The characteristic feature of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19 disease) is that its course is asymptomatic or mild in the majority of cases, while increasing age and/or underlying cardiovascular diseases predispose for a severalfold increased case fatality rate.1 This association has not been explained as yet, and several potential mechanisms have been put forward to uncover why the course of the disease is more severe in elderly patients with underlying cardiovascular risk factors and/or cardiovascular diseases. Some hypotheses have been proposed, including the role of angiotensin-converting enzyme 2 (ACE2) (a functional receptor for SARS-CoV-2), accelerated ageing of the immune system, or other mechanisms linked to comorbidities.1 However, it has been recently reported that SARS-CoV-2 virus-induced endotheliitis and microvascular endothelium pathology could contribute to vascular bed dysfunction in different organs and to fatal clinical sequelae in COVID-19 patients.2 Indeed, in patients who died from COVID-19, severe endothelial injury, widespread thrombosis, and microangiopathy were detected,3 pointing to the important role of vascular pathophysiology and alterations in endothelial function in COVID-19 disease. In fact, a biomarker of endothelial activation and altered endothelial permeability, angiopoietin-2, was found to be a good predictive factor for severe cases of COVID-194 disease underscoring important pathophysiological role of vascular endothelial dysfunction in COVID-19, with its distinct vascular endotype.5
Here we suggest that the severity of COVID-19, increasing with patient age and/or the presence of cardiovascular comorbidities, might also be associated with the impairment of platelet-dependent mechanisms preserving the integrity of the endothelial barrier. Indeed, platelet-dependent endothelium-protective mechanisms play an important role in acute and chronic inflammatory conditions,6 and might safeguard the endothelial barrier of the pulmonary microcirculation alongside COVID-19-induced hyperinflammation. These protective mechanisms might be hampered or lost, particularly in patients with pre-existing endothelial dysfunction with inhibited platelet function or evolving thrombocytopenia, which was reported to predict severe cases of COVID-19.7
Classical and non-classical inflammation-associated haemostasis
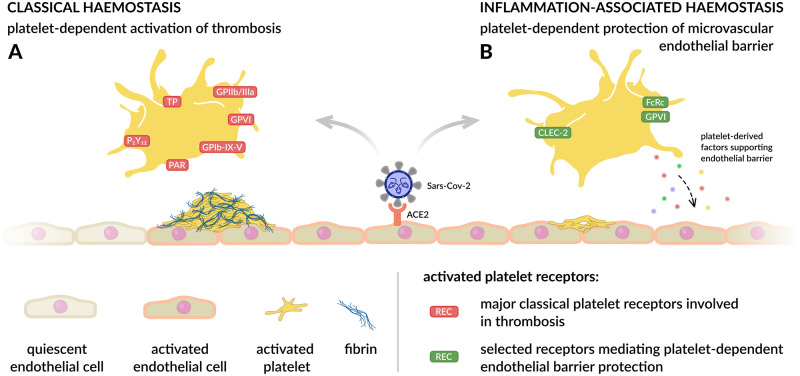
Mechanisms of classical haemostasis activated in response to vascular injury and contributing to cardiovascular diseases are well known. They involve binding of the GPIb–IX–V complex on platelets to immobilized von Willebrand factor and platelet GPVI binding to collagen, thromboxane A2 production, ADP release, as well as activation of the platelet GPIIb/IIIa receptor with subsequent prothrombinase complex formation and thrombin generation to convert soluble fibrinogen into fibrin (Figure 1A). However, platelet-dependent mechanisms are also involved in the protection of the endothelial barrier in acute and chronic inflammation in the processes that have been recently termed as non-classical inflammation-associated haemostasis.6 In fact, platelets that participate in the early immune response serve as gatekeepers of the vascular wall, protecting the endothelial barrier against leaks, subsequent bleeding, and excessive inflammatory damage.6 The mechanisms of platelet-dependent maintenance of endothelial barrier integrity also seem to be critical in the context of viral infections as their impairment results in bleeding and vascular damage.8 Platelet-dependent mechanisms maintaining endothelial barrier also operate in a number of other conditions, including bacterial infections, injection of immune complexes and irritants, ischaemia–reperfusion, and irradiation,6 and may be of importance in cancer-related inflammation, as recently reviewed by us.9
Figure 1.
Prothrombotic and protective facets of platelet function that both could be of importance in SARS-CoV-2 infection. (A) Platelet-dependent mechanisms leading to thrombus formation involve activation of classical platelet receptors: TP (thromboxane receptor), P2Y12 (ADP receptor), PAR (thrombin receptors), GPIb–IX–V (von Willebrand receptor), GPVI (collagen receptor), and GPIIb/IIIa (fibrinogen receptor). (B) Platelet-dependent mechanisms of inflammation-associated haemostasis preventing bleeding associated with inflammation are stimulus and organ dependent and may involve the platelet hemITAM receptor CLEC-2 activated by podoplanin (expressed, for example, on activated monocytes), platelet ITAM FcRc receptor functionally associated with platelet collagen receptor GPVI, platelet secretion of factors supporting the endothelial barrier (angiopoetin-1), and/or direct sealing of the hole within the endothelial monolayer by platelets.6,9,11,15
The mechanisms by which platelets preserve vascular integrity and prevent inflammatory bleeding are not well understood. Although they initially seemed to be quite distinct and independent from coagulation-related mechanisms, recent evidence suggests that they overlap with classical prothrombotic platelet pathways. Platelets may prevent inflammatory bleeding by (i) the release of endothelium-stabilizing factors from platelet granules; (ii) the activation of platelet C-type lectin receptor CLEC-2 containing the hemITAM motif (binding to podoplanin or S100A13) or the activation of the platelet collagen GPVI receptor associated constitutively with the FcRγ; (iii) by direct interaction of single platelets plugging the exit sites for erythrocytes within the endothelial monolayer (Figure 1B)6,9.
Platelets safeguard the integrity of the pulmonary microcirculation
It is increasingly recognized that patients with COVID-19 are at significant risk of thrombo-embolic complications affecting the arterial and venous vascular systems, as well as the pulmonary circulation,3 and, therefore, various thromboprophylactic regimens are recommended.10 Increased SARS-CoV-2 infection-induced risk of thrombosis seems to result from excessive platelet activation, endothelial dysfunction, and stasis.2,3 On the other hand, severe COVID-19 disease features exaggerated systemic inflammation associated with cytokine storm characterized by multiple organ failure, including the lungs affected by acute respiratory distress syndrome (ARDS).11 The intensity of the inflammatory response is closely linked to mortality, as shown by retrospective clinical studies revealing that non-survivors exhibited higher levels of interleukin-6 (IL-6), ferritin, and C-reactive protein (CRP).12 Furthermore, pulmonary endothelium may play a central role in the pathogenesis of ARDS related to COVID-19, not only by altering vessel integrity but also by fostering procoagulative and proinflammatory processes, as well as by gate-keeping of the immune response to virus infection.13 Therefore, it is tempting to suspect that mechanisms of non-classical platelet-dependent inflammation-associated haemostasis could be of key importance with respect to endothelial barrier integrity in the pulmonary circulation in COVID-19.
Indeed, platelet-dependent mechanisms have been shown to preserve pulmonary vascular integrity in health and alongside an inflammatory disease, as evidenced by induction of thrombocytopenia that increased permeability of the pulmonary microcirculation in several experimental models, such as isolated perfused sheep and rabbit lungs, and in in vivo murine models of bacterial pneumonia-induced sepsis and lipopolysaccharide-induced acute lung injury.14 These observations were supported by in vitro experiments whereby isolated human platelets reduced the permeability of endothelial cell monolayers.14 Vascular leak associated with low platelet counts was also reported in a patient with mild thrombocytopenia in inflamed skin areas following a sunburn insult.14 Finally, in a recent study, Lax and colleagues demonstrated in the mouse model of ARDS that platelet CLEC-2 protected against lung injury and subsequent inflammation-induced alveolar capillary permeability via effects of its ligand podoplanin on inflammatory alveolar macrophages.11 Altogether, solid evidence supports the role of platelets in the protection of vascular integrity, and novel mechanisms of platelet-dependent protection against passive fluid leakage in inflammation based on platelet-derived angiopetin-1 are emerging.15 The safeguarding role of platelets might be of particular importance in the acute inflammatory lung response to infection, as summarized in an excellent review by Middleton and colleagues.14
Summary
Based on the evidence supporting platelet-dependent mechanisms protecting endothelial barrier integrity in inflammation, it is tempting to speculate that increased microcirculation permeability associated with thrombocytopenia or prolonged use of antiplatelet agents and pre-existising endothelial dysfunction of cardiovascular diseases may contribute to the increased severity of COVID-19-related ARDS. Given the age-related decline of the endothelial barrier and platelet function, the detrimental effect of thrombocytopenia or prolonged use of antiplatelets may be specially detrimental for elderly COVID-19 patients. Therefore, it is fundamental to better understand how to dissociate the prothrombotic/proinflammatory mechanisms of platelets from those that protect against vascular leakage so as to be able to strengthen the latter pharmacologically to safeguard the endothelial barrier in the pulmonary microcirculation in patients with acute inflammation at high risk of a severe course of COVID-19 disease. Better understanding of these seemingly opposite, but well-orchestrated facets of platelet function might pave the way for future therapies mimicking platelet-dependent mechanisms maintaining endothelial barrier homeostatis in acute hyperinflammation syndromes such as COVID-19.
Acknowledgements
The authors acknowledge support by the following grants: FNP TEAM POIR.04.04.00-00-5CAC/17-00, SYMFONIA NCN, No DEC-2015/16/W/NZ4/00070, OPUS NCN, No 2018/29/B/NZ7/01684, and STRATEGMED1/233226/11/NCBR/2015 (to S.C.H.). The open-access publication of this article was funded by the Priority Research Area BioS under the program “Excellence Initiative – Research University” at the Jagiellonian University in Krakow.
Conflict of interest: none declared.
Authors

Biography: Marta Smeda is a research assistant in the Jagiellonian Centre of Experimental Therapeutics (JCET) at the Jagiellonian University in Krakow, Poland. Currently her interests are concentrated around the effects of antiplatelet regimens on cancer progression and metastatic spread, the non-classical functions of platelets, and endothelial mechanisms of haemostasis.

Biography: Stefan Chlopicki is a Professor of Pharmacology at the Chair of Pharmacology at Jagiellonian University Medical College, and an initiator and Director of the Jagiellonian Centre for Experimental Therapeutics (JCET), the newly established interdisciplinary academic research centre at Jagiellonian University (www.jcet.eu) devoted to interdisciplinary research on endothelial biomedicine. His major research interests include the pathophysiology, biochemistry, and pharmacology of endothelium, the role of endothelial mediators in vascular inflammation, and the pharmacology of platelets.
References
- 1. Kreutz R, Algharably EAE-H, Azizi M, Dobrowolski P, Guzik T, Januszewicz A, Persu A, Prejbisz A, Riemer TG, Wang J-G, Burnier M.. Hypertension, the renin–angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for COVID-19. Cardiovasc Res 2020;116:1688–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H.. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ackermann M, Verleden SE, Kuehnel MK, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Danny Jonigk D.. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 2020;doi:10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smadja DM, Guerin CL, Chocron R, Yatim N, Boussier J, Gendron N, Khider L, Hadjadj J, Goudot G, Debuc B, Juvin P, Hauw-Berlemont C, Augy J-L, Peron N, Messas E, Planquette B, Sanchez O, Charbit B, Gaussem P, Duffy D, Terrier B, Mirault T, Diehl J-L.. Angiopoietin-2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID-19 patients. Angiogenesis 2020;doi: 10.1007/s10456-020-09730-0.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mangalmurti NS., Reilly JP., Cines DB., Hunter CA., Meyer NJ., Vaughan AE. COVID-ARDS Clarified: A Vascular Endotype? Am J Respir Crit Care Med 2020; 10.1164/rccm.202006-2598LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ho-Tin-Noé B, Boulaftali Y, Camerer E.. Platelets and vascular integrity: how platelets prevent bleeding in inflammation. Blood 2018;131:277–288. [DOI] [PubMed] [Google Scholar]
- 7. Lippi G, Plebani M, Henry BM.. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 2020;506:145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zapata JC, Cox D, Salvato MS.. The role of platelets in the pathogenesis of viral hemorrhagic fevers. PLoS Negl Trop Dis 2014;8:e2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smeda M, Przyborowski K, Stojak M, Chlopicki S.. The endothelial barrier and cancer metastasis: does the protective facet of platelet function matter? Biochem Pharmacol 2020;176:113886. [DOI] [PubMed] [Google Scholar]
- 10. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Der Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur A, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH.. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol 2020;75:2950–2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lax S, Rayes J, Wichaiyo S, Haining EJ, Lowe K, Grygielska B, Laloo R, Flodby P, Borok Z, Crandall ED, Thickett DR, Watson SP.. Platelet CLEC-2 protects against lung injury via effects of its ligand podoplanin on inflammatory alveolar macrophages in the mouse. Am J Physiol 2017;313:L1016–L1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Akhmerov A, Marban E.. COVID-19 and the heart. Circ Res 2020;126:1443–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Teuwen L-A, Geldhof V, Pasut A, Carmeliet P.. COVID-19: the vasculature unleashed. Nat Rev Immunol 2020;20:389–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Middleton EA, Weyrich AS, Zimmerman GA.. Platelets in pulmonary immune responses and inflammatory lung diseases. Physiol Rev 2016;96:1211–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Braun LJ, Stegmeyer R, Schäfer K, Volkery S, Currie SM, Kempe B, Nottebaum AF, Vestweber D.. Platelets docking to VWF prevent leaks during leukocyte extravasation by stimulating Tie-2. Blood 2020;doi: 10.1182/blood.2019003442. [DOI] [PMC free article] [PubMed] [Google Scholar]