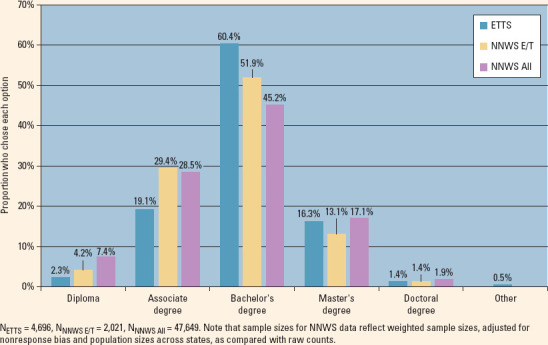
Highest nursing education degree held by ETTS RNs vs. NNWS RNs
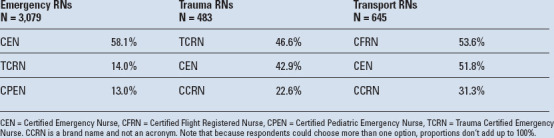
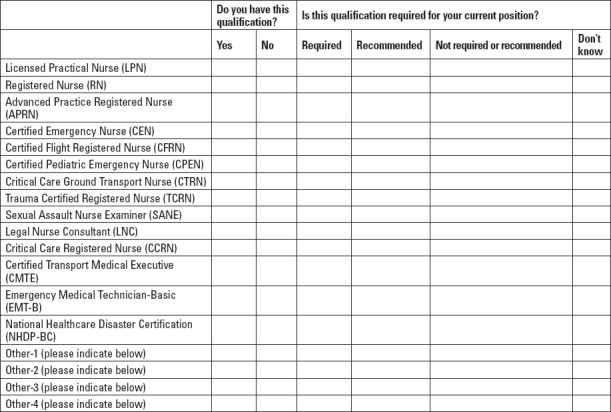
National board certification validates specialty knowledge, clinical judgment, and expertise, and is the highest professional credential a nurse can hold. Over three-quarters of ETTS respondents (77.0%) indicate that they hold one or more board certifications, 28.5% hold two or more, and 8.0% hold three or more, with the Certified Emergency Nurse being the most commonly held certification (55.4%). The most-held emergency nursing board credentials by specialty are shown in Table 1.
Table 1:
Most commonly held board certifications for emergency/trauma/transport nurses by specialty
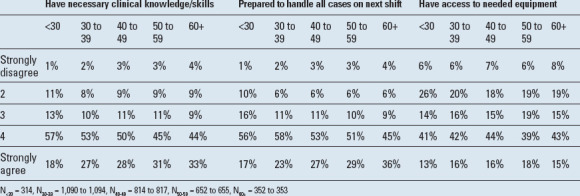
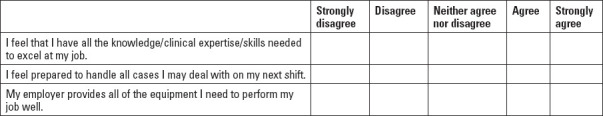
Self-reported preparedness/competency. ETTS respondents rated the extent to which they agree that they have the knowledge/clinical expertise/skills needed to excel at their job, feel prepared to handle all cases they may deal with on their next shift, and have access to all the equipment they need to perform their job well. We averaged responses to these questions to create an overall preparedness/competency score. Most respondents (69%) report feeling prepared/competent overall, although nearly 10% don't. Looking at the individual components of preparedness/competency, most in each age cohort agree or strongly agree that they have the knowledge/clinical expertise/skills to excel and are prepared to handle all cases on their next shift. However, one-third (32%) of the age 29 and younger group and at least one-quarter (25% to 27%) of all other ages report that they don't have access to all the equipment they need to perform their job well. (See Table 2.)
Table 2:
Preparedness/competency ratings for all emergency/trauma/transport nurses by age
Perceived skill/ability shortages and need for training. ETTS respondents were asked which skill/ability shortages and training needs exist among nurses in their respective specialties. The overall magnitude of the perceived shortages is generally similar across the three specialties, with fewer skill/ability gaps indicated by transport nurses. The skill/ability shortages that the highest proportion of emergency/trauma/transport nurses indicate as existing among their peers are stress management (63.7%), critical-thinking skills (52.1%), clinical knowledge and skills (43.7%), decision-making under pressure (43.0%), time management (40.5%), leadership (39.8%), and mentorship (39.5%). Training on specific equipment (39.2%), leadership/management training (38.5%), crisis management training (33.1%), stress management (32.3%), and workplace violence/incivility/bullying education (30.1%) are the types of training most needed.
The skill/ability gaps most perceived in new nurses include critical-thinking skills (75.2%), decision-making under pressure (71.7%), time management (65.1%), unrealistic job expectations (64.1%), and clinical knowledge/skills (61.5%). Respondents' top recommended changes to new nurse training include more hands-on training (87.1%), better simulations (61.1%), pharmacologic training (40.1%), and training on interpersonal skills (38.1%). (See online bonus content.)
Occupational profile
In the ETTS, the top three work settings overall are ED (59.2%), trauma center (15.5%), and air (rotor wing) transport (6%). Whereas 65.3% of all nurses work full time according to NNWS data, 85.4% of emergency/trauma/transport nurses work full time, with 13.7% working per diem and 11.5% working part time, according to ETTS data. Most emergency/trauma/transport nurses work 12-hour shifts (65.1%), whereas 15.2% work 8-hour shifts and 7.2% work 24-hour shifts.
Approximately two-thirds (69.3%) of emergency/trauma/transport nurses hold one nursing job, 24.1% hold two, and 6.5% hold three or more. By comparison, 83.3% of all NNWS respondents hold one position, 13.9% have two, and 2.8% have three or more. Just under half of ETTS respondents (49.4%) report working about the same number of hours as they were hired to work, whereas 39.4% report working more hours than they were hired to work and 8.3% report working far more hours. However, when asked how often mandatory overtime is assigned, 82.3% indicate that they're never or almost never assigned mandatory overtime.
When asked to evaluate their workload, 5.5% of all ETTS respondents report their workload is overwhelming, 33.0% say it's too heavy, and 57.4% indicate that it's about right. (See Figure 2.) By specialty, 42.9% of emergency nurses and 41.6% of trauma nurses report that their workload is overwhelming or too heavy versus 15.3% of transport nurses. Regarding staffing levels, few participants (1.8%) overall describe their organization as overstaffed, 42.6% describe staffing levels as about right, and over half (55.6%) indicate that their organization is understaffed.
Figure 2:
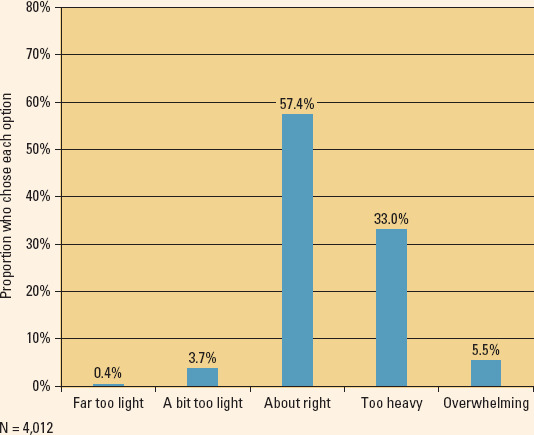
Perceptions of workload across all emergency/trauma/transport nurses
Most ETTS respondents (97%) report that their role involves direct patient care. Across emergency/trauma/transport nurses serving in a role focused primarily on direct patient care (as indicated by their job title), direct patient care accounts for 59.4% of their time, with 27.7% spent on documentation and 9.1% on administrative responsibilities. Across all nurses working directly with patients, of the time spent on direct patient care, 50.8% is medical; 27.3%, injury-related; and 14.6%, behavioral. Also, of that time, 40.3% of participants' time is spent on treating adults, 32.1% on older adults, 14.7% on infants and children, and 12.9% on adolescents.
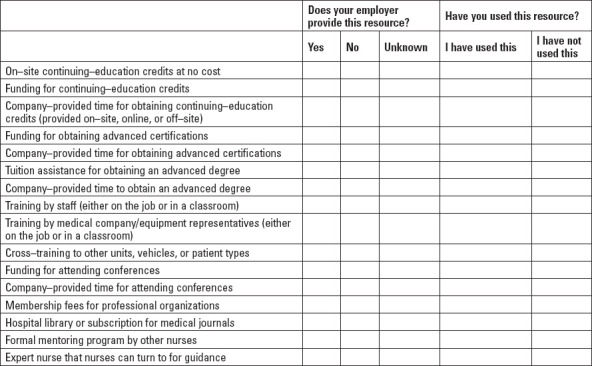
ETTS respondents indicate high degrees of professional development offerings at their organizations, including training by staff, onsite continuing education, tuition assistance for advanced degrees, funding for advanced certifications and continuing education, and company-provided time for continuing education. The three most desired types of professional development resources are funding for professional organization membership fees (41%), funding for conferences (31.6%), and funding for advanced certification (24.1%.). Utilization rates for many of the resources offered by organizations tend to increase with age. For example, among the age 29 and younger group, 45.9% say they take advantage of funding for advanced certification and 33.3% take advantage of the membership fees for professional organizations, whereas 60% and 58.5% of the age 30 and older group, respectively, take advantage of those opportunities.
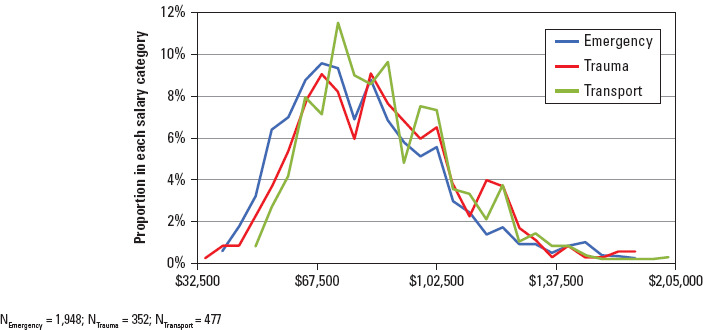
According to ETTS data, the median annual salary for emergency/trauma/transport nurses is $77,500, whereas the median annual salary is $68,000 for emergency/trauma nurses and $63,000 for all nurses, according to NNWS data. When only considering nurses working full time in the ETTS data, the median salary is $77,500 (with the 25th and 75th percentiles being $67,500 and $97,500) versus $69,000 in the NNWS emergency/trauma data. (See Figure 3.) Based on ETTS data by specialty for nurses working full time, the median annual salary is $77,500 for emergency nurses and $82,500 for both trauma and transport nurses. (See online bonus content.)
Figure 3:
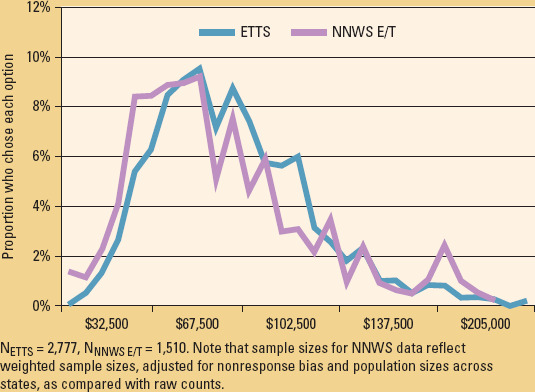
Salary distribution across emergency/trauma/transport nurses working full time vs. NNWS emergency/trauma nurses working full time
Well-being profile
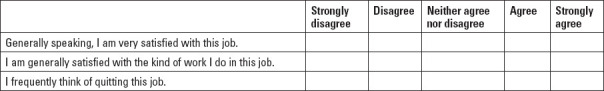
ETTS respondents indicated their job satisfaction by rating the extent to which they're satisfied with their job and the kind of work they do, and the extent to which they think about quitting. The majority of emergency/trauma/transport nurses are satisfied with their job (67.0% agree or strongly agree) and with the work they do (86.7% agree or strongly agree). Nearly one-quarter (24.4%) say they frequently think about quitting, whereas over half (54.5%) report they don't. (See Figure 4.) Satisfaction scores are somewhat higher for transport nurses than for emergency and trauma nurses.
Figure 4:
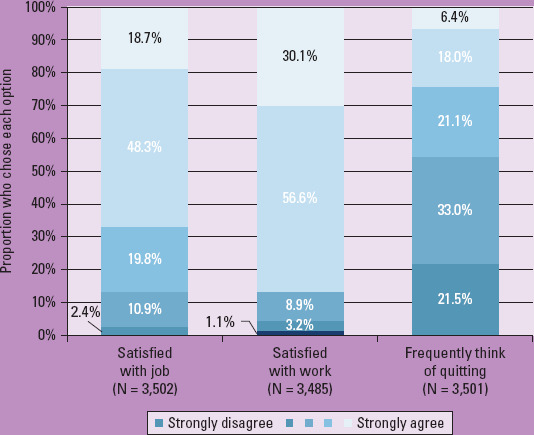
Job satisfaction components across all emergency/trauma/transport nurses
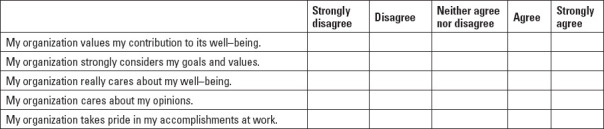
Perceived organizational support is measured by employees' belief that their employer values their contribution and cares about their well-being.6 High levels of perceived organizational support lead to increased job satisfaction, commitment, and employee performance.7 ETTS respondents rated the extent to which their employer values their contributions, considers their goals and values, cares about their well-being, cares about their opinions, and takes pride in their accomplishments at work. Responses were averaged to create an overall perceived organizational support score. Across all emergency/trauma/transport nurses, 41.9% have high or very high perceived organizational support scores and 25.7% have low or very low perceived organizational support scores. (See Figure 5.)
Figure 5:
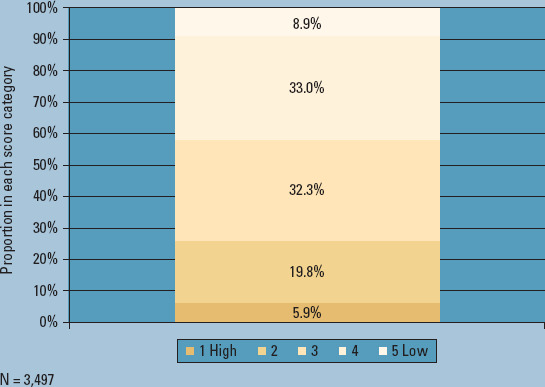
Overall perceived organizational support score across all emergency/trauma/transport nurses
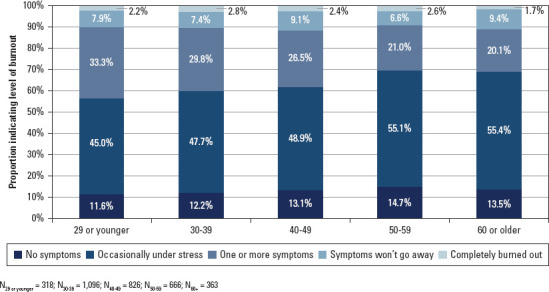
ETTS respondents rated their level of burnout, such as feeling work-related stress, reduced motivation, fatigue, and exhaustion. Whereas 12.9% report no burnout symptoms, 50% report occasional stress, 26.7% indicate that they're definitely burning out, 8% report persistent symptoms, and 2.5% feel completely burned out. Burnout symptoms decrease slightly by age, and transport nurses report the lowest levels of burnout. When asked what resources are most commonly provided by employers to address burnout, the most frequent response is access to counselors (50%). Notably, the second most common response is that their employer provides no resources (35.7%). (See Figure 6.)
Figure 6:
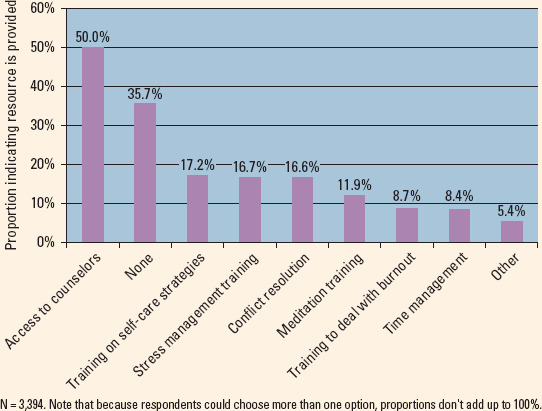
Burnout resources offered to emergency/trauma/transport nurses by their employers, as reported by respondents
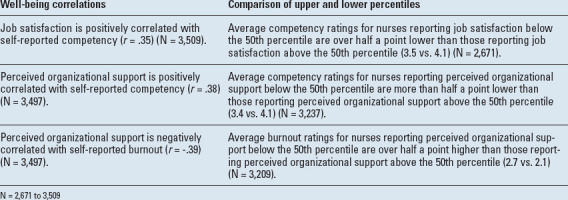
We also examined the relationships between certain nurse well-being variables, and our findings support the importance of nurse well-being to nursing outcomes. Specifically, our analyses show that perceived organizational support and job satisfaction are related to feelings of preparedness/competency and burnout. (See Table 3.) We compared perceived organizational support with the likelihood of quitting. Of ETTS respondents who report high levels of organizational support, 76.1% are unlikely to quit, whereas 52.7% of emergency/trauma/transport nurses reporting low perceived organizational support indicate being likely to quit.
Table 3:
Relationships between well-being variables for all emergency/trauma/transport nurses
Workforce pipeline
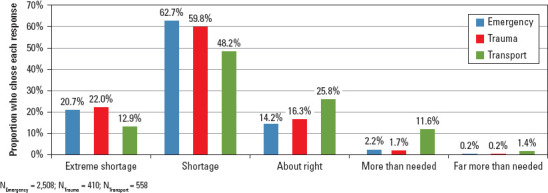
ETTS respondents were asked to comment on the future of the emergency/trauma/transport nursing workforce, including their own career plans. Most (79.6%) expect a shortage or extreme shortage of nurses across the emergency spectrum in the next 5 to 10 years, with transport nurses predicting a less pronounced trend for their specialty.
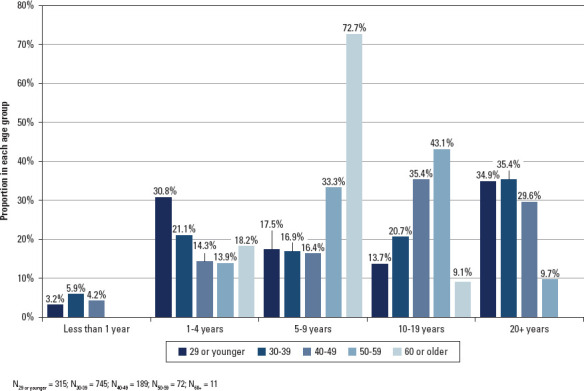
Across all ETTS respondents, 34.1% of nurses age 29 and younger and 25.8% of nurses ages 30 to 39 expect to leave the field of emergency nursing within the next 4 years, which may erode the pipeline of experienced nurses. (See Figure 7.) This pattern of planned exodus by early-career nurses holds when considering the recency of receiving an RN license, indicating that age, not tenure, is related to plans to leave the field. (See online bonus content.) Similarly, 64% of emergency/trauma/transport nurses age 29 and younger and 46.7% of those ages 30 to 39 plan to stay with their current employer for 4 years or less. Likewise, 69.3% of emergency/trauma/transport nurses age 29 and younger and 55.4% of those ages 30 to 39 plan to leave their current primary nursing position within the next 4 years.
Figure 7:
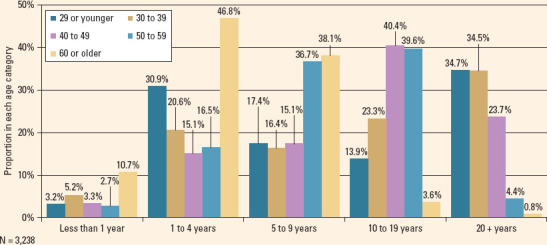
Anticipated number of years emergency/trauma/transport nurses indicate they're planning to remain in their specialty by age group
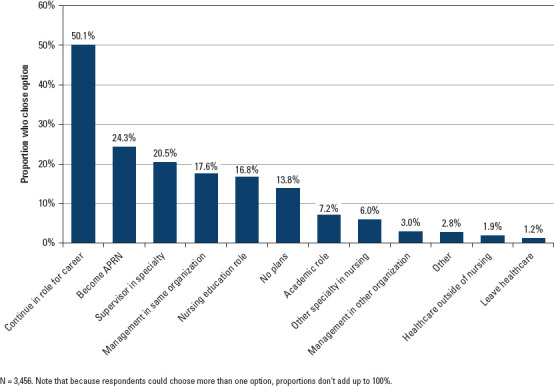
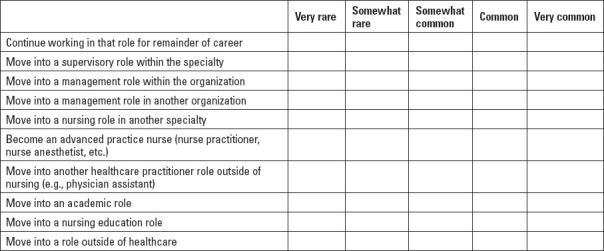
Most ETTS respondents indicate that when they entered the field of emergency nursing, they planned to continue in their specialty, either in their current role (50.1%) or by advancing into a supervisory position (20.5%), whereas 24.3% planned to become an APRN. Regarding their current career plans, 46.6% expect to continue in their current role, 35.1% plan to earn a specialty certification, 21.2% plan to become an APRN, 18.1% plan to take on a nursing education role, and 14.5% aspire to a supervisory role in their specialty. (See Figure 8.) Among respondents under age 40 who intend to leave the field in the next 5 to 10 years, their career plans include becoming an APRN (42.8%), earning a specialty certification (35.7%), continuing in their current role (28.8%), becoming a nurse in another specialty (23.8%), and taking on a nursing education role (22.4%). (See Figure 9.)
Figure 8:
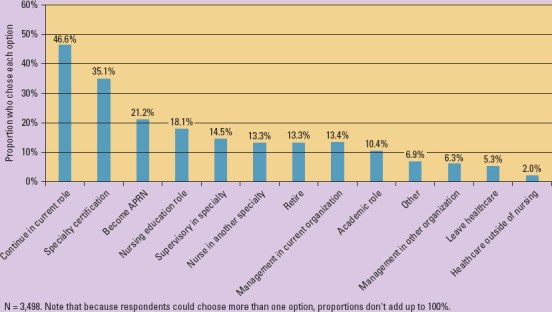
Current career plans for the next 5 to 10 years for all emergency/trauma/transport nurses
Figure 9:
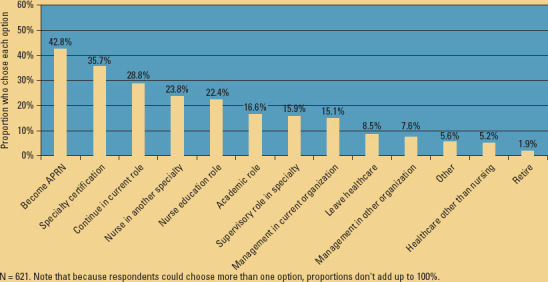
Career paths for emergency/trauma/transport nurses younger than age 40 planning to leave their specialty in the next 5 to 10 years
When asked which approaches to maintaining and building the pipeline of nurses would be most helpful, respondents overall indicate better pay (75.9%), better nurse-patient ratios (57.2%), and employer support (53.2%).
Nursing challenges and impact
The ETTS included two open-ended questions. When asked to indicate the biggest challenges emergency/trauma/transport nurses face, responses from 2,777 participants frequently cite burnout, ineffective leadership, insufficient staffing, lack of support and appreciation, underprepared new recruits, inadequate nurse-patient ratios, and workplace incivility/violence.
Respondents were also asked to describe a critical incident(n = 1,984) where they or a nursing colleague had an impact on clinical or operational outcomes. Emergency/trauma/transport nurses positively impact outcomes as they assess, intervene, evaluate, and communicate regarding patients' clinical conditions; increase patient safety or prevent errors; advocate for patients with physicians and management; provide counsel and support to patients and their families; and increase the quality, speed, and effectiveness of operations.
Key observations
The 2019 ETTS provides the first comprehensive and detailed description of the emergency nursing workforce, including core demographics (age, gender, diversity, education, and professional credentials), occupational profile (work setting, workload, time spent across duties, professional development, and salary), nurse well-being (job satisfaction, perceived organizational support, and burnout), pipeline prospects (nursing shortage and career plans), top challenges, and impact on outcomes. One limitation of our study was its sampling strategy, which was limited to the membership databases of relevant professional organizations that include board-certified nurses, certification candidates, and other stakeholders. Our sample may be more professionally involved than emergency/trauma/transport nurses as a whole, which may, in turn, affect at least some of our findings (such as board certification rate).
However, findings from ETTS and NNWS data on identical questions are similar, suggesting that the ETTS sample is likely representative of the emergency/trauma/transport nursing workforce overall. As such, this research offers important information and insights for nurse leaders, healthcare administrators, and other stakeholders to consider as they work collaboratively and organizationally to solve the challenges that are unique to emergency/trauma/transport nursing. This survey may also serve as a benchmark for future research.
As the findings from this expansive study continue to be unpacked and analyzed, we offer the following high-level observations. First, emergency/trauma/transport nurses need more support in the form of critical resources, including staffing, equipment, and professional development, to meet the demands for their services. These demands include staying current and competent on a wide, ever-changing range of clinical knowledge, procedures, protocols, best practices, technology, and equipment so they're prepared to respond to every patient and scenario, from the more commonplace, low-risk cases to the low-volume, high-risk ones. Emergency/trauma/transport nurses demonstrate a high level of commitment to education and want comprehensive, continuous professional development to attain and maintain the mastery that emergent care warrants. Yet our findings suggest more can be done to ensure that all emergency/trauma/transport nurses, particularly younger nurses, leverage the training and developmental resources their organizations offer.
Second, our research indicates that emergency/trauma/transport nurses demonstrate an exceptional level of dedication to their jobs. Over 85% work full time (versus 65% of all NNWS nurses), nearly one-third hold more than one position (versus 17% of all NNWS nurses), many work 12-hour or longer shifts, and nearly half (47%) work more hours than they were hired to despite mandatory overtime rarely being assigned. Although emergency/trauma/transport nurses report facing formidable on-the-job challenges, their impact on clinical, human, and operational outcomes is significant. Emergency/trauma/transport nurses are explicitly asking for effective, competent leaders who'll work to ensure that their dedication is matched with reasonable workloads, a supportive and safe work environment, and meaningful concern for their well-being, including knowing they're genuinely valued team members.
Third, our research indicates that substantial proportions of early-career nurses intend to leave the emergency/trauma/transport specialty in less than 5 years. Given that 45% of emergency nurses are younger than age 40 and nearly 70% are younger than age 50, and with more than half of trauma nurses (55%) and over two-thirds (67%) of transport nurses in the ages 30 to 49 group, the emergency/trauma/transport nursing profession must be attractive to new recruits and remain so for all ages. Once new recruits are hired, our findings point to onboarding considerations, such as more hands-on training and better simulations, along with the development of critical-thinking and decision-making skills so novices may move up the clinical and professional learning curves thoughtfully, completely, and expeditiously. Our findings also suggest that the confidence, competence, and knowledge transfer that come with experienced nurses are hard to replace.
Finally, our findings suggest that increased organizational support across all age groups may increase preparedness/ competency measures and overall job satisfaction, reduce burnout, and limit attrition, which may help sustain and hopefully expand an engaged, high-performing workforce eager to deliver expert and compassionate care when patients need it the most.
Our nurses have spoken
The ETTS offers rich data for emergency/trauma/transport nurse leaders and the C-suite to assess, address, and improve a wide range of emergency nursing workforce measures and issues, including important specialty-specific benchmarks. The study also underscores the need for and urgency of addressing systemic organizational issues impacting nursing and patient care across the emergency spectrum, such as patient boarding in the ED. Perhaps most significantly, the findings make a powerful case for nurse leaders to prioritize regular one-on-one communication with each of their team members.
Emergency/trauma/transport nurses have spoken. They're dedicated professionals who want to be heard, want to be part of the decision-making process and help problem solve, want to grow and develop, and want to be recognized. No matter their age or tenure, they're looking for effective leadership and support. Their stated career plans mandate making nursing across the emergency spectrum attractive, particularly for newer and younger nurses. Leaders who prioritize connection and engagement on each of these fronts will find that their investment pays dividends for nurses and patients alike.
Bonus content
Head to www.nursingmanagement.com and click on “Results from the 2019 Emergency/Trauma/Transport Nursing Workforce Survey” in the Online Exclusives tab for more ETTS results and the survey instrument.
INSTRUCTIONS The emergency, trauma, and transport nursing workforce: Highlights of a benchmark 2019 survey
TEST INSTRUCTIONS
Read the article. The test for this CE activity is to be taken online at http://nursing.ceconnection.com.
You'll need to create (it's free!) and login to your personal CE Planner account before taking online tests. Your planner will keep track of all your Lippincott Professional Development online CE activities for you.
There's only one correct answer for each question. A passing score for this test is 13 correct answers. If you pass, you can print your certificate of earned contact hours and access the answer key. If you fail, you have the option of taking the test again at no additional cost.
For questions, contact Lippincott Professional Development: 1-800-787-8985.
Registration deadline is December 3, 2021.
PROVIDER ACCREDITATION
Lippincott Professional Development will award 1.0 contact hour for this continuing nursing education activity.
Lippincott Professional Development is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation.
This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 1.0 contact hour, and the District of Columbia, Georgia, and Florida CE Broker #50-1223.
Payment: The registration fee for this test is $12.95.
REFERENCES
- 1.Smiley RA, Lauer P, Bienemy C, et al. The 2017 national nursing workforce survey. J Nurs Reg. 2018;9(3):S1–S88. [Google Scholar]
- 2.US Department of Health and Human Services, Health Resources and Services Administration. The Registered Nurse Population: Findings from the 2008 National Sample Survey of Registered Nurses. Washington, DC: US Department of Health and Human Services; 2010. [Google Scholar]
- 3.Robinson KS, Jagim MM, Ray CE. Nursing workforce issues and trends affecting emergency departments. Nurs Manage. 2005;36(9):46–53. [DOI] [PubMed] [Google Scholar]
- 4.National Council of State Boards of Nursing. 2017 National Nursing Workforce Survey: Emergency/Trauma RN Extract. Chicago, IL: National Council of State Boards of Nursing; 2019. [Google Scholar]
- 5.Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eisenberger R, Huntington R, Hutchison S, Sowa D. Perceived organizational support. J Appl Psychol. 1986;71(3):500–507. [Google Scholar]
- 7.Rhoades L, Eisenberger R. Perceived organizational support: a review of the literature. J Appl Psychol. 2002;87(4):698–714. [DOI] [PubMed] [Google Scholar]
Results from the 2019 Emergency/Trauma/Transport Nursing Workforce Survey
Figure.

Bonus figure 1: Age distribution of ETTS and NNWS RNs
Figure.
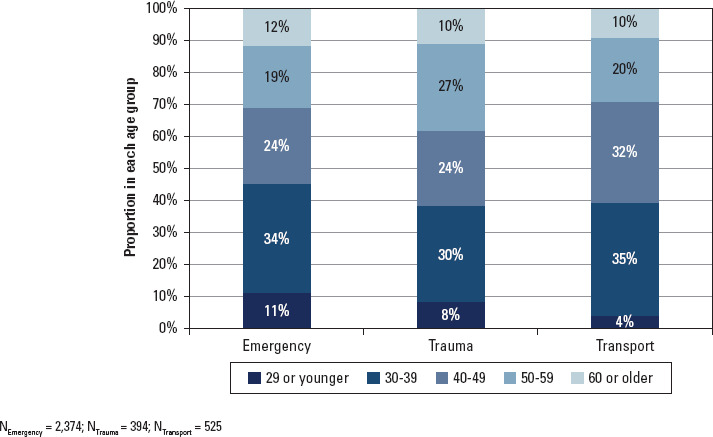
Bonus figure 2: Emergency/trauma/transport nurse age by specialty
Figure.
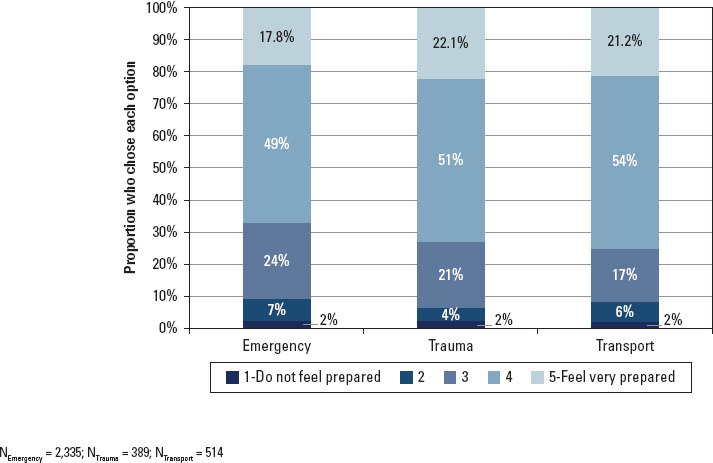
Bonus figure 3: Average preparedness/competency ratings by specialty for emergency/trauma/transport nurses
Figure.
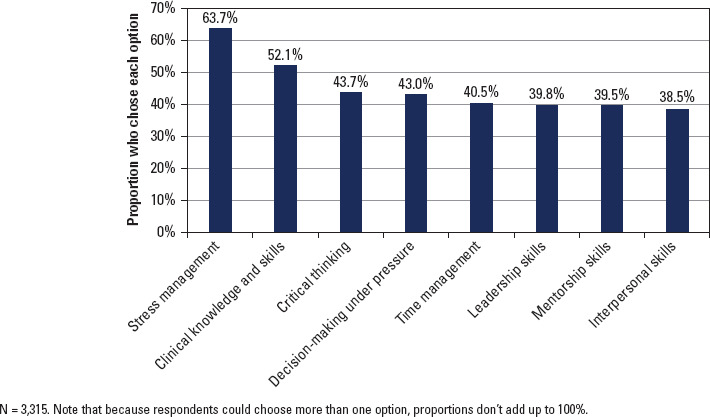
Bonus figure 4: Perceived skill/ability shortages indicated by emergency/trauma/transport nurses
Figure.
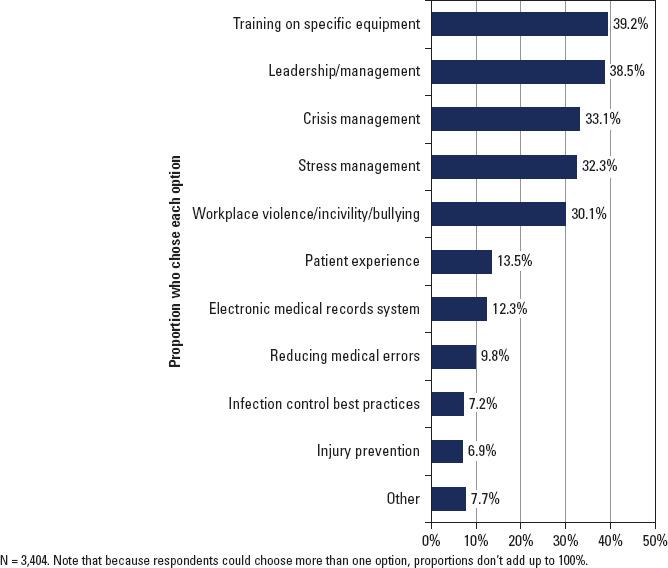
Bonus figure 5: Types of most-needed training indicated by emergency/trauma/transport nurses
Figure.
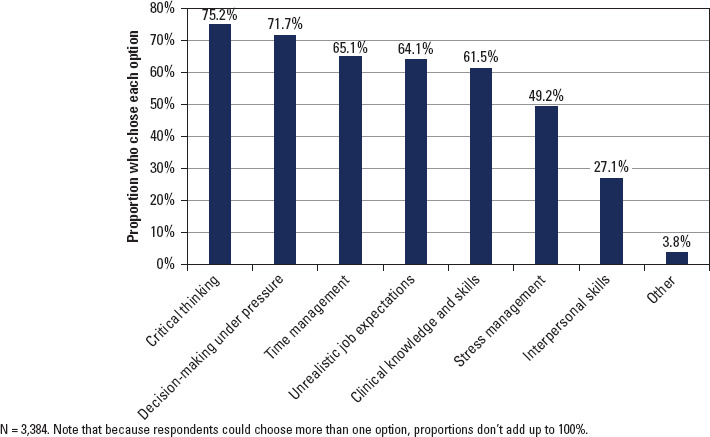
Bonus figure 6: Perceived skill/ability gaps of new emergency/trauma/transport nurses
Figure.
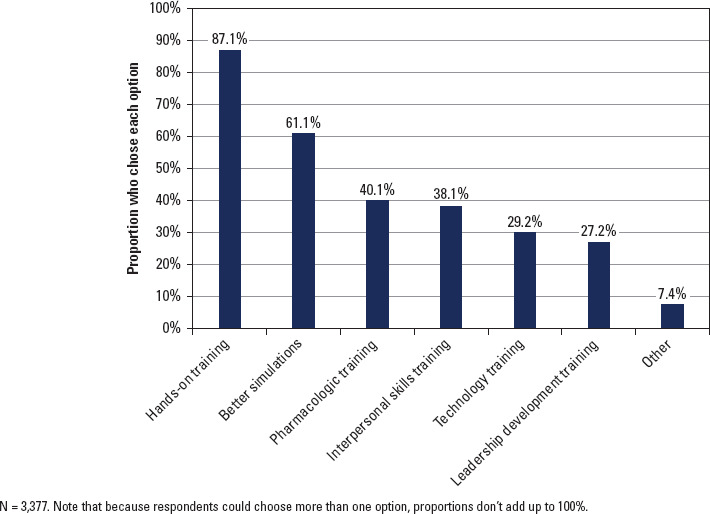
Bonus figure 7: Recommended changes to nursing education to prepare emergency/trauma/transport nurses
Figure.
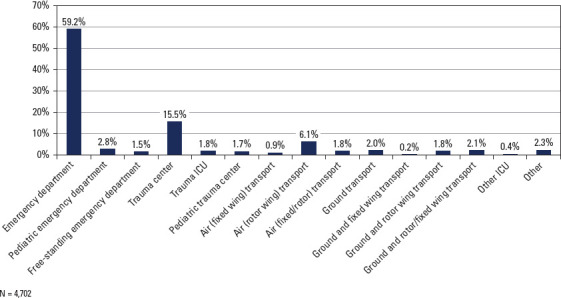
Bonus figure 8: Work setting of emergency/trauma/transport nurses
Figure.
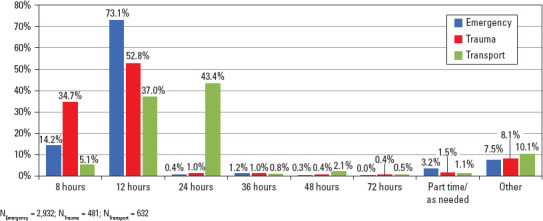
Bonus figure 9: Shift length/work schedule for emergency/trauma/transport nurses by specialty
Figure.
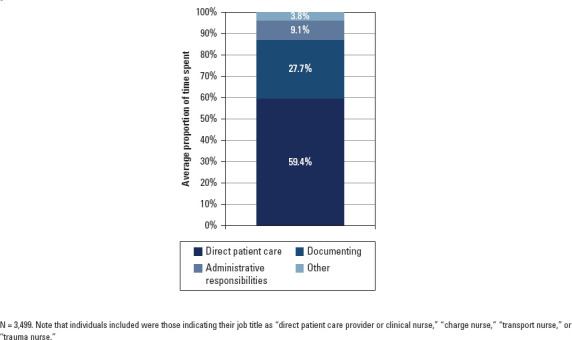
Bonus figure 10: Time spent across activities for emergency/trauma/transport nurses in direct patient care roles
Figure.
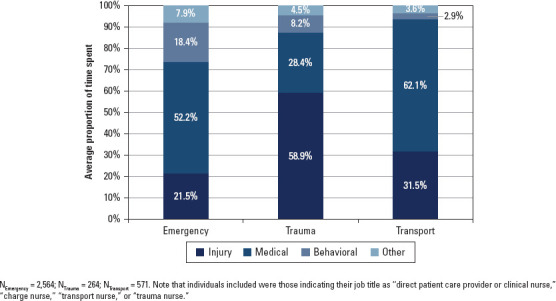
Bonus figure 11: Time spent in direct patient care for emergency/trauma/transport nurses in direct patient care roles, by specialty, across types of cases
Figure.
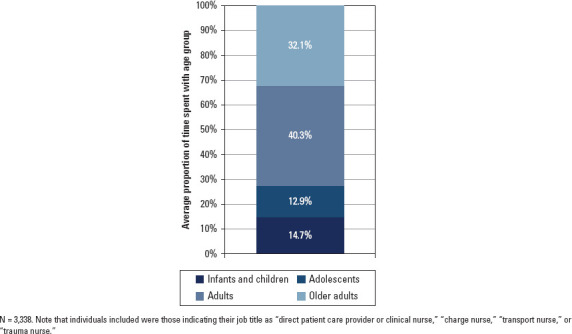
Bonus figure 12: Time spent in direct patient care across age groups for emergency/trauma/transport nurses in direct patient care roles
Figure.
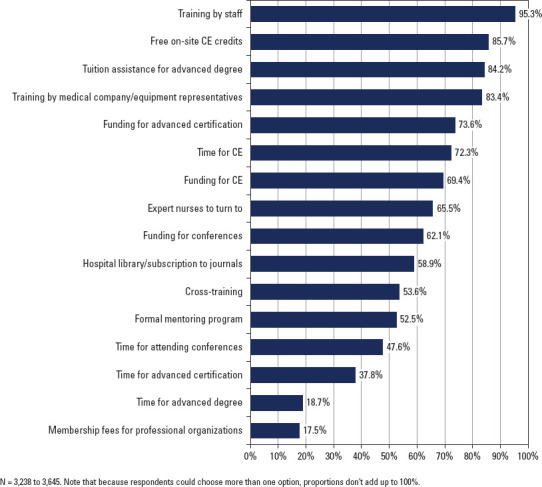
Bonus figure 13: Professional development resources provided for emergency/trauma/transport nurses by their employers
Figure.
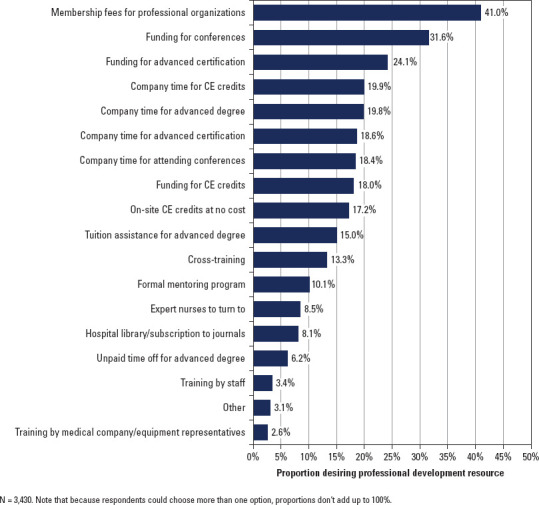
Bonus figure 14: Professional development resources most desired by emergency/trauma/transport nurses
Figure.
Bonus figure 15: Salary distribution for full-time emergency/trauma/transport nurses by specialty
Figure.
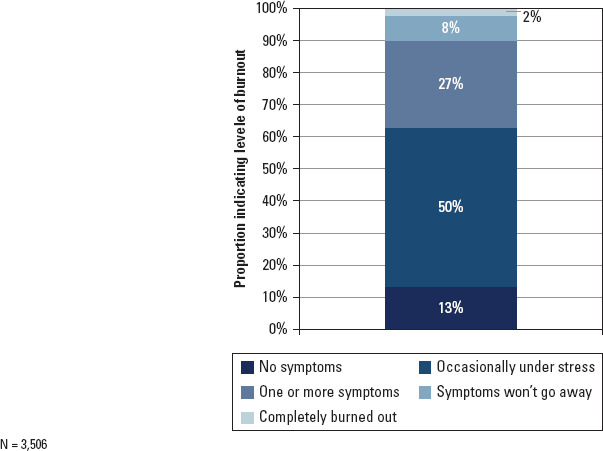
Bonus figure 16: Burnout levels reported by emergency/trauma/transport nurses
Figure.
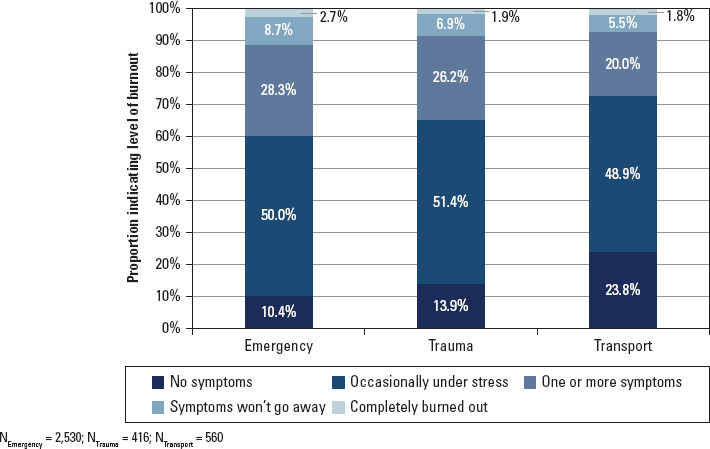
Bonus figure 17: Burnout levels reported by emergency/trauma/transport nurses by specialty
Figure.
Bonus figure 18: Burnout levels reported by emergency/trauma/transport nurses by age
Figure.
Bonus figure 19: Emergency/trauma/transport nurses forecast for the degree of shortage of nursing professionals in their emergency nursing specialty in the next 5 to 10 years
Figure.
Bonus figure 20: Original career plans for emergency/trauma/transport nurses when they first entered their respective fields
Figure.
Bonus figure 21: Age distribution for emergency/trauma/transport nurses who've obtained their RN in the last 10 years
Emergency, Trauma, and Transport Nursing Workforce Study
Purpose of the Research, What Will be Required of Participants, and Length of Commitment
The Board of Certification for Emergency Nursing (BCEN), the Air & Surface Transport Nurses Association (ASTNA), the Emergency Nurses Association (ENA), and the Society of Trauma Nurses (STN) have partnered with MedEvac Foundation International and the Human Resources Research Organization (HumRRO) to conduct a survey to better understand the workforce along the emergency nursing spectrum, including emergency, trauma, and transport nurses.
The survey will ask about your experience in emergency, trauma, and transport nursing, including the challenges you face, the resources that are most valuable to you, your overall job satisfaction and feelings of burnout, typical career paths for someone in your role, and your future career plans. Completing this survey will take about 20-30 minutes of your time.
Potential Risks
Participating in this study presents no risks. Participation is completely voluntary, and you may choose not to answer any or all questions or stop the survey at any time without consequence. If you choose not to answer a question for any reason, you may simply skip it and continue with the rest of the survey.
Potential Benefits
The results of this study will provide a profile of the workforce along the emergency nursing spectrum and inform future research and other actions to address the issues facing this particular workforce.
All individuals who participate may choose to be entered in a drawing for one of 20 gift cards, each worth $200. Click here for full details regarding the drawing.
How Data will be Secured and Respondent Confidentiality Maintained
Your responses to this survey will be anonymous, and all responses will be stored on a secure server. If you choose to enter the drawing for a gift card, your email address will be stored in a separate database from the rest of your survey results. Furthermore, HumRRO will provide only aggregated data when reporting the results; no individual data will be provided.
We thank you in advance for your time to complete the survey. Questions about the purpose of the study as well as questions about technical support may be directed to MedEvac@humrro.org.
By clicking “Start Survey” below you are indicating that you agree to participate in this research.
Once you begin the survey, we encourage you to save the link found at the bottom of the survey. This will allow you to resume completion of the survey in case you need to finish the survey at a later time.
Section 1: Education/Licensure
1. What is your highest level of nursing education?
Vocational/Practical certificate–nursing
Diploma–nursing
Associate degree–nursing
Bachelor's degree–nursing
Master's degree–nursing
Doctoral degree–nursing
N/A
Other (please specify)
2. In what year did you obtain each of the following nursing licenses? If you have not obtained the nursing license, please select NA.
LPN:
RN:
APRN:
2a. (If have obtained an APRN) What is your specific certification as an Advanced Practice RN?
Nurse Practitioner
Clinical Nurse Specialist
Certified Registered Nurse Anesthetist
Certified Nurse Midwife
Not licensed/certified as any of the above
Other (please specify)
3a. What is your highest level of nonnursing education?
High school diploma/GED
Some college
Associate degree
Bachelor's degree
Master's degree
Doctoral degree
Other (please specify)
3b. Please indicate the specific area of study (for example, general studies, biology, engineering).
4. What is the current status of the highest nursing license you have obtained?
Active
Inactive
Unknown
I have not obtained a nursing license
5. How many nursing jobs do you currently hold?
0
1
2
3 or more
6. How many total hours do you work during a typical week across all your nursing positions?
Section 2: Current and Past Work
7. What is your employment status? (select all that apply)
Actively employed in nursing – Full–time
Actively employed in nursing – Part–time
Actively employed in nursing – Active duty military
Actively employed in nursing – Reserve military (e.g., Army National Guard, Navy Reserve, etc.)
Actively employed in nursing – Per diem
Actively employed in nursing – Seasonal
Actively employed in a field other than nursing – Full–time
Actively employed in a field other than nursing – Part–time
Actively employed in a field other than nursing – Per diem
Actively employed in a field other than nursing – Seasonal
Volunteering as a nurse
In transition/unemployed – Seeking work as a nurse
In transition/unemployed – Not currently seeking work as a nurse
Active student – Full–time
Active student – Part–time
Retired
Other (please specify)
7a. (If “In Transition”) How many years ago did you leave your most recent emergency/trauma/ transport nursing position?
7b. (If “Active Duty Military” or “Reserve Military”) In what branch of the military are you currently serving?
7c. (If “Active Duty Military” or “Reserve Military”) Where are you currently stationed?
7d. (If not Actively employed or Volunteering as a nurse) Please indicate the reason(s) that you are not currently seeking work as a nurse. (select all that apply)
Taking care of home and family
Disabled
Inadequate salary
School
Difficulty in finding a nursing position
Seeking work in other fields instead
Other (please specify)
8a. In what specialty do you currently and primarily work? If you are not currently employed, please indicate the specialty in which you primarily worked most recently.
Emergency
Trauma
Critical Care
Transport
Other (please specify)
8b. In what other specialties do you currently work? (select all that apply)
Emergency
Trauma
Critical Care
Transport
Other (please specify)
9. How long have you worked in your current and primary specialty? (in years) Please include time in your current organization and other organizations where you were working in the same specialty. If less than 1 year, please input a decimal response, such as .25 for 3 months, .5 for 6 months, .75 for 9 months.
The next series of questions are about your primary nursing position. If you work in more than one setting, please focus on the one where you spend the most time. If you are unemployed, please answer regarding your most recent emergency/trauma/transport nursing role. If any questions do not apply to your current situation you may simply leave those questions blank.
10. How many years have you worked in your current primary nursing position for your current organization? If less than 1 year, please input a decimal response, such as .25 for 3 months, .5 for 6 months, .75 for 9 months.
11. Please identify the position title that most closely corresponds to your primary nursing position.
Direct Patient Care Provider or Clinical Nurse
Charge Nurse
Transport Nurse
Consultant/Nurse Researcher
Nurse Executive
Nurse Manager
Nurse Faculty/Educator
Advanced Practice Nurse
Trauma Program Manager/Coordinator
Trauma Nurse
Other–Health Related
Other–Not Health Related
Table.
No caption available.
11a. If you selected “Other–Health Related” or “Other–Not Health Related,” please indicate your position title in the box below.
12. Below is a list of credentials, board certifications, and certificates. Please indicate a) which of the following you have and b) whether it is required or recommended for your current primary nursing position. Note that if you must have one of two potential credentials (for example, either LPN or RN), you may simply indicate that both are required.
12a. If you indicated other credentials, board certifications, or certificates above, please indicate the name of each in the box below.
13. In what setting do you primarily work?
Hospital – Emergency Department
Hospital – Trauma Center
Hospital – Pediatric Emergency Department
Hospital – Pediatric Trauma Center
Hospital – ICU (Neonatal ICU)
Hospital – ICU (Pediatric ICU)
Hospital – ICU (Neuro ICU)
Hospital – ICU (Coronary/Cardiothoracic ICU)
Hospital – ICU (Trauma ICU)
Hospital – ICU (Surgical ICU)
Hospital – ICU (Other than those listed above)
Hospital – Burn Unit
Hospital – Neurological Unit
Transport – Ground
Transport – Air (Fixed Wing)
Transport – Air (Rotor Wing)
Transport – Air (Both Fixed Wing and Rotor Wing)
Transport – Both Ground and Air (Rotor Wing)
Transport – Both Ground and Air (Fixed Wing)
Transport – Both Ground and Air (Both Fixed Wing and Rotor Wing)
Transport – Commercial Medical Escort
Nursing Home/Extended Care/Assisted Living Facility
Rehabilitation Center
Free–standing Emergency Department
Urgent Care
Home Health
Correctional Facility
Academic Setting
Public Health
Community Health
School Health Service
Occupational Health
Ambulatory Care Setting
Insurance Claims/Benefits
Policy/Planning/Regulatory/Licensing Agency
Other (please specify)
13a. (If Transport) On average, how many calls does your unit respond to in a 24–hour period?
13b. (If Hospital [but not ICU]) What is the bed count of the hospital where you work?
13c. (If Hospital or Pediatric Trauma Center) What type of trauma center do you work in?
Level I
Level II
Level III
Level IV
Level V
14. Please indicate the proportion of your time that you spend in each of the following activities at your primary nursing position (values must add to 100%):
Direct patient care
Documenting
Administrative responsibilities
Other
14a. If you indicated a percentage greater than zero for “Other,” please explain below.
15. For the time you spend on direct patient care, please indicate the proportion of your time you spend working with patients in each of the categories below (values must add to 100%). If you do not currently work in direct patient care in your primary nursing position, please leave this question blank.
Injury (burn, car crash, fall, gunshot wound, etc.)
Medical Emergencies (heart attack, stroke, asthma, etc.)
Behavioral Health
Other
15a. If you indicated a percentage greater than zero for “Other,” please explain below.
16. Approximately what percentage of your time in direct patient care is spent with patients in each of the following age categories (values must add to 100%)? If you do not currently work in direct patient care in your primary nursing position, please leave this question blank.
Infants and children (0 years to approximately 12 years)
Adolescents (approximately 13 years to approximately 18 years)
Adults (approximately 19 years to approximately 65 years)
Older adults (approximately 66 years and older)
17. Please indicate the number of years you have worked in the areas of the nursing field listed below, including in your current primary nursing position. You may leave the areas where you have not worked blank. If less than 1 year, please use decimals, such as .25 for 3 months. If you worked in the medical field in an area other than as a nurse (for example, as an EMT) then list that area in the “Other” category. If you worked in two areas at the same time (for example, fixed wing and rotor wing) then divide the time you spent between the two areas (for example, if you worked 10 years doing both fixed wing and rotor wing flights, but only 10% of your time was spent doing fixed wing flights, then enter 1 for fixed wing and 9 for rotor wing).
Hospital – Emergency Department (not including Trauma Centers or Pediatric Emergency Departments)
Hospital – Trauma Center (not including Pediatric Trauma Centers)
Hospital – Pediatric Emergency Department
Hospital – Pediatric Trauma Center
Hospital – ICU (Neonatal ICU)
Hospital – ICU (Pediatric ICU)
Hospital – ICU (Neuro ICU)
Hospital – ICU (Coronary/Cardiothoracic ICU)
Hospital – ICU (Trauma ICU)
Hospital – ICU (Surgical ICU)
Hospital – ICU (other: please specify)
Hospital – Burn Unit (not including ICU)
Hospital – Neurological Unit (not including ICU)
Hospital – Cardiology (not including ICU)
Hospital – General surgery (not including ICU)
Hospital – Other (not including ICU, please specify)
Transport – Ground (Nurse)
Transport – Air (Fixed Wing)
Transport – Air (Rotor Wing)
Transport – Commercial Medical Escort
Nursing Home/Extended Care/Assisted Living Facility
Rehabilitation Center
Free–standing Emergency Department
Urgent Care
Home Health
Correctional Facility
Academic Setting
Public Health
School Health Service
Occupational Health
Ambulatory Care Setting
Insurance Claims/Benefits
Policy/Planning/Regulatory/Licensing Agency
Other (please specify)
18. What positions and experiences have been most beneficial in preparing you for your current primary nursing position? If you are not currently employed, please answer regarding your most recent emergency/trauma/transport nursing position.
19a. Please indicate the type of military experience you have. (select all that apply)
None
National Guard
Army
Air Force
Navy
Marines
Coast Guard
Other (please specify)
19b. How has your military service impacted your current work as an emergency/trauma/transport nurse? If you are not currently employed, please answer regarding your most recent emergency/trauma/transport nursing role.
20. How many hours do you work during a typical week? Please indicate how many hours you actually work, instead of how many hours you're scheduled to work. As with all questions on the pages in this section, please answer regarding your primary nursing position.
21. On average, how many days per week do you typically work in your primary nursing position?
0
1
2
3
4
5
6
7
22. What is your typical work schedule?
As–needed shifts
Part–time (less than 8–hour shifts)
8–hour shifts
12–hour shifts
24–hour shifts
36–hour shifts
48–hour shifts
72–hour shifts
Other (please specify)
23. When does your shift begin?
Morning
Afternoon
Evening
Middle of the night
Varies
Other (please specify)
24. How many hours do you typically work compared with what you were hired to work?
Far fewer hours than I was hired to work
Fewer hours than I was hired to work
About the same number of hours I was hired to work
More hours than I was hired to work
Far more hours than I was hired to work
25. How often are you assigned mandatory overtime?
More than once per week
Once per week
Two to three times per month
Once per month
A few times a year
Once a year
Almost never
Never
26. How would you describe your workload?
Far too light
A bit too light
About right
Too heavy
Overwhelming
27. How would you describe the staffing level of nurses in your organization?
Understaffed
About right
Overstaffed
28. Which best describes the main setting of your work?
Urban
Suburban
Rural
Other (please specify)
29. What responsibilities/duties do you have that fall outside the typical scope of patient care (because of understaffing, because of the unique nature of emergency/trauma/transport nursing, etc.)? If you are not currently employed, please answer regarding your most recent emergency/trauma/transport nursing role. If you do not work in patient care, you may skip this question.
Section 3: Job Attitudes and Resources
30. Which resources does your primary employer provide to support your professional growth and development? Of the resources/professional growth opportunities that your employer does provide, which have you used? Note that “company–provided time” indicates that you do not need to use time off (either paid time off, unpaid time off, or times outside the typical work day) for the specific activity.
Table.
No caption available.
31. What other resources not listed on the previous pages does your primary employer provide to support your professional growth and development? Have you used these resource(s)? If you are not currently employed, please answer regarding your most recent emergency/trauma/transport nursing role.
32. Of the resources below, please indicate the top three resources that you wish your employer would provide. Please use the “other” box at the bottom to list any other resources you wish your employer would provide.
On–site continuing–education credits at no cost
Funding for continuing–education credits
Company–provided time for obtaining continuing–education credits (provided on–site, online, or off–site)
Funding for obtaining advanced certifications
Company–provided time for obtaining advanced certifications
Tuition assistance for obtaining an advanced degree
Company–provided time to obtain an advanced degree
Unpaid time off to obtain an advanced degree
Training by staff (either on the job or in a classroom)
Training by medical company/equipment representatives (either on the job or in a classroom)
Cross–training to other units, vehicles, or patient types
Funding for attending conferences
Company–provided time for attending conferences
Membership fees for professional organizations
Hospital library or subscription for medical journals
Formal mentoring program by other nurses
Expert nurse that nurses can turn to for guidance
Other (please specify)
33. Please indicate your agreement with the following statements regarding your primary nursing position.
Table.
No caption available.
34. What type of training and development do you feel most in need of? (select up to 3)
Training on specific types of equipment
Leadership/management training
Crisis management training
Training for reducing medical errors
Training on infection control best practices
Electronic medical record system training
Stress management training
Patient experience training
Injury prevention
Workplace violence/incivility/bullying
Other (please specify)
Table.
No caption available.
34a. If you indicated in the question above that you are in most need of training on specific types of equipment, please describe the equipment here. If you did not indicate you are in most need of this type of training, please leave the field blank.
35. Using the scale below, please indicate the extent to which you agree or disagree with the following statements regarding your primary nursing position.
Table.
No caption available.
36. Using the scale below, please indicate the extent to which you agree or disagree with the following statements regarding your primary nursing position.
37. Overall, based on your definition of burnout, how would you rate your level of burnout?
I enjoy my work. I have no symptoms of burnout.
Occasionally I am under stress, and I don't always have as much energy as I once did, but I don't feel burned out.
I am definitely burning out and have one or more symptoms of burnout, such as physical and emotional exhaustion.
The symptoms of burnout that I'm experiencing won't go away. I think about frustration at work a lot.
I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help.
38. What resources does your employer provide to deal with the stress of the job and/or help prevent burnout? (select all that apply)
Access to counselors
Meditation training (e.g., mindfulness)
Training on managing stress
Training on dealing with burnout
Training on self–care strategies
Conflict resolution
Time management
None
Other (please specify)
39. What resources would you like your employer to provide to deal with stress/burnout?
Section 4: Job Outlook
40. How many more years do you plan to stay in your current primary nursing position?
1 = Less than 1 year
2 = 1-4 years
3 = 5-9 years
4 = 10-19 years
5 = 20+ years
41. How many more years do you plan to stay with your current organization (that is, the organization in which you have your current primary nursing position)?
Less than 1 year
1-4 years
5-9 years
10-19 years
20+ years
42. How many more years do you plan to stay in the field of emergency/trauma/transport nursing?
Less than 1 year
1-4 years
5-9 years
10-19 years
20+ years
43. What are your career plans in the next 5 to 10 years? (select all that apply)
Continue working in your current role
Obtain specialty nursing certification
Move into a supervisory role within your specialty
Move into a management role within your organization
Move into a management role in another organization
Move into a nursing role in another specialty
Become an advanced practice nurse (nurse practitioner, nurse anesthetist, etc.)
Move into another healthcare practitioner role outside of nursing (e.g., physician assistant)
Move into a role outside of healthcare
Move into an academic role
Move into a nursing education role
Retire from nursing
Other (please specify)
44. Based on current trends, what do you perceive as the forecast for the number of nursing professionals in your specific industry in the next 5 to 10 years? (If you are in transport nursing, answer regarding transport nurses, if you are in emergency nursing, answer regarding emergency nurses, etc.)
Extreme shortage
Shortage
About right
More than needed
Far more than needed
45. What would be the most helpful in the next 5 to 10 years to ensure that there is a sufficient number of emergency/trauma/transport nurses in the US? (You may select up to 3; if you are in transport nursing, answer regarding transport nurses, if you are in emergency nursing, answer regarding emergency nurses, etc.)
Higher pay
More publicity regarding the profession of emergency/trauma/transport nursing
More reasonable hours
More discussion of the profession in nursing school
More employer support of nursing in general
Improved nurse–to–patient ratios
Other (please specify)
46. When you entered the field of emergency/trauma/transport nursing, what were your long–term career plans? (select all that apply)
Continue working in that role for remainder of career
Move into a supervisory role within the specialty
Move into a management role within the organization
Move into a management role in another organization
Move into a nursing role in another specialty
Become an advanced practice nurse (nurse practitioner, nurse anesthetist, etc.)
Move into another healthcare practitioner role outside of nursing (e.g., physician assistant)
Move into an academic role
Move into a nursing education role
Move into a role outside of healthcare
No specific plans
Other (please specify)
47a. We are interested in understanding the typical career path for someone in your emergency/trauma/transport nursing position. Please indicate how common the following career paths are for someone in your current primary nursing position.
Table.
No caption available.
47b. Please list any other typical career paths, along with how common they are using the same scale as above.
48. What skill or ability shortages currently exist among nurses in your field of emergency/trauma/transport nursing? (Select all that apply. If you are in transport nursing, answer regarding transport nurses, if you are in emergency nursing, answer regarding emergency nurses, etc.)
Stress management
Decision–making under pressure
General clinical knowledge and skills
Interpersonal skills
Leadership skills
Mentorship skills
Time management
Critical thinking
Other (please specify)
49. In what ways are new recruits to your specialty in emergency/trauma/ transport nursing unprepared? (Select all that apply. If you are in emergency nursing, answer regarding emergency nurses, etc.)
Stress management
Decision–making under pressure
General clinical knowledge and skills
Interpersonal skills
Unrealistic job expectations
Time management
Critical thinking
Other (please specify)
50. In what ways must nursing education be adjusted to prepare nurses for emergency/trauma/transport nursing as it will exist in the future? (Select all that apply. If you are in emergency nursing, answer regarding emergency nurses, etc.)
More training on technology
More hands–on training
More pharmacologic training
Better simulations
More training on interpersonal skills
More leadership development training
Other (please specify)
51. What are the biggest challenges you see that emergency/trauma/transport nursing faces overall?
Section 5: Impact
52. We would like to help others understand how vital a role emergency/trauma/transport nurses have. To explore this, please provide an example of when you, or one of your nursing colleagues, did something that had an important impact on human, medical, or operational outcomes. Please describe the situation and location, what happened, your response, and the resolution or outcomes. Do not use specific names of people or places.
Section 6: Demographics
53. What is your gender?
I prefer not to answer.
Male
Female
Other
54. What is your race/ethnicity? (select all that apply)
Native American or Alaska Native
Asian
Black
Native Hawaiian or Other Pacific Islander
White
Hispanic
Other (please specify)
Table.
No caption available.

55. In what year were you born? (drop down list from 1900 to 2005)
56. To what organizations do you belong? (select all that apply)
Air & Surface Transport Nurses Association (ASTNA)
Board of Certification for Emergency Nursing (BCEN)
Emergency Nurses Association (ENA)
Society of Trauma Nurses (STN)
Other (please specify)
57. What type of nursing degree/credential qualified you for your first US nursing license?
Vocational/Practical certificate–nursing
Diploma–nursing
Associate degree–nursing
Bachelor's degree–nursing
Master's degree–nursing
Doctoral degree–nursing (PhD)
Doctoral degree–nursing (DNP)
58. In what zip code do you primarily work?
59. Please indicate the locations in which you are currently practicing as a nurse. (select all that apply)
60. What is your annual salary for your primary nursing position?
Less than $35,000
$35,000-$39,999
$40,000-$44,999
$45,000-$49,999
$50,000-$54,999
$55,000-$59,999
$60,000-$64,999
$65,000-$69,999
$70,000-$74,999
$75,000-$79,999
$80,000-$84,999
$85,000-$89,999
$90,000-$94,999
$95,000-$99,999
$100,000-$104,999
$105,000-$109,999
$110,000-$114,999
$115,000-$119,999
$120,000-$124,999
$125,000-$129,999
$130,000-$134,999
$135,000-$139,999
$140,000-$149,999
$150,000-$159,999
$160,000-$169,999
$170,000-$179,999
$180,000-$189,999
$190,000-$199,999
$200,000 or more
Throughout the survey, there were multiple questions asking you to type a response. When reporting results of these types of studies, sometimes it helps to provide verbatim responses from such questions to highlight certain themes that arose. May we have permission to use your verbatim responses in our reporting of this study. Note that at no point will we ever link your responses to your identity.
Yes
No
Thank you very much for completing the survey. If you would like to enter the drawing for one of the 20 $200 gift cards, please click the link below. The link will take you to a separate page where you can enter your email. By redirecting you to another page, we are making it so that your email address is stored in a separate dataset from the rest of your data. Once the survey closes, we will randomly select the winners. Winners will be notified via email by March 14, 2019. Click here for full details regarding the drawing.
Note that the gift card can be used at a variety of retailers or donated to a variety of nonprofit organizations.
Thank you again for completing the survey. To be entered into the drawing for one of 20 $200 gift cards, please enter your email address below. Your email address will be stored in a separate dataset from the rest of your survey data. For full details regarding the drawing, please click here.


