Perceived energy predicts survival, physical function, and physical activity (PA)1–5. However, the evidence is among patient populations or young adults. Whether perceived energy plays a role in PA and health outcomes in older adults living in the community is unknown. We hypothesized that in older men and women, higher self-reported energy would be associated with higher levels of PA assessed objectively via the SenseWear Armband (SWA). Assessing perceived energy levels may offer a potential behavioral screening test for PA behaviors among community-dwelling older adults, who are likely to benefit from continued PA behaviors.
We identified 96 participants from the Health, Aging and Body Composition Study with concurrent data on self-reported energy and SWA between 2011 and 2012. All participants provided written informed consent. The University of Pittsburgh Institutional Review Board approved the protocol.
Participants answered the question “What was your usual energy level during the past month?” on a 0–10 scale, 0 indicating no energy and 10 indicating the most energy. We used the SWA to detect daily mean total energy expenditure (kcal), active energy expenditure (kcal), intensity (METs), duration (minutes) of PA (≥3 METs), and step counts. SWA measures were obtained via pattern detection algorithms6, with good accuracy and reliability in a free-living environment, validated in older adults7. Participants were instructed to wear the SWA on the left upper arm for seven consecutive days (SenseWear Pro 7.0). Data with ≥3days of the on-body time were included. Values >4 SD were excluded for analysis. Other measures of interest included physical function measured as usual pace gait speed while walking a 4-m-long walkway using the GaitMat II™ system (EQ Inc., Chalfont, Pennsylvania). Depressive symptoms were measured using the Center for Epidemiologic Study Depression short form (CES-D 10), a 10-item scale scored 0–308. Dementia diagnosis was adjudicated using an extensive neuropsychological battery and medical records since 19976.
Associations of self-reported energy with SWA measures and other variables were tested using Spearman’s correlation and independent t-tests as appropriate (SAS v9.4, SAS Institute, Inc., Cary, NC). The association of self-reported energy with each SWA measure was adjusted for usual gait speed, because the physical function may limit PA participation in older adults. We did not adjust for age, sex, body weight, and height because these were accounted for in the calculation of SWA measures6.
The study participants (mean age: 86.6 (SD=2.4) 52% women, 45% Black) had mean self-report energy of 6.0 (SD=2.0), and usual gait speed of 0.81 m/sec (SD=0.20). 11% had dementia. Self-reported energy was not associated with age, sex, race, education level, gait speed, or cognitive status (p>0.05). There was a trend of higher self-reported energy being associated with lower CES-D 10 (p=0.08). Self-reported energy was positively associated with daily active energy expenditure, METs, minutes of PA, and step counts, but not with total energy expenditure (Figure 1). After controlling for gait speed, results remained substantially unchanged.
Figure 1.
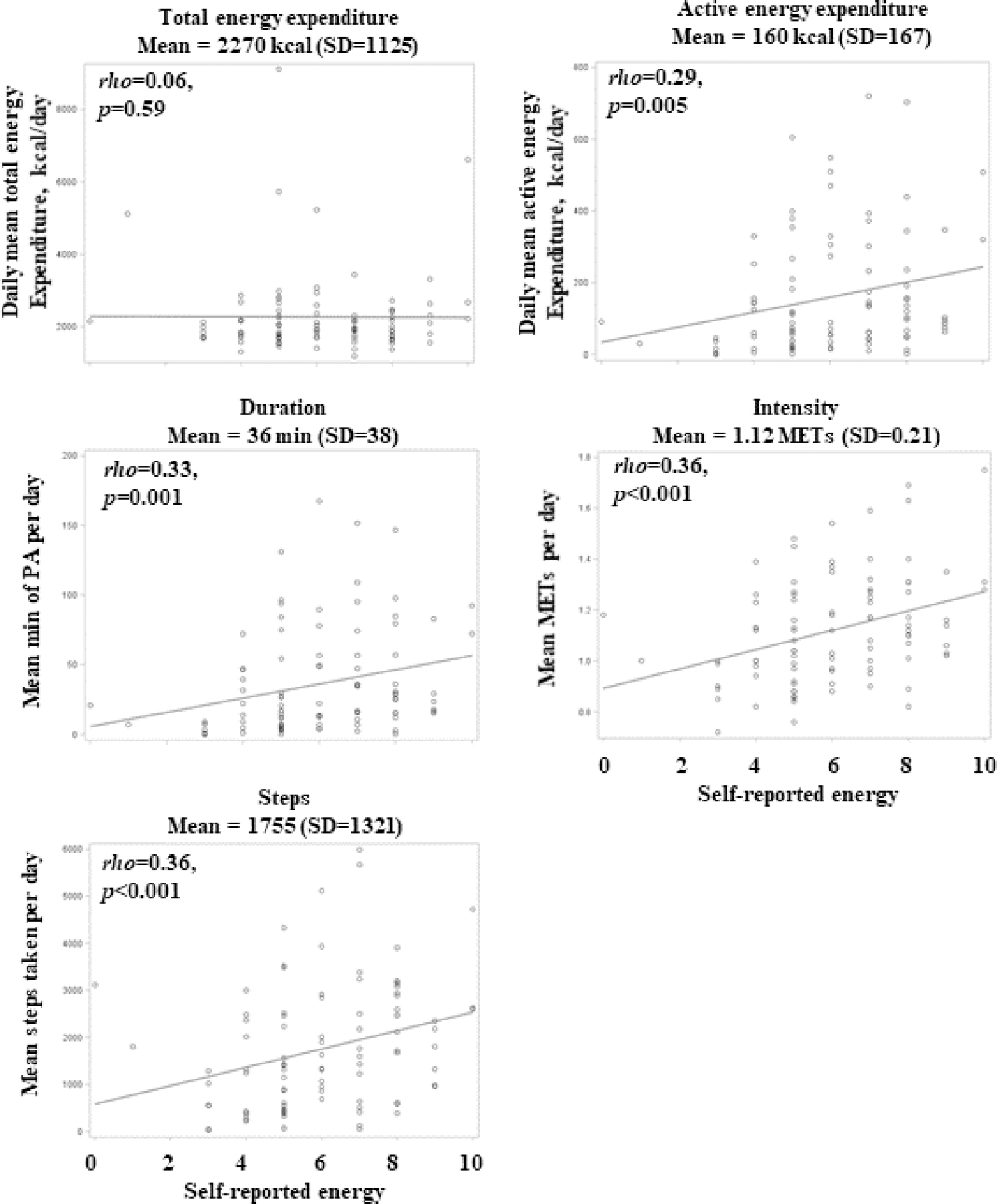
Scatterplots between self-reported energy and measures by the SenseWear Armband.
In this sample of older adults in their 80s, self-reported energy was positively associated with PA behaviors and the amount of energy expended while being active, independent of physical function. Associations were consistent across PA measures, albeit stronger for step counts and intensity (effect size toward moderate9). Perhaps step counts and intensity capture a wider spectrum of PA compared to active energy expenditure and duration, which measure activities at or above 3 METs.
Self-reported energy was not associated with total energy expenditure, perhaps because total energy expenditure also includes energy spent for food thermogenesis and for homeostasis, including resting metabolic rate10. The trend of perceived energy with depressive symptoms suggests a role in psychological factors or motivation. However, we did not find an association with cognitive status.
Limitations include modest sample size, somewhat healthier than the general population due to their voluntary participation and eligibility for brain MRI6. This study is cross-sectional, and causation or direction of association cannot be established. It is possible that physically active individuals feel more energy. The relationship may also be bidirectional or explained by a common cause. The use of SWA is a strength, as it provided a wealth of validated energy expenditure and PA measures7. The study sample is well-characterized biracial (45% Black) community-dwelling older adults, including both men and women.
In sum, assessing energy levels on a simple 0–10 scale may offer a potential behavioral screening test to identify older individuals who lead a sedentary lifestyle. These individuals may be targeted for tailored counseling and/or coaching to reduce the risks of being sedentary. Longitudinal studies of self-reported energy predicting changes in PA are warranted.
Acknowledgments
Funding source: This research was supported in part by the Intramural Research Program of the National Institute on Aging. This research was supported by National Institute on Aging (NIA) Contracts N01-AG-6-2101, N01-AG-6-2103, N01-AG-6-2106; NIA grants R01-AG028050, P30-AG024827, T32AG055381, U01AG061393, and NINR grant R01-NR012459, and supported by 8th Annual Department of Epidemiology Small Grant program, University of Pittsburgh.
Sponsor’s role: None.
Footnotes
Conflict of Interest: None declared.
REFERENCES
- 1.Hayashino Y, Okamura S, Tsujii S, Ishii H. Predictive Validity of Each Item of the 8-Item Short-Form Health Survey for All-Cause Mortality in Japanese patients with type 2 diabetes: A prospective Cohort Study (Diabetes Distress and Care Registry at Tenri [DDCRT 19]). Experimental and Clinical Endocrinology & Diabetes. 2019. [DOI] [PubMed]
- 2.Jason L, Benton M, Torres-Harding S, Muldowney K. The impact of energy modulation on physical functioning and fatigue severity among patients with ME/CFS. Patient Educ Couns. 2009;77(2):237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurita N, Akizawa T, Fukuhara S. Vitality Measured as Self-reported Energy Level and Clinical Outcomes in Hemodialysis Patients: The Japanese Dialysis Outcomes and Practice Pattern Study (J-DOPPS). Am J Kidney Dis. 2019;73(4):486–495. [DOI] [PubMed] [Google Scholar]
- 4.Lerdal A, Kottorp A, Gay CL, Lee KA. Lee Fatigue And Energy Scales: exploring aspects of validity in a sample of women with HIV using an application of a Rasch model. Psychiatry Res. 2013;205(3):241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellingson LD, Kuffel AE, Vack NJ, Cook DB. Active and sedentary behaviors influence feelings of energy and fatigue in women. Med Sci Sports Exerc. 2014;46(1):192–200. [DOI] [PubMed] [Google Scholar]
- 6.Tian Q, Glynn NW, Erickson KI, et al. Objective measures of physical activity, white matter integrity and cognitive status in adults over age 80. Behav Brain Res. 2015;284:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mackey DC, Manini TM, Schoeller DA, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66(10):1108–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 9.Schober P, Boer C, Schwarte LA. Correlation Coefficients: Appropriate Use and Interpretation. Anesth Analg. 2018;126(5):1763–1768. [DOI] [PubMed] [Google Scholar]
- 10.Alexander NB, Taffet GE, Horne FM, et al. Bedside-to-Bench conference: research agenda for idiopathic fatigue and aging. J Am Geriatr Soc. 2010;58(5):967–975. [DOI] [PMC free article] [PubMed] [Google Scholar]


