Abstract
Exposure to acute hypoxia causes a detrimental effect on the brain which is also manifested by a decrease in the ability to perform psychomotor tasks. Conversely, brain-derived neurotrophic factor (BDNF), whose levels are elevated in response to exercise, is a well-known factor in improving cognitive function. Therefore, the aim of our study was to investigate whether the exercise under hypoxic conditions affects psychomotor performance. For this purpose, 11 healthy young athletes performed a graded cycloergometer exercise test to volitional exhaustion under normoxia and acute mild hypoxia (FiO2 = 14.7%). Before, immediately after exercise and after a period of recovery, choice reaction time (CRT) and number of correct reactions (NCR) in relation to changes in serum BDNF were examined. Additionally, other selected factors which may modify BDNF production, i.e., cortisol (C), nitrite, catecholamines (adrenalin-A, noradrenaline-NA, dopamine-DA, serotonin-5-HT) and endothelin-1 (ET-1), were also measured. Exercise in hypoxic conditions extended CRT by 13.8% (p < 0.01) and decreased NCR (by 11.5%) compared to rest (p < 0.05). During maximal workload, NCR was lower by 9% in hypoxia compared to normoxia (p < 0.05). BDNF increased immediately after exercise in normoxia (by 29.3%; p < 0.01), as well as in hypoxia (by 50.0%; p < 0.001). There were no differences in BDNF between normoxia and hypoxia. Considering the fact that similar levels of BDNF were seen in both conditions but cognitive performance was suppressed in hypoxia, acute elevation of BDNF did not compensate for hypoxia-induced cognition impairment. Moreover, neither potentially negative effects of C nor positive effects of A, DA and NO on the brain were observed in our study.
Keywords: brain-derived neurotrophic factor, moderate hypoxia, physical exercise, psychomotor function, reaction time, cortisol, catecholamines, nitrite, endotheline-1, lactate
1. Introduction
Hypoxia is a condition in which some organ(s) or a whole organism is deprived of adequate oxygen supply. Except in very short or static exercises [1,2,3], hypoxia negatively affects exercise performance [4,5]. In particular, the maximal aerobic workload that can be sustained during exercise involving large muscle groups (e.g., cycling, running) is considerably lower in hypoxia compared with normoxia. The origin of human performance limitation in hypoxia is attributed to a decrease in maximal oxygen uptake (VO2max). Dempsey and Wagner [6] observed that each 1% decrement in SaO2% below the 95% level approximates to a 1–2% decrement in VO2max. Diminished VO2max in hypoxia is accompanied by a lowered O2 partial pressure in arterial blood (PaO2), which reduces O2 delivery to tissues and negatively affects muscle metabolism and contraction [7,8], leading to so-called peripheral fatigue. There is also evidence that maximal cardiac output and maximal heart rate (HRmax) during maximal exercise in hypoxia are decreased [9] and the decrease in HRmax is linearly related to the decrease in SaO2% [10]. This effect can be reversed by oxygen administration during hypoxia exposure in both acute [11] and chronic hypoxia [9,11,12,13].
The aforementioned factors do not fully explain the hypoxia-induced reduction in exercise performance. As biochemical, electromyographic and mechanical signs of muscle fatigue are reduced in severe hypoxia compared with normoxia, peripheral (muscle) fatigue may not be the main factor responsible for impaired exercise performance [12,14]. It is well recognized that metabolites produced in working muscles can directly modulate central nervous system (CNS) functions by changes in sensory nerve impulses. Moreover, chemical messengers originating from working muscle are released into the circulation [15] and can affect brain function after their translocation to the CNS. An alternative hypothesis that may, at least partially, explain reduced exercise performance in hypoxic condition attributes it to so-called central fatigue [16]. This assumption is supported by studies showing impairment of cognitive performance [17] by reduced O2 delivery. Several studies [18,19] have reported that moderate levels of hypoxia degraded the ability to perform psychomotor tasks, and the main cause of cognitive impairment is the low PaO2 regardless of the type of hypoxia (normobaric vs. hypobaric) [20].
The negative impact of hypoxia on cognitive functions is manifested by memory deterioration, reduced learning ability, decreased concentration, and psychomotor performance [21]. One of the best indicators of the speed and efficiency of mental processes is choice reaction time (CRT) and the number of correct reactions (NCR), especially if these variables are used to assess the cognitive function within the same group of participants [22,23]. However, in previous studies, the effect of hypoxia on CRT was ambiguous and most likely depended on the time of exposure [24,25] and level of hypoxia: moderate vs. severe [24,26,27]. Some studies show that acute exposure to severe hypoxia led to an increase in CRT [24,27]. However, prolonged exposure to moderate hypoxia did not disturb CRT [24,27]. Animal studies reveal that hypoxia causes neuronal injuries in the hippocampus and cortex, leading to functional and behavioral deficits [28,29,30]. Likewise, data obtained from neuroimaging proved that intermittent hypoxia may result in a decrease in the volume of the hippocampus in humans [31].
Some previous studies performed in normoxia indicated that exercise of low or moderate intensity improves psychomotor performance [32,33,34,35,36,37], while other studies showed a significant decrease in psychomotor performance during heavy exhaustive exercise [34,37,38]. It is not known if these aforementioned effects can be modulated by a hypoxia-induced deleterious influence on the CNS. Most recent data suggest that an essential role in these phenomena is played by brain-derived neurotrophic factor (BDNF) (for review, see [39,40]).
BDNF plays a key role in the physiology of the developing and mature CNS, showing a high affinity for the TrkB receptor. Consequently, it is responsible for neurogenesis, differentiation, survival, and remodeling of neurons, and it also positively affects synaptogenesis, synaptic plasticity, and long-term potentiation [41,42,43]. The upregulation of BDNF may influence brain functions including learning and memory [44].
Several lines of evidence suggest a link between BDNF and physical activity. Both acute and chronic aerobic activity were effective for increasing peripheral BDNF concentrations [45]. An elevated level of BDNF was also seen in active sportsman compared to sedentary individuals [46,47]. Another factor that can be considered a stimulator of BDNF production within the brain is nitric oxide (NO). A role for NO in increased BDNF production in response to exercise has been recently evidenced [48,49]. Exercises of extreme intensity or duration are known to greatly elevate blood cortisol (C) [50,51], while high circulating corticosterone has been shown to suppress brain production of BDNF in rats [52]. Of importance, BDNF induces expression of the monocarboxylate transporter that enables the use of lactate as an alternative energy source [53].
There are also very limited data about the efficacy of hypoxia exposure on psychomotor performance where subjects performed exercise with low and high intensity. Some data suggest that exposure to hypoxia reduces cognitive functions [17]. Also, mechanisms of hypoxia’s effect on the CNS are still poorly understood. One possible candidate which might take part in this phenomenon is BDNF. It has been shown that cognitive impairment is noticeable in neurodegenerative diseases, which is associated with a lower serum BDNF level as compared to healthy individuals [54]. Moreover, the level of this decrease depends on the degree of cognitive impairment [54]. On the other hand, BDNF is thought to be responsible for improving cognitive function as a result of exercise effort [55]. Moreover, it has been proven that both resting and post-exercise peripheral BDNF levels correspond to its brain production [45,56] and its level is elevated in response to exercise effort [46].
Therefore, the aim of this study was to examine the impact of a single bout of exercise to volitional exhaustion during acute exposure of well-trained endurance athletes to moderate hypoxia on psychomotor performance. For this purpose, we measured a peripheral level of BDNF and CRT and NCR as indices of psychomotor performance during graded cycloergometer exercise test. Furthermore, we examined a level of selected circulating biochemical factors, such as C, NO pathway-related metabolites (nitrite, endothelin-1(ET-1), catecholamines), because they are known to affect BDNF expression/production [48,49,52,57,58,59,60] and their expression can be influenced by both exercise and hypoxia [34,48,49,50,51,61,62,63,64,65,66,67,68].
2. Results
2.1. Maximal Workload and Respiratory Variables
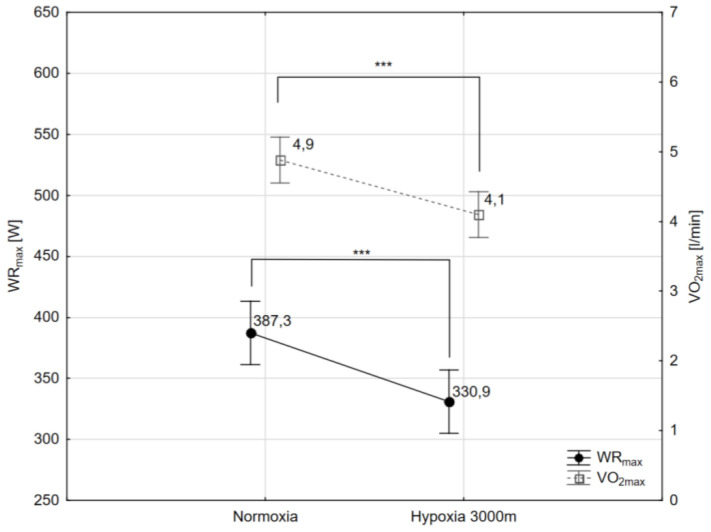
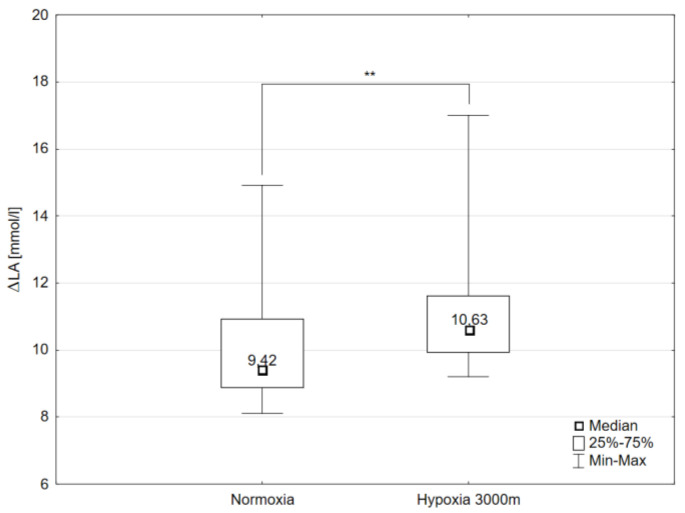
The paired sample t-test showed that maximal workload (WRmax) decreased significantly (p < 0.001) by 16.3% in hypoxia (3000 m) compared to the initial measurements in normoxia (Figure 1). The same trend of changes was observed in VO2max values. The values of VO2max decreased significantly (p < 0.001) in hypoxia compared to normoxia respectively by 14.5% (Figure 1). Additionally, there were statistically significant changes in delta values of blood lactate concentration (ΔLA) after the incremental test between normoxia and hypoxia 3000 m. The Wilcoxon test showed that ΔLA increased significantly (p < 0.01) by 6.05% despite the significant reduction in WRmax in hypoxia 3000 m compared to the measurements in normoxia (Figure 2).
Figure 1.
Maximal workload (WRmax), and maximal oxygen uptake (VO2max) during incremental test performed in different conditions. *** p < 0.001.
Figure 2.
Delta values of blood lactate concentration (ΔLA) during incremental test performed in different conditions. ** p < 0.01.
2.2. Choice Reaction Time and Number of Correct Reactions
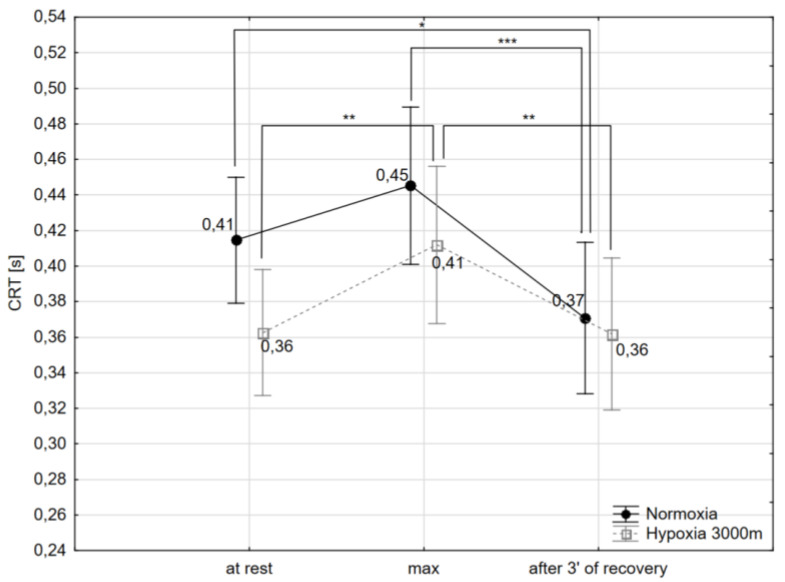
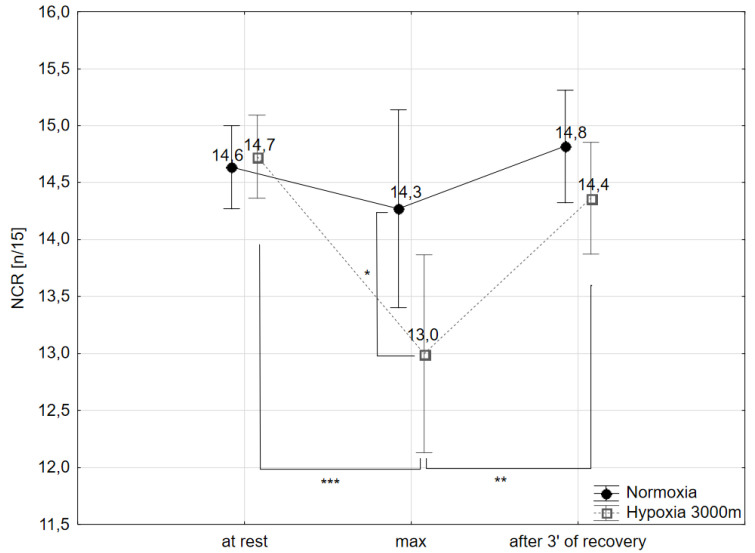
No significant interaction (condition x time of measure) effect was found on CRT but only a significant main effect of time of measurement (at rest, max and after 3 min of recovery) on CRT values (F = 21.88; p < 0.001) was observed. Additionally, there was a significant interaction (condition x time of measure) effect in the NCR (F = 3.44; p < 0.05) during the incremental test.
The post-hoc Tukey’s test showed that CRT decreased significantly (p < 0.05) by 9.7% after 3 min of recovery after the incremental test (CRTafter 3′ of recovery) compared to initial values observed at rest (CRTrest) in normoxia. Additionally, the values of CRTafter 3′ of recovery decreased significantly in normoxia (p < 0.001) and hypoxia (p < 0.01) compared to CRT during maximal workload of the incremental test (CRTmax) respectively by 17.7 and 12.2% However, CRTmax increased significantly (p < 0.01) by 13.8% compared to CRTrest in hypoxic conditions (Figure 3).
Figure 3.
Choice reaction time (CRT) at rest, during maximal effort (max) and after 3 min of the recovery period in normoxia and hypoxia (3000 m). * p < 0.05; ** p < 0.01; *** p < 0.001.
The post-hoc Tukey’s test showed that number of correct reactions (NCR) during maximal workload of the incremental test (NCRmax) decreased significantly (p < 0.05) by 9% in hypoxic conditions compared to normoxia. NCRmax values in hypoxia were significantly lower compared to NCR at rest (11.5%; p < 0.001) and NCR after 3 min of recovery after the incremental test (9.7%; p < 0.01) (Figure 4).
Figure 4.
Number of correct reactions (NCR) at rest, during maximal effort (max) and after 3 min of the recovery period in normoxia and hypoxia (3000m). * p < 0.05; ** p < 0.01; *** p < 0.001.
2.3. Brain-Derived Neurotrophic Factor and Selected Biochemical Variables
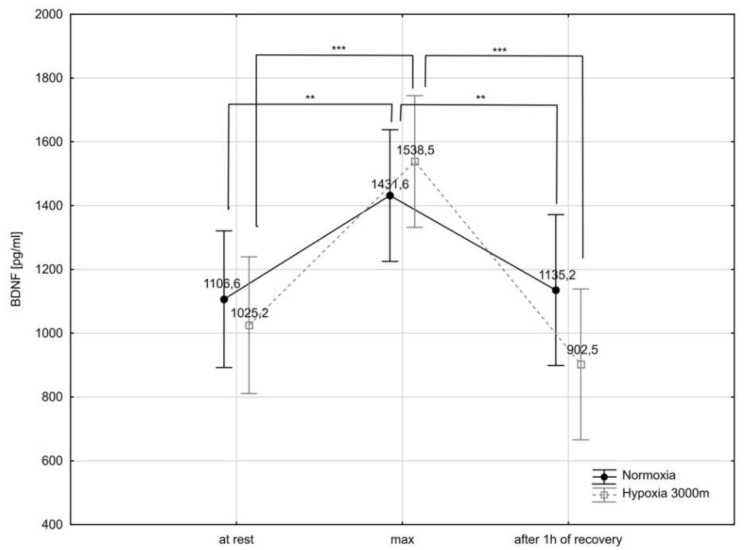
There was a significant interaction (condition x time of measure) effect in the BDNF (F = 3.66; p < 0.05) serum concentrations.
The post-hoc Tukey’s test showed that BDNF concentration increased significantly immediately after the incremental test (BDNFmax) in normoxia (by 29.3%; p < 0.01), as well as in hypoxia (by 50.0% p < 0.001). Additionally, BDNF concentration decreased significantly after a 1 h recovery period (BDNFrest) by 20.7% (p < 0.01) in normoxia and by 41.3% (p < 0.001) in hypoxia (Figure 5). There were no statistically significant differences in BDNF concentration between normoxia and hypoxia trials.
Figure 5.
Brain-derived neurotrophic factor (BDNF) serum concentration at rest, during maximal effort (max) and after 1 h recovery of the recovery period in normoxia and hypoxia (3000 m). ** p < 0.01; *** p < 0.001.
The Friedman test showed a statistically significant effect of the time of measurement on selected biochemical variables such as NO2−, C, adrenalin (A) and dopamine (DA) in both conditions (normoxia and hypoxia) (Table 1).
Table 1.
Mean values of selected biochemical variables registered in the different conditions (normoxia, hypoxia 3000 m) at rest, after incremental test (max) and after 1 h recovery period (after 1 h).
| Variables | Normoxia (N) | Hypoxia 3000 m (H3) | Significance of Differences (* p < 0.05; ** p < 0.01) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| at Rest (1) |
Max (2) |
after 1 h (3) |
at Rest (4) |
Max (5) |
after 1 h (6) |
||||||||
| x ± SD | Me | x ± SD | Me | x ± SD | Me | x ± SD | Me | x ± SD | Me | x ± SD | Me | ||
|
ET-1 (pg/mL) |
2.5 ± 0.8 | 2.5 | 2.4 ± 1.7 | 2.3 | 2.0 ± 1.1 | 1.8 | 2.3 ± 0.8 | 2.5 | 2.3 ± 1.0 | 2.61 | 2.7 ± 1.2 | 2.5 | |
|
NO2− (pg/mL) |
28.7 ± 12.1 | 23.2 | 47.6 ± 21.2 | 38.8 | 30.2 ± 12.7 | 25.6 | 33.8 ± 16.3 | 39.1 | 52.3 ± 16.3 | 49.8 | 29.5 ± 9.3 | 26.3 |
N: X2 = 13.81; p = 0.001 1–2 *; 2–3 * H3: X2 = 16.9; p = 0.002 4–5 *; 5–6 * |
|
C (pg/mL) |
8.7 ± 4.1 | 7.1 | 11.5 ± 3.8 | 11.1 | 12.4 ± 1041 | 9.8 | 7.2 ± 2.7 | 6.7 | 8.2 ± 2.48 | 8.8 | 9.4 ± 5.9 | 7.2 |
N vs. H3: 2–5 * (U = 29.0; p = 0.041) |
|
NA (pg/L) |
338.9 ± 213.4 | 337.2 | 555.6 ± 25.6 | 575.6 | 406.8 ± 28.4 | 329.3 | 334.6 ± 153.2 | 238.7 | 1109.2 ± 1045.4 | 348.5 | 575.2 ± 359 | 435.2 | |
|
A (pg/L) |
53.9 ± 29.4 | 48.8 | 479 ± 358.1 | 369 | 112.5 ± 102.3 | 117.1 | 206.9 ± 70.7 | 228.5 | 1436.1 ± 622.9 | 1384.7 | 827.4 ± 263.7 | 742.7 |
N: X2 = 16.9; p = 0.002 1–2 *; 2–3 * H3: X2 = 18.2; p = 0.001 4–5 *; 4–6 * N vs. H3: 1–4 ** (U = 1.0; p = 0.001) 2–5 ** (U = 9.0; p = 0.001) 3–6 ** (U = 0.0; p = 0.001) |
|
DA (pg/L) |
7.6 ± 10.9 | 4.3 | 8.9 ± 5.8 | 7.8 | 5.6 ± 1.4 | 5.7 | 7.3 ± 2.5 | 6.7 | 12.5 ± 2.7 | 13.2 | 12.1 ± 5.5 | 13.7 |
N: X2 = 10.1; p = 0.006 2–3 * H3: X2 = 10.4; p = 0.005 4–5 *; 4–6 * N vs. H3: 2–5 ** (U = 17.0; p = 0.008) 3–6 ** (U = 16.0; p = 0.006) |
|
5-HT (pg/L) |
155.1 ± 104.2 | 135.4 | 212.6 ± 148.1 | 150.3 | 192.1 ± 90.1 | 190.7 | 136.5 ± 67.1 | 156.7 | 205.9 ± 124.3 | 150.4 | 156.4 ± 82.1 | 148.3 | |
x—arithmetic means; SD—standard deviations; Me—median; ET-1—endothelin-1; C—cortisol; NA—noradrenaline; A—adrenalin; DA—dopamine; 5-HT—serotonin; * p < 0.05; ** p < 0.001.
The post-hoc Friedman test showed that NO2− concentration measured immediately after the incremental test was significantly higher (p < 0.05) compared to the NO2− concentration observed at rest and 1 h after the incremental test in normoxia as well as hypoxia. However, the Wilcoxon test showed that were no significant differences between normoxia and hypoxia in NO2− concentrations (Table 1).
There was no significant effect of the time of measurement (at rest, max, 1 h after test) on C concentrations in both conditions. However, there was a significant effect of conditions (normoxia vs. hypoxia) on C concentration. The Wilcoxon test showed that C concentration measured immediately after the incremental test (Cmax) was significantly higher (p < 0.05) by 20.7% in normoxic conditions compared to hypoxia (Table 1).
Moreover, the post-hoc Friedman test showed that A concentration measured immediately after the incremental test (Amax) was significantly higher (p < 0.05) compared to the A concentration observed at rest (Arest; by 656.1%) and 1 h after the incremental test (A1h after; by 215,1%) in normoxia. However, in hypoxia, Amax and A1h after were significantly higher (p = 0.001) compared to Arest respectively by 505.9% and 86.4%. The Wilcoxon test showed that Arest, Amax and A1h after in hypoxia were significantly higher (p = 0.001) compared to these values in normoxia, respectively by 368.2%, 275% and 534.2% (Table 1).
The post-hoc Friedman test showed that DA concentration measured 1 h after the incremental test (DA1h after) significantly decreased (p < 0.05) by 26.9% compared to the DA concentration measured immediately after the incremental test (DAmax) in normoxia. However, in hypoxia, DAmax and DA1h after significantly increased (p < 0.05) compared to the DA concentration at rest, respectively by 97% and 104.5%. Additionally, the Wilcoxon test showed that DAmax and DA1h after in hypoxia were significantly higher (p < 0.01) compared to these values in normoxia, respectively by 69.2% and 140.3% (Table 1).
3. Discussion
Physical training is planned to improve physical fitness and performance, which confers numerous positive effects on the whole body function [69]. A pivotal role in regulation of these changes is assigned to the brain, particularly the prefrontal cortex, which takes part in regulation of many executive functions to prepare humans for situations demanding high levels of working memory, attention and cognitive flexibility [70]. On the other hand, altitude training, which nowadays has become a standard training protocol in many sports to increase exercise capacity [71,72,73], causes cognitive frailty [74]. The cognitive decline is most intensely manifested after acute hypoxic exposure and is more profound in athletes than non-trained individuals [75]. Therefore, the primary purpose of this study was to examine the impact of a single bout of exercise to volitional exhaustion during acute exposure well endurance-trained athletes to moderate hypoxia on psychomotor performance. We also measured serum BDNF, some selected hormones (C and catecholamines), the NO pathway metabolites (nitrite), as well as ET-1, as a possible candidate that may be involved in modulation of this phenomenon. We used measurements of CRT and NCR as indicators of psychomotor skills because these variables were demonstrated to be a dependable measure of cognition in different experimental approaches [22].
Results from this investigation revealed that exercise to volitional exhaustion extended CRT in both experimental conditions but only the impact of hypoxic conditions on this variable was statistically significant. A similar alteration, but with statistically significant changes in both cases, was seen in NCR (Figure 4). Additionally, NCR was significantly increased in response to exercise to volitional exhaustion performed in hypoxia as compared with normoxia. These results are in agreement with previous data reported by others which showed cognitive impairment of trained subjects at high altitude [75] and additionally suggested that NCR which specified response accuracy was a more sensitive tool for estimating cognitive state than CRT. Interestingly, the aforementioned exercise-induced effect was transient in both experimental conditions and studied variables returned to basal values within a few minutes after cessation of exercise.
Increasingly more evidence supports the action of BDNF as an underlying factor that elicits exercise/training-induced beneficial changes CNS [76,77,78]. Moreover, there are also suggestions that the negative impact on cognitive function in hypoxia can be at least partially explained by the simultaneous decrease of BDNF [79,80]. Studies with animal models have shown that this neurotrophin is produced, among other tissues, in brain by motor neurons [81] and intermittent hypoxia increases BDNF levels in neurons of the primary motor cortex [82]. Also, central BDNF cannot be measured in living humans. It has been suggested that the brain is the main source of the increased BDNF in circulation [83,84]. If so, and considering the fact that in our study similar circulating levels of BDNF were seen in both experimental groups but cognitive performance was suppressed in hypoxia, one could conclude that acute elevation of BDNF did not compensate for hypoxia-induced cognition impairment. Previous evidence suggests that BDNF plays a key role in memory and learning [85] and is a vital regulator of neuronal function and plasticity [86,87]. However, these aforementioned effects appeared almost selectively in response to a repetitive or chronic stimulus or in studies in vitro. Results of the current research are in line with reports of some studies using cognitive tasks such as executive function or attention which were unrelated to changes in BDNF after acute exercise [88,89,90]. One reason which at least theoretically might be considered for the acute action of BDNF is its involvement in synaptic transmission [91]. The results from animal studies indicate that during hypoxia neurons can within minutes alter synaptic transmission [92,93]. Support for a link between exposure to hypoxia and run-down of synaptic transmission has been widely documented in in vitro studies [94,95] and in rats subjected to severe (6100 m) hypoxia [96]. The mechanism by which severe hypoxia induced cognitive impairment was accompanied by a decrease in Acetylcholine (Ach) level and increase in Acetylcholinesterase (AChE) in the cortex [96].
Apart from BDNF, C has been identified as a possible endocrinological mediator of exercise which may modulate brain function [97,98]. Both hypoxia and exercise stimulate the gland cortex to release C. While it is well recognized that elevation of C has been observed in response to acute exercise of higher than moderate intensities, data from hypoxic studies are less consistent. In response to this environmental stimulus, increases or lack of changes have been reported. In our study, when maximal effort was performed in moderate hypoxia the C level was significantly lower compared to normoxia. As this hormone impairs the prefrontal cortex [99,100], the region of the brain that controls more of our cognitive function, one can argue that its deteriorative impact on psychomotor performance, if any, was negligible. However, there is a study showing similar exercised increased plasma C in normoxia and acute hypobaric hypoxia (3000 m altitude) [101]. This discrepancy may be the result of different research designs between aforementioned and our studies (normobaric vs. hypobaric hypoxia as well as cyclists vs. cross-country skiers and ice hockey players).
Previous studies demonstrated that physically active persons have shorter CRT than sedentary ones [102] and the regular U-shaped curve was obtained in athletes when CRT values were plotted against A and noradrenaline (NA) during graded incremental exercise to volitional exhaustion [34,62]. The latter results indicate that CRT exceeds the resting values at exercise loads close to maximal, and catecholamines may play a role in this phenomenon. Although most studies agree that catecholamine levels increase at rest and exercise at high altitude, brief or moderate hypoxia does not always elevate their levels [103,104], and this is especially true for NA [105]. The present finding reflects this phenomenon in the case of NA and serotonin (5-HT) while indicating elevated A as a potential player in cognitive control in our experimental paradigm. In favor of such an assumption is the significantly elevated A level during maximal effort in hypoxia with simultaneous statistically significant extension of CRT. Previous studies on patients with psychological trauma indicate that A and DA are involved in the activation of the prefrontal cortex [106] and similarly stress and aggressive behavior were shown to increase turnover of both A and DA in this area in rodents [107]. Acute hypoxia is considered as a systemic stress factor and was also seen to reduce cognitive function in rats, which was associated with DA signaling in the prefrontal cortex [63]. This finding is additionally supported by increased errors in the cognitive test, which were associated with reduced DA signaling in the prefrontal cortex [108]. However, the lack of significant differences in DA between our investigated groups probably excludes DA participation in the modulation of cognitive function in our subjects. It is worth noting that there is also a study [66] showing that during a short episode of anoxia, an increase in A level can have a protective effect against its disruptive effects. In the present study, this effect did not occur in response to exercise either in normoxia or in moderate hypoxia despite an elevated level of A in both cases. Collectively, the aforementioned results lead to the conclusion that A probably reveals biphasic action on cognitive function in hypoxic conditions, i.e., a positive effect during short-term and negative after prolonged actions.
It is well established that hypoxia releases a diffusible vasoconstrictor and vasodilator substance and this process can affect blood flow to the brain. Some evidence supports the view that an increase of blood flow to the brain may induce cognitive improvement by delivering elevated oxygenated hemoglobin [109]. In accordance with the above knowledge, we have measured in this research ET-1 and NO metabolites as the most potent representatives of endothelial released vasoconstrictors [110] and vasodilators [111], respectively. In humans, no changes in ET-1 response to maximal exercise in acute hypobaric hypoxia (3000) were noted as compared to normoxia [101]. In our study, both exercise and exercise in hypoxia also provoked no changes in ET-1, confirming occurrence of the above-mentioned effect in normobaric hypoxia, and suggesting that ET-1 had no important influence on blood low regulation in the acute response to moderate hypoxia.
Nitric oxide is mainly generated in the body by endothelial cells, but it is also produced in the CNS, where it is closely involved in neurotransmission and modulation of neuron metabolism [112]. A previous study conducted with diabetic patients indicated that increased bioavailability of NO was a factor that might enhance cognitive function [113]. However, the latest data questioned this possibility when psychomotor performance was tested in hypoxic conditions [114]. Our research conducted in a normobaric hypoxic chamber revealed an inconsiderable rise in serum NO2− levels both in basal and exercise conditions as compared to normoxia. Since simultaneously cognitive performance was blunted it implied that NO production under these circumstances was likely too low to affect cognitive functions or NO was not a crucial player in this phenomenon. These assumptions are partially in line with recent findings which do not support a beneficial effect of NO3− supplementation on cognitive function in sedentary males at moderate and very high simulated altitude [115]. However, it is clear that if during a profound reduction of absolute work under hypoxia the NO2− level was higher than in normoxia then an additional exercise-independent system was responsible for NO2− formation. This pathway is activated in parallel during exercise under hypoxic conditions, yet it needs to be identified.
Physical exercise involves markedly increased activity of many brain structures [116]. The metabolites produced in the muscles, which can diffuse into the CNS and can be utilized as a fuel to sustain increased energy requirements, may participate in this process [117]. Such possibility underscores the importance of the muscle produced lactate (LA) during exercise which can be transferred to neurons via monocarboxylate carriers and used in addition to LA delivered via astrocytes-neurons lactate shuttle [118] as energy fuel during neuronal activation as well. On the other hand, LA was recognized as a signaling molecule in the brain [119]. Among others, it can bind a receptor of the G protein coupled receptor family (GPRs) [120] and thereby cause a decrease of cyclic adenosine monophosphate (cAMP) level. This raises the possibility of interaction between LA and A in metabolism regulation on a subcellular level. If true, this phenomenon should have been more strongly connected with hypoxic conditions because A level during maximal effort in hypoxia was significantly elevated while lowering LA (as compared to controls). This was accompanied with simultaneous statistically significant extension of CRT.
4. Materials and Methods
4.1. Participants
Eleven cyclists (20 ± 1.4 years of age) were recruited for the study as volunteers. All participants had current valid medical examinations and showed no contraindications that would exclude them from the study. They declared that for at least one month before testing they did not take either medications or dietary supplements. Written informed consent was obtained prior to study commencement.
The basic anthropometric data of the volunteers (body height—BH, body mass—BM, fat content—FAT) are presented in Table 2. The experimental procedures involved, and the related risks were explained to all the participants verbally, informed written consent was taken from each participant and they could withdraw at any time of the study. The research project was conducted according to the Helsinki Declaration and was approved (no. 5/2013, approval date: 26.06.2013) by the Ethics Committee for Scientific Research at the Jerzy Kukuczka Academy of Physical Education in Katowice, Poland.
Table 2.
Mean values of body height (BH), body mass (BM) and fat content (FAT) of study participants (n = 11).
| BH (cm) | BM (kg) | FAT (%) |
|---|---|---|
| 180.5 ± 6.5 | 70.3 ± 6.8 | 9.4 ± 3.1 |
The subjects participating in the study were tested on two randomized occasions separated by 5 days duration in normoxic and hypoxic conditions. Participants were allocated to conditions using a computer-generated randomized list [121].
Hypoxic conditions were created using a normobaric hypoxia chamber (LOSA HYP/HYOP-2/3NU system, LOWOXYGEN SYSTEMS, Berlin, Germany) that is in use in the Laboratory of Hypoxia of the Jerzy Kukuczka Academy of Physical Education and the selected hypoxia was an equivalent of 3000 m altitude (FiO2 = 14.7%).
On each occasion, the participants were subject to two graded ergocycle tests each performed under normobaric normoxic and normobaric hypoxic conditions (3000 m asl). Before each test, body mass and body composition of each participant was determined using a model Inbody 720 (Biospace Co., Tokio, Japan) body composition analyzer using electrical impedance measurements.
4.2. Ergocycle Graded Exercise Test
The ergocycle tests were performed on a model Excalibur Sport (Lode BV, Groningen Netherlands) cycloergometer, beginning at a work load of 40 W, which was increased by 40 W every 3 min until volitional exhaustion. If a subject terminated the test before completing a given workload, then the maximum workload was calculated from the formula WRmax = WRk + (t/T × WRp) [122], where WRk—previous workload, t—exercise duration with the work-load until premature failure, T—duration of each workload, WRp—the amount of workload by which exercise intensity increased during the test.
During the tests, heart rate (HR), minute ventilation (VE), breathing frequency (BF), oxygen uptake (VO2) and carbon dioxide content in expired air (VCO2) were recorded in the subjects with the MetaMax 3B gas analyzer (Cortex, Leipzig, Germany). Fingertip capillary blood samples for the assessment of LA concentration (Biosen C-line Clinic, EKF-diagnostic GmbH, Barleben, Germany) were drawn at rest and at the end of each step of the test, as well as during the 3rd, 6th, 9th, and 12th minute of recovery. Additionally, capillary rest and post-exercise blood samples were used to determine acid-base equilibrium and oxygen saturation of hemoglobin (Rapid Lab 248, Siemens/Bayer Diagnostics, Erlangen, Germany).
4.3. Psychomotor Performance Determination
The choice reaction time and NCR were selected as indices of psychomotor performance as described previously [26]. Briefly, the CRT console was mounted on the wall in front of the ergometer at eye level, 1.5 m away from the subject. The test included 15 positive (red light or a sound) and 15 negative (green and yellow lights) stimuli applied in a randomized order in 1 to 4 s intervals. The subjects were asked to press and then to release, as quickly as possible, the button of the switch devised kept in the right hand in response to the red light, the button in the left hand in response to the sound and not react to the negative stimuli. The total time for each CRT was 107 s. The stimuli and the subjects’ responses were recorded using the reaction time measuring device (MRK 432, ZEAM, Zabrze, Poland). The reaction time was determined to the nearest 0.01 s. The results are presented at the mean reaction time of 15 responses to positive stimuli. The subjects were familiarized with the procedure a week before the study by practicing the task both at rest and during cycling.
4.4. Venous Blood
The participants were cannulated into the antecubital vein on the day of ergocycle testing 15 min prior to the breakfast. Venous blood samples (2 samples per time point) were collected 10 min later, then immediately after cessation of each ergocycle test, and 1 h after each ergocycle test. One sample of each pair was taken using ethylenediaminetetraacetic (EDTA) tubes (for morphology analysis); the other one was drawn using no anti-coagulant tubes and processed for serum for the other biochemical assays (BDNF, ET-1, C, catecholamines). After 30 min, blood samples were centrifuged at 1500× g for 15 min. The sera obtained were stored at −80 °C until analyzed.
4.5. Determination of Brain-Derived Neurotrophic Factor, Cortisol and Endothelin-1 Concentrations
Serum BDNF, C, and ET-1 concentrations were determined using a commercially available Quantikine ELISA kit (R&D Systems, Minneapolis, MN, USA) according to the procedure supplied by the manufacturer. This method allows measurement of BDNF, C, and ET-1 in the range of 0.372–4000 pg/mL, 0.030–100 ng/mL, and 0.031–50 ng/mL respectively. The intra-assay coefficient of variance was <4.0%, <8%, <4%, respectively. To quantify the level, a standard curve was performed using a standard solution.
4.6. Determination of Catecholamines by HPLC Method
Adrenalin, NA, DA and 5-HT were assayed in the serum using high performance liquid chromatography (HPLC, Gynkotek, Copenhagen, Denmark) with electrochemical detection using Coulochem III model 520 (ESSA, Copenhagen, Denmark).
Serum samples were mixed with 0.1 M perchloric acid containing 22.5 ng/mL ascorbic acid (ASC, Sigma-Aldrich, St. Louis, MO, USA). After centrifugation at 15,000 g, 10 min, at 4 °C, supernatant was filtered through a nylon syringe filter (Millipore, 0.22 μm, Merck KGaA, Darmstadt, Germany). Samples of 20 μL filtrate were injected into a high performance liquid chromatography system (Gynkotek, Copenhagen, Denmark) equipped with a Hypersil Gold (15 cm × 4.6 mm) column (Thermo Electron Corporation, Kleinostheim, Germany). The samples were eluted by a mobile phase made of 107 mM of Na2HPO4 × 2H2O, 107 mM citric acid, 0.3 mM octane-1 sulfonic acid sodium salt (OSA), 0.2 μM of EDTA, pH, 4.6, 1.5% methanol and 1.5% acetonitrile at a flow rate of 0.8 mL/min. The column temperature was set at 25 °C. Peaks were detected by electrochemical detection (Coulochem III, ESSA, Copenhagen, Denmark) at potentials of E1 = −50 mV and E2 = +400 mV. Data were collected and analyzed using Chromeleon software run on a PC (Gynkotek, Copenhagen, Denmark). DA and 5-HT contents in the sample were calculated by extrapolating the peak area from a standard cure.
4.7. Determination of Nitrite Concentration
Serum nitrite concentration were determined using a commercially colorimetric kit (R&D Systems, Minneapolis, MN, USA) according to the procedure supplied by the manufacturer.
4.8. Statistical Analysis
The results of the study were analyzed using Statistica 13.0 software (StatSoft, Cracow, Poland). The results are presented as arithmetic means (x) and standard deviations (SD). The statistical significance was set at p < 0.05. Prior to all statistical analyses, the normality of the distribution of variables was verified using the Shapiro-Wilk test. The paired sample t-test was used to determine the significance of differences in VO2max, WRmax between the two trials in different conditions. Furthermore, due to the lack of normality of distribution, the Wilcoxon test was used to determine the significance of differences in delta values in lactate concentrations (Delta LA) between the trials. The intergroup differences between the research trials (condition × time of measurement) were determined using the two-way ANOVA for repeated measures. When significant differences were found, the post hoc Tukey’s test was used. If the normality assumption was violated, the Friedman test was applied, whereas when significant differences were found, we used the post hoc Friedman test. The comparisons of repeated measurements (normoxia vs. hypoxia) were assessed by the Wilcoxon signed-rank test.
5. Conclusions
In conclusion, the results of this study showed that maximal physical exercise, regardless of whether it is performed under normoxia or mild normobaric hypoxia (equivalent of 3000 m altitude) caused a similar increase in BDNF concentration in the blood of well-trained athletes. Despite the fact that BDNF has been known to possess a protective effect on the brain, an elevated BDNF level did not protect our participants from cognitive impairment due to acute exposure to hypoxia, because indices of this variable, i.e., CRT and NCR, were worse in hypoxic conditions. All examined potential circulating factors that are known to affect BDNF expression/production (C, nitrite, ET-1, catecholamines, LA) most likely did not affect psychomotor functions in our experimental paradigm.
Abbreviations
| BDNF | brain-derived neurotrophic factor |
| ET-1 | endothelin-1 |
| 5-HT | serotonin |
| CRT | choice reaction time |
| NCR | number of correct reactions |
| DA | dopamine |
| LA | lactate |
| NA | noradrenaline |
| C | cortisol |
| A | adrenalin |
Author Contributions
Conceptualization Z.P., M.C. (Miłosz Czuba), and J.L.; methodology, Z.P., M.C. (Miłosz Czuba), and J.L.; formal analysis, K.P. and M.C. (Miłosz Czuba); investigation, Z.P., M.C. (Małgorzata Chalimoniuk) and M.C. (Miłosz Czuba); data curation, M.C. (Małgorzata Chalimoniuk) and K.P.; writing—original draft preparation, Z.P., M.C. (Małgorzata Chalimoniuk), K.P., M.C. (Miłosz Czuba), J.L.; writing—review and editing, Z.P., M.C. (Miłosz Czuba) and J.L.; visualization, Z.P. and K.P.; supervision, M.C. (Małgorzata Chalimoniuk) and J.L.; funding acquisition, J.L. All authors have read and agreed to the published version of the manuscript.
Funding
The research was supported by the grant No. 2013/09/B/NZ7/00726 from the National Science Centre of Poland.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Bendahan D., Badier M., Jammes Y., Confort-Gouny S., Salvan A.M., Guilot C., Conzzone P. Metabolic and myoelectrical effects of acute hypoxaemia during isometric contraction of forearm muscles in humans: A combined 31P-magnetic resonance spectroscopy-surface electromyogram (MRS-SEMG) study. Clin. Sci. 1998;94:279–286. doi: 10.1042/cs0940279. [DOI] [PubMed] [Google Scholar]
- 2.Calbet J.A., De Paz J.A., Garatachea N., Cabeza de Vaca S., Chavarren J. Anaerobic energy provision does not limit Wingate exercise performance in endurance-trained cyclists. J. Appl. Physiol. 2003;94:668–676. doi: 10.1152/japplphysiol.00128.2002. [DOI] [PubMed] [Google Scholar]
- 3.Perrey S. Decrease in cerebral oxygenation influences central motor output in humans. Acta Physiol. 2009;196:279–281. doi: 10.1111/j.1748-1716.2009.02007.x. [DOI] [PubMed] [Google Scholar]
- 4.Amann M., Eldridge M.W., Lovering A.T., Stickland M.K., Pegelow D.F., Dempsey J.A. Arterial oxygenation influences central motor output and exercise performance via effects on peripheral locomotor muscle fatigue in humans. J. Physiol. 2006;575:937–952. doi: 10.1113/jphysiol.2006.113936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peltonen J.E., Rusko H.K., Rantamaki J., Sweins K., Nittymaki S., Vitasalo J.T. Effects of oxygen fraction in inspired air on force production and electromyogram activity during ergometer rowing. Eur. J. Appl. Physiol. 1997;76:495–503. doi: 10.1007/s004210050281. [DOI] [PubMed] [Google Scholar]
- 6.Dempsey J.A., Wagner P.D. Exercise-induced arterial hypoxemia. J. Appl. Physiol. 1999;87:1997–2006. doi: 10.1152/jappl.1999.87.6.1997. [DOI] [PubMed] [Google Scholar]
- 7.Adams R.P., Welch H.G. Oxygen uptake, acid-base status, and performance with varied inspired oxygen fractions. J. Appl. Physiol. 1980;49:863–868. doi: 10.1152/jappl.1980.49.5.863. [DOI] [PubMed] [Google Scholar]
- 8.Hogan M.C., Richardson R.S., Haseler L.J. Human muscle performance and PCr hydrolysis with varied inspired oxygen fraction: A 31P-MRS study. J. Appl. Physiol. 1999;86:1367–1373. doi: 10.1152/jappl.1999.86.4.1367. [DOI] [PubMed] [Google Scholar]
- 9.Peltonen J.E., Tikkanen H.O., Ritola J.J., Ahotupa M., Rusko H.K. Oxygen uptake response during maximal cycling in hyperoxia, normoxia and hypoxia. Aviat. Space Environ. Med. 2001;72:904–911. [PubMed] [Google Scholar]
- 10.Benoit H., Busso T., Castells J., Geyssant A., Denis C. Decrease in peak heart rate with acute hypoxia in relation to sea level VO(2max) Eur. J. Appl. Physiol. 2003;90:514–519. doi: 10.1007/s00421-003-0899-y. [DOI] [PubMed] [Google Scholar]
- 11.Lundby C., Moeller P., Kanstrup I.L., Olsen N.V. Heart rate response to hypoxic exercise: Role of dopamine D2-receptors and effect of oxygen supplementation. Clin. Sci. 2001;101:377–383. doi: 10.1042/cs1010377. [DOI] [PubMed] [Google Scholar]
- 12.Kayser B., Narici M., Binzoni T., Grassi B., Cerretelli P. Fatigue and exhaustion in chronic hypobaric hypoxia: Influence of exercising muscle mass. Am. J. Physiol. 1994;76:634–640. doi: 10.1152/jappl.1994.76.2.634. [DOI] [PubMed] [Google Scholar]
- 13.Boushel R., Calbet J.A., Rådegran G., Sondergaard H., Wagner P.D., Saltin B. Parasympathetic neural activity accounts for the lowering of exercise heart rate at high altitude. Circulation. 2001;104:1785–1791. doi: 10.1161/hc4001.097040. [DOI] [PubMed] [Google Scholar]
- 14.Amann M., Romer L.M., Subudhi A.W., Pegelow D.F., Dempsey J.A. Severity of arterial hypoxaemia affects the relative contributions of pripheral muscle fatigue to exercise performance in healthy humans. J. Physiol. 2007;581:389–403. doi: 10.1113/jphysiol.2007.129700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pedersen B.K., Febbraio M.A. Muscle as an endocrine organ: Focus on muscle-derived interleukin-6. Phys. Rev. 2008;88:1379–1406. doi: 10.1152/physrev.90100.2007. [DOI] [PubMed] [Google Scholar]
- 16.Davis J.M., Bailey S.P. Possible mechanisms of central nervous system fatigue during exercise. Med. Sci. Sports Exerc. 1997;29:45–57. doi: 10.1097/00005768-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Lieberman P., Protopapas A., Reed E., Youngs J.W., Kankim B.G. Cognitive defects at altitude. Nature. 1994;372:325. doi: 10.1038/372325a0. [DOI] [PubMed] [Google Scholar]
- 18.Blogg S.L., Gennser M. Cerebral blood flow velocity and psychomotor performance during acute hypoxia. Aviat. Space Environ. Med. 2006;77:107–113. [PubMed] [Google Scholar]
- 19.Temme L.A., Still D.L., Acromite M.T. Hypoxia and flight performance of military instructor pilots in a flight simulator. Aviat. Space Environ. Med. 2010;81:654–659. doi: 10.3357/ASEM.2690.2010. [DOI] [PubMed] [Google Scholar]
- 20.McMorris T., Hale B.H., Barwood M., Costello J., Corbett J. Effect of acute hypoxia on cognition: A systematic review and meta-regression analysis. Neurosci. A Biobehav. Rev. 2017;74:225–232. doi: 10.1016/j.neubiorev.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 21.Lal C., Strange C., Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest. 2012;141:1601–1610. doi: 10.1378/chest.11-2214. [DOI] [PubMed] [Google Scholar]
- 22.Jensen A.R. Clocking the Mind: Mental Chronometry and Individual Differences. 1st ed. Elsevier Science; London, UK: 2006. pp. 43–54. [Google Scholar]
- 23.Salthouse T.A., Hedden T. Interpreting reaction time measures in between-group comparisons. J. Clin. Exp. Neuropsychol. 2002;24:858–872. doi: 10.1076/jcen.24.7.858.8392. [DOI] [PubMed] [Google Scholar]
- 24.Caldwell H.G., Coombs G.B., Tymko M.M., Nowak-Fluck D., Ainslie P.N. Severity-dependent influence of isocapnic hypoxia on reaction time is independent of neurovascular coupling. Physiol. Behav. 2018;1:262–269. doi: 10.1016/j.physbeh.2018.02.035. [DOI] [PubMed] [Google Scholar]
- 25.De Aquino-Lemos V., Santos R.V.T., Antunes H.K.M., Lira F.S., Bittar I.G.L., Caris L.V., Tufik S., de Mello M.T. Acute physical exercise under hypoxia improves sleep, mood and reaction time. Physiol. Behav. 2016;154:90–99. doi: 10.1016/j.physbeh.2015.10.028. [DOI] [PubMed] [Google Scholar]
- 26.Ochi G., Kanazawa J., Hyodo K., Suwabe K., Shimizu T., Fukuie T., Byun K., Soya H. Hypoxia-induced lowered executive function depends on arterial oxygen desaturation. J. Physiol. Sci. 2018;68:847–853. doi: 10.1007/s12576-018-0603-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pramsohler S., Wimmer S., Kopp M., Gatterer H., Faulhaber M., Burtscher M., Netzer N.C. Normobaric hypoxia overnight impairs cognitive reaction time. BMC Neurosi. 2017;18:43. doi: 10.1186/s12868-017-0362-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hartman R.E., Lee J.M., Zipfel G.J., Wozniak D.F. Characterizing learning deficits and hippocampal neuron loss following transient global cerebral ischemia in rats. Brain Res. 2005;1043:48–56. doi: 10.1016/j.brainres.2005.02.030. [DOI] [PubMed] [Google Scholar]
- 29.Maiti P., Singh S.B., Muthuraju S., Veleri S., Ilavazhagen G. Hypobaric hypoxia damages the hippocampal pyramidal neurons in the rat brain. Brain Res. 2007;1175:1–9. doi: 10.1016/j.brainres.2007.06.106. [DOI] [PubMed] [Google Scholar]
- 30.Hota S.K., Barhwal K., Singh S.B., Ilavazhagan G. Chronic hypobaric hypoxia induced apoptosis in CA1 region of hippocampus: A possible role of NMDAR mediated p75NTR upregulation. Exp. Neurol. 2008;212:5–13. doi: 10.1016/j.expneurol.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 31.Gale S.D., Hopkins R.O. Effects of hypoxia on the brain: Neuroimaging and neuropsychological findings following carbon monoxide poisoning and obstructive sleep apnea. J. Int. Neuropsychol. Soc. 2004;10:60–71. doi: 10.1017/S1355617704101082. [DOI] [PubMed] [Google Scholar]
- 32.Levitt S., Gutin B. Multiple-choice reaction time and movement time during physical exertion. Res. Q. 1971;42:406–410. doi: 10.1080/10671188.1971.10615088. [DOI] [PubMed] [Google Scholar]
- 33.Sjöberg H. Relations between heart rate, reaction speed and subjective effort at different work loads on a bicycle ergometer. J. Hum. Stress. 1975;1:21–27. doi: 10.1080/0097840X.1975.9939549. [DOI] [PubMed] [Google Scholar]
- 34.Chmura J., Nazar K., Kaciuba-Uscilko H. Choice reaction time during graded exercise in relation to blood lactate and plasma catecholamine thresholds. Int. J. Sports Med. 1994;15:172–176. doi: 10.1055/s-2007-1021042. [DOI] [PubMed] [Google Scholar]
- 35.Chmura J., Krysztofiak H., Ziemba A.W., Nazar K., Kaciuba-Uscilko H. Psychomotor performance during prolonged exercise above and below lactate threshold. Eur. J. Appl. Physiol. 1998;77:77–80. doi: 10.1007/s004210050303. [DOI] [PubMed] [Google Scholar]
- 36.Travlos A.K., Marisi D.Q. Information processing and concentration as a function of fitness level and exercise-induced activation to exhaustion. Percept. Mot. Skills. 1995;80:15–26. doi: 10.2466/pms.1995.80.1.15. [DOI] [PubMed] [Google Scholar]
- 37.Kruk B., Chmura J., Krzeminski K., Ziemba A.W., Nazar K., Pekkarinen H., Kaciuba-Uscilko H. Influence of caffeine, cold and exercise on multiple choice reaction time. Psychopharmacology. 2001;157:197–201. doi: 10.1007/s002130100787. [DOI] [PubMed] [Google Scholar]
- 38.Bender V.L., McGlynn L. The effect of various levels of strenuous to exhausting exercise on reaction time. Eur. J. Appl. Physiol. 1976;35:95–110. doi: 10.1007/BF02333799. [DOI] [PubMed] [Google Scholar]
- 39.Rothman S.M., Griffioen K.J., Wan R., Mattson M.P. Brain-derived neurotrophic factor as a regulator of systemic and brain energy metabolism and cardiovascular health. Ann. N. Y. Acad. Sci. 2012;1264:49–63. doi: 10.1111/j.1749-6632.2012.06525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang T., Larsen K.T., Ried-Larsen M., Møller N.C., Andersen L.B. The effects of physical activity and exercise on brain-derived neurotrophic factor in healthy humans: A review. Scand. J. Med. Sci. Sports. 2014;24:1–10. doi: 10.1111/sms.12069. [DOI] [PubMed] [Google Scholar]
- 41.Hohn A., Leibrock J., Bailey K., Barde Y.A. Identyfication and characterization of a novel member of the nerve growth factor/brain-derived neurotrophic factor family. Nature. 1990;344:339–341. doi: 10.1038/344339a0. [DOI] [PubMed] [Google Scholar]
- 42.Binder D.K., Scharfman H.E. Brain-derived neurotrophic factor. Growth Factors. 2004;22:123–131. doi: 10.1080/08977190410001723308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Małczyńska P., Piotrowicz Z., Drabarek D., Langfort J., Chalimoniuk M. Rola mózgowego czynnika neurotroficznego (BDNF) w procesach neurodegeneracji oraz w mechanizmach neuroregeneracji wywołanej wzmożoną aktywnością fizyczną. Postępy Biochem. 2019;65:2–8. doi: 10.18388/pb.2019_251. [DOI] [PubMed] [Google Scholar]
- 44.Tyler W.J., Alonso M., Bramham C.R., Pozzo-Miller L.D. From acquisition to consolidation: On the role of brain-derived neurotrophic factor signaling in hippocampal-dependent learning. Learn. Mem. 2002;9:224–237. doi: 10.1101/lm.51202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Knaepen K., Goekint M., Heyman E.M., Meeusen R. Neuroplasticity-exercise-induced response of peripheral brain-derived neurotrophic factor: A systematic review of experimental studies in human subjects. Sports Med. 2010;40:765–801. doi: 10.2165/11534530-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 46.Zoladz J.A., Pilc A., Majerczak J., Grandys M., Zapart-Bukowska J., Duda K. Endurance training increases plasma brain-derived neurotrophic factor concentration in young healthy men. J. Physiol. Pharmacol. 2008;59:119–132. [PubMed] [Google Scholar]
- 47.Correia P.R., Scorza F.A., Gomes da Silva S., Pansani A., Toscano-Silva M., de Almeida A.C., Arida R.M. Increased basal plasma brain-derived neurotrophic factor levels in sprint runners. Neurosci. Bull. 2011;27:325–329. doi: 10.1007/s12264-011-1531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cheng A., Wang S., Cai J., Rao M.S., Mattson M.P. Nitric oxide acts in a positive feedback loop with BDNF to regulate neural progenitor cell proliferation and differentiation in the mammalian brain. Dev. Biol. 2003;258:319–333. doi: 10.1016/S0012-1606(03)00120-9. [DOI] [PubMed] [Google Scholar]
- 49.Chen M.J., Ivy A.S., Russo-Neustadt A.A. Nitric oxide synthesis is required for exercise-induced increases in hippocampal BDNF and phosphatidylinositol 3′ kinase expression. Brain Res. Bull. 2006;68:257–268. doi: 10.1016/j.brainresbull.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 50.Zajac A., Poprzecki S., Zebrowska A., Chalimoniuk M., Langfort J. Arginine and ornithine supplementation increases growth hormone and insulin-like growth factor-1 serum levels after heavy-resistance exercise in strength-trained athletes. J. Strength Cond. Res. 2010;24:1082–1090. doi: 10.1519/JSC.0b013e3181d321ff. [DOI] [PubMed] [Google Scholar]
- 51.Dessypris A., Wägar G., Fyhrquist F., Mäkinen T., Welin M.G., Lamberg B.A. Marathon run: Effects on blood cortisol-ACTH, iodothyronines-TSH and vasopressin. Acta Endocrinol. (Copenh.) 1980;95:151–157. doi: 10.1530/acta.0.0950151. [DOI] [PubMed] [Google Scholar]
- 52.Yau S.Y., Lau B.W., Zhang E.D., Lee J.C., Li A., Lee T.M., Ching Y.P., Xu A.M., So K.F. Effects of voluntary running on plasma levels of neurotrophins, hippocampal cell proliferation and learning and memory in stressed rats. Neuroscience. 2012;222:289–301. doi: 10.1016/j.neuroscience.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 53.Robinet C., Pellerin L. Brain-derived neurotrophic factor enhances the expression of the monocarboxylate transporter 2 through translational activation in mouse cultured cortical neurons. J. Cereb. Blood Flow Metab. 2010;30:286–298. doi: 10.1038/jcbfm.2009.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ng T.K.S., Ho C.S.H., Tam W.W.S., Kua E.H., Ho R.C. Decreased Serum Brain-Derived Neurotrophic Factor (BDNF) Levels in Patients with Alzheimer’s Disease (AD): A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2019;20:257. doi: 10.3390/ijms20020257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu P.Z., Nusslock R. Exercise-Mediated Neurogenesis in the Hippocampus via BDNF. Front. Neurosci. 2018;12:52. doi: 10.3389/fnins.2018.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pan W., Banks W.A., Fasold M.B., Bluth J., Kastin A.J. Transport of brain-derived neurotrophic factor across the blood-brain barrier. Neuropharmacology. 1998;37:1553–1561. doi: 10.1016/S0028-3908(98)00141-5. [DOI] [PubMed] [Google Scholar]
- 57.Ward R., Abdul Y., Ergul A. Endothelin-1 inhibition improves the mBDNF/proBDNF ratio in endothelial cells and HT22 neurons under high glucose/palmitate growth conditions. Physiol. Res. 2018;67(Suppl. 1):S237–S246. doi: 10.33549/physiolres.933837. [DOI] [PubMed] [Google Scholar]
- 58.Hyman C., Hofer M., Barde Y.A., Juhasz M., Yancopoulos G.D., Squinto S.P., Lindsay R.M. BDNF is a neurotrophic factor for dopaminergic neurons of the substantia nigra. Nature. 1991;350:230–232. doi: 10.1038/350230a0. [DOI] [PubMed] [Google Scholar]
- 59.Popova N.K., Naumenko V.S. Neuronal and behavioral plasticity: The role of serotonin and BDNF systems tandem. Expert Opin. Ther. Targets. 2019;23:227–239. doi: 10.1080/14728222.2019.1572747. [DOI] [PubMed] [Google Scholar]
- 60.Venezia A.C., Quinian E., Roth S.M. A single bout of exercise increase hippocampal Bdnf: Influence of chronic exercise and noradrenaline. Genes Brain Behav. 2017;16:800–811. doi: 10.1111/gbb.12394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cooke M., Cruttenden R., Mellor A., Lumb A., Pattman S., Burnett A., Boot C., Burnip L., Boos C., O’Hara J., et al. A pilot investigation into the effects of acute normobaric hypoxia, high altitude exposure and exercise on serum angiotensin-converting enzyme, aldosterone and cortisol. J. Renin Angiotensin Aldosterone Syst. 2018;19:1470320318782782. doi: 10.1177/1470320318782782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schneider D.A., McGuiggin M.E., Kamimorim G.H. A comparison of the blood lactate and plasma catecholamine thresholds in untrained male subjects. Int. J. Sports Med. 1992;13:52. doi: 10.1055/s-2007-1024565. [DOI] [PubMed] [Google Scholar]
- 63.Miguel P.M., Deniz B.F., Deckmann I., Confortim H.D., Diaz R., Diaz R., Laureano D.P., Silveira P.P., Pereira L.O. Prefrontal Cortex Dysfunction in Hypoxic-Ischaemic Encephalopathy Contributes to Executive Function Impairments in Rats: Potential Contribution for Attention-Deficit/Hyperactivity Disorder. World J. Biol. Psychiatry. 2018;19:547–560. doi: 10.1080/15622975.2016.1273551. [DOI] [PubMed] [Google Scholar]
- 64.Newsholme E.A., Acworth I.N., Blomstrand E. Amino acids, brain neurotransmitters and a functional link between muscle brain that is important in sustained exercise. In: Benzi G., editor. Advances in Biochemistry. John Libby Eurotext; London, UK: 1987. pp. 127–138. [Google Scholar]
- 65.Wang G.J., Volkow N.D., Fowler J.S., Franceschi D., Logan J., Pappas N.R., Wong C.T., Netusilm N. PET studies of the effects of aerobic exercise on human striatal dopamine release. J. Nucl. Med. 2000;41:1352–1356. [PubMed] [Google Scholar]
- 66.El-Khodor B.F., Boksa P. Long-term reciprocal changes in dopamine levels in prefrontal cortex versus nucleus accumbens in rats born by Caesarean section compared to vaginal birth. Exp. Neurol. 1997;145:118–129. doi: 10.1006/exnr.1997.6437. [DOI] [PubMed] [Google Scholar]
- 67.Piotrowicz ż., Chalimoniuk M., Ploszczyca K., Czuba M., Langfort J. Acute normobaric hypoxia does not affect the simultaneous exercise-induced increase in circulating BDNF and GDNF in young healthy men: A feasibility study. PLoS ONE. 2019;14:e0224207. doi: 10.1371/journal.pone.0224207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang H., Niu F., Fan W., Shi J., Zhang J., Li B. Modulating effects of predconditioning exercise in the expression of ET-1 and BNP via HIF-1a in ischemically injured brain. Metab. Brain Dis. 2019;34:1299–1311. doi: 10.1007/s11011-019-00450-z. [DOI] [PubMed] [Google Scholar]
- 69.Cotman C.W., Engesser-Cesar C. Exercise Enhances and Protects Brain Function. Exerc. Sport Sci. Rev. 2002;30:75–79. doi: 10.1097/00003677-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 70.Ludyga S., Gerber M., Brand S., Holsboer-Trachsler E., Puhse U. Acute Effects of Moderate Aerobic Exercise on Specific Aspects of Executive Function in Different Age and Fitness Groups: A Meta-Analysis. Psychophysiology. 2016;53:1611–1626. doi: 10.1111/psyp.12736. [DOI] [PubMed] [Google Scholar]
- 71.Czuba M., Wilk R., Karpiński J., Chalimoniuk M., Zajac A., Langfort J. Intermittent hypoxic training improves anaerobic performance in competitive swimmers when implemented into a direct competition mesocycle. PLoS ONE. 2017;12:e0180380. doi: 10.1371/journal.pone.0180380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Czuba M., Bril G., Płoszczyca K., Piotrowicz Z., Chalimoniuk M., Roczniok R., Zembron-Lacny A., Gerasimuk D., Langfort J. Intermittent hypoxic training at lactate threshold intensity improves aiming performance in well-trained biathletes with little change of cardiovascular variables. Biomed. Res. Int. 2019;2019:1287506. doi: 10.1155/2019/1287506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Millet G.P., Roels B., Schmitt L., Woorons X., Richalet J.P. Combining hypoxic methods for peak performance. Sports Med. 2010;40:1–25. doi: 10.2165/11317920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 74.Dobashi S., Horiuchi M., Endo J., Kiuchi M., Koyama K. Cognitive Function and Cerebral Oxygenation during Prolonged Exercise under Hypoxia in Healthy Young Males. High Alt. Med. Biol. 2016;17:214–221. doi: 10.1089/ham.2016.0036. [DOI] [PubMed] [Google Scholar]
- 75.Li P., Zhang G., You H.Y., Zheng R., Gao Y.Q. Training-dependent cognitive advantage is suppressed at high altitude. Physiol. Behav. 2012;106:439–445. doi: 10.1016/j.physbeh.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 76.Chang Y.K., Labban J.D., Gapin J.I., Etnier J.L. The effects of acute exercise on cognitive performance: A meta-analysis. Brain Res. 2012;1453:87–101. doi: 10.1016/j.brainres.2012.02.068. [DOI] [PubMed] [Google Scholar]
- 77.Archer T., Josefsson T., Lindwall M. Effects of Physical Exercise on Depressive Symptoms and Biomarkers in Depression. CNS Neurol. Disord. Drug Targets. 2014;13:1640–1653. doi: 10.2174/1871527313666141130203245. [DOI] [PubMed] [Google Scholar]
- 78.Campos C., Rocha N.B., Lattari E., Nardi A.E., Machado S. Exercise Induced Neuroplasticity to Enhance Therapeutic Outcomes of Cognitive Remediation in Schizophrenia: Analyzing the Role of Brai Nderived Neurotrophic Factor. CNS Neurol. Disord. Drug Targets. 2017;16:638–651. doi: 10.2174/1871527315666161223142918. [DOI] [PubMed] [Google Scholar]
- 79.Das A.K., Dhar P., Sharma V.K., Barhwal K., Hota S.K., Norboo T., Singh S.B. High Altitude With Monotonous Environment Has Significant Impact on Mood and Cognitive Performance of Acclimatized Lowlanders: Possible Role of Altered Serum BDNF and Plasma Homocysteine Level. J. Affect. Disord. 2018;237:94–103. doi: 10.1016/j.jad.2018.04.106. [DOI] [PubMed] [Google Scholar]
- 80.Wang W.H., He G.P., Xiau P., Gu C., Chen H.Y. Relationship Between Brain-Derived Neurotrophic Factor and Cognitive Function of Obstructive Sleep Apnea/Hypopnea Syndrome Patients. Asian Pac. J. Trop. Med. 2012;5:906–910. doi: 10.1016/S1995-7645(12)60169-2. [DOI] [PubMed] [Google Scholar]
- 81.Halievski K., Nath S., Katsuno M., Adachi H., Sobue G., Breedlove S., Lieberman A., Jordan C. Disease Affects Bdnf Expression in Synaptic and Extrasynaptic Regions of Skeletal Muscle of Three SBMA Mouse Models. Int. J. Mol. Sci. 2019;20:1314. doi: 10.3390/ijms20061314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Satriotomo I., Nichols N.I., Dale E.A., Emery A.T., Dahlberg J.M., Mitcell G.S. Repetitive Acute Intermittent Hypoxia Increases Growth/Neurotrophic Factor Expression in Non-Respiratory Motor Neurons. Neuroscience. 2016;332:449–488. doi: 10.1016/j.neuroscience.2016.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Karege F., Schwald M., Cisse M. Postnatal developmental profile of brain-derived neurotrophic factor in rat brain and platelets. Neurosci. Lett. 2002;328:261–264. doi: 10.1016/S0304-3940(02)00529-3. [DOI] [PubMed] [Google Scholar]
- 84.Rasmussen P., Brassard P., Adser H., Pedersen M.V., Leick L., Hart E., Secher N.H., Pedersen B.K., Pilegaard H. Evidence for a release of brain-derived neurotrophic factor from the brain during exercise. Exp. Physiol. 2009;94:1062–1069. doi: 10.1113/expphysiol.2009.048512. [DOI] [PubMed] [Google Scholar]
- 85.Erickson K.I., Voss M.W., Prakas R.S., Basak C., Szabo A., Chaddock L., Kim J.S., Heo S., Alves H., White S.M. Exercise Training Increases Size of Hippocampus and Improves Memory. Proc. Natl. Acad. Sci. USA. 2011;108:3017–3322. doi: 10.1073/pnas.1015950108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lipski R.H., Marini A.M. Neurotrophic factor in neuronal survival and behavior-related plasticity. Ann. N. Y. Acad. Sci. 2007;1122:130–143. doi: 10.1196/annals.1403.009. [DOI] [PubMed] [Google Scholar]
- 87.Huang E.J., Reichardt L.E. Neurotrophins: Roles in neuronal development and function. Annu. Rev. Neurosci. 2009;24:677–736. doi: 10.1146/annurev.neuro.24.1.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ferris L.T., Williams J.S., Shen C.L. The Effect of Acute Exercise on Serum Brain-Derived Neurotrophic Factor Levels and Cognitive Function. Med. Sci. Sports Exerc. 2007;39:728–734. doi: 10.1249/mss.0b013e31802f04c7. [DOI] [PubMed] [Google Scholar]
- 89.Tsai C.L., Chen F.C., Pan C.Y., Wang C.H., Huang T.H., Chen T.C. Impact of Acute Aerobic Exercise and Cardiorespiratory Fitness on Visuospatial Attention Performance and Serum BDNF Levels. Psychoneuroedocrinology. 2014;41:121–131. doi: 10.1016/j.psyneuen.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 90.Slusher A.L., Patterson V.T., Schwartz C.S., Acevedo E.O. Impact of high intensity exercise on execrative function and brain derived neurotrophic factor in healthy college aged males. Phsiol. Behav. 2018;191:116–122. doi: 10.1016/j.physbeh.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 91.Sasi M., Vignoli B., Cannossa M., Blum R. Neurobiology of Local and Intercellular BDNF Signaling. Plugers Arch. Eur. J. Physiol. 2017;469:593–610. doi: 10.1007/s00424-017-1964-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fowler C., Gervitz L., Hamilton E., Walker J.A. Systemic Hypoxia and the Depression of Synaptic Transmission in Rat Hippocampus after Carotid Artery Occlusion. J. Physiol. 2003;550:961–972. doi: 10.1113/jphysiol.2003.039594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lanigan S., Corcoran A.E., Wall A., Mukandala G., O’Connor J.J. Acute Hypoxic Exposure and Prolyl-Hydroxylase Inhibition Improves Synaptic Transmission Recovery Time from a Subsequent Hypoxic Insult in Rat Hippocampus. Brain Res. 2018;1701:212–218. doi: 10.1016/j.brainres.2018.09.018. [DOI] [PubMed] [Google Scholar]
- 94.Kline D.D., Ramirez-Navarro A., Kunze D.L. Adaptive Depression in Synaptic Transmission in the Nucleus of the Solitary Tract after In Vivo Chronic Intermittent Hypoxia: Evidence for Homeostatic Plasticity. J. Neurosci. 2007;27:4663–4673. doi: 10.1523/JNEUROSCI.4946-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jonas E., Hickman J.A., Hardwick J.M., Kaczmarek L.K. Exposure to Hypoxia Rapidly Induces Mitochondrial Channel Activity within a Living Synapse. J. Biol. Chem. 2005;280:4491–4497. doi: 10.1074/jbc.M410661200. [DOI] [PubMed] [Google Scholar]
- 96.Muthuraju S., Maiti P., Solanki P., Sharma A.K., Amitabh, Singh S.B., Prasad D., Ilavazhagan G. Acetylcholinesterase Inhibitors Enhance Cognitive Functions in Rats Following Hypobaric Hypoxia. Behav. Brain Res. 2009;203:1–14. doi: 10.1016/j.bbr.2009.03.026. [DOI] [PubMed] [Google Scholar]
- 97.Echouffo-Tcheugui J.B., Conner S.C., Himali J.J., Maillard P., DeCarli C.S., Beiser A.S., Vasan R.S., Seshadri S. Circulating Cortisol and Cognitive and Structural Brain Measures: The Framingham Heart Study. Neurology. 2018;91:e1961–e1970. doi: 10.1212/WNL.0000000000006549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sroykham W., Wongsawat Y. Effects of Brain Activity, Morning Salivary Cortisol, and Emotion Regulation on Cognitive Impairment in Elderly People. Medicine. 2019;98:e16114. doi: 10.1097/MD.0000000000016114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stomby A., Boraxbekk C.J., Lundquist A., Nordin A., Nilsson L.G., Adolfsson R., Nyberg L., Olsson T. Higher Diurnal Salivary Cortisol Levels Are Related to Smaller Prefrontal Cortex Surface Area in Elderly Men and Women. Eur. J. Endocrinol. 2016;175:117–126. doi: 10.1530/EJE-16-0352. [DOI] [PubMed] [Google Scholar]
- 100.Dominguez G., Henkous N., Prevot T., David V., Guillou J.L., Belzung C., Mons N., Béracochéa D. Sustained Corticosterone Rise in the Prefrontal Cortex Is a Key Factor for Chronic Stress-Induced Working Memory Deficits in Mice. Neurobiol. Stress. 2019;10:100161. doi: 10.1016/j.ynstr.2019.100161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Vuolteenaho O., Koistinen P., Martikkala V., Takala T. Leppaluoto. Effect of physical exercise in hypobaric conditions o atrial natriuretic peptide secretion. Am. J. Physiol. 1992;263:647–652. doi: 10.1152/ajpregu.1992.263.3.R647. [DOI] [PubMed] [Google Scholar]
- 102.Rikki R.E., Edwards M.E. Effects of a three-year exercise program on motor function and cognitive processing speed I older woe. Res. Qart. Exerc. Sport. 1991;62:61–67. doi: 10.1080/02701367.1991.10607519. [DOI] [PubMed] [Google Scholar]
- 103.Bouissou P., Peronnet F., Brisson G., Helie R., Ledoux M. Metabolic and endocrine responses to graded exercise under acute hypoxia. Eur. J. Appl. Physiol. 1986;55:290–294. doi: 10.1007/BF02343801. [DOI] [PubMed] [Google Scholar]
- 104.Bouissou P., Peronnet F., Brisson G., Helie R., Ledoux M. Fluid-electrolyte shift and renin-aldosterone responses to exercise under hypoxia. Horm. Met. Res. 1987;19:331–334. doi: 10.1055/s-2007-1011814. [DOI] [PubMed] [Google Scholar]
- 105.Rostrup M. Catecholamines, hypoxia and high altitude. Acta Phsiol. Scand. 1988;11:389–399. doi: 10.1046/j.1365-201X.1998.00335.x. [DOI] [PubMed] [Google Scholar]
- 106.Weber D.A., Reynolds C.R. Clinical Perspectives on Neurobiological Effects of Psychological Trauma. Neuropsychol. Rev. 2004;14:115–129. doi: 10.1023/B:NERV.0000028082.13778.14. [DOI] [PubMed] [Google Scholar]
- 107.Reader T.A. Distribution of Catecholamines and Serotonin in the Rat Cerebral Cortex: Absolute Levels and Relative Proportions. J. Neural Transm. 1981;50:13–27. doi: 10.1007/BF01254910. [DOI] [PubMed] [Google Scholar]
- 108.Miguel P.M., Pereira L.O., Barth B., Filho E.J.M., Pokhvisneva I., Nguyen T.T.T., Garg E., Razzolini B.R., Koh D.X.P. Prefrontal Cortex Dopamine Transporter Gene Network Moderates the Effect of Perinatal Hypoxic-Ischemic Conditions on Cognitive Flexibility and Brain Gray Matter Density in Children. Biol. Psychiatry. 2019;86:621–630. doi: 10.1016/j.biopsych.2019.03.983. [DOI] [PubMed] [Google Scholar]
- 109.Ogh S., Tsukamoto H., Hirasawa A., Hasegawa H., Hirose N., Hashimoto T. The Effect of Changes in Cerebral Blood Flow on Cognitive Function during Exercise. Physiol. Rep. 2014;2:e12163. doi: 10.14814/phy2.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Adachi M., Yang Y., Furiuchi Y., Miiyamoto C. Cloning and characterization of cDNA encoding human A-type endothelin receptor. Biochem. Biophys. Res. Commun. 1991;180:1265–1272. doi: 10.1016/S0006-291X(05)81332-4. [DOI] [PubMed] [Google Scholar]
- 111.Palmer R.M., Ferrige A.G., Moncada S. Nitric Oxide Release Accounts for the Biological Activity of Endothelium-Derived Relaxing Factor. Nature. 1987;327:524–526. doi: 10.1038/327524a0. [DOI] [PubMed] [Google Scholar]
- 112.Garthwaite J. Nitric oxide as a multimodal transmitter in the brain: Discovery and current status. Br. J. Pharmacol. 2019;176:197–211. doi: 10.1111/bph.14532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gilchrist M., Winyard P.G., Fulford J., Anning C., Shore A.C., Benjamin N. Dietary nitrate supplementation improves reaction time in type 2 diabetes: Development and application of a novel nitrate-depleted beetroot juice placebo. Nitric Oxide. 2014;19:333–337. doi: 10.1016/j.niox.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 114.Lefferts W.K., Hughes W.E., White C.N., Brutsaert T.D., Heffernan K.S. Effect of acute nitrate supplementation on neurovascular coupling and cognitive performance in hypoxia. Appl. Physiol. Nutr. Metab. 2016;41:133–141. doi: 10.1139/apnm-2015-0400. [DOI] [PubMed] [Google Scholar]
- 115.Shannon O.M., Duckworth L., Barlow M.J., Deighton K., Matu J., Williams E.L., Woods D., Xie L., Stephan B.C.M., Siervo M., et al. Effects of Dietary Nitrate Supplementation on Physiological Responses, Cognitive Function, and Exercise Performance at Moderate and Very-High Simulated Altitude. Front. Physiol. 2017;8:401. doi: 10.3389/fphys.2017.00401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Basso J.C., Suzuki W.A. The Effects of Acute Exercise on Mood, Cognition, Neurophysiology, and Neurochemical Pathways: A Review. Brain Plast. 2017;2:127–152. doi: 10.3233/BPL-160040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Adeva-Andany M., Lopez-Ojen M., Funcasta-Calderon R., Ameneiros-Rodríguez E., Donapetry-García C., Vila-Altesor M., Rodríguez-Seijas J. Comprehensive review on Lactate Metabolism in Human Health. Mitochondrion. 2014;17:76–100. doi: 10.1016/j.mito.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 118.Pellerin L., Pellegri G., Bittar P.G., Charnay Y., Bouras C., Martinm J.L., Stella N., Magistretti P.J. Evidence supporting the existence of an activity-dependent astrocyte neuron lactate shuttle. Dev. Neurosci. 1998;20:291–299. doi: 10.1159/000017324. [DOI] [PubMed] [Google Scholar]
- 119.Carrard A., Elsayed M., Margineanu M., Boury-Jamot B., Fragnière L., Meylan E.M., Petit J.M., Fiumelli H., Magistretti P.J., Martin J.L. Peripheral administration of lactate produces antidepressant-like effects. Mol. Psychiatry. 2018;23:392–399. doi: 10.1038/mp.2016.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Liu C., Wu J., Zhu J., Kuei C., Yu J., Shelton J., Sutton S.W., Li X., Yun S.J., Mirzadegan T. Lactate inhibits lipolysis in fat cells through activation of an orphan G-protein-coupled receptor, GPR81. J. Biol. Chem. 2009;284:2811–2822. doi: 10.1074/jbc.M806409200. [DOI] [PubMed] [Google Scholar]
- 121.Urbaniak G.C., Plous S. Research Randomizer (Version 4.0) [Computer Software] [(accessed on 25 March 2017)];2013 Available online: http://www.randomizer.org/
- 122.Kuipers H., Verstappen F.T.J., Keizer H.A., Guerten P., van Kranenburg G. Variability of aerobic performance in the laboratory and its physiological correlates. Int. J. Sports Med. 1985;6:197–201. doi: 10.1055/s-2008-1025839. [DOI] [PubMed] [Google Scholar]