Abstract
Background
Behavioural therapies represent one of several categories of psychological therapies that are currently used in the treatment of depression. However, the effectiveness and acceptability of behavioural therapies for depression compared with other psychological therapies remain unclear.
Objectives
1. To examine the effects of all BT approaches compared with all other psychological therapy approaches for acute depression.
2. To examine the effects of different BT approaches (behavioural therapy, behavioural activation, social skills training and relaxation training) compared with all other psychological therapy approaches for acute depression.
3. To examine the effects of all BT approaches compared with different psychological therapy approaches (CBT, third wave CBT, psychodynamic, humanistic and integrative psychological therapies) for acute depression.
Search methods
We searched the Cochrane Depression Anxiety and Neurosis Group Trials Specialised Register (CCDANCTR, 31/07/2013), which includes relevant randomised controlled trials from The Cochrane Library (all years), EMBASE, (1974‐), MEDLINE (1950‐) and PsycINFO (1967‐). We also searched CINAHL (May 2010) and PSYNDEX (June 2010) and reference lists of the included studies and relevant reviews for additional published and unpublished studies.
Selection criteria
Randomised controlled trials that compared behavioural therapies with other psychological therapies for acute depression in adults.
Data collection and analysis
Two or more review authors independently identified studies, assessed trial quality and extracted data. We contacted study authors for additional information.
Main results
Twenty‐five trials involving 955 participants compared behavioural therapies with one or more of five other major categories of psychological therapies (cognitive‐behavioural, third wave cognitive‐behavioural, psychodynamic, humanistic and integrative therapies). Most studies had a small sample size and were assessed as being at unclear or high risk of bias. Compared with all other psychological therapies together, behavioural therapies showed no significant difference in response rate (18 studies, 690 participants, risk ratio (RR) 0.97, 95% confidence interval (CI) 0.86 to 1.09) or in acceptability (15 studies, 495 participants, RR of total dropout rate 1.02, 95% CI 0.65 to 1.61). Similarly, in comparison with each of the other classes of psychological therapies, low‐quality evidence showed better response to cognitive‐behavioural therapies than to behavioural therapies (15 studies, 544 participants, RR 0.93, 95% CI 0.83 to 1.05) and low‐quality evidence of better response to behavioural therapies over psychodynamic therapies (2 studies, 110 participants, RR 1.24, 95% CI 0.84 to 1.82).
When compared with integrative therapies and humanistic therapies, only one study was included in each comparison, and the analysis showed no significant difference between behavioural therapies and integrative or humanistic therapies.
Authors' conclusions
We found low‐ to moderate‐quality evidence that behavioural therapies and other psychological therapies are equally effective. The current evidence base that evaluates the relative benefits and harms of behavioural therapies is very weak. This limits our confidence in both the size of the effect and its precision for our key outcomes related to response and withdrawal. Studies recruiting larger samples with improved reporting of design and fidelity to treatment would improve the quality of evidence in this review.
Plain language summary
Behavioural therapies versus other psychological therapies for depression
Major depression is one of the common mental illnesses characterised by persistent low mood and loss of interest in pleasurable activities, accompanied by a range of symptoms, including weight loss, insomnia, fatigue, loss of energy, inappropriate guilt, poor concentration and morbid thoughts of death. Whilst antidepressants remain the mainstay of treatment for depression in healthcare settings, psychological therapies are still important alternative or additional interventions for depressive disorders. Nowadays, a diverse range of psychological therapies are available (such as cognitive‐behavioural therapies, behavioural therapies, psychodynamic therapies, humanistic therapies and integrative therapies). It is very important to know whether one type of psychological therapy is more effective than another, and to know which psychological therapy is the most effective treatment for depression. In this review, we focused on one of these—behavioural therapies (BT)—because they are relatively simple to deliver, and interest in them has recently been renewed. Behavioural therapies are usually based purely on operant and respondent principles, aimed to change the patient's depressive mood by changing his or her behaviour patterns. Whilst a number of BT models have been developed, we categorised the following approaches as behavioural therapies in this review: behavioural therapy (based on Lewinsohn's model, which focused on increasing pleasant activities), behavioural activation (originated from behavioural component of cognitive‐behavioural therapy and based on Jacobson's work in 1996), social skills training/assertiveness training and relaxation therapy.
In this review, we assessed the efficacy and acceptability of behavioural therapies compared with all other psychological therapies in the treatment of acute phase depression (neither long‐term nor treatment‐resistant depression) in adults. Twenty‐five randomised controlled trails were included in this review. The quality of evidence in our review is low because of issues with the design of the studies that we found and lack of precision in our results. Although we found that behavioural therapies and all other psychological therapies are equally effective and acceptable, more research is needed to confirm this finding.
Summary of findings
Background
Description of the condition
Major depression is characterised by persistent low mood and loss of interest in pleasurable activities, accompanied by a range of symptoms, including weight loss, insomnia, fatigue, loss of energy, inappropriate guilt, poor concentration and morbid thoughts of death (APA 2000). Somatic complaints are also a common feature of depression, and people with severe depression may develop psychotic symptoms (APA 2000).
Depression is the third leading cause of disease burden worldwide and is expected to show a rising trend over the next 20 years (WHO 2004; WHO 2008). A recent European study has estimated the point prevalence of major depression and dysthymia at 3.9% and 1.1%, respectively (ESEMeD/MHEDEA 2004). As the largest source of non‐fatal disease burden in the world, accounting for 12% of years lived with disability (Ustun 2004), depression is associated with marked personal, social and economic morbidity and loss of functioning and productivity, and it creates significant demands on service providers in terms of workload (NICE 2009). Depression is also associated with a significantly increased risk of mortality (Cuijpers 2002). The strength of this association, even when confounders such as physical impairment, health‐related behaviours and socio‐economic factors are taken into account, has been shown to be comparable with, or greater than, the strength of the association between smoking and mortality (Mykletun 2009).
Description of the intervention
Clinical guidelines recommend pharmacological and psychological interventions, alone or in combination, in the treatment of moderate to severe depression (NICE 2009). The prescribing of antidepressants has increased dramatically in many Western countries over the past 20 years, mainly with the advent of selective serotonin reuptake inhibitors and other agents such as serotonin–noradrenaline reuptake inhibitors (SNRIs) and noradrenalinergic and specific serotonergic antidepressants (NaSSAs). Antidepressants remain the mainstay of treatment for depression in healthcare settings (Ellis 2004; NICE 2009).
Whilst antidepressants are of proven efficacy for the acute treatment of depression (Cipriani 2005; Guaiana 2007; Arroll 2009; Cipriani 2009; Cipriani 2009a; Cipriani 2009b), adherence rates remain very low (Hunot 2007; van Geffen 2009), in part because of patients' concerns about side effects and possible dependency (Hunot 2007). Furthermore, surveys consistently demonstrate patients' preference for psychological therapies over treatment with antidepressants (Churchill 2000; Riedel‐Heller 2005). Therefore, psychological therapies offer an important alternative or adjunctive intervention for depressive disorders.
A diverse range of psychological therapies are now available for the treatment of common mental disorders (Pilgrim 2002). Psychological therapies may be broadly categorised into four separate philosophical and theoretical schools, comprising psychoanalytic/dynamic (Freud 1949; Klein 1960; Jung 1963), behavioural (Watson 1924; Skinner 1953; Wolpe 1958), humanistic (Maslow 1943; Rogers 1951; May 1961) and cognitive approaches (Lazarus 1971; Beck 1979). Each of these four schools incorporates several different and overlapping psychotherapeutic approaches. Some psychotherapeutic approaches, such as cognitive‐analytic therapy (CAT) (Ryle 1990), explicitly integrate components from several theoretical schools. Other approaches, such as interpersonal therapy (IPT) for depression (Klerman 1984), have been developed to address characteristics considered specific to the disorder of interest.
Behaviour therapy (BT) became a dominant force in the 1950s, drawing from the work of Skinner 1953, Wolpe 1958 and Eysenck 1960. BT emphasises the role of environmental cues in influencing the acquisition and maintenance of behaviours (Nelson‐Jones 1990) and, in contrast with psychoanalysis, was developed through experimentally derived principles of learning (Rachman 1997).
Several BT models have been developed for the treatment of depression, including Lewinsohn's behavioural therapy approach (Lewinsohn 1974), behavioural activation (BA) (Jacobson 1996) and social skills training (Bellack 1980). Some models initially developed as behavioural treatments, including problem‐solving therapy (Nezu 1986), self‐control therapy (Fuchs 1977; Rehm 1977) and the Coping with Depression programme (Lewinsohn 1984), have, over time, integrated cognitive techniques (Jacobson 2001) (see Types of interventions section for a description of these approaches).
How the intervention might work
Skinner 1953 proposed that depression was associated with an interruption in established sequences of healthy behaviour that were previously positively reinforced by the social environment and were based on operant conditioning principles (in which behaviour patterns are learnt, rather than instinctive). In subsequent expansions of this model, reduction of positively reinforced healthy behaviour has also been attributed to a decrease in the number and range of reinforcing stimuli available to the individual, lack of skill in obtaining positive reinforcement (Lewinsohn 1974) and/or increased frequency of punishment (Lewinsohn 1984).
Conventional BT models for depression focus attention on facilitating access to pleasant events and positive reinforcers and decreasing the intensity and frequency of events and consequences deemed to be unpleasant/negative (Lewinsohn 1972), through monitoring of pleasant events, activity scheduling, social skills development, assertiveness training, relaxation therapy and time management training (Hopko 2003a).
Why it is important to do this review
With the advent of cognitive therapy in the 1970s, BT approaches based purely on operant and respondent principles became regarded as insufficient. However, over the past 10 to 15 years, interest in the feasibility of behavioural treatments for depression has been renewed (Hopko 2003a; Dimidjian 2011). Jacobson 1996 showed that the behavioural component of cognitive‐behavioural therapy (CBT) was as effective as the full package of CBT, and investigators developed a new and more comprehensive model of behavioural activation that would be amenable to dissemination (Jacobson 2001). According to the updated clinical guidelines produced by the National Institute for Health and Clinical Excellence, behavioural activation (BA) is one of the recommended treatment options for moderate to major depressive disorder, along with cognitive‐behavioural therapy and IPT, although the guidelines acknowledge that evidence for BA is currently less robust (NICE 2009). In this and other recent systematic reviews, inclusion of a heterogeneous group of studies and studies using an 'extended' behavioural activation approach (eBA, regarded as a 'third wave' CBT intervention) limits interpretation of the findings (Cuijpers 2007; Ekers 2008).
A recent meta‐analysis of 17 randomised controlled trials (RCTs) comparing BT against controls or other psychological therapies suggested superior outcomes compared with supportive counselling and brief psychological therapy and equivalence between CBT and BT, in terms of depression recovery rates, symptom levels and participant dropout (Ekers 2008). However, inclusion of studies using eBA, together with inclusion of minimal contact computerised interventions, limits interpretation of these findings. An earlier meta‐analysis of 16 studies conducted by Cuijpers 2007 comprised a heterogeneous group of studies that included individuals with dementia and inpatient populations; this again makes interpretation of the findings difficult. Another systematic review of brief psychological therapies for depression (Churchill 2001) is now out of date.
As described in Description of the intervention, patients still prefer psychological therapies for the treatment of depression, and many different types of psychological therapies are available. Thus it is very important for clinicians to know whether any difference has been noted between psychological therapies in terms of efficacy or acceptability. Given the resurgence of interest in the use of BT as a cost‐effective intervention for depression that is potentially simpler to deliver (Kanter 2010) and easier to implement than other psychological therapy models, a comprehensive review of the comparative effectiveness and acceptability of BT interventions for depression is now timely to inform and update clinical practice and future clinical guideline development. This review forms part of a programme of 12 reviews covering BT, CBT, third wave CBT, psychodynamic therapies, humanistic therapies and integrative therapies, all compared with control conditions or with one another.
Objectives
To examine the effects of all BT approaches compared with all other psychological therapy approaches for acute depression.
To examine the effects of different BT approaches (behavioural therapy, behavioural activation, social skills training and relaxation training) compared with all other psychological therapy approaches for acute depression.
To examine the effects of all BT approaches compared with different psychological therapy approaches (CBT, third wave CBT, psychodynamic, humanistic and integrative psychological therapies) for acute depression.
Methods
Criteria for considering studies for this review
Types of studies
Methods used in our review were set out in a published protocol (Churchill 2010). Minor changes from this original protocol have been deemed necessary and implemented; their details are listed in the 'Differences between protocol and review' subsection below.
Randomised controlled trials (RCTs) were eligible for inclusion in this review. Trials employing a cross‐over design were included in the review (whilst it is acknowledged that this design is rarely used in psychological therapy trials), but only data from the first active treatment phase were used. Cluster RCTs were also eligible for inclusion.
Quasi‐randomised controlled trials, in which treatment assignment is decided through methods such as alternate days of the week, were not eligible for inclusion. Trials that replaced dropouts without randomisation were included only when the proportion of replaced participants was less than 20%.
Types of participants
Participant characteristics
Studies of men and women aged ≥ 18 years were included. A Cochrane review on psychotherapy for depression in children and adolescents (< 18 years) has been undertaken (Watanabe 2004). The increasing prevalence of memory decline (Ivnik 1992), cognitive impairment (Rait 2005) and multiple comorbid physical disorders/polypharmacy (Chen 2001) in individuals over 74 years may differentially influence the process and effect of psychological therapy interventions. Therefore, to ensure that older participants are appropriately represented in the review (Bayer 2000; McMurdo 2005), an upper age cut‐off of < 75 years was used (when a study may have included individuals ≥ 75, we included it so long as the average age was < 75). A previously published Cochrane review on psychotherapeutic treatments for older depressed people (Wilson 2008) is being updated concurrently by the review authors.
Setting
Studies could be conducted in a primary, secondary or community setting and included volunteers. Studies involving inpatients were excluded. Studies that focused on specific populations—nurses, care givers, depressed participants at a specific workplace—were included if all participants met the criteria for depression.
Diagnosis
We included all studies that focused on acute phase treatment of clinically diagnosed depression.
Studies adopting any standardised diagnostic criteria to define participants suffering from an acute phase unipolar depressive disorder were included. Accepted diagnostic criteria included Feighner criteria, Research Diagnostic Criteria and criteria of the Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM‐III) (APA 1980), DSM‐III‐Revised (R) (APA 1987),DSM‐Fourth Edition (IV) (APA 1994), DSM‐IV‐Text Revision (TR) (APA 2000) and International Classification of Diseases, Tenth Edition (ICD)‐10 (WHO 1992). Earlier studies may have used ICD‐Ninth Edition (9) (WHO 1978), but ICD‐9 is not based on operationalised criteria, so studies using ICD‐9 were excluded from this category.
Mild, moderate and severe depressive disorders are all included in primary care (Mitchell 2009; Rait 2009; Roca 2009). To fully represent the broad spectrum of severity of depressive symptoms encountered by healthcare professionals in primary care, studies that used non‐operationalised diagnostic criteria or a validated clinician or self‐report depression symptom questionnaire, such as the Hamilton Rating Scale for Depression (Hamilton 1960) or the Beck Depression Inventory (Beck 1961), to identify depression caseness as based on a recognised threshold, were included. However, it was planned to examine the influence of including this category of studies in a sensitivity analysis.
Accepted strategies for classifying mild, moderate and severe depression on the basis of criteria used in the evidence syntheses underpinning the NICE 2009 guidelines for depression were used when possible. NICE 2009 defines severity of depression in accordance with DSM‐IV as follows: mild depression: few, if any, symptoms in excess of the five required to make the diagnosis, with symptoms resulting in only minor functional impairment. Moderate depression: symptoms of functional impairment between 'mild' and 'severe'. Severe depression: most symptoms, and marked interference of the symptoms with functioning. Can occur with or without psychotic symptoms.
Studies focusing on chronic depression or treatment‐resistant depression (i.e. studies that list these conditions as inclusion criteria) were excluded from the review. Studies in which participants were receiving treatment to prevent relapse after a depressive episode (i.e. where participants were not depressed at study entry) were also excluded. Treatments for chronic depression and treatment‐resistant depression will be covered in separate Cochrane reviews.
Studies of people described as ‘at risk of suicide’ or with dysthymia or other affective disorders such as panic disorder were included if participants met the criteria for depression as stated above, but otherwise were excluded.
We did not include subgroup analyses of people with depression selected from people with mixed diagnoses because such studies would be susceptible to publication bias (the study authors reported such subgroup studies because the results were "interesting"). In other words, we included these studies only if the inclusion criteria for the entire study satisfied our eligibility criteria.
Comorbidity
Studies involving participants with comorbid physical or common mental disorders were eligible for inclusion as long as the comorbidity was not the focus of the study. In other words, we excluded studies that focused on depression among individuals with Parkinson's disease or after acute myocardial infarction but accepted studies that may have included some participants with Parkinson's disease or with acute myocardial infarction.
Types of interventions
Experimental interventions
We created the categories of BTs and the comparator on the basis of both treatment approach (e.g. their theoretical background and the manuals they used) and content (what therapeutic techniques they mainly used or what was their area of focus). BT approaches eligible for inclusion were grouped into four main subcategories, according to the specific therapeutic principles and techniques described by trial authors, as follows: behavioural therapy (based on the Lewinsohn model, which focuses on increasing pleasant activities), behavioural activation (originated from the behavioural component of cognitive‐behavioural therapy), social skills training/assertiveness training and relaxation therapy (see also Appendix 1).
Behavioural therapy (Lewinsohn)
Lewinsohn 1974 proposed that depressed individuals have low rates of pleasant activities and obtained pleasure, that their mood covaries with rates of pleasant and aversive activities, that their mood improves with increases in pleasant activities and that they lack social skills during the depressed phase. Therefore, behavioural therapy based on the approach developed by Lewinsohn and colleagues involves helping individuals increase their frequency and quality of pleasant activities, producing corresponding improvement in mood and overall quality of life (Lewinsohn 1974).
Behavioural activation (original model) (Jacobson)
The original model of behavioural activation (BA) developed by Jacobson 1996 was defined primarily by the proscription of cognitive interventions (Dimidjian 2006) and was tested in a dismantling study in which the behavioural activation component of cognitive therapy for depression was isolated (Beck 1979). On the basis of its original design, BA model components include increasing access to pleasant events and consequences, activity scheduling and developing social skills, thereby helping people to make contact with potentially reinforcing experiences (Jacobson 2001). No attempt is made to directly restructure cognitions.
Social skills training/assertiveness training
The social skills training model (SST) proposes that depressed people may have difficulty initiating, maintaining and ending conversations (Jackson 1985). Because of these deficits, the individual is unable to elicit mutually reinforcing behaviour from other people in his or her environment. SST subsumes assertion and conversational skills, together with more specialised subskills such as dating and job interview skills. Four social contexts of interacting with strangers— friends, family members and people at work and school—are targeted (Bellack 1980), and interventions such as instruction, modelling, rehearsal, feedback and reinforcement are used to enable the development of new responses (Jackson 1985). As assertiveness training represents a key component of SST, it was included in the SST category.
Relaxation therapy
Relaxation training is a behavioural stress management technique that induces a relaxation response, helping to switch off the fight/flight response and causing levels of stress hormones in the bloodstream to fall. A variety of techniques may be used to induce relaxation, the most common of which is Jacobson's progressive muscle relaxation training (Bernstein 1973).
Other behavioural therapies
For studies evaluating a behavioural therapy intervention not listed above, a post hoc decision was made about their inclusion in the review. The impact of their inclusion was examined in a sensitivity analysis (see Methods section).
Format of psychological therapies
Psychological therapies that were provided wholly by telephone or over the Internet were not eligible for inclusion. Interventions in which face‐to‐face therapy was augmented by telephone‐ or Internet‐based support but in which most psychotherapy sessions were provided through face‐to‐face interviews were included in the review. On the other hand, guided self‐help, in which the practitioner provided only brief face‐to‐face non‐therapeutic support to participants who were using a self‐help psychological therapy intervention, was excluded, as were bibliotherapy and writing therapies.
Psychological therapies conducted on an individual or group basis were eligible for inclusion.
The number of sessions was not limited, and we accepted psychological therapies delivered in only one session.
Comparators
The comparator intervention consisted of all other types of psychological therapies, categorised as CBT, third wave CBT, psychodynamic, humanistic and integrative approaches. We categorised each type of psychological therapy into several subcategories, according to the specific therapeutic principles and techniques applied, but here we have listed only the names of these subcategories within each category. Details of classification of subcategories will be described in upcoming companion reviews (see also Appendix 1).
Cognitive‐behavioural therapies (CBTs)
In cognitive‐behavioural therapy, therapists aim to work collaboratively with patients to understand the link between thoughts, feelings and behaviours, and to identify and modify unhelpful thinking patterns, underlying assumptions and idiosyncratic cognitive schemata about the self, others and the world (Beck 1979). Cognitive change methods for depression are targeted at the automatic thought level in the first instance and include thought catching, reality testing and task assigning as well as generating alternative strategies (Williams 1997). Behavioural experiments are then used to re‐evaluate underlying beliefs and assumptions (Bennett‐Levy 2004). We categorised these therapies into six subcategories: cognitive therapy, rational emotive behaviour therapy, problem‐solving therapy, self‐control therapy, a coping with depression course and other cognitive‐behavioural therapies.
'Third wave' cognitive and behavioural therapies (third wave CBTs)
Third wave CBT approaches conceptualise cognitive thought processes as a form of 'private behaviour' (Hayes 2006; Hofmann 2008). Third wave CBTs target the individual's relationship with cognitions and emotions, focusing primarily on the function of cognitions, such as thought suppression or experiential avoidance (an attempt or desire to suppress unwanted internal experiences, such as emotions, thoughts and bodily sensations) (Hofmann 2008). A range of strategies, including mindfulness exercises, acceptance of unwanted thoughts and feelings and cognitive diffusion (stepping back and seeing thoughts as just thoughts), are used to bring about change in the thinking process. Drawing from psychodynamic and humanistic principles, third wave CBT approaches place great emphasis on use of the therapeutic relationship. We categorised these therapies into eight subcategories: acceptance and commitment therapy, compassionate mind training, functional analytic psychotherapy, extended behavioural activation, metacognitive therapy, mindfulness‐based cognitive therapy, dialectical behaviour therapy and other third wave CBTs.
Psychodynamic therapies
Grounded in psychoanalytic theory (Freud 1949), psychodynamic therapy (PD) uses the therapeutic relationship to explore and resolve unconscious conflict through transference and interpretation, with development of insight and circumscribed character change as therapeutic goals, and relief of symptoms as an indirect outcome. Brief therapy models have been devised by Malan 1963, Mann 1973 and Strupp 1984. We categorised these therapies into four subcategories: drive/structural model (Freud), relational model (Strupp, Luborsky), integrative analytic model (Mann) and other psychodynamic therapies.
Humanistic therapies
Contemporary models of humanistic therapies differ from one another somewhat in clinical approach, but all focus attention on the therapeutic relationship (Cain 2002), within which therapist ‘core conditions’ of empathy, genuineness and unconditional positive regard (Rogers 1951) are regarded as cornerstones for facilitating client insight and change. We categorised these therapies into seven subcategories: person‐centred therapy (Rogerian), gestalt therapy, experiential therapies, transactional analysis, existential therapy, non‐directive/supportive therapies and other humanistic therapies.
Interpersonal, cognitive analytic and other integrative therapies
Integrative therapies are approaches that combine components of different psychological therapy models. Integrative therapy models include interpersonal therapy (IPT) (Klerman 1984), cognitive analytic therapy (CAT) (Ryle 1990) and Hobson’s conversational model (Hobson 1985), manualised as psychodynamic interpersonal therapy (Shapiro 1990). With its focus on the interpersonal context, IPT was developed to specify what was thought to be a set of helpful procedures commonly used in psychotherapy for depressed outpatients (Weissman 2007), drawing in part from attachment theory (Bowlby 1980) and cognitive‐behavioural therapy (isIPT [ND]) within a time‐limited framework. CAT, also devised as a time‐limited psychotherapy, integrates components from cognitive and psychodynamic approaches. The conversational model integrates psychodynamic, interpersonal and person‐centred model components.
Counselling interventions traditionally draw from a wide range of psychological therapy models, including person‐centred, psychodynamic and cognitive‐behavioural approaches, applied integratively, according to the theoretical orientation of practitioners (Stiles 2008). Therefore, studies of counselling usually will be included in the integrative therapies reviews. However, if the counselling intervention consists of a single discrete psychological therapy approach, it will be categorised as such, even if the intervention is referred to as 'counselling'. If the intervention is manualised, this will inform our classification. We categorised these therapies into seven subcategories: interpersonal therapy, cognitive‐analytic therapy, psychodynamic‐interpersonal therapy, cognitive‐behavioural analysis system of psychotherapy, counselling, motivational interviewing and other integrative therapy approaches.
Excluded interventions
The behavioural activation approach has been extended (Jacobson 2001; Martell 2001) by the introduction of contextual and idiosyncratic functional analysis into the assessment and treatment of depression. The extended behavioural activation approach (eBA) is regarded as a third wave CBT; therefore, for the purposes of this review, eBA was categorised as a comparator third wave CBT intervention (Hunot 2010).
Studies of long‐term, continuation or maintenance therapy interventions designed to prevent relapse of depression or to treat chronic depressive disorders were excluded from the review. Similarly, studies of interventions designed to prevent a future episode of depression were excluded.
Studies of dual modality treatments, in which participants are randomly assigned to receive a combination of psychological and pharmacological treatments concurrently, were included in the review only if the study of interest compared two psychological models and both groups were prescribed the same concomitant pharmacological/placebo intervention. Otherwise, these studies were excluded from the current review and will be examined in a separate programme of reviews on combination treatments for depression.
Component or dismantling studies, in which the effectiveness of individual components of a behavioural therapeutic approach were investigated, were not included. Only such arms as were constructed as stand‐alone treatments were eligible for the present review.
Psychological therapy models based on social constructionist principles (that focus on the ways in which individuals and groups participate in the construction of their perceived social reality), including couples therapy, family therapy, solution‐focused therapy (de Shazer 1988), narrative therapy, personal construct therapy, neuro‐linguistic programming and brief problem solving (Watzlavick 1974), were excluded. These therapies work with patterns and dynamics of relating within and between family, social and cultural systems to create a socially constructed framework of ideas (O'Connell 2007), rather than focusing on an individual's reality. Previously published Cochrane reviews on couples therapy for depression (Barbato 2006) and family therapy for depression (Henken 2007) will be updated concurrently.
When the description of a suggested intervention did not meet the inclusion criteria for an active psychological therapy approach, that study/study arm was excluded from the review. If the intervention involved significant time spent with participants, the review team made a post hoc decision about whether it should be included as a psychological or an attentional placebo control in a linked review on BT versus control conditions for depression.
Types of outcome measures
Primary outcomes
1. Treatment efficacy: the number of participants who responded to treatment, as determined by changes in Beck Depression Inventory (BDI) (Beck 1961), Hamilton Rating Scale for Depression (HAM‐D) (Hamilton 1960) or Montgomery‐Asberg Depression Rating Scale (MADRS) (Montgomery 1979) scores, or in scores from any other validated depression scale. Many studies define response as 50% or greater reduction on BDI, HAM‐D, etc., with some studies defining response using Jacobson's Reliable Change Index; we accepted the study authors' original definition. If the original authors reported several outcomes corresponding with our definition of response, we gave preference for BDI as a self‐rating scale and for HAM‐D as an observer‐rating scale.
2. Treatment acceptability: the number of participants who dropped out of psychological therapy for any reason.
Secondary outcomes
3. The number of participants who remitted while receiving treatment, based on the endpoint absolute status of participants, as measured by the Beck Depression Inventory (BDI) (Beck 1961), the Hamilton Rating Scale for Depression (HAM‐D) (Hamilton 1960), the Montgomery‐Asberg Depression Rating Scale (MADRS) (Montgomery 1979) or any other validated depression scale. Examples of definitions of remission include 10 or less on BDI, 7 or less on HAM‐D and 10 or less on MADRS; we accepted the study authors' original definition. If the original authors reported several outcomes that corresponded with our definition of response, we gave preference to BDI as a self‐rating scale and to HAM‐D as an observer‐rating scale.
4. Improvement in depression symptoms, based on a continuous outcome of group mean scores at the end of treatment using BDI, HAM‐D, MADRS or any other validated depression scale.
5. Improvement in overall symptoms, as determined by using the Clinical Global Impressions scale (CGI) (Guy 1976).
6. Improvement in anxiety symptoms, as measured using a validated continuous scale, either assessor‐rated, such as the Hamilton Anxiety Scale (HAM‐A) (Hamilton 1959), or self‐report, including the Trait subscale of the Spielberger State‐Trait Anxiety Inventory (STAI‐T) (Spielberger 1983) and the Beck Anxiety Inventory (BAI) (Beck 1988).
7. Adverse effects, such as completed suicides, attempted suicides and worsening of symptoms, when reported, were summarised in narrative form.
8. Social adjustment and social functioning, including Global Assessment of Function (Luborsky 1962) scores, when reported, were summarised in narrative form.
9. Quality of life, as assessed with the use of validated measures such as Short Form (SF)‐36 (Ware 1993), Health of the Nation Outcome Scales (HoNOS) (Wing 1994) and World Health Organization Quality of Life (WHOQOL) (WHO 1998), when reported, was summarised in narrative form.
10. Economic outcomes (e.g. days of work absence/ability to return to work, number of appointments with primary care physician, number of referrals to secondary services, use of additional treatments), when reported, were summarised in narrative form.
Search methods for identification of studies
This review is one in a programme of 12 reviews. We ran one search (detailed below) to identify studies relevant to all 12 linked reviews. From these search results three reviewers (RC,VH and TAF) then allocated studies to the individual reviews.
No language restrictions were applied.
Electronic searches
The Cochrane, Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR)
We searched two clinical trials registers created and maintained by the Cochrane Depression, Anxiety and Neurosis Group (CCDAN)—the CCDANCTR‐Studies Register and the CCDANCTR‐References Register—in June 2010, and updated searches were carried out in April 2011 and February 2012 (Register up to date as of January 2012), using an extensive list of search terms for a programme of reviews on all psychological therapies for depression. An updated search restricting to search terms relevant to behavioural therapies was conducted in July 2013 (Appendix 2).
References to trials for inclusion in the Group's registers were collated from routine (weekly) searches of MEDLINE, EMBASE and PsycINFO and quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL). These searches employed generic terms for depression, anxiety and neuroses, together with sensitive (database‐specific) RCT filters. Details of CCDAN's generic search strategies can be found on the Group‘s website.
CCDANCTR‐Studies Register
The CCDANCTR‐Studies Register contains more than 11,000 trials for the treatment or prevention of depression, anxiety and neurosis. Each trial has been coded using the EU‐Psi coding manual (as a guide) and includes information on intervention, condition, comorbidities, age, treatment setting, etc.
The studies register was searched using the following search terms:
Condition = (depress* or dysthymi*) and Intervention = (*therap* or training)
CCDANCTR‐References Register
The CCDANCTR‐References Register contains bibliographic records of reports of trials coded in the CCDANCTR‐Studies Register, together with several other uncoded references (total number of records > 31,500). This register was searched using a comprehensive list of terms for ‘psychotherapies’, as indicated in Appendix 3. Records already retrieved from the search of the CCDANCTR‐Studies Register were de‐duplicated.
CINAHL and PSYNDEX
In addition to CCDANCTR, we searched CINAHL May 2010 and PSYNDEX in June 2010 as indicated in Appendix 4; Appendix 5.
No restriction on date, language or publication status was applied to the searches.
ClinicalTrials.gov
ClinicalTrials.gov was searched (July 2013) using advanced search and Age = Adults (18‐65) or Senior (66+); Study Type = Interventional; Condition = (depression or depressive or depressed or MDD); and Intervention = (behavior or behaviour or behavioral or behavioural).
Searching other resources
Reference lists
The references of all selected studies were searched for more published reports and citations of unpublished studies. Relevant review papers were checked.
Personal communication
Subject experts were contacted to check that all relevant studies, published and unpublished, had been considered for inclusion.
Data collection and analysis
Selection of studies
Two review authors (RC, VH) examined the abstracts of all publications obtained through the search strategy. Full articles of all studies identified by either of the review authors were then obtained and inspected by the same two review authors to identify trials meeting the following criteria.
Randomised controlled trial.
Participants had depression diagnosed by operationalised criteria.
Any BT approach (behavioural therapy, behavioural activation, social skills training and relaxation training) compared with any other psychological therapy approach.
Conflicts of opinion regarding eligibility of a study were discussed with a third review author after the full paper had been retrieved and consultation with the study authors sought, if necessary, until consensus was reached. External subject or methodological experts were consulted as necessary.
Data extraction and management
Data from each study were extracted independently by at least three review authors. Any disagreement was discussed with an additional review author, and, when necessary, the authors of the studies were contacted for further information.
Information related to study population, sample size, interventions, comparators, potential biases in the conduct of the trial, outcomes including adverse events, follow‐up and methods of statistical analysis was abstracted from the original reports into specially designed paper forms and then was entered onto a spreadsheet.
Management of time points
We had planned to summarise and categorise post‐treatment outcomes and outcomes at each reported follow‐up point as follows: short term (up to 6 months post‐treatment), medium term (7 to 12 months post‐treatment) and long term (longer than 12 months). However, because no study adequately reported follow‐up outcomes at longer than six months post‐treatment, we performed analyses only for short‐term outcomes.
Assessment of risk of bias in included studies
Risk of bias was assessed for each included study using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2008). The following five domains were considered.
Sequence generation: Was the allocation sequence adequately generated?
Allocation concealment: Was allocation adequately concealed, or was it based on a validated rating scale?
Blinding of participants, personnel and outcome assessors for each main outcome or class of outcomes: Was knowledge of the allocated treatment adequately prevented during the study?
Incomplete outcome data for each main outcome or class of outcomes: Were incomplete outcome data adequately addressed?
Selective outcome reporting: Are reports of the study free of any suggestion of selective outcome reporting?
In addition, the following risks of bias specific to psychological therapy trials were systematically appraised.
Therapist qualification/training: Are the therapists qualified to deliver psychological therapy, and have they received specialist training for the intervention they are providing?
Treatment fidelity: Was the therapy monitored against a manual or a scale through audiotapes or videotapes?
Researcher allegiance/Conflict of interest: Did the researcher have a vested interest for or against the therapies under examination?
Therapist allegiance/Conflict of interest: Did the therapist have a vested interest for or against the therapies provided?
Other sources of bias: Was the study apparently free of other problems that could put it at high risk of bias?
A description of what was reported to have happened in each study was recorded, and a judgement on the risk of bias was made for each domain within and across studies, based on the following three categories.
Low risk of bias.
Unclear risk of bias.
High risk of bias.
Two review authors independently assessed the risk of bias in selected studies. Any disagreement was discussed with a third review author. Where necessary, study authors were contacted for further information. All risk of bias data were presented graphically and described in the text. Allocation concealment was used as a marker of trial quality for the purpose of undertaking sensitivity analyses.
Measures of treatment effect
Continuous outcomes
Where studies used the same outcome measure for comparison, data were pooled by calculating the mean difference (MD). When different measures were used to assess the same outcome, data were pooled with standardised mean difference (SMD) and 95% confidence intervals (95% CIs) calculated.
Dichotomous outcomes
These outcomes were analysed by calculating a pooled odds ratio (OR) and 95% CIs for each comparison. Because ORs can be difficult to interpret, these pooled ORs were converted to risk ratios (RRs) using the formula provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008a) and were presented in this form for ease of interpretation.
Unit of analysis issues
Cluster‐randomised trials
Cluster‐randomised trials were to be included as long as proper adjustment for the intracluster correlation could be conducted in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
Cross‐over trials
Trials employing a cross‐over design were to be included in the review, but only data from the first active treatment phase were used.
Studies with multiple treatment groups
Multiple‐arm studies (those with greater than two intervention arms) can pose analytical problems in pair‐wise meta‐analysis. For studies with more than two relevant active treatment arms, data were managed in this review as follows.
Continuous data
Means, SDs and numbers of participants for all active treatment groups were pooled across treatment arms as a function of the number of participants in each arm to be compared against the control group (Law 2003; Higgins 2008;Higgins 2008a).
Dichotomous data
Data from relevant active intervention arms were collapsed into a single arm for comparison, or data from relevant active intervention arms were split equally between comparator arms.
Dealing with missing data
Missing dichotomous data were managed through intention‐to‐treat (ITT) analysis, in which it was assumed that participants who dropped out after randomisation had a negative outcome. It was also planned to conduct best/worse case scenarios for the clinical response outcome, in which it would be assumed that dropouts in the active treatment group had positive outcomes and those in the control group had negative outcomes (best case scenario), and that dropouts in the active treatment group had negative outcomes and those in the control group had positive outcomes (worst case scenario), thus providing boundaries for the observed treatment effect. If a large amount of information was missing, these best/worst case scenarios were to be given greater emphasis in the presentation of results.
Missing continuous data were analysed on an endpoint basis, including only participants with a final assessment, or were analysed by using the last observation carried forward to the final assessment (LOCF), if LOCF data were reported by the trial authors. When standard deviations (SDs) were missing, attempts were made to obtain these data by contacting trial authors. When SDs were not available from trial authors, they were calculated from P values, t‐values, confidence intervals or standard errors, if these were reported in the articles (Deeks 1997). When SDs were missing, attempts were made to obtain these data by contacting trial authors.
When a vast majority of actual SDs were available and only a minority of SDs were unavailable or unobtainable, it was planned to use a method for imputing SDs and calculating percentage responders; the method devised by Furukawa and colleagues (Furukawa 2005; Furukawa 2006; da Costa 2012) was used. If this method was employed, data would be interpreted with caution and the degree of observed heterogeneity would be taken into account. A sensitivity analysis would also be undertaken to examine the effect of the decision to use imputed data.
When additional figures were not available or obtainable and it was not deemed appropriate to use the Furukawa method as described above, the study data were not included in the comparison of interest.
Assessment of heterogeneity
Statistical heterogeneity was formally tested using the Chi2 test, which provides evidence of variation in effect estimates beyond that of chance. Because the Chi2 test has low power to assess heterogeneity when a small number of participants or trials are included, the P value was conservatively set at 0.1. Heterogeneity was also quantified using the I2 statistic, which calculated the percentage of variability due to heterogeneity rather than to chance. We expected, a priori, that considerable clinical heterogeneity would be noted between studies, and so I2 values in the range of 50% to 90% were considered to represent substantial statistical heterogeneity and were to be explored further. However, the importance of the observed I2 depended on the magnitude and direction of treatment effects and the strength of evidence for heterogeneity (Higgins 2003; Deeks 2008). Forest plots generated in RevMan 5 now provide an estimate of tau2, the between‐study variance in a random‐effects meta‐analysis. To provide an indication of the spread of true intervention effects, we also used the tau2 estimate to determine an approximate range of intervention effects using the method outlined in Section 9.5.4 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2008). This was to be done only for the primary outcomes.
Assessment of reporting biases
As far as possible, the impact of reporting biases was minimised by undertaking comprehensive searches of multiple sources (including trial registries), increasing efforts to identify unpublished material and including non–English language publications.
We also tried to identify outcome reporting bias in trials by recording all trial outcomes, planned and reported, and noting where outcomes were missing. When we found evidence of missing outcomes, we attempted to obtain any available data directly from the authors.
When sufficient numbers of trials allowed for a meaningful analysis, funnel plots were constructed to establish the potential influence of reporting biases and small‐study effects.
Data synthesis
Given the potential heterogeneity of psychological therapy approaches for inclusion, together with the likelihood of differing secondary comorbid mental disorders in the population of interest, a random‐effects model was used in all analyses.
Subgroup analysis and investigation of heterogeneity
Clinical heterogeneity
We had planned to conduct the following subgroup analyses, but we could not perform some of them because of lack of data.
Baseline depression severity: The severity of depression on entry into the trial was expected to have an impact on outcomes. We had planned to categorise baseline severity as mild, moderate or severe. However, we did not conduct this analysis because baseline depression severity was categorised as moderate in most of the studies, and this analysis was not meaningful.
Number of sessions: Differences in the numbers of therapy sessions received were likely, and this was expected to affect treatment outcomes. We had planned subgroup analysis according to the numbers of therapy sessions (1 to 7, 8 to 12, 13 to 20, more than 20). However, because included studies were too few, we conducted sensitivity analysis only by excluding studies in which the number of sessions was greater than 12.
Type of comparison: The type of comparator used was likely to influence the observed effectiveness of the intervention. We had planned subgroup analyses about subtype comparisons. However, only two subtype comparisons included more than one study (BT‐Lewinsohn vs CBT‐Cogntive therapy and BT‐SST/assertion vs CBT‐Self‐control).
Strength of therapeutic alliance/perceived therapist empathy based on validated measures such as the Barrett‐Lennard Relationship Inventory (Barrett‐Lennard 1986) or the Working Alliance Inventory (Horvath 1986): We did not conduct this analysis because of lack of available data.
Sensitivity analysis
Fidelity to treatment: Studies that did not assess fidelity to the psychological therapy model(s) under evaluation through assessment of audiotapes or videotapes of therapy sessions were excluded.
Study quality: Allocation concealment was to be used as a marker of trial quality. We planned to conduct sensitivity analysis excluding studies that did not use allocation concealment. However, we did not do so because no study reported how allocation concealment was ensured.
Trials for which missing data were imputed were excluded.
Trials that included the use of antidepressant treatment (naturalistic use; combination treatment used in both psychological therapy arms) were excluded.
Trials included in the review after post hoc decisions were made about their eligibility as behavioural therapeutic approaches were excluded.
Trials in which dropouts were replaced without randomisation were excluded.
Results
Description of studies
Results of the search
See Figure 1. We conducted a search for all psychological therapies in January 2012. After removing duplicates, we identified 6710 records relevant to this review or to the reviews of all psychological therapies for treating depression in adults. We excluded 6524 records on the basis of titles and abstracts and read 186 full text studies to assess for eligibility. A total of 122 studies were judged eligible for inclusion in this review or the reviews of all psychological therapies. Of those 122 studies, 30 studies had BT arms, but 5 studies were not included in this review because they compared BT with control conditions only. Finally 25 studies were included in this review.
1.
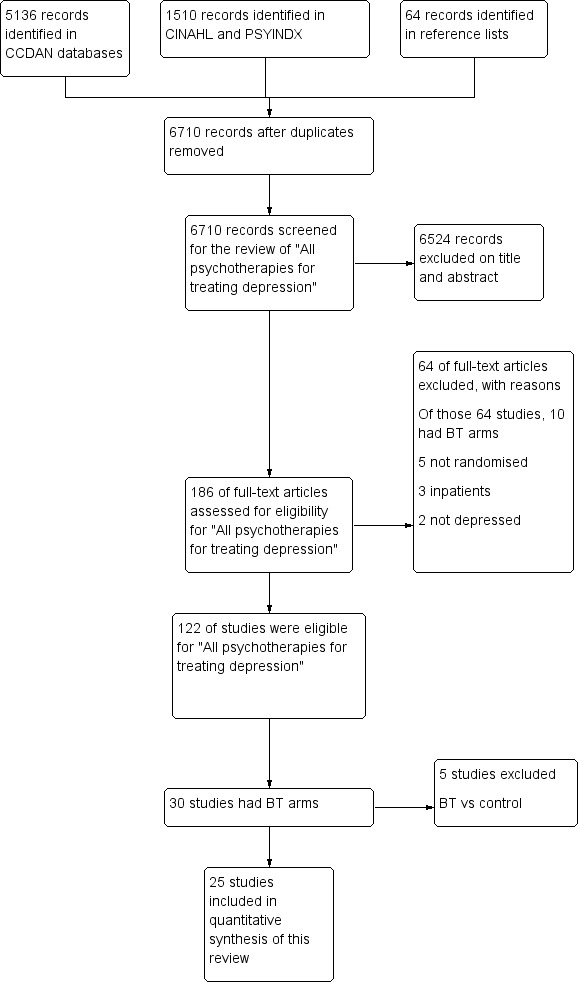
Study flow diagram.
In July 2013 we updated the searches while restricting to search terms relevant to behavioural therapies only (CCDANCTR to 31/07/13). A total of 632 new references were identified. On the basis of the information provided in abstracts, four potentially relevant studies were noted; however, on retrieving the full text papers, we found none of the studies to be eligible.
In July 2013 we also searched ClinicalTrials.gov. A total of 186 references were identified, of which five were potentially relevant studies; however, on retrieving the full text papers, we found none of the studies to be eligible.
We tried to contact 13 trial authors for missing information; seven responded, three of whom provided the desired information (Gardner 1981; Rehm 1979; Taylor 1977).
Included studies
Design
We had planned to include randomised controlled trials (RCTs), cluster RCTs and cross‐over design trials.
Twenty‐two of the included 25 studies had a parallel‐group, individually randomised design. One study (Lapointe 1980) had a parallel‐group cluster‐randomised design. But these studies did not adequately report outcomes. One study (Rude 1986) had a cluster‐randomised cross‐over design, and one study (Kelly 1983) had an individually randomised cross‐over design; in this case, only data from the first half of the trial were used. Two studies (Breckenridge 1985; Wilson 1982) replaced the dropouts.
Sample size
The sample sizes per arm were small in the great majority of the studies. Of 25 included studies, six studies did not report the numbers of participants randomly assigned at baseline. In all, 11 studies recruited fewer than 10 participants per arm, and six studies recruited 10 to 20 participants per arm. Only two studies recruited 30 or more participants to each arm (Bellack 1981; Rehm 1984).
Setting
In seven studies, the setting was unclear. In 13 studies, non‐medical university settings such as university departments of psychology were reported. In five studies, the setting was a secondary/tertiary care or other medical setting.
Eighteen of 25 studies were carried out in the USA. Other studies were carried out in Australia (three), Spain (two), Greece (one) and Canada (one).
Participants
Proportion of women
Three studies did not report the number of female participants. Seven studies recruited only women. The proportion of females among all participants ranged between 56% and 80% in the remaining 15 studies.
Age
Seven studies did not provide the mean age of participants. The mean age was in the twenties in three studies, in the thirties in 11 studies, and in the forties in two studies. The remaining two studies (Breckenridge 1985; Gallagher 1979) recruited elderly individuals only, whose average age was in the sixties.
Diagnosis
In eight studies, investigators stated that they used one of the following operationalised criteria: Research Diagnostic Criteria in four studies, DSM‐III in two studies, DSM‐III‐R in one study and Feighner criteria in one study. In most of the other studies, a depression symptom questionnaire was used to identify depression.
Eight studies reported that they enrolled only participants with a diagnosis of major depressive disorder. Other studies reported that they recruited participants with dysthymia or depressive disorder not otherwise specified, in addition to major depression, or they just stated that participants had a diagnosis of "depression".
Baseline severity of depression was reported on the basis of BDI in 21 studies, the Zung Self‐Rating Scale in two studies and the Minnesota Multiphasic Personality Inventory (MMPI) in one study. One study did not report baseline severity. Of 21 studies that used BDI, the severity of depression was classified as mild in one study, moderate in 16 studies and severe in four studies, in accordance with the following rules of thumb for interpretation of BDI: scores 0 to 13 minimal, 14 to 19 mild, 20 to 28 moderate and 29 to 63 severe (Beck 1996; Steer RA 2001).
Intervention
As described in the Methods section, we classified BT into five subcategories. The subcategories of BT in the included studies were as follows: behavioural therapy (Lewinsohn) in 11 studies (Breckenridge 1985; Comas‐Diaz 1981; Gallagher 1979; Kelly 1982; Kelly 1983; McNamara 1986; Padfield 1975; Shaw 1977; Skinner 1983; Taylor 1977; Wilson 1983), behavioural activation (Jacobson) in one study (Jacobson 1996), SST/assertion in eight studies (Bellack 1981; Lapointe 1980; Maldonado 1982; Maldonado 1984; Rehm 1979; Rude 1986; Sanchez 1980; Schmitt 1988), relaxation in two studies (Pace 1977; Wetzel 1992) and other behavioural therapies in two studies (Gardner 1981; Rehm 1984). The remaining study included both behavioural therapy (Lewinsohn) and SST/assertion (Zeiss 1979).
In slightly less than half of the included studies (10 of 25), the participants received group therapy, and in nearly half of the studies (12 of 25), they received individual therapy. Two studies did not report whether the therapy provided was group or individual treatment. One study compared group BT with individual humanistic therapy (Bellack 1981).
The duration of intervention ranged form 3.5 to 16 weeks, most often between one and three months.
The number of sessions varied among studies and ranged from 5 to 20: 1 to 7 sessions in 11 studies, 8 to 12 sessions in 10 studies and 13 to 20 sessions in 3 studies. One study did not report the number of sessions.
Eighteen studies provided follow‐up assessment, but some did not report the outcomes. The timing of follow‐up assessment varied among the studies (five weeks to 10 months)
Comparisons
Three studies compared BT with two comparator psychological therapies: two studies compared BT with CBT and psychodynamic therapies (Breckenridge 1985; Lapointe 1980), and one study compared BT with CBT and humanistic therapies (McNamara 1986).
A total of 22 studies compared BT with a single comparator psychological therapy: 17 studies compared BT with CBT, two studies compared BT with psychodynamic therapies, two studies compared BT with humanistic therapies and one study compared BT with integrative therapies. No study compared BT with third wave CBT.
Scale used to measure outcomes
BDI was the scale most frequently used to measure depressive symptoms; it was used in 22 studies. The second most often used scale was the Hamilton Rating Scale for Depression (HAM‐D), which was used in 12 studies. In almost half of the studies, investigators did not use a validated assessor‐rated scale. Only one study (Wetzel 1992) reported "response" as outcome based on the use of a validated scale.
Although five studies reported "remission" using the authors' definition, this definition was heterogeneous among studies. For example, the definition was "no major depressive disorder at posttest and BDI scores less than eight" in Jacobson 1996, and "a score of 11 or less on BDI" in Rehm 1979.
Excluded studies
We excluded 64 studies from this review and from the other reviews of all psychological therapies for depression, and 10 of those 64 studies had BT arms.
The reasons for exclusion of 10 studies were as follows: 5 studies did not randomise participants adequately (Bowers 1990; Gallagher 1982; Mclean 1979; Rokke 1999; Turner 1979), 3 studies recruited inpatients (Brand 1992; Hopko 2003b; Snarski 2011) and 2 studies appeared to include participants who did not have a diagnosis of depression (Losada 2011; Reynolds 2011). We excluded five studies because they compared BT only with control conditions (Barrera 1979; Broota 1990; Cullen 2002; Hayman 1980; Wilson 1982).
No studies for this review are awaiting classification or are ongoing.
Risk of bias in included studies
Please see Figure 2 for the 'Risk of bias' summary.
2.
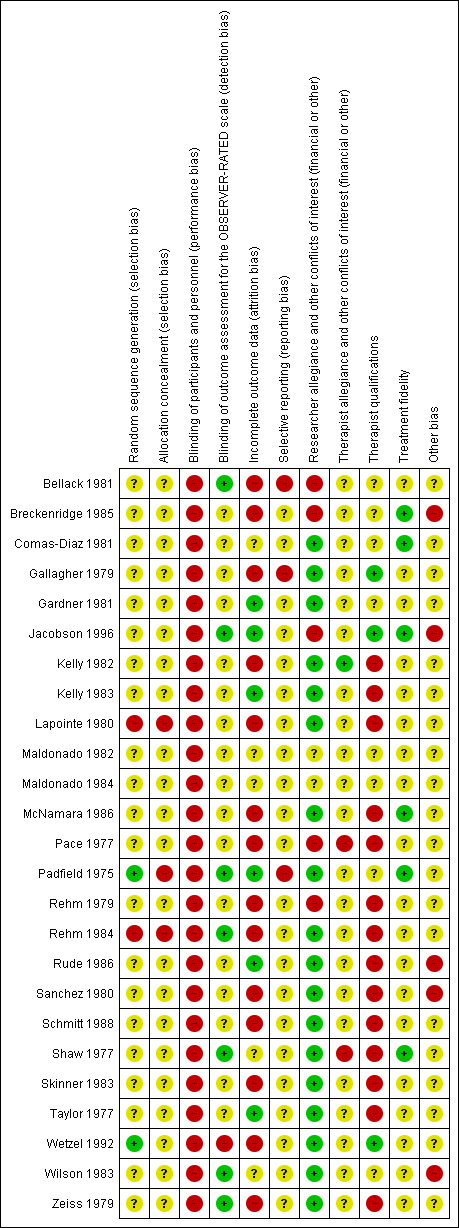
Risk of bias summary.
Allocation
No study reported how investigators had concealed the treatment allocation.
Blinding
As it is impossible to blind participants and therapists in psychological therapy trials, all studies were at high risk of performance bias.
Seven studies reported that outcome assessors were blind to the allocation of participants. However, we used BDI and other self‐rated scale scores for analysis because BDI was the most commonly used scale among the included studies. Therefore, a high risk of detection bias was determined for all studies. (In other words, we reasoned that pooled self‐rated scale scores would be easier to interpret than blinded observer‐rated scale scores mixed with non‐blinded observer‐rated scale scores and non‐blinded self‐rated scale scores.)
Incomplete outcome data
More than half of the studies were determined to be at high risk of bias because they analysed only completers, and the attrition rate was high or different between arms. One study (Gallagher 1979) did not report relevant outcomes. In some studies (Comas‐Diaz 1981; Lapointe 1980; McNamara 1986; Sanchez 1980; Shaw 1977; Zeiss 1979 ), continuous outcomes were reported without the numbers of participants assessed, and it was unclear how investigators dealt with incomplete outcome data.
Selective reporting
Two studies (Bellack 1981; Gallagher 1979) reported only a portion of the outcomes that they had measured. One study (Padfield 1975) reported that two suicide attempts took place during the time of study, but the allocated treatment arms of these participants were not stated. As no protocol was provided in the remaining studies, they were categorised as having unclear risk of bias.
Other potential sources of bias
Therapist qualifications/training
Most studies stated only that therapists had received specialist training and did not describe details of training in relation to time or to experiments reported. Therefore we were obliged to categorise a study as having low risk of bias when the study authors stated something about therapist training. Three studies were rated as having low risk of bias because the therapists were qualified and had received specific training for the treatment (Gallagher 1979; Jacobson 1996; Wetzel 1992). In more than half of the studies, the therapists were not qualified or had not received training (Kelly 1982; Kelly 1983;McNamara 1986Lapointe 1980; Pace 1977; Rehm 1979; Rehm 1984; Rude 1986; Sanchez 1980;Shaw 1977;Schmitt 1988;Skinner 1983; Taylor 1977; Zeiss 1979). In almost one‐third of studies, trial authors provided no information on therapist qualifications or training. Overall, we believed that most studies were at high risk of bias.
Treatment fidelity
We classified a study as having low risk of bias when therapy sessions were monitored through audiotapes or videotapes and when monitoring was performed against a manual or by using a scale. Only six studies satisfied these criteria (Breckenridge 1985; Comas‐Diaz 1981; Jacobson 1996; McNamara 1986; Padfield 1975; Shaw 1977). Almost three‐quarters of studies did not provide enough information on monitoring. Overall, we believed that most studies could be assigned a high risk of bias.
Researcher allegiance/conflict of interest
In more than half of the studies, no evidence indicated that the authors had any allegiance for or against one of the psychological therapies that they were studying. In some studies (Bellack 1981; Breckenridge 1985; Jacobson 1996; Rehm 1979), researchers developed the manual of therapy that they were studying, and it seemed that they had allegiance or vested interests in it. In Pace 1977, the author appears to have a specific interest in BT because the study article explicitly states that integrative therapy was set as the control.
Therapist allegiance/conflict of interest
Except for one study, the included studies did not confirm whether therapists had a vested interest in a specific treatment. In one study (Shaw 1977), therapists seemed to have allegiance for BT‐Lewinsohn's behavioural activation.
Other potential sources of bias
Other potential risks of bias varied among studies. Notably, several studies did not provide the numbers of participants originally randomly assigned to each arm. Two studies (Breckenridge 1985; Wilson 1982) supplemented for the dropouts by providing additional recruits, thus breaking randomisation.
The details are described in Characteristics of included studies.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. BT compared with all other psychological therapies for depression.
| BT compared with all other psychological therapies for depression | ||||||
| Participants or population: people with depression Settings: outpatient Intervention: BT Comparison: all other psychological therapies | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| All other psychological therapies | BT | |||||
| Response | 584 per 1000 | 567 per 1000 (503 to 637) | RR 0.97 (0.86 to 1.09) | 690 (18 studies) | ⊕⊕⊝⊝ lowa,b,c | The confidence interval crosses no difference |
| Remission | 554 per 1000 | 504 per 1000 (443 to 576) | RR 0.91 (0.8 to 1.04) | 694 (18 studies) | ⊕⊕⊝⊝ lowa,b,d | The confidence interval crosses no difference |
| Response at follow‐up Follow‐up: 5 to 24 weeks | 678 per 1000 | 522 per 1000 (400 to 685) | RR 0.77 (0.59 to 1.01) | 356 (9 studies) | ⊕⊕⊝⊝ lowa,b,e | The confidence interval crosses no difference |
| Depression severity | Mean depression severity in the intervention groups was 0.03 standard deviations lower (0.2 lower to 0.15 higher) | 656 (18 studies) | ⊕⊕⊕⊝ moderatea,b | SMD ‐0.03 (‐0.2 to 0.15). The confidence interval crosses no difference | ||
| Dropouts for any reason | 119 per 1000 | 122 per 1000 (78 to 192) | RR 1.02 (0.65 to 1.61) | 495 (15 studies) | ⊕⊕⊕⊝ moderatea,b | The confidence interval crosses no difference |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aAll studies were at unclear or high risk of bias in sequence generation and allocation concealment. bThe comparison groups were heterogeneous. cOnly one study reported this outcome, and we used imputed data in other studies. dBecause five studies reported this outcome, we used imputed data in other studies. eNo study reported this outcome; we used imputed data.
Summary of findings 2. BT compared with CBT for depression.
| BT compared with CBT for depression | ||||||
| Participants or population: people with depression Settings: outpatient Intervention: BT Comparison: CBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| CBT | BT | |||||
| Response | 632 per 1000 | 588 per 1000 (525 to 664) | RR 0.93 (0.83 to 1.05) | 544 (15 studies) | ⊕⊕⊝⊝ lowa,b,c | The confidence interval crosses no difference |
| Remission | 586 per 1000 | 510 per 1000 (439 to 586) | RR 0.87 (0.75 to 1) | 560 (16 studies) | ⊕⊕⊝⊝ lowa,c,d | The confidence interval crosses no difference |
| Response at follow‐up Follow‐up: 5 to 24 weeks | 698 per 1000 | 530 per 1000 (412 to 691) | RR 0.76 (0.59 to 0.99) | 344 (8 studies) | ⊕⊕⊝⊝ lowa,c,e | |
| Remission at follow‐up Follow‐up: 5 to 24 weeks | 659 per 1000 | 507 per 1000 (402 to 645) | RR 0.77 (0.61 to 0.98) | 344 (8 studies) | ⊕⊕⊝⊝ lowa,c,e | |
| Depression severity | Mean depression severity in the intervention groups was 0.06 standard deviations higher (0.12 lower to 0.23 higher) | 529 (15 studies) | ⊕⊕⊕⊝ moderatea,c | SMD 0.06 (‐0.12 to 0.23). The confidence interval crosses no difference | ||
| Dropouts for any reason | 64 per 1000 | 93 per 1000 (44 to 201) | RR 1.46 (0.68 to 3.14) | 363 (11 studies) | ⊕⊕⊕⊝ moderatea,c | The confidence interval crosses no difference |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aAll studies were at unclear or high risk of bias in sequence generation and allocation concealment. bOnly one study reported this outcome, and we used imputed data in other studies. cThe confidence interval is wide. dBecause four studies reported this outcome, we used imputed data in other studies. eNo study reported this outcome; we used imputed data.
Summary of findings 3. BT compared with psychodynamic therapies for depression.
| BT compared with psychodynamic therapies for depression | ||||||
| Participants or population: people with depression Settings: outpatients Intervention: BT Comparison: psychodynamic therapies | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Psychodynamic therapies | BT | |||||
| Response | 426 per 1000 | 529 per 1000 (358 to 776) | RR 1.24 (0.84 to 1.82) | 110 (2 studies) | ⊕⊕⊝⊝ lowa,b,c | The confidence interval crosses no difference |
| Remission | 377 per 1000 | 498 per 1000 (320 to 777) | RR 1.32 (0.85 to 2.06) | 110 (2 studies) | ⊕⊕⊝⊝ lowa,b,d | The confidence interval crosses no difference |
| Depression severity | Mean depression severity in the intervention groups was 0.37 standard deviations lower (0.79 lower to 0.05 higher) | 93 (2 studies) | ⊕⊕⊕⊝ moderatea,b | SMD ‐0.37 (‐0.79 to 0.05). The confidence interval crosses no difference | ||
| Dropouts for any reason | 298 per 1000 | 268 per 1000 (140 to 506) | RR 0.9 (0.47 to 1.7) | 96 (2 studies) | ⊕⊕⊕⊝ moderatea,b | The confidence interval crosses no difference |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aAll studies were at unclear or high risk of bias in sequence generation and allocation concealment. bThe confidence interval is wide. cNo study reported this outcome; we used imputed data. dOnly one study reported this outcome, and we used imputed data in other studies.
Comparison 1. BT versus all other psychological therapies
Primary outcomes
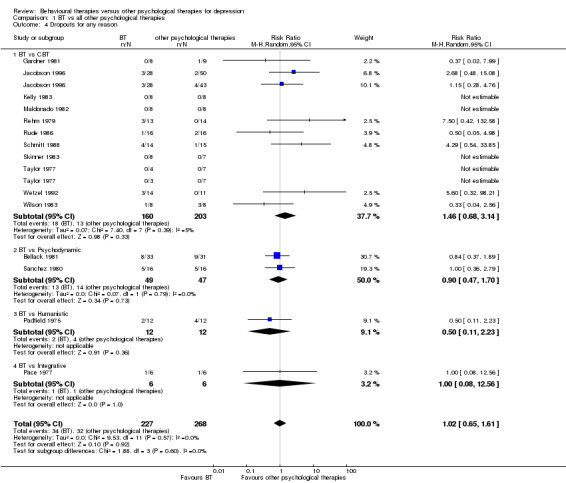
1.1 Treatment efficacy: response
Except for one study (Wetzel 1992), none of the included studies reported the number of participants who responded to treatment as based on a validated depression scale (50% or greater reduction on BDI, HAM‐D, MADRS, etc) or on the authors' original definition. After reviewing the protocol, we imputed response rates using the methods described in Dealing with missing data and analysed them in accordance with the intention‐to‐treat (ITT) principle. Two studies (Breckenridge 1985; Rehm 1984) did not report numbers of randomly assigned participants, and we conducted completer analyses for these studies. Three studies (Gardner 1981; Kelly 1983; Rehm 1979) did not report standard deviation (SD), so we borrowed SD from the other included studies by taking their weighted average.
In total, 18 of 25 studies that adequately reported outcomes were included in the analysis. We used response rate based on HAM‐D in 1 study (Wetzel 1992) and imputed response rate in 17 studies (in 15 studies on the basis of BDI and in 2 studies according to the Zung Self‐Rating Depression Scale). No evidence of significant difference between BT and all other psychological therapies was noted in terms of response rate (Figure 3, Analysis 1.1; 18 studies, 690 participants, risk ratio (RR) 0.97, 95% confidence interval (CI) 0.86 to 1.09, I2 = 0%).
3.
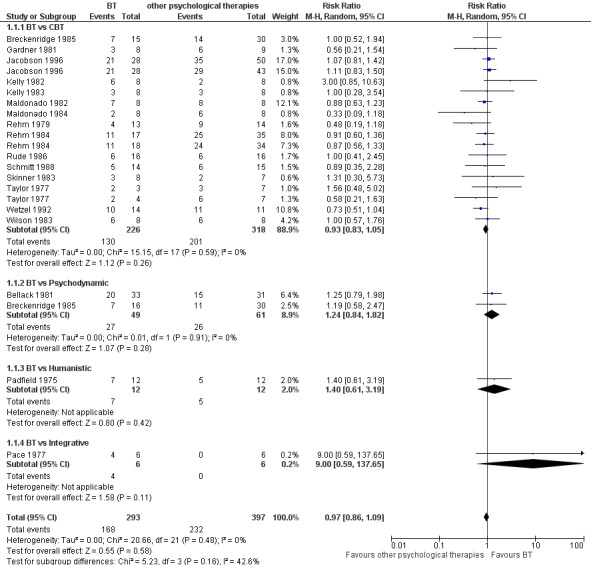
Forest plot of comparison: 1 BT vs all other psychological therapies, outcome: 1.1 Response.
1.1. Analysis.
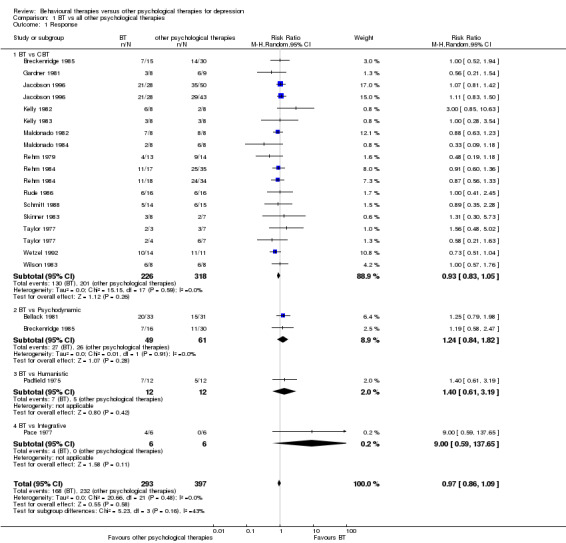
Comparison 1 BT vs all other psychological therapies, Outcome 1 Response.
1.2 Treatment acceptability: dropouts for any reason
For 15 studies, authors reported the number of dropouts. In four studies, dropout rates were not estimable because no dropout was reported for both arms. Analysis revealed no significant differences between BT and all other psychological therapies in terms of total dropout rates (Figure 4, Analysis 1.4; 15 studies, 495 participants, RR 1.02, 95% CI 0.65 to 1.61, I2 = 0%).
4.
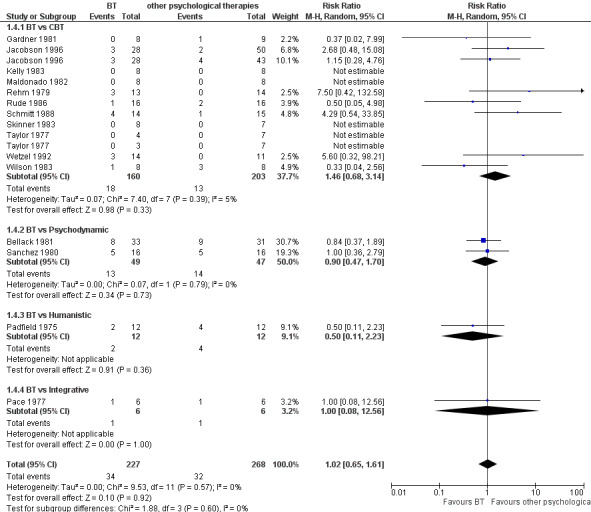
Forest plot of comparison: 1 BT vs all other psychological therapies, outcome: 1.4 Dropouts for any reason.
1.4. Analysis.
Comparison 1 BT vs all other psychological therapies, Outcome 4 Dropouts for any reason.
Secondary outcomes
1.3 Remission
Among 25 studies, 18 adequately reported outcomes and were included in the analysis. Five studies reported the numbers of participants who remitted at the end of the treatment as based on BDI or HAM‐D or on the authors' definitions. In accordance with the protocol, we imputed remission rates for the studies that reported only continuous outcomes. We basically abided by the ITT principle, but we conducted completer analyses for two studies (Breckenridge 1985; Rehm 1984) because investigators did not report the numbers of randomly assigned participants. Altogether, no significant difference was observed between BT and all other psychological therapies in terms of remission rate (Analysis 1.2; 18 studies, 694 participants, RR 0.91, 95% CI 0.80 to 1.04).
1.2. Analysis.
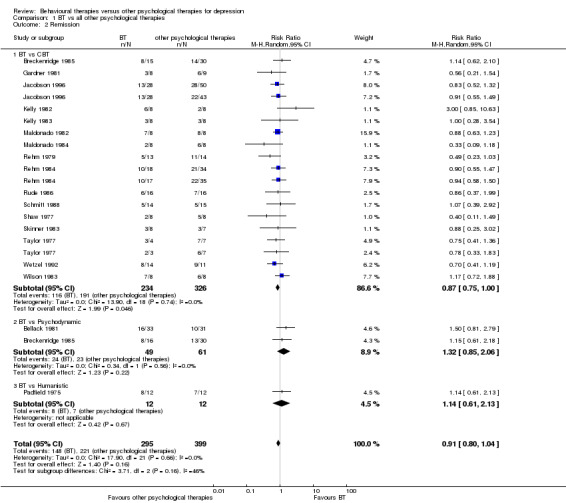
Comparison 1 BT vs all other psychological therapies, Outcome 2 Remission.
1.4 Severity of depression symptoms
Among 18 studies that reported continuous outcomes, we calculated the standardised mean difference using BDI in 16 studies and using the Zung Self‐Rating Depression Scale in 2 studies. Analysis revealed no significant differences between BT and all other psychological therapies in terms of severity of depression symptoms at the end of treatment (Analysis 1.3; 18 studies, 656 participants, SMD ‐0.03, 95% CI ‐0.20 to 0.15).
1.3. Analysis.
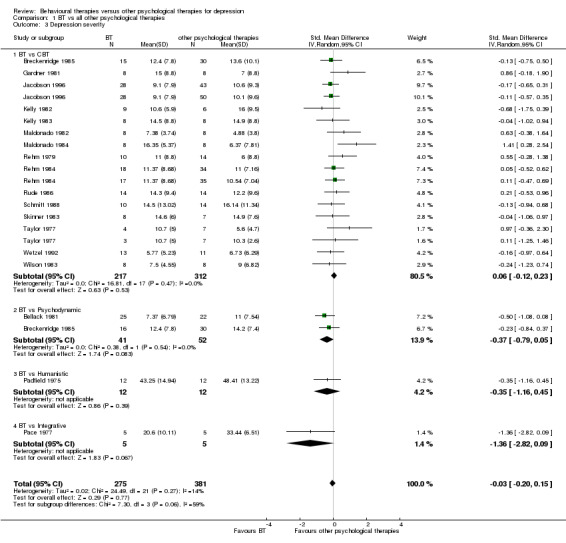
Comparison 1 BT vs all other psychological therapies, Outcome 3 Depression severity.
1.5 Improvement in overall symptoms
No relevant data were reported.
1.6 Anxiety symptoms
Among all included studies, two studies (Breckenridge 1985; Pace 1977) reported anxiety symptoms using a validated scale. Breckenridge 1985 compared BT with CBT and psychodynamic therapies using a brief symptom inventory. Pace 1977 compared BT with integrative therapies using anxiety state. Analysis revealed no evidence of significant differences between BT and other psychological therapies (CBT and psychodynamic and integrative therapies taken together) (Analysis 1.5).
1.5. Analysis.
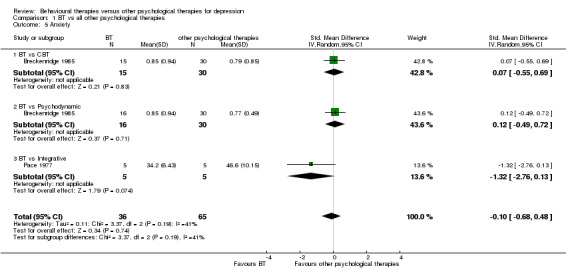
Comparison 1 BT vs all other psychological therapies, Outcome 5 Anxiety.
1.7 Adverse effects
No study provided reports of adverse effects.
1.8 Social adjustment
Among all included studies, two studies (Breckenridge 1985; Rehm 1984) reported social adjustment based on a social adjustment scale. Rehm 1984 compared BT with CBT, and Breckenridge 1985 compared BT with CBT and psychodynamic therapies. Analysis revealed no evidence of significant differences between BT and other psychological therapies (CBT and psychodynamic therapies taken together) (Analysis 1.6).
1.6. Analysis.
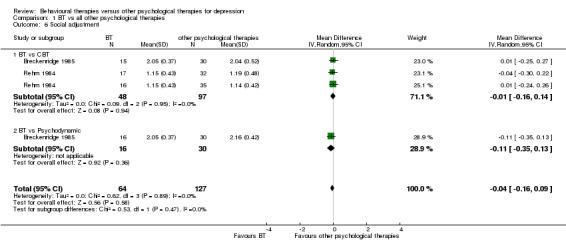
Comparison 1 BT vs all other psychological therapies, Outcome 6 Social adjustment.
1.9 Quality of life
No relevant data were reported.
1.10 Economic outcomes
No relevant data were reported.
Comparison 2. BT subcategories (Lewinsohn, Jacobson, SST/assertiveness, Relaxation) versus all other psychological therapies
2.1 BT‐Lewinsohn versus all other psychological therapies
Primary outcomes
2.1.1 Treatment efficacy: response
A total of 13 studies compared BT‐Lewinsohn with other psychological therapies, and eight studies adequately reported outcomes. Analysis revealed no evidence of significant differences in response rate between BT‐Lewinsohn and all other psychological therapies (Analysis 2.1; 8 studies, 303 participants, RR 1.00, 95% CI 0.82 to 1.23).
2.1. Analysis.
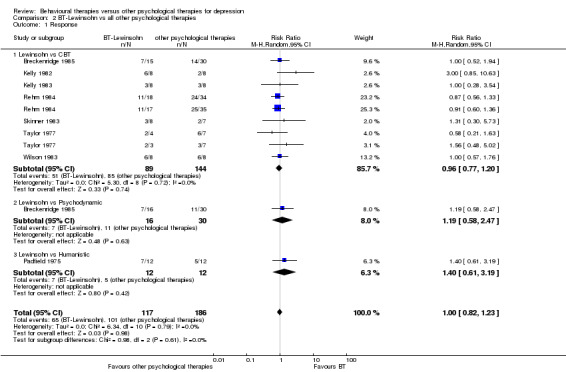
Comparison 2 BT‐Lewinsohn vs all other psychological therapies, Outcome 1 Response.
2.1.2 Treatment acceptability: dropouts for any reason
In 13 studies, BT‐Lewinsohn was compared with other psychological therapies, and five studies adequately reported outcomes. Analysis revealed no evidence of significant differences in acceptability between BT‐Lewinsohn and all other psychological therapies (Analysis 2.2; 5 studies, 92 participants, RR 0.43, 95% CI 0.13 to 1.45).
2.2. Analysis.
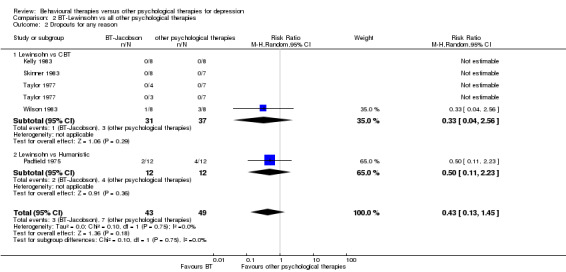
Comparison 2 BT‐Lewinsohn vs all other psychological therapies, Outcome 2 Dropouts for any reason.
2.2 BT‐Jacobson versus all other psychological therapies
Primary outcomes
2.2.1 Treatment efficacy: response
Only one study compared BT‐Jacobson with other psychological therapies (CBT). Analysis revealed no evidence of significant differences in response rate between BT‐Jacobson and CBT (Analysis 3.1; 1 study, 149 participants, RR 1.09, 95% CI 0.89 to 1.34).
3.1. Analysis.
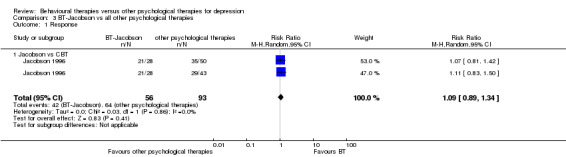
Comparison 3 BT‐Jacobson vs all other psychological therapies, Outcome 1 Response.
2.2.2 Treatment acceptability: dropouts for any reason
Only one study compared BT‐Jacobson with other psychological therapies (CBT). Analysis revealed no evidence of significant differences in acceptability between BT‐Jacobson and CBT (Analysis 3.2; 1 study, 149 participants, RR 1.62, 95% CI 0.54 to 4.85).
3.2. Analysis.
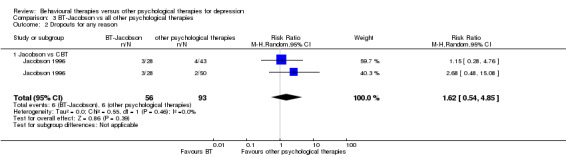
Comparison 3 BT‐Jacobson vs all other psychological therapies, Outcome 2 Dropouts for any reason.
2.3 BT‐SST/assertiveness versus all other psychological therapies
Primary outcomes
2.3.1 Treatment efficacy: response
Nine studies compared BT‐SST/assertiveness with other psychological therapies, and six studies adequately reported outcomes. Analysis revealed no evidence of significant differences in response rate between BT‐SST/assertiveness and all other psychological therapies (Analysis 4.1; 6 studies, 184 participants, RR 0.88, 95% CI 0.66 to 1.19).
4.1. Analysis.
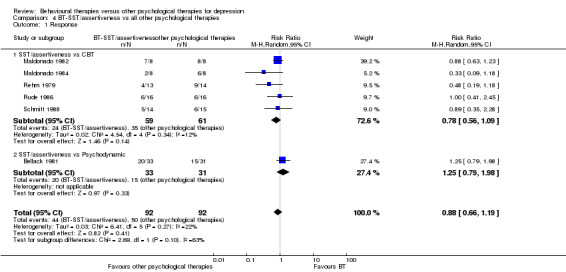
Comparison 4 BT‐SST/assertiveness vs all other psychological therapies, Outcome 1 Response.
2.3.2 Treatment acceptability: dropouts for any reason
In nine studies, investigators compared BT‐SST/assertiveness with other psychological therapies, and outcomes were adequately reported for six studies. Analysis revealed no evidence of significant differences in acceptability between BT‐SST/assertiveness and all other psychological therapies (Analysis 4.2; 6 studies, 200 participants, RR 1.11, 95% CI 0.58 to 2.12).
4.2. Analysis.
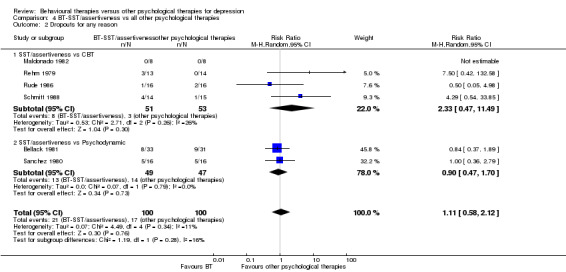
Comparison 4 BT‐SST/assertiveness vs all other psychological therapies, Outcome 2 Dropouts for any reason.
2.4 BT‐relaxation versus all other psychological therapies
Primary outcomes
2.4.1 Treatment efficacy: response
Two studies compared BT‐relaxation with all other psychological therapies. Analysis revealed no evidence of significant differences in response rate between BT‐relaxation and all other psychological therapies (Analysis 5.1; 2 studies, 37 participants, RR 2.12, 95% CI 0.07 to 64.37).
5.1. Analysis.
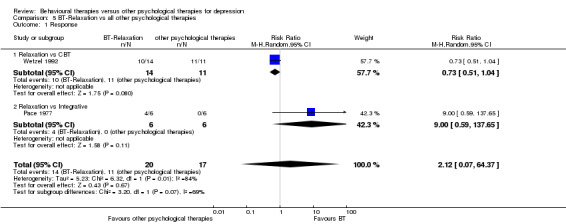
Comparison 5 BT‐Relaxation vs all other psychological therapies, Outcome 1 Response.
2.4.2 Treatment acceptability: dropouts for any reason
Two studies compared BT‐relaxation with all other psychological therapies. Analysis revealed no evidence of significant differences in acceptability between BT‐relaxation and all other psychological therapies (Analysis 5.2; 2 studies, 37 participants, RR 2.13, 95% CI 0.32 to 14.17).
5.2. Analysis.
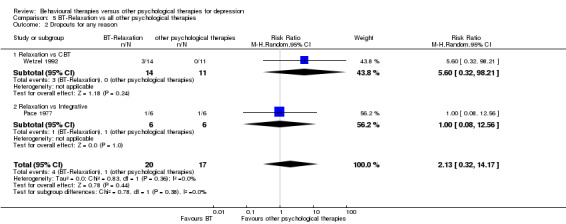
Comparison 5 BT‐Relaxation vs all other psychological therapies, Outcome 2 Dropouts for any reason.
Comparison 3. BT versus each psychological therapy (CBT, third wave CBT, psychodynamic, humanistic, integrative therapies)
3.1 BT versus CBT
Primary outcomes
3.1.1 Treatment efficacy: response
In 20 studies, investigators compared BT with CBT; five studies did not adequately report outcomes. One study (Wetzel 1992) reported "response" based on HAM‐D, but the remaining 14 studies reported only continuous outcomes. We imputed response rates of these 14 studies on the basis of BDI scores. In total, 15 studies were included in the analysis. Low‐quality evidence revealed better response to CBT than to BT (Figure 3, Analysis 1.1.1; 15 studies, 544 participants, RR 0.93, 95% CI 0.83 to 1.05).
3.1.2 Treatment acceptability: dropouts for any reason
Investigators in 11 studies compared BT with CBT and reported the number of dropouts. Analysis revealed no evidence of significant differences in acceptability between BT and CBT (Figure 4, Analysis 1.4.1; 11 studies, 363 participants, RR 1.46, 95% CI 0.68 to 3.14).
Secondary outcomes
3.1.3 Remission
A total of 20 studies compared BT with CBT, but four studies did not adequately report outcomes. Four studies (Shaw 1977; Jacobson 1996; Rehm 1979; Wetzel 1992) reported remission rates based on the authors' definition. For the remaining 12 studies, we imputed remission rates based on BDI. In total, 16 studies were included in the analysis. Analysis revealed no evidence of significant differences in response rates between BT and CBT (Analysis 1.2.1, 16 studies, 560 participants, RR 0.87, 95% CI 0.75 to 1.00).
3.1.4 Severity of depression symptoms
A total of 15 studies compared BT with CBT on the basis of BDI. Analysis revealed no evidence of significant differences between BT and CBT (Analysis 1.3.1; 15 studies, 529 participants, SMD 0.06, 95% CI ‐0.12 to 0.23).
3.1.5 Improvement in overall symptoms
No data were reported.
3.1.6 Anxiety symptoms
One study (Breckenridge 1985) compared BT with CBT and psychodynamic therapies and reported anxiety symptoms based on a brief symptom Inventory. Analysis revealed no evidence of significant differences when BT was compared with CBT (Analysis 1.5.1).
3.1.7 Adverse effects
No study provided reports of adverse effects.
3.1.8 Social adjustment
Two studies (Breckenridge 1985, which compared BT with CBT and psychodynamic therapies, and Rehm 1984, which compared BT with CBT) reported social adjustment based on a social adjustment scale. Analysis revealed no evidence of significant differences when BT was compared with CBT (Analysis 1.6.1).
3.1.9 Quality of life
No data were reported.
3.1.10 Economic outcomes
No data were reported.
3.2 BT versus third wave CBT
No third wave CBT was included in our review.
3.3 BT versus psychodynamic therapies
Primary outcomes
3.3.1 Treatment efficacy: response
Four studies compared BT with psychodynamic therapies, but two studies did not adequately report outcomes. The remaining two studies (Bellack 1981; Breckenridge 1985) reported continuous outcome based on BDI. We analysed the imputed response rate for these two studies. Analysis revealed no evidence of significant differences in response rate between BT and psychodynamic therapies (Figure 3, Analysis 1.1.2; 2 studies, 110 participants, RR 1.24, 95% CI 0.84 to 1.82).
3.3.2 Treatment acceptability: dropouts for any reason
Four studies compared BT with psychodynamic therapies, but two studies did not report the numbers of dropouts. We analysed dropout rates for the remaining two studies (Bellack 1981; Sanchez 1980). Analysis revealed no evidence of significant differences in acceptability between BT and psychodynamic therapies (Figure 4, Analysis 1.4.2; 2 studies, 96 participants, RR 0.90, 95% CI 0.47 to 1.70)
Secondary outcomes
3.3.3 Remission
Four studies compared BT with psychodynamic therapies, but two studies did not adequately report outcomes. The remaining two studies (Bellack 1981; Breckenridge 1985) reported continuous outcomes based on BDI. We analysed the imputed remission rate for these two studies. Analysis revealed no evidence of significant differences between response rates for BT and psychodynamic therapies (Analysis 1.2.2; 2 studies, 110 participants, RR 1.32, 95% CI 0.85 to 2.06).
3.3.4 Severity of depression symptoms
Two studies (Bellack 1981; Breckenridge 1985) reported continuous outcomes based on BDI. Analysis revealed no evidence of significant differences in response rate between BT and psychodynamic therapies (Analysis 1.3.2; 2 studies, 93 participants, SMD ‐0.37, 95% CI ‐0.79 to 0.05).
3.3.5 Improvement in overall symptoms
No data were reported.
3.3.6 Anxiety symptoms
One study (Breckenridge 1985, which compared BT with CBT and psychodynamic therapies) reported anxiety symptoms based on a brief symptom Inventory. Analysis revealed no evidence of significant differences when BT was compared with psychodynamic therapies (Analysis 1.5.2).
3.3.7 Adverse effects
No study provided reports of adverse effects.
3.3.8 Social adjustment
One study (Breckenridge 1985, which compared BT with CBT and psychodynamic therapies) reported social adjustment based on a social adjustment scale. Analysis revealed no evidence of significant differences when BT was compared with psychodynamic therapies (Analysis 1.6.2).
3.3.9 Quality of life
No data were reported.
3.3.10 Economic outcomes
No data were reported.
3.4 BT versus humanistic therapies
Primary outcomes
3.4.1 Treatment efficacy: response
Three studies compared BT with humanistic therapies, but two studies did not report the numbers of participants at the end of treatment. The remaining study (Padfield 1975) reported continuous outcomes based on the Zung Self‐Rating Depression Scale. We analysed the imputed response rate for this study. Analysis revealed no evidence of significant differences in response rates between BT and humanistic therapies (Figure 3, Analysis 1.1.3; 1 study, 24 participants, RR 1.40, 95% CI 0.61 to 3.19).
3.4.2 Treatment acceptability: dropouts for any reason
One study (Padfield 1975, which compared BT with humanistic therapies) reported the number of dropouts. Analysis revealed no evidence of significant differences in acceptability between BT and humanistic therapies (Figure 4, Analysis 1.4.3; 1 study, 24 participants, RR 0.50, 95% CI 0.11 to 2.23).
Secondary outcomes
3.4.3 Remission
Three studies compared BT with humanistic therapies, but two studies did not adequately report outcomes. The remaining study (Padfield 1975) reported continuous outcomes based on the Zung Self‐ Rating Depression Scale. We analysed the imputed remission rate for this study. Analysis revealed no evidence of significant differences between response rates of BT and humanistic therapies (Analysis 1.2.3; 1 study, 24 participants, RR 1.14, 95% CI 0.61 to 2.13).
3.4.4 Severity of depression symptoms
One study (Padfield 1975) reported continuous outcomes based on the Zung Self‐Rating Depression Scale. Analysis revealed no evidence of significant differences in response rates between BT and humanistic therapies (Analysis 1.3.3; 1 study, 24 participants, SMD ‐0.35, 95% CI ‐1.16 to 0.45).
3.4.5 Improvement in overall symptoms
No data were reported.
3.4.6 Anxiety symptoms
No data were reported.
3.4.7 Adverse effects
No study provided reports of adverse effects.
3.4.8 Social adjustment
No data were reported.
3.4.9 Quality of life
No data were reported.
3.4.10 Economic outcomes
No data were reported.
3.5 BT versus integrative therapies
Primary outcomes
3.5.1 Treatment efficacy: response
One study (Pace 1977, which compared BT with integrative therapies) reported continuous outcomes based on the Zung Self‐Rating Depression Scale. We analysed the imputed response rate for this study. Analysis revealed no evidence of significant differences in the response rates between BT and integrative therapies (Figure 3, Analysis 1.1.4; 1 study, 12 participants, RR 9.00, 95% CI 0.59 to 137.65).
3.5.2 Treatment acceptability: dropouts for any reason
One study (Pace 1977, which compared BT with integrative therapies) reported the number of dropouts. Analysis revealed no evidence of significant differences in acceptability between BT and integrative therapies (Figure 4, Analysis 1.4.4; 1 study, 12 participants, RR 1.00, 95% CI 0.08 to 12.56).
Secondary outcomes
3.5.3 Remission
No data were reported.
3.5.4 Severity of depression symptoms
One study (Pace 1977, which compared BT with integrative therapies) reported continuous outcomes based on the Zung Self‐Rating Depression Scale. Analysis revealed no evidence of significant differences in the response rate between BT and integrative therapies (Analysis 1.3.4; 1 study, 10 participants, SMD ‐1.36, 95% CI ‐2.82 to 0.09).
3.5.5 Improvement in overall symptoms
No data were reported.
3.5.6 Anxiety symptoms
One study (Pace 1977, which compared BT with integrative therapies) reported anxiety symptoms based on anxiety state. Analysis revealed no evidence of significant differences when BT was compared with integrative therapies (Analysis 1.5.3).
3.5.7 Adverse effects
No study provided reports of adverse effects.
3.5.8 Social adjustment
No data were reported.
3.5.9 Quality of life
No data were reported.
3.5.10 Economic outcomes
No data were reported.
Outcomes at follow‐up assessment within 6 months
Nine studies (eight studies comparing BT with CBT and one study comparing BT with integrative therapies) reported continuous outcomes at various follow‐up time points (within six months). Time points ranged from five weeks to six months. Because five weeks to six months falls into the short‐term follow‐up time interval set out in Data extraction and management, we decided to combine the findings of these studies as short‐term follow‐up results.
No study reported a response or remission rate based on a depression scale or on the authors' definition, and we imputed response and remission rates from continuous outcomes. In two studies, we had to use imputed SDs to calculate remission and response rates.
As a result of this ITT analysis, BT was found to be inferior to CBT in terms of remission, response and depression severity at follow‐up. The RR of BT over CBT was 0.76 (Analysis 14.1.1; 95% CI, 0.59 to 0.99) for response and 0.77 (Analysis 14.2.1; 95% CI 0.61 to 0.98) for remission, corresponding with the number needed to treat for an additional beneficial outcome (NNTB) of six (95% CI 4 to 143) for response and seven (95% CI 4 to 72) for remission (Table 2).
14.1. Analysis.
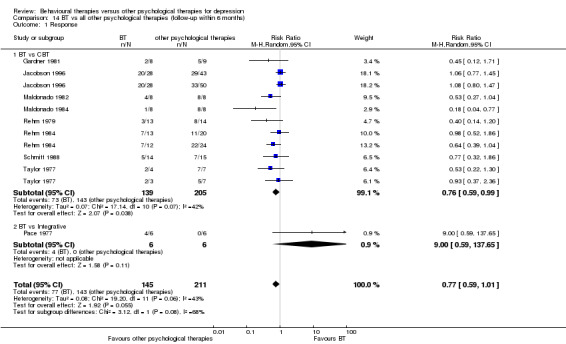
Comparison 14 BT vs all other psychological therapies (follow‐up within 6 months), Outcome 1 Response.
14.2. Analysis.
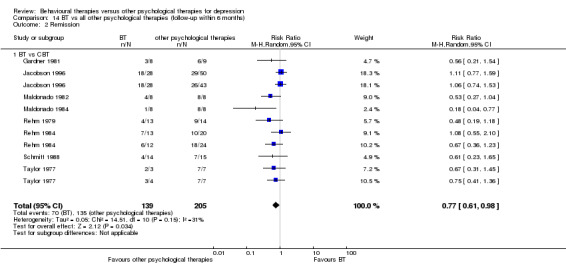
Comparison 14 BT vs all other psychological therapies (follow‐up within 6 months), Outcome 2 Remission.
Sensitivity analyses
None of the sensitivity analyses led to a change in the main findings concerning primary outcomes. No significant differences were noted between BT and all other psychological therapies in terms of response rate, remission and acceptability when BT was compared with other psychological therapies all together or when BT was compared with each therapy. Only when we excluded imputed data did CBT show slight superiority to BT in terms of one secondary outcome, namely, remission, but not in terms of severity of depression. In all other sensitivity analyses, no significant differences were noted between BT and other psychological therapies.
Excluding studies in which treatment fidelity was not assessed
When studies with high risk or unclear risk of bias in treatment fidelity were excluded, three studies (Breckenridge 1985; Jacobson 1996; Padfield 1975) that adequately reported outcomes were included in this analysis. No study compared BT with integrative therapies. The result did not change the main findings of primary outcomes (Analysis 7.1; Analysis 7.2; Analysis 7.3).
7.1. Analysis.
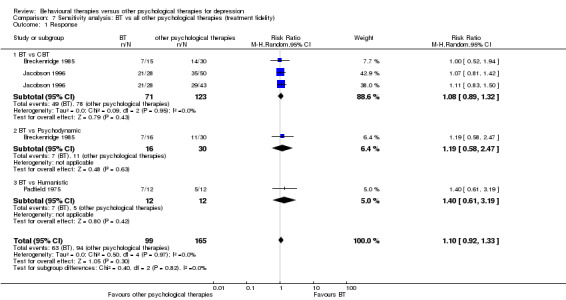
Comparison 7 Sensitivity analysis: BT vs all other psychological therapies (treatment fidelity) , Outcome 1 Response.
7.2. Analysis.
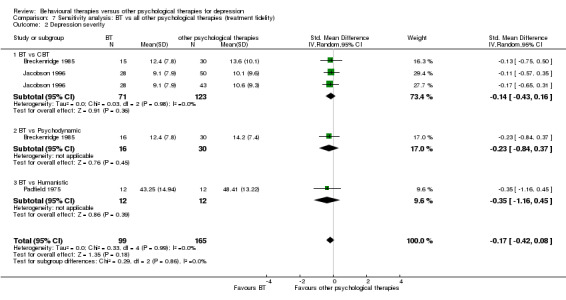
Comparison 7 Sensitivity analysis: BT vs all other psychological therapies (treatment fidelity) , Outcome 2 Depression severity.
7.3. Analysis.
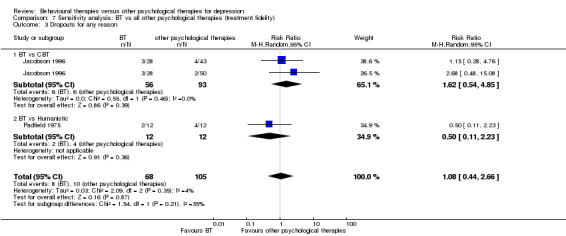
Comparison 7 Sensitivity analysis: BT vs all other psychological therapies (treatment fidelity) , Outcome 3 Dropouts for any reason.
Excluding studies that did not use allocation concealment
We could not conduct this sensitivity analysis because no study reported how investigators maintained allocation concealment.
Excluding studies in which imputed data were used
Because only one study reported response rate based on a validated depression scale, we had to use imputed data to calculate response rates for most of the studies. Therefore, we conducted sensitivity analyses of remission rates and depression severity, in addition to response rate. Four studies (Jacobson 1996; Rehm 1979; Shaw 1977; Wetzel 1992) that compared BT with CBT and one study (Bellack 1981) that compared BT with psychodynamic therapies reported remission rates using authors' definitions, and they were included in the analysis of remission.
When BT was compared with all other psychological therapies, the result did not change the main findings of primary outcomes (Analysis 8.1).
8.1. Analysis.
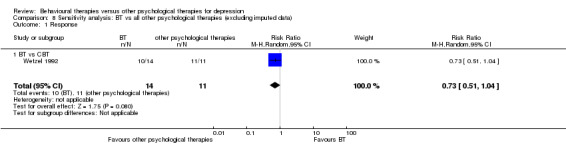
Comparison 8 Sensitivity analysis: BT vs all other psychological therapies (excluding imputed data), Outcome 1 Response.
When BT was compared with each class of psychological therapies, CBT showed superiority to BT in terms of remission (Analysis 8.2.1; RR 0.74, 95% CI 0.57 to 0.96). On the other hand, in the analysis of severity of depression, 12 studies that compared BT with CBT were included in the analysis, and no significant differences between BT and CBT were noted (Analysis 8.3.1; standardised mean difference (SMD) 0.00, 95% CI ‐0.18 to 0.19).
8.2. Analysis.
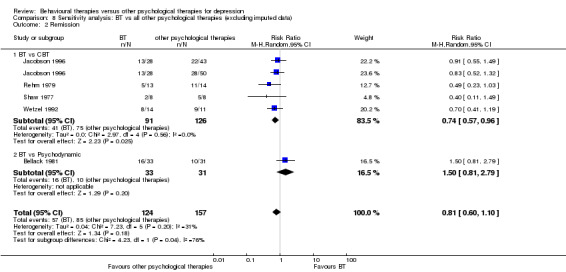
Comparison 8 Sensitivity analysis: BT vs all other psychological therapies (excluding imputed data), Outcome 2 Remission.
8.3. Analysis.
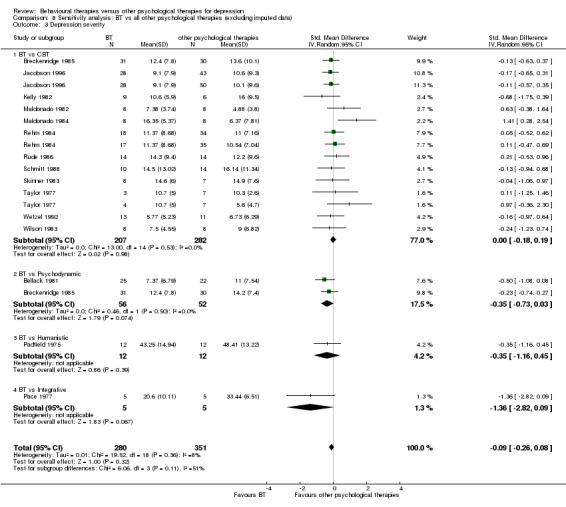
Comparison 8 Sensitivity analysis: BT vs all other psychological therapies (excluding imputed data), Outcome 3 Depression severity.
In comparison with other psychological therapies (psychodynamic, humanistic and integrative therapies), the results did not change the main findings of primary outcomes. No data were provided on remission when BT was compared with integrative or humanistic therapies.
Excluding studies in which antidepressant treatment was allowed
When studies in which pharmacotherapy was allowed were excluded, four studies (Kelly 1983; Pace 1977; Padfield 1975; Taylor 1977) were included in this analysis. The results did not change the main findings of primary outcomes. No studies compared BT with psychodynamic therapies (Analysis 9.1; Analysis 9.2; Analysis 9.3).
9.1. Analysis.
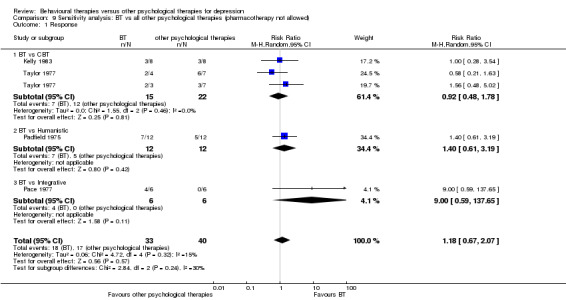
Comparison 9 Sensitivity analysis: BT vs all other psychological therapies (pharmacotherapy not allowed), Outcome 1 Response.
9.2. Analysis.
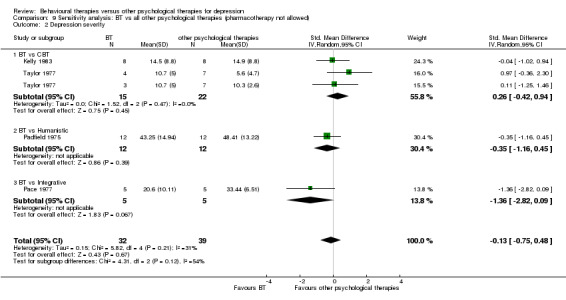
Comparison 9 Sensitivity analysis: BT vs all other psychological therapies (pharmacotherapy not allowed), Outcome 2 Depression severity.
9.3. Analysis.
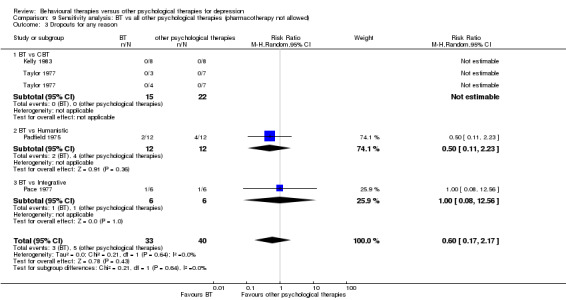
Comparison 9 Sensitivity analysis: BT vs all other psychological therapies (pharmacotherapy not allowed), Outcome 3 Dropouts for any reason.
Excluding studies of other subcategories
We excluded studies that classified "other" subcategories such as "other BT" or "other CBT" to compare our predefined "standard" BT with "standard" other psychological therapies. In this sense, no study compared BT with integrative therapies. The results did not change the main findings of primary outcomes (Analysis 10.1; Analysis 10.2; Analysis 10.3).
10.1. Analysis.
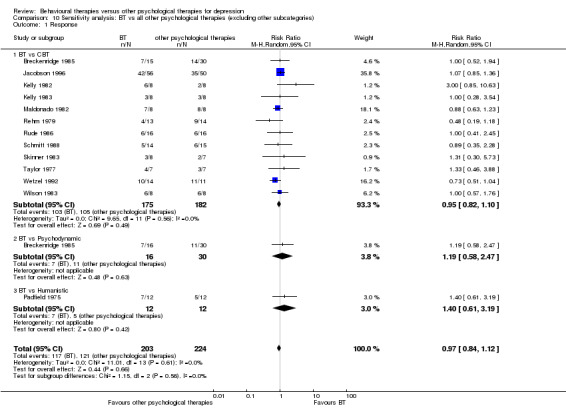
Comparison 10 Sensitivity analysis: BT vs all other psychological therapies (excluding other subcategories), Outcome 1 Response.
10.2. Analysis.
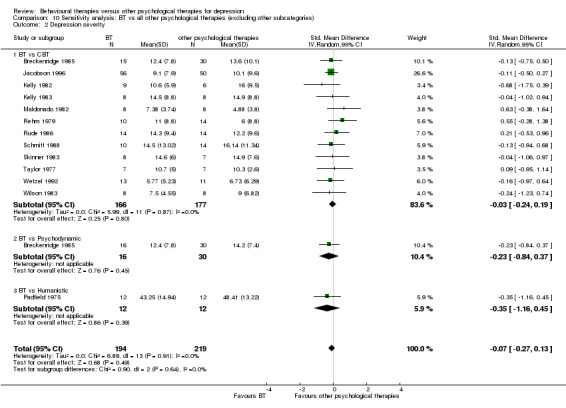
Comparison 10 Sensitivity analysis: BT vs all other psychological therapies (excluding other subcategories), Outcome 2 Depression severity.
10.3. Analysis.
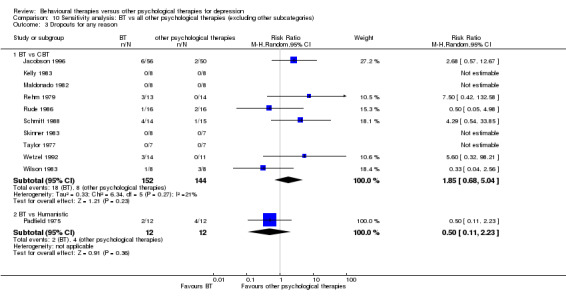
Comparison 10 Sensitivity analysis: BT vs all other psychological therapies (excluding other subcategories), Outcome 3 Dropouts for any reason.
Excluding studies in which participants with non‐operationalised diagnoses were included
When studies were included in which only participants with a diagnosis of major depressive disorder were recruited, five studies were included in this analysis. The results did not change the main findings of primary outcomes. No study compared BT with integrative or humanistic therapies (Analysis 11.1; Analysis 11.2; Analysis 11.3).
11.1. Analysis.
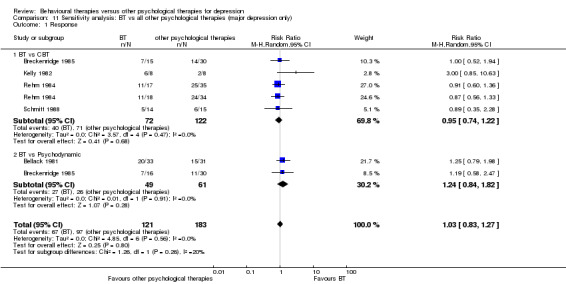
Comparison 11 Sensitivity analysis: BT vs all other psychological therapies (major depression only), Outcome 1 Response.
11.2. Analysis.
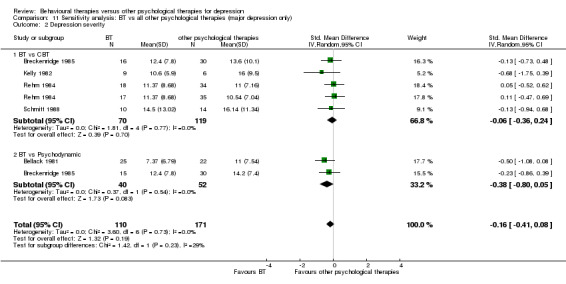
Comparison 11 Sensitivity analysis: BT vs all other psychological therapies (major depression only), Outcome 2 Depression severity.
11.3. Analysis.
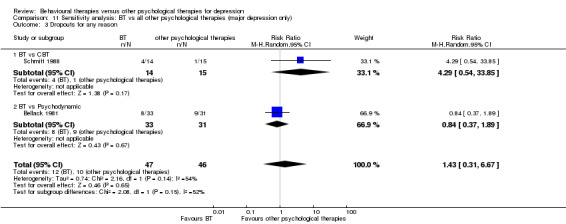
Comparison 11 Sensitivity analysis: BT vs all other psychological therapies (major depression only), Outcome 3 Dropouts for any reason.
Excluding studies in which the number of sessions was greater than 12
Because the number of studies was insufficient, we conducted sensitivity analyses that excluded studies in which the number of sessions was greater than 12. The results did not change the main findings of primary outcomes (Analysis 12.1; Analysis 12.2; Analysis 12.3).
12.1. Analysis.
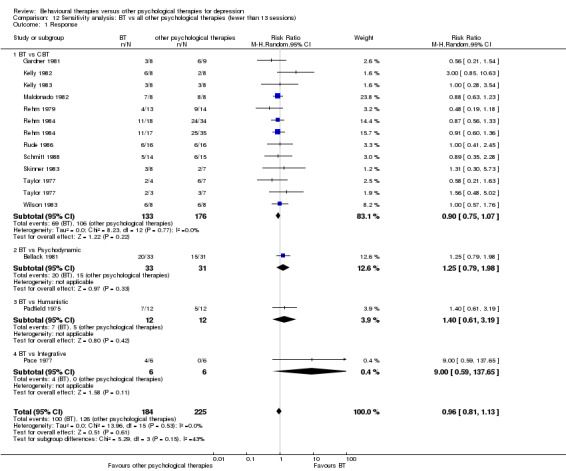
Comparison 12 Sensitivity analysis: BT vs all other psychological therapies (fewer than 13 sessions), Outcome 1 Response.
12.2. Analysis.
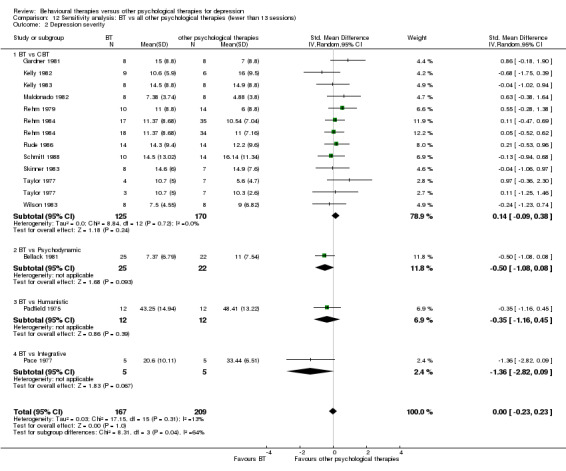
Comparison 12 Sensitivity analysis: BT vs all other psychological therapies (fewer than 13 sessions), Outcome 2 Depression severity.
12.3. Analysis.
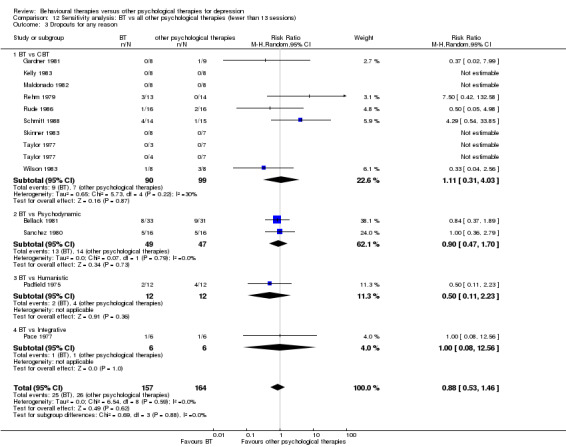
Comparison 12 Sensitivity analysis: BT vs all other psychological therapies (fewer than 13 sessions), Outcome 3 Dropouts for any reason.
Excluding studies in which dropouts were replaced
Two studies (Breckenridge 1985; Wilson 1982) replaced dropouts without randomisation. When those studies were excluded, the results did not change the main findings of primary outcomes (Analysis 13.1; Analysis 13.2; Analysis 13.3).
13.1. Analysis.
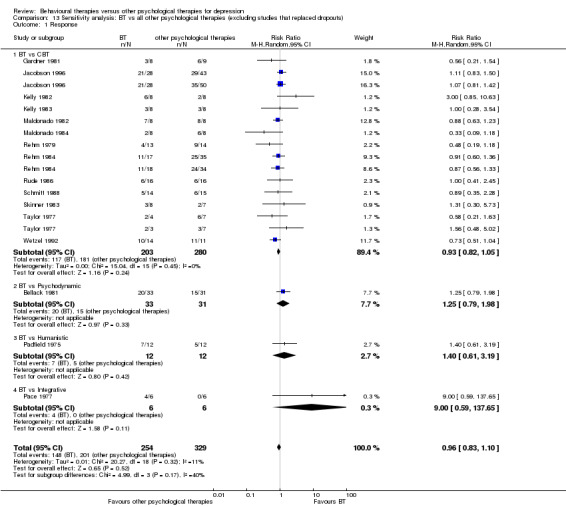
Comparison 13 Sensitivity analysis: BT vs all other psychological therapies (excluding studies that replaced dropouts), Outcome 1 Response.
13.2. Analysis.
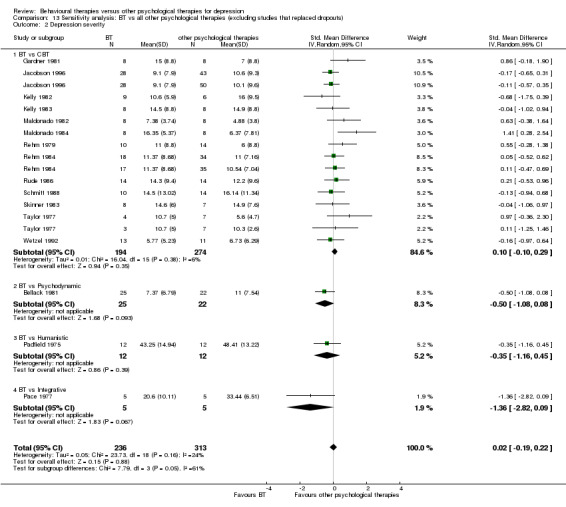
Comparison 13 Sensitivity analysis: BT vs all other psychological therapies (excluding studies that replaced dropouts), Outcome 2 Depression severity.
13.3. Analysis.
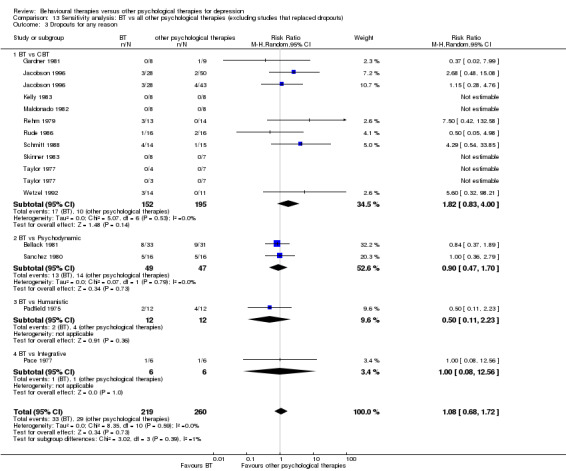
Comparison 13 Sensitivity analysis: BT vs all other psychological therapies (excluding studies that replaced dropouts), Outcome 3 Dropouts for any reason.
Best/worst case scenarios
We calculated response rates in best/worst case scenarios in 16 studies that reported the numbers of randomly assigned participants (Analysis 6.1; Analysis 6.2).
6.1. Analysis.
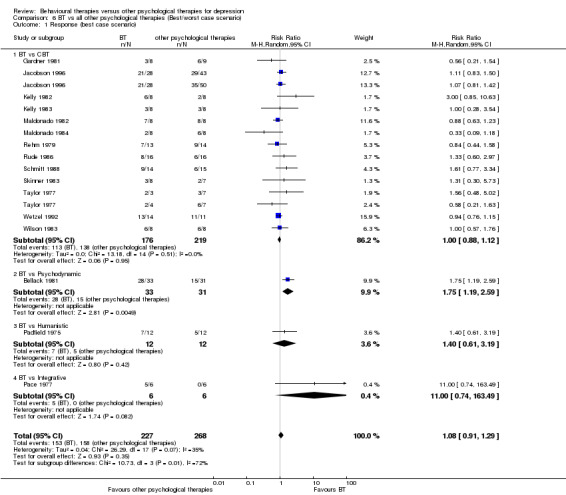
Comparison 6 BT vs all other psychological therapies (Best/worst case scenario), Outcome 1 Response (best case scenario).
6.2. Analysis.
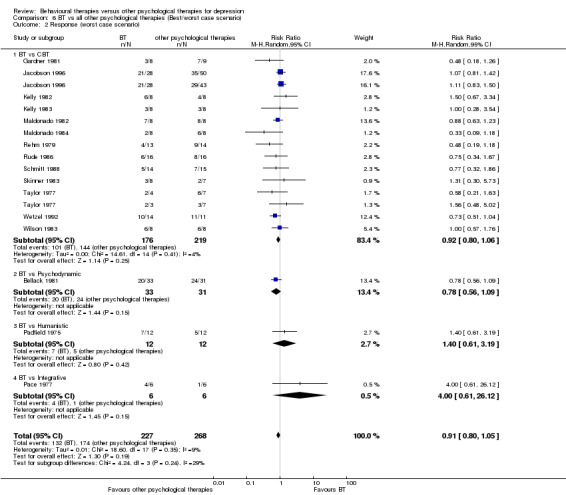
Comparison 6 BT vs all other psychological therapies (Best/worst case scenario), Outcome 2 Response (worst case scenario).
When BT was compared with all other psychological therapies, analysis revealed no evidence of significant differences in best or worst case scenarios.
When BT was compared with each class of psychological therapies, BT showed superiority to psychodynamic therapies In best case scenarios (RR 1.75, 95% CI 1.19 to 2.59), but in worst case scenarios, no significant differences were noted between these two treatments (RR 0.78, 95% CI 0.56 to 1.09). Other results did not change the main findings of primary outcomes.
Subgroup analyses
We conducted preplanned subgroup analyses only when a meaningful number of relevant studies had been identified. Only two subtype comparisons included more than one study (BT‐Lewinsohn vs CBT‐Cognitive therapy and BT‐SST/assertion vs CBT‐self‐control).
Baseline depression severity
We did not conduct this analysis because baseline depression severity was categorised as moderate in most of the studies, and this analysis was not meaningful.
Number of sessions
See our sensitivity analysis "Excluding studies in which the number of sessions was greater than 12".
BT‐Lewinsohn vs CBT‐cognitive therapy
No significant differences were noted between BT‐Lewinsohn vs CBT‐cognitive therapy in terms of response, severity of depression and dropout rate (Analysis 15.1; Analysis 15.2; Analysis 15.3).
15.1. Analysis.
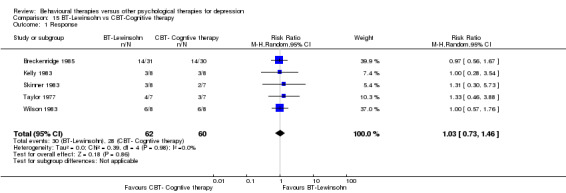
Comparison 15 BT‐Lewinsohn vs CBT‐Cognitive therapy, Outcome 1 Response.
15.2. Analysis.
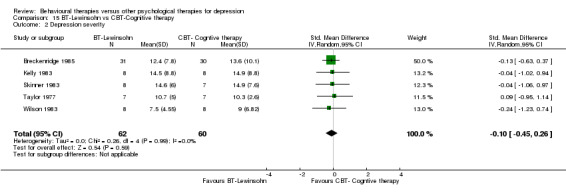
Comparison 15 BT‐Lewinsohn vs CBT‐Cognitive therapy, Outcome 2 Depression severity.
15.3. Analysis.
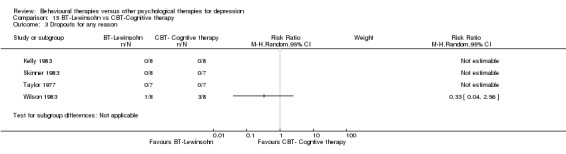
Comparison 15 BT‐Lewinsohn vs CBT‐Cognitive therapy, Outcome 3 Dropouts for any reason.
BT‐social skills training/assertiveness training vs CBT‐self‐control
No significant differences were noted between BT‐SST/assertiveness training vs CBT‐self‐control in terms of response, severity of depression and dropout rate (Analysis 16.1; Analysis 16.2; Analysis 16.3).
16.1. Analysis.
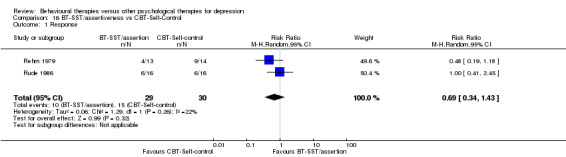
Comparison 16 BT‐SST/assertiveness vs CBT‐Self‐Control, Outcome 1 Response.
16.2. Analysis.
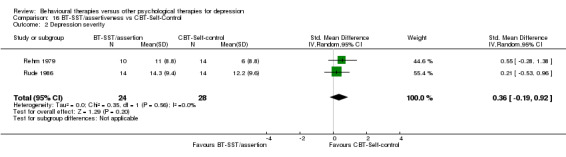
Comparison 16 BT‐SST/assertiveness vs CBT‐Self‐Control, Outcome 2 Depression severity.
16.3. Analysis.
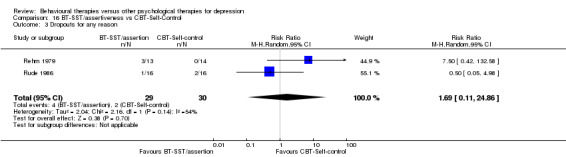
Comparison 16 BT‐SST/assertiveness vs CBT‐Self‐Control, Outcome 3 Dropouts for any reason.
Strengh of therapeutic alliance
No data were provided.
Funnel plot analyses
The funnel plot of response on BT versus all other psychological therapies at end of treatment was not suggestive of small‐study effects (Figure 5). However, the funnel plot of response (Figure 6) or remission when BT was compared with CBT at follow‐up appeared asymmetrical and was suggestive of small‐study effects in favour of CBT.
5.
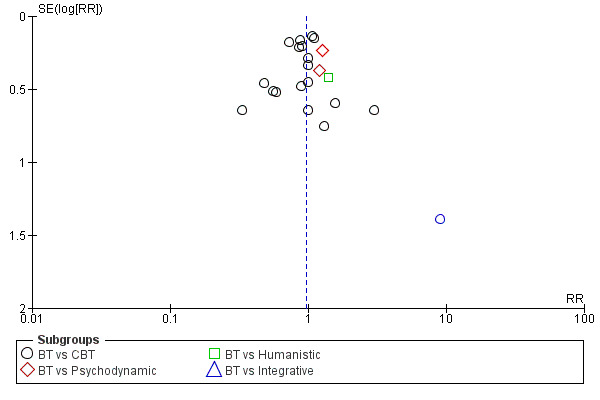
Funnel plot of comparison: 1 BT vs all other psychological therapies outcome: 1.1 Response.
6.
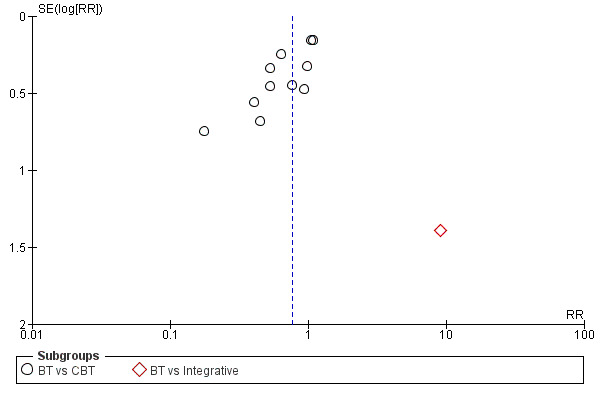
Funnel plot of comparison: 13 BT vs all other psychological therapies (follow up within 6 months), outcome: 13.1 Response.
Summary of findings
We prepared three 'Summary of findings' tables.
BT compared with all other psychological therapies for depression.
BT compared with CBT for depression.
BT compared with psychodynamic therapies for depression.
As is evident from the foregoing presentation of results, no statistically significant findings emerged, except possibly for differences in response and remission at follow‐up between BT and CBT. The most notable finding from these 'Summary of findings' tables is the low quality of evidence determined by GRADE rating: The randomised evidence synthesised in this review had to be downgraded usually by two levels because all studies were rated at unclear or high risk of bias in random sequence generation and allocation concealment, the sample sizes were very small and many data had to be imputed. No estimates indicated high quality of evidence.
Discussion
Summary of main results
In this review, we assessed the efficacy and acceptability of BT in three types of comparison: all BT approaches with all other psychological therapies, different BT approaches (subcategories of BT) with other psychological therapies and all BT approaches with the other five major categories of psychological therapies (CBT, third wave CBT, psychodynamic, humanistic and integrative).
We identified and included 25 studies, 20 of which compared BT with CBT. The results revealed no evidence of significant differences between BT and other psychological therapies taken all together in terms of efficacy (RR of response 0.97, 95% CI 0.86 to 1.09) or acceptability (RR of dropout, RR 1.02, 95% CI 0.65 to 1.61) at end of treatment.
When different BT approaches were compared (Lewinsohn, Jacobson, SST/assertiveness, Relaxation; note that only one study used the Jacobson model) with all other psychological therapies, no evidence suggested significant differences between each BT approach and other psychological therapies at end of treatment.
Similarly, when all BT approaches were compared with other major classes of psychological therapies (CBT, third wave CBT, psychodynamic, humanistic and integrative), no evidence revealed significant differences between BT and CBT, or between BT and psychodynamic therapies, in terms of efficacy or acceptability at post‐treatment. In the comparison of response between BT and CBT, the RR of BT over CBT was 0.93 (95% CI 0.83 to 1.05). Low‐quality evidence suggests a small difference in response favouring CBT. For all other comparisons (BT compared with psychodynamic, humanistic, integrative or third wave therapies), this review provides little or no information because only two studies using psychodynamic therapies (one study using humanistic and one using integrative therapies) were included in this review. No study compared BT with third wave CBT.
However, we have to note that all of these results should be interpreted with great caution because most of the studies were small to very small and were rated as being at unclear or high risk of bias. Also, most of the studies did not report our a priori defined outcomes, and we had to use imputed data for remission and response in many studies.
Overall completeness and applicability of evidence
We have been able to include the largest number of trials (25 RCTs) among several systematic reviews focused on behavioural therapies (e.g. 16 RCTs in Cuijpers 2007, 17 RCTs in Ekers 2008), and the funnel plot analysis has not revealed apparent small‐study effects in our data set. Although we have made extensive efforts to search for relevant trials, it is possible that unpublished trials remain irretrievable to us.
It is important to note that given this possibly incomplete set of randomised evidence (25 RCTs), we could include only a limited number of studies in each of our primary and secondary outcomes (18 of 25 at most). Moreover, none of the studies reported on adverse effects or economic outcomes.
The publication years of the included studies spanned from 1975 to 1996. A great majority had been conducted in North America, and the remainder in Western countries. Only eight studies had used operationalised diagnostic criteria. It is therefore not straightforward to generalise the present findings to today's patients with operationally diagnosed depression and/or in non‐Western countries.
Another inherent difficulty in applying the current evidence involved ensuring the content and the quality of BT. In general, when the results of psychological therapy trials are evaluated, two things must be considered. One is categorisation of therapy ("Was the BT approach used in the study the same as our BT approach?" We will discuss this issue in Potential biases in the review process). The other is treatment fidelity ("Did study investigators deliver treatment as they intended? Did they check?"), because the way a study has been designed does not guarantee that the treatment was provided as intended. For example, a behavioural approach could be used not as a therapeutic model but only as a simple therapeutic technique in psychological therapy sessions without a trained provider. Therefore, to ensure the quality of BT, we thought it was necessary to assess treatment fidelity. However, in this review, only six studies examined treatment fidelity in a satisfactory manner. Although sensitivity analyses did not change the main results, treatment fidelity remained unclear in most studies. In other words, it cannot be known if what was claimed to be a behavioural therapy in these studies was in fact a behavioural therapy, because study authors reported no or unclear checking on the manipulation, and vice versa. What today's clinicians plan to administer as a behavioural therapy can be truly behavioural and yet effectiveness as indicated in the current body of evidence can be unclear if they conduct psychological therapy without proper quality control (e.g. using manuals, using appropriately qualified and trained therapists, checking treatment fidelity as by monitoring through audiotapes).
Quality of the evidence
Most of the included studies were not of sufficient quality and quantity to provide strong evidence. This body of evidence was downgraded for the following reasons: risk of bias and statistical imprecision.
First of all, the sample size of included participants was very small in most of the studies. The low number of small studies limits the power of our analyses, and we have downgraded the quality of evidence for a number of outcomes across the 'Summary of findings' tables on the basis of imprecision. We identified 25 studies for this review, but only two studies recruited 30 or more participants for each arm. Other studies recruited fewer participants or did not report the number of participants randomly assigned.
Second, because most studies did not report remission or response rates based on any validated scale, we had to impute response and remission rates from the reported continuous outcomes. In addition, because self‐rated scales were used most commonly to report continuous outcomes, detection bias was present.
Inadequate reporting in many of the older studies led to our ratings of unclear or high risk of bias. No study described how allocation was concealed, and most studies did not report on randomisation sequence generation. Two studies replaced a small proportion of participants who dropped out with additional recruits, thus breaking randomisation.
In addition to these common sources of bias, other areas for potential risks of bias are specific to psychotherapy trials: treatment fidelity and therapist qualification/training. However, in most of the included studies, these areas were not assessed or reported. Of 25 included studies, 19 provided insufficient information about treatment fidelity as determined by recording and monitoring with a scale. Among 18 studies that adequately reported outcomes, only three studies indicated that therapies were provided by qualified therapists who had received specific training. In the remaining studies, the therapists were not qualified (e.g. students), or the therapists had not received training or no information was provided. Therefore, the quality of therapies was heterogeneous among the included studies.
To assess publication bias, we constructed a funnel plot (Figure 5), which did not suggest publication bias for BT in comparison with all other psychological therapies. The apparent superiority of BT over CBT in maintaining response or remission over a short‐term follow‐up may be subject to small‐study effects (Figure 6).
Overall, the body of evidence in this review must be considered too weak to permit robust conclusions.
Potential biases in the review process
Factors that might have introduced biases into this review process include the following.
First, two of the review authors specialise in CBT (TAF is a diplomate of the Academy of Cognitive Therapy, and VH provides CBT in general practice), whereas no one who specialises in other psychological therapies was included as a member of the review team. This could suggest a potential bias in favour of CBT.
Second, to answer the practical and general question, "Is BT more effective and acceptable than other psychological therapies?", we set the comparison between BT and all other psychological therapy approaches as our main comparison in the protocol. However, "all other psychological therapies" include different psychological approaches (CBT, third wave CBT, psychodynamic, humanistic and integrative), and the efficacy of each approach considered may be different. Therefore, one can argue that results of the comparison between BT and each of the different psychological approaches (BT vs CBT, BT vs psychodynamic and so on) are more meaningful and practical than those derived from the comparison between BT and all other psychological approaches taken together. On the other hand, when we compared BT with different psychological approaches, fewer studies could be included in the analyses, and the evidence was too weak to lead to any meaningful conclusions.
In addition, as we described in Overall completeness and applicability of evidence, it is difficult to make a clear distinction between BT and other psychological therapies. We classified BT as a particular group of psychological therapies that use similar techniques. However, CBT and extended behavioural activation (we classified eBA as a subcategory of third wave CBT) definitely show overlap with BT in terms of therapeutic techniques used, and no unanimous agreement was reached about what should and should not be included in the "standard BT" category.
Furthermore, even within BT, the psychological therapeutic techniques used in each study could involve many variations. For example, a study that used BT‐Lewinsohn appeared to be different from a study using BT‐Relaxation. Thus, when we compare one subcategory of BT with another subcategory of other psychological therapies (e.g. BT‐Lewinsohn vs CBT‐Cognitive therapy), we can assess the differences between most "pure" types of psychological therapy. However, as we mentioned above, if we had done this, it would have been more difficult to include a meaningful number of studies in the analysis.
Agreements and disagreements with other studies or reviews
As far as we know, two other recent systematic reviews have focused on broadly conceived behavioural treatments (Cuijpers 2007; Ekers 2008). As we described in Why it is important to do this review, Ekers 2008 compared BT with controls and other psychological therapies (CBT, brief psychological therapies and supportive therapy). These investigators suggested that BT was superior to brief psychological therapies and to supportive therapy, and that BT was equivalent to CBT in terms of depression recovery rates, symptom levels and participant dropout. However, Ekers 2008 included the interventions that we excluded from the analyses (i.e. bibliotherapy and third wave CBT). Although some of the included studies in the Ekers review were different from ours, the conclusions of both reviews were the same: BT has efficacy and acceptability equal to those of CBT. On the other hand, Cuijpers 2007 compared BT with controls and other therapies (mainly cognitive therapy) and included a heterogeneous group of studies (they included inpatient populations and individuals with dementia, which were excluded in this review). The results reported by Cuijpers et al indicate that no evidence was found of significant differences in efficacy between BT and cognitive therapy, and their conclusion is again consistent with that of the present review.
Authors' conclusions
Implications for practice.
At present, no strong evidence suggests that BT may differ from other psychological therapies in terms of efficacy or acceptability for the treatment of depression in adults. Although most of the included studies, whether considered individually or taken together, were too low in both quality and quantity to provide strong evidence, BT appeared to be as effective as other psychological therapies. When we compared BT with CBT, we were able to include in the analysis relatively large numbers of studies and participants, and our results suggest the following.
At best, BT is not superior to CBT.
The wide confidence intervals suggest that BT is not much different from CBT (i.e. statistical imprecision).
The point estimate is close to 1, but the truth is that results show BT to be marginally inferior to CBT, with only a small chance that it could be marginally better than CBT.
In other words, all therapeutic approaches seem to be equally effective across all schools of psychological therapies. It may be suggested that common factors shared by different psychological therapies (such as therapeutic alliance) are much more powerful than the contributions of specific techniques (Lambert 2013). However, it is difficult to estimate the magnitude of this relationship because no consensual definition of therapeutic alliance has been reached and because diverse instruments were used to measure it (Horvath 2011; McLeod 2011) (this is why we did not include alliance in our outcomes). We could not comment on this issue further in this review.
We should consider the problems associated with classification of psychological therapies when we use the results of studies of psychological therapy provided in clinical settings. As we described under Discussion, classification of psychological therapies (e.g. what should be categorised as BT, what should be categorised as eBA) varied among researchers, and no widely used let alone unanimously agreed‐upon categorisation of psychological therapies is known so far. Therefore, when we interpret the results of BT studies to compare efficacy, we should be careful that the "BT" used in the trial is the "BT" we want to know about. We believe that information on which manuals study investigators used and which component or therapeutic techniques were the focus of therapy will help people in making a judgement.
Implications for research.
This review highlights the need for better and larger studies of psychological therapies to assess their efficacy and acceptability. Most of the studies included in this review were small and were deemed to have unclear or high risk of bias. Future studies should provide sufficient information on the general risk of bias (such as random sequence generation or allocation concealment) and on quality indicators of treatment (such as assessment of treatment fidelity and therapist qualification/training). Also, detailed information on therapeutic approaches (not only the theoretical background but also which manual(s) were used and which kinds of therapeutic techniques were the focus) is necessary to clarify the investigators' conceptual framework.
Furthermore, future studies need to report "remission" and "response" based on both self‐rated and blinded observer–rated validated scales to enable ready comparison with other studies. In addition, outcomes should be measured at follow‐up time points.
Interest in the use of BT has once declined (as is shown in the publication years of the included studies), and new types of BT (such as eBA) have been developed. However, this review indicates that conventional BT may have efficacy and acceptability similar to those of other psychological therapies, despite their ease of implementation. These findings reveal the need for continued research on the use of BT in diverse clinical settings, with consideration of cost‐effectiveness and pragmatic feasibility.
Acknowledgements
This review is one publication of the High Impact Reviews of Effectiveness in Depression (HIRED) project, in which a group of researchers within the Cochrane Collaboration Depression, Anxiety and Neurosis Group conducted a systematic review of all available evidence for all psychological therapies for treating depression. Taken together, they will contribute data to the network meta‐analysis of psychological therapies for treating depression.
We would like to thank the CCDAN Editorial Team for the support, information and advice provided.
We would also like to thank the following original study authors for responding to our inquiries and providing precious additional information, oftentimes after hours of searching for original data that were decades old: Gallagher DE, Gardner P, Kelly FD, Maldonado A, McNamara K, Marshall WL, Rehm LP and Sleimani M.
Special thanks are due to Bruno Da Costa (University of Bern) and Lucas Ford (Nagoya, Japan) for helping TAF to extract data from Spanish and Persian papers, respectively.
CRG Funding Acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Depression, Anxiety and Neurosis Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, the NHS or the Department of Health.
Appendices
Appendix 1. Categories of psychological therapies
| Categories | Abbreviation | Subcategories | Abbreviation |
| 1. Behavioural therapies | BT | Behavioural therapy (Lewinsohn) | |
| Behavioural activation (original model) (Jacobson) | BA | ||
| Social skills training/assertiveness training | SST/assertion | ||
| Relaxation therapy | |||
| Other behavioural therapies | |||
| 2. Cognitive‐behavioural therapies | CBT | Cognitive therapy | |
| Rational emotive behaviour therapy | |||
| Problem‐solving therapy | |||
| Self‐control therapy | |||
| Coping with Depression course | |||
| Other cognitive‐behavioural therapies | |||
| 3. Mindfulness‐based 'third wave' cognitive and behavioural therapies | Third wave CBT | Acceptance and commitment therapy | |
| Compassionate mind training | |||
| Functional analytic psychotherapy | |||
| Extended behavioural activation | eBA | ||
| Metacognitive therapy | |||
| Mindfulness‐based cognitive therapy | |||
| Dialectical behaviour therapy | |||
| Other third wave cognitive and behavioural therapies (other third wave CBT) |
|||
| 4. Psychodynamic therapies | Drive/structural model (Freud) | ||
| Relational model (Strupp, Luborsky) | |||
| Integrative analytic model (Mann) | |||
| Other psychodynamic therapies | |||
| 5. Humanistic therapies | Person‐centered therapy (Rogerian) | ||
| Gestalt therapy | |||
| Experiential therapies | |||
| Transactional analysis | |||
| Existential therapy | |||
| Non‐directive/supportive therapies | |||
| Other humanistic therapies | |||
| 6. Interpersonal, cognitive analytic and other integrative therapies (integrative therapies) |
Interpersonal therapy | IPT | |
| Cognitive‐analytic therapy | CAT | ||
| Psychodynamic‐interpersonal therapy | |||
| Cognitive‐behavioural analysis system of psychotherapy | |||
| Counselling | |||
| Motivational interviewing | |||
| Other integrative therapy approaches |
Appendix 2. Search strategy: CCDANCTR update search—limited to behavioural therapies
#1. (behavio* NEAR2 (activation or contract* or intervention or modification or *therap* or train* or treatment)) #2. (behavioural or behavioral):ti #3. (abreaction or “activity scheduling” or ((assertive* or autogenic) NEAR (schedule* or training)) or (aversion NEXT *therap*) or biofeedback or “contingency management” or “conversion *therap*” or “covert sensiti*” or desensiti* or “distraction *therap*” or (implosive NEAR *therap*) or (exposure NEAR *therap*) or imagery or Lewinsohn* or ((pleasant or pleasing) NEAR (activit* or event*)) or “problem focus*” or psychoeducat* or “reciprocal inhibition” or relaxation or “response cost” or “sensitivity training” or (social* NEAR (effectiveness or skill*)) or socio‐environment* or “socio environment*”) #4. depress*:ti,ab #5. (#1 or #2 or #3) and #4
Appendix 3. Search strategy: CCDAN references register (psychotherapies for depression) 1/1/2012
| 1 | Title/Abstract= | therap* or psychotherap* |
| 2 | Keywords= | psychotherapy |
| 3 | Free‐Text= | acceptance* or commitment* or “activity scheduling” or adlerian or art or aversion or behvio* or brief or “client cent*” or cognitive* or color or colour or compassion‐focused or “compassion* focus*” or compassionate or conjoint or conversion or conversational or couples or dance or dialectic* or diffusion or distraction or eclectic or (emotion and focus*) or emotion‐focus* or existential or experiential or exposure or expressive or family or focus‐oriented or “focus oriented” or freudian or gestalt or “group” or humanistic or implosive or insight or integrative or interpersonal or jungian or kleinian or logo or marital or metacognitive or meta‐cognitive or milieu or morita or multimodal or multi‐modal or music or narrative or nondirective or non‐directive or “non directive” or nonspecific or non‐specific or “non specific” or “object relations” or “personal construct” or “person cent*” or person‐cent* or persuasion or play or ((pleasant or pleasing) and event*) or primal or problem‐focused or “problem focused” or problem‐solving or “problem solving” or process‐experiential or “process experiential” or psychodynamic or “rational emotive” or reality or “reciprocal inhibition” or relationship* or reminiscence or restructuring or rogerian or schema* or self‐control* or “self control*” or “short term” or short‐term or sex or “social effectiveness” or “social skill*” or socio‐environment* or “socio environment*” or “solution focused” or solution‐focused or “stress management” or supportive or time‐limited or “time limited” or “third wave” or transference or transtheoretical or validation |
| 4 | Free‐Text= | (abreaction or “acting out” or “age regression” or ((assertive* or autogenic or mind or sensitivity) and train*) or autosuggestion or “balint group” or ((behavior* or behaviour*) and (activation or therap* or treatment or contracting or modification)) or biofeedback or catharsis or cognitive* or “mind training” or counsel* or “contingency management” or countertransference or “covert sensitization” or “eye movement desensiti*” or “crisis intervention” or “dream analysis” or “emotional freedom” or “free association” or “functional analys*” or griefwork or “guided imagery” or hypno* or imagery or meditation* or “mental healing” or mindfulness* or psychoanaly* or psychodrama or psychoeducat* or “psycho* support*” or psychotherap* or relaxation or “role play*” or “self analysis” or “self esteem” or “sensitivity training” or “support* group*” or therapist or “therapeutic technique*” or “transactional analysis”) |
| 5 | ((1 or 2) and 3) or 4 | |
| 6 | Title/Abstract= | (depress* or dysthymi*) |
| 7 | 5 and 6 | |
| 8 | Tagged to CCDANCTR‐Study= | Empty |
| 9 | 7 and 8 |
Appendix 4. Search strategy: CINAHL
Psychotherapies for depression(n1114) 2010‐05‐19 (310 duplicates ‐ CCDAN Registers)
EBSCO CINAHL (Cumulative Index to Nursing and Allied Health Literature) was searched as follows: 1. (MH "Clinical Trials+") 2. TI (clinic* N1 trial*) or AB (clinic* N1 trial*) 3. TI ((singl* or doubl* or trebl* or tripl*) and (blind* or dummy or mask)) or AB ((singl* or doubl* or trebl* or tripl*) and (blind* or dummy or mask)) 4. TI ( randomi?ed or randomly) or AB (randomi?ed or randomly) 5. AB (random* N3 allocat*) or AB (random* N3 assign*) 6. (MH "Random Assignment") 7. PT clinical trial 8. (MH "Placebos") 9. TI placebo* or AB placebo* 10. AB (control N3 trial*) or AB (control N3 study) or AB (control N3 studies) 11. S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 12. (MM "Depression+") 13. (MM "Psychotherapy+") 14. (MH "Psychotherapy+") 15. (MM "Psychological Processes and Principles+") 16. (MM "Behavior and Behavior Mechanisms+") 17. (acceptance* or commitment* or “activity scheduling” or adlerian or art or aversion or brief or “client cent*” or cognitive or color or colour or “compassion focused” or compassionate or conjoint or conversion or conversational or couples or dance or dialectic* or diffusion or eclectic or (emotion* W1 focus*) or existential or experiential or exposure or expressive or family or (focus W1 oriented) or gestalt or group or humanistic or implosive or insight or integrative or interpersonal or marital or metacognitive or milieu or morita or multimodal or “multi‐modal” or music or narrative or nondirective or “non‐directive” or “non directive” or nonspecific or “non‐specific” or “non specific” or “object relations” or “personal construct” or “person cent*” or persuasion or play or “pleasant event*” or primal or “problem‐focused” or “problem focused” or “problem‐solving” or “problem solving” or “process‐experiential” or “process experiential” or psychodynamic or “rational emotive” or reality or “reciprocal inhibition” or relationship* or reminiscence or restructuring or schema* or “self‐control*” or “self contol*” or “short term” or “short‐term” or sex or “social effectiveness” or “social skill*” or socioenvironmental or “solution focused” or “stress management” or supportive or “time‐limited” or “time limited” or transference or transtheoretical or validation) 18.(S13 or S14 or S15 or S16) and S17 19. behavio#r W3 modification* 20. behavio#r W3 contract* 21. behavio#r W3 treat* 22. behavio#r W3 therap* 23. (sensitivity W3 train*) 24. (mind W3 train*) 25. (autogenic W3 train*) 26. (assertive* W3 train*) 27. (autosuggestion or “balint group” or biofeedback or catharsis or cognitive or “mind training” or counsel* or “contingency management” or countertransference or “covert sensitization” or “eye movement desensiti*” or “crisis intervention” or distraction or “dream analysis” or “emotional freedom” or “free association” or freudian or “functional analys*” or griefwork or “guided imagery” or hypno* or imagery or jungian or kleinian or meditation* or “mental healing” or mindfulness* or psychoanaly* or psychodrama or psychoeducat* or “psycho* support*” or psychotherap* or relaxation or rogerian or “role play*” or “self analysis” or “self esteem” or “sensitivity training” or “support* group*” or therapist or “therapeutic technique*” or third‐wave or “third wave” or “transactional analysis”) 28.S13 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 29. S11 and S12 and S28
Appendix 5. Search strategy: PSYNDEX
OVID PSYNDEX Search Strategy (11 June 2010 726 records NOT de‐duplicated) 1. Clinical Trials.sh. 2. Treatment Effectiveness Evaluation.sh. 3. Mental Health Program Evaluation.sh. 4. randomi#ed.mp. 5. randomly.mp. 6. randomized.ep. 7. pla#ebo$.mp. 8. trial$.ti,ab. 9. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 10. clinical study.ep. 11. experimental study.md. 12. multicenter study.md. 13. (zugewiesen and kontrollgruppe$).ab. 14. randomisiert$.ab,ti. 15. ((zufa?ll$ or randomi$) and (experiment$ or evalu$ or effe?t$) and treat$).mp. 16. (doppelblind$ or doppel‐blind$).ti,ab. 17. or/1‐16 18. major depression/ or anaclitic depression/ or dysthymic disorder/ or endogenous depression/ or postpartum depression/ or reactive depression/ or recurrent depression/ or treatment resistant depression/ 19. atypical depression/ 20. or/18‐19 21. exp Psychotherapy/ (psychotherapy/ or adlerian psychotherapy/ or analytical psychotherapy/ or autogenic training/ or behavior therapy/ or brief psychotherapy/ or client centered therapy/ or cognitive behavior therapy/ or conversion therapy/ or eclectic psychotherapy/ or emotion focused therapy/ or existential therapy/ or experiential psychotherapy/ or expressive psychotherapy/ or eye movement desensitization therapy/ or feminist therapy/ or geriatric psychotherapy/ or gestalt therapy/ or group psychotherapy/ or guided imagery/ or humanistic psychotherapy/ or hypnotherapy/ or individual psychotherapy/ or insight therapy/ or integrative psychotherapy/ or interpersonal psychotherapy/ or logotherapy/ or narrative therapy/ or persuasion therapy/ or primal therapy/ or psychoanalysis/ or psychodrama/ or psychodynamic psychotherapy/ or psychotherapeutic counseling/ or rational emotive behavior therapy/ or reality therapy/ or relationship therapy/ or solution focused therapy/ or supportive psychotherapy/ or transactional analysis/) 22. exp Behavior Therapy/ (behavior therapy/ or aversion therapy/ or conversion therapy/ or dialectical behavior therapy/ or exposure therapy/ or implosive therapy/ or reciprocal inhibition therapy/ or response cost/ or systematic desensitization therapy/) 23. exp Cognitive Behavior Therapy/ (cognitive behavior therapy/ or acceptance and commitment therapy/) 24. exp Cognitive Techniques (cognitive techniques/ or cognitive restructuring/ or cognitive therapy/ or self instructional training/) 25. Schema/ 26. Group Psychotherapy/ (group psychotherapy/ or encounter group therapy/ or therapeutic community/) 27. Milieu Therapy/ 28. Family Therapy/ or Couples Therapy/ or Cotherapy/ or Conjoint Therapy/ or Sex Therapy/ 29. Educational Therapy/ or Psychoeducation/ 30. exp Psychotherapeutic processes/ (psychotherapeutic processes/ or contertransference/ or insight (psychotherapeutic process) or negative therapeutic reaction/ or psychotherapeutic breakthrough/ or psychotherapeutic resistance// or psychotherapeutic transference/ or therapeutic alliance/) 31. exp Psychotherapeutic techniques/ (psychotherapeutic techniques/ or animal assisted therapy/ or autogenic training/ or cotherapy/ or dream analysis/ or guided imagery/ or mirroring/ morita therapy/ or motivational interviewing/ or mutual storytelling technique/ or paradoxical techniques/ or psychodrama/) 32. exp Psychoanalysis/ (psychoanalysis or alderian psychotherapy/ or dream analysis/ or self analysis/) 33 Covert Sensitization/ 34. Behavior Contracting/ 35. exp Biofeedback/ (biofeedback/ or biofeedback training/ or neurofeedback/) 36. Assertiveness Training/ or Behavior Modification/ or Sensitivity Training/ 37. Social Skills Training/ 38. exp Counseling/ 39. exp Contingency Management/ (contingency management/ or token economy programs/) 40. Functional Analysis/ 41. exp Problem Solving/ (problem solving/ or anagram problem solving/ or cognitive hypothesis testing/ or group problem solving/ or heuristics/) 42. exp Relaxation Therapy/ (relaxation therapy/ or progressive relaxation therapy/) 43. Meditation/ or Mindfulness/ 44. Stress Management/ 45. Self Control/ 46. Existential Therapy/ 47. Gestalt Therapy/ 48. exp Jungian Psychology/ (Jungian Psychology/ or Collective Unconscious) 49. Free Association/ 50. Object Relations/ 51. Multimodal Treatment Approach/ 52. Acting Out/ 53. exp Hypnotherapy/ (hypnotherapy/ or age regression/) 54. exp Hypnosis/ (hypnosis/ or age regression (hypnotic) or autohypnosis) 55. exp Creative Arts Therapy/ (creative arts therapy/ or art therapy/ or dance therapy/ or music therapy/ or poetry therapy/ or recreation therapy/) 56. Catharsis/ 57. Crisis Intervention/ 58. Play Therapy/ 59. (third wave or mind train* or person cent* or person* construct*).mp. 60. (person cent* or person* construct*).mp. 61. (activity scheduling or behavioral activation or pleasant event*).mp. 62. ((therap* or psychotherap*) adj1 (abreaction or analytic* or color or colour or compassion or diffusion or distraction or emotion* or interpersonal or inter‐personal* or insight oriented or focus* or functional anal* or metacognitive or nondirective or non directive or problem focus* or process experiential or reciprocal inhibition or reminiscence or socioenvironmental or socio environmental or supportive or transference or transtheoretical)).mp. 63. (freudian or jungian or klenian or rogerian).mp. 64. griefwork.mp. 65. mental healing.mp. 66. or/21‐65 67. (17 and 20 and 66)
Data and analyses
Comparison 1. BT vs all other psychological therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 18 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.09] |
| 1.1 BT vs CBT | 15 | 544 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.83, 1.05] |
| 1.2 BT vs Psychodynamic | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.84, 1.82] |
| 1.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 1.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [0.59, 137.65] |
| 2 Remission | 18 | 694 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.80, 1.04] |
| 2.1 BT vs CBT | 16 | 560 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.75, 1.00] |
| 2.2 BT vs Psychodynamic | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.85, 2.06] |
| 2.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.61, 2.13] |
| 3 Depression severity | 18 | 656 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.20, 0.15] |
| 3.1 BT vs CBT | 15 | 529 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.12, 0.23] |
| 3.2 BT vs Psychodynamic | 2 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.79, 0.05] |
| 3.3 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 3.4 BT vs Integrative | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.82, 0.09] |
| 4 Dropouts for any reason | 15 | 495 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.65, 1.61] |
| 4.1 BT vs CBT | 11 | 363 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [0.68, 3.14] |
| 4.2 BT vs Psychodynamic | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.70] |
| 4.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
| 4.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.08, 12.56] |
| 5 Anxiety | 2 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.68, 0.48] |
| 5.1 BT vs CBT | 1 | 45 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.55, 0.69] |
| 5.2 BT vs Psychodynamic | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.49, 0.72] |
| 5.3 BT vs Integrative | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.76, 0.13] |
| 6 Social adjustment | 2 | 191 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.16, 0.09] |
| 6.1 BT vs CBT | 2 | 145 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.16, 0.14] |
| 6.2 BT vs Psychodynamic | 1 | 46 | Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.35, 0.13] |
Comparison 2. BT‐Lewinsohn vs all other psychological therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 8 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.23] |
| 1.1 Lewinsohn vs CBT | 7 | 233 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.77, 1.20] |
| 1.2 Lewinsohn vs Psychodynamic | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.58, 2.47] |
| 1.3 Lewinsohn vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 2 Dropouts for any reason | 5 | 92 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.13, 1.45] |
| 2.1 Lewinsohn vs CBT | 4 | 68 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 2.56] |
| 2.2 Lewinsohn vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
Comparison 3. BT‐Jacobson vs all other psychological therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.89, 1.34] |
| 1.1 Jacobson vs CBT | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.89, 1.34] |
| 2 Dropouts for any reason | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [0.54, 4.85] |
| 2.1 Jacobson vs CBT | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [0.54, 4.85] |
Comparison 4. BT‐SST/assertiveness vs all other psychological therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 6 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.66, 1.19] |
| 1.1 SST/assertiveness vs CBT | 5 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.56, 1.09] |
| 1.2 SST/assertiveness vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.79, 1.98] |
| 2 Dropouts for any reason | 6 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.58, 2.12] |
| 2.1 SST/assertiveness vs CBT | 4 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 2.33 [0.47, 11.49] |
| 2.2 SST/assertiveness vs Psychodynamic | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.70] |
Comparison 5. BT‐Relaxation vs all other psychological therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 2 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 2.12 [0.07, 64.37] |
| 1.1 Relaxation vs CBT | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.51, 1.04] |
| 1.2 Relaxation vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [0.59, 137.65] |
| 2 Dropouts for any reason | 2 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 2.13 [0.32, 14.17] |
| 2.1 Relaxation vs CBT | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 5.6 [0.32, 98.21] |
| 2.2 Relaxation vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.08, 12.56] |
Comparison 6. BT vs all other psychological therapies (Best/worst case scenario).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response (best case scenario) | 16 | 495 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.29] |
| 1.1 BT vs CBT | 13 | 395 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.88, 1.12] |
| 1.2 BT vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [1.19, 2.59] |
| 1.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 1.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 11.00 [0.74, 163.49] |
| 2 Response (worst case scenario) | 16 | 495 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.80, 1.05] |
| 2.1 BT vs CBT | 13 | 395 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.06] |
| 2.2 BT vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.56, 1.09] |
| 2.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 2.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 4.0 [0.61, 26.12] |
Comparison 7. Sensitivity analysis: BT vs all other psychological therapies (treatment fidelity) .
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 3 | 264 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.92, 1.33] |
| 1.1 BT vs CBT | 2 | 194 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.89, 1.32] |
| 1.2 BT vs Psychodynamic | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.58, 2.47] |
| 1.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 2 Depression severity | 3 | 264 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.42, 0.08] |
| 2.1 BT vs CBT | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.43, 0.16] |
| 2.2 BT vs Psychodynamic | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.84, 0.37] |
| 2.3 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 3 Dropouts for any reason | 2 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.44, 2.66] |
| 3.1 BT vs CBT | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [0.54, 4.85] |
| 3.2 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
Comparison 8. Sensitivity analysis: BT vs all other psychological therapies (excluding imputed data).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.51, 1.04] |
| 1.1 BT vs CBT | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.51, 1.04] |
| 2 Remission | 5 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.60, 1.10] |
| 2.1 BT vs CBT | 4 | 217 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.57, 0.96] |
| 2.2 BT vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.81, 2.79] |
| 3 Depression severity | 15 | 631 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.26, 0.08] |
| 3.1 BT vs CBT | 12 | 489 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.18, 0.19] |
| 3.2 BT vs Psychodynamic | 2 | 108 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.73, 0.03] |
| 3.3 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 3.4 BT vs Integrative | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.82, 0.09] |
Comparison 9. Sensitivity analysis: BT vs all other psychological therapies (pharmacotherapy not allowed).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 4 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.67, 2.07] |
| 1.1 BT vs CBT | 2 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.48, 1.78] |
| 1.2 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 1.3 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [0.59, 137.65] |
| 2 Depression severity | 4 | 71 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.75, 0.48] |
| 2.1 BT vs CBT | 2 | 37 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.42, 0.94] |
| 2.2 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 2.3 BT vs Integrative | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.82, 0.09] |
| 3 Dropouts for any reason | 4 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.17, 2.17] |
| 3.1 BT vs CBT | 2 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
| 3.3 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.08, 12.56] |
Comparison 10. Sensitivity analysis: BT vs all other psychological therapies (excluding other subcategories).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 13 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.84, 1.12] |
| 1.1 BT vs CBT | 12 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.82, 1.10] |
| 1.2 BT vs Psychodynamic | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.58, 2.47] |
| 1.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 2 Depression severity | 13 | 413 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.27, 0.13] |
| 2.1 BT vs CBT | 12 | 343 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.24, 0.19] |
| 2.2 BT vs Psychodynamic | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.84, 0.37] |
| 2.3 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 3 Dropouts for any reason | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 BT vs CBT | 10 | 296 | Risk Ratio (M‐H, Random, 95% CI) | 1.85 [0.68, 5.04] |
| 3.2 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
Comparison 11. Sensitivity analysis: BT vs all other psychological therapies (major depression only).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 5 | 304 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.83, 1.27] |
| 1.1 BT vs CBT | 4 | 194 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.74, 1.22] |
| 1.2 BT vs Psychodynamic | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.84, 1.82] |
| 2 Depression severity | 5 | 281 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.41, 0.08] |
| 2.1 BT vs CBT | 4 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.36, 0.24] |
| 2.2 BT vs Psychodynamic | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.80, 0.05] |
| 3 Dropouts for any reason | 2 | 93 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [0.31, 6.67] |
| 3.1 BT vs CBT | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 4.29 [0.54, 33.85] |
| 3.2 BT vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.37, 1.89] |
Comparison 12. Sensitivity analysis: BT vs all other psychological therapies (fewer than 13 sessions).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 14 | 409 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.81, 1.13] |
| 1.1 BT vs CBT | 11 | 309 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.75, 1.07] |
| 1.2 BT vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.79, 1.98] |
| 1.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 1.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [0.59, 137.65] |
| 2 Depression severity | 14 | 376 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.23, 0.23] |
| 2.1 BT vs CBT | 11 | 295 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.09, 0.38] |
| 2.2 BT vs Psychodynamic | 1 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.08, 0.08] |
| 2.3 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 2.4 BT vs Integrative | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.82, 0.09] |
| 3 Dropouts for any reason | 13 | 321 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.53, 1.46] |
| 3.1 BT vs CBT | 9 | 189 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.31, 4.03] |
| 3.2 BT vs Psychodynamic | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.70] |
| 3.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
| 3.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.08, 12.56] |
Comparison 13. Sensitivity analysis: BT vs all other psychological therapies (excluding studies that replaced dropouts).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 16 | 583 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.83, 1.10] |
| 1.1 BT vs CBT | 13 | 483 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.82, 1.05] |
| 1.2 BT vs Psychodynamic | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.79, 1.98] |
| 1.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 1.4 [0.61, 3.19] |
| 1.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [0.59, 137.65] |
| 2 Depression severity | 16 | 549 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.19, 0.22] |
| 2.1 BT vs CBT | 13 | 468 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.10, 0.29] |
| 2.2 BT vs Psychodynamic | 1 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.08, 0.08] |
| 2.3 BT vs Humanistic | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.16, 0.45] |
| 2.4 BT vs Integrative | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐2.82, 0.09] |
| 3 Dropouts for any reason | 14 | 479 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.68, 1.72] |
| 3.1 BT vs CBT | 10 | 347 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.83, 4.00] |
| 3.2 BT vs Psychodynamic | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.70] |
| 3.3 BT vs Humanistic | 1 | 24 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.11, 2.23] |
| 3.4 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.08, 12.56] |
Comparison 14. BT vs all other psychological therapies (follow‐up within 6 months).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 9 | 356 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.59, 1.01] |
| 1.1 BT vs CBT | 8 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.59, 0.99] |
| 1.2 BT vs Integrative | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [0.59, 137.65] |
| 2 Remission | 8 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 2.1 BT vs CBT | 8 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.98] |
| 3 Depression severity | 9 | 330 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.05, 0.78] |
| 3.1 BT vs CBT | 8 | 322 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.04, 0.81] |
| 3.2 BT vs Integrative | 1 | 8 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.41 [‐4.57, ‐0.25] |
14.3. Analysis.
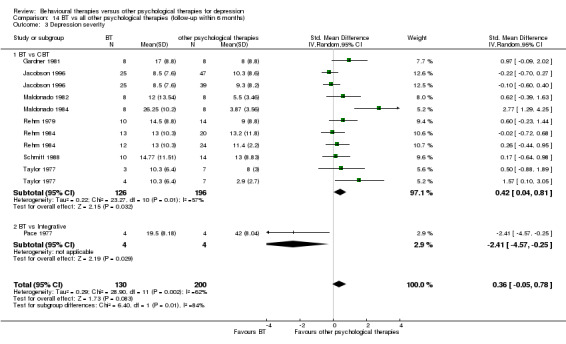
Comparison 14 BT vs all other psychological therapies (follow‐up within 6 months), Outcome 3 Depression severity.
Comparison 15. BT‐Lewinsohn vs CBT‐Cognitive therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 5 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.73, 1.46] |
| 2 Depression severity | 5 | 122 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.45, 0.26] |
| 3 Dropouts for any reason | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only |
Comparison 16. BT‐SST/assertiveness vs CBT‐Self‐Control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response | 2 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.34, 1.43] |
| 2 Depression severity | 2 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.19, 0.92] |
| 3 Dropouts for any reason | 2 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.11, 24.86] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bellack 1981.
| Methods | Design: RCT. Study duration: 12 weeks of initial therapy and 6 months of maintenance treatment Follow‐up: 6 months (end of 6 months' maintenance treatment) | |
| Participants |
Sample size: 125 individuals eligible and randomly assigned into four groups Recruitment: media advertisements and others (participants referred but did not mention from where they were referred) Inclusion criteria: diagnostic classification criteria:DSM‐III Inclusion criteria: rating scales: scores of 7 or higher on Raskin Eligibility Depression Scale Included disorders: major depressive disorder Gender: 125 women Mean age: 30.4 years Country/Ethnicity: USA/90% of samples: white Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: BT‐social skills training/assertiveness training plus pill placebo.
Group 2: social skill training plus amitriptyline: n = 31 Group 3: amitriptyline only: n = 30 Group 4: psychodynamic‐other psychodynamic therapies plus pill placebo
|
|
| Outcomes | BDI 24‐Item NIMH version of HAM‐D Raskin Depression Scale (for eligibility) Lubin Depression Adjective Checklist Hopkins Symptom Checklist Social Ajustment Scale Eysenck Personality Inventory Wolpe‐Lazarus Assertiveness Scale |
|
| Notes | We extracted data mainly from Hersen 1984. We analysed outcomes only for group 1 and group 4 in this trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Assessments performed by Independent researchers "Assessments were conducted by members of research staff who were blind to group assignment"—page 25, 1st paragraph, last sentence |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis performed but high attrition rate and imbalance in attrition rates among arms |
| Selective reporting (reporting bias) | High risk | Not all outcomes reported (Social Ajustment Scale) |
| Researcher allegiance and other conflicts of interest (financial or other) | High risk | Social skill training manual developed by author |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | Therapists qualified: yes Received specialist training: unclear "Social skill training was administered by one of two Ph.D. psychologists"—page 25, 5th paragraph "Therapy was conducted by one of three Ph.D. psychologists"—page 27, 2nd paragraph |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | Unclear risk | Not enough information provided |
Breckenridge 1985.
| Methods | Design: RCT (however, waiting list people re‐randomised after 6 weeks and allocated into treatment arms) Study duration: 12 to 16 weeks Follow‐up: not stated | |
| Participants |
Sample size: 115 individuals eligible and randomly assigned into four groups Recruitment: referred by GP or GP surgery, or referred from outpatient setting and media advertisements Inclusion criteria: diagnostic classification criteria: Research Diagnostic Criteria Inclusion criteria: rating scales: scores of 17 and higher on BDI, and scores of 14 and higher on HAM‐D Included disorders: major depressive disorder Gender: 31 men and 64 women Mean age: 67.07 (SD 5.84) years Country/Ethnicity: USA/European American Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐Lewinsohn's behavioural activation
Group 3: psychodynamic‐relational model (Strupp, Luborsky)
Group 4: waiting list Participants were re‐randomly assigned after 6 weeks and were allocated into other active treatment arms |
|
| Outcomes | BDI HAM‐D Geriatric Depression Scale Brief Symptom Inventory–Depression Brief Symptom Inventory–Global Severity Brief Symptom Inventory–Anxiety Global Assessment Scale Brief Psychiatric Rating Scale Automatic Thought Questionnaire Young Loneliness Inventory Social Ajustment Scale Behavioral, Cognitive and Avoidance Coping scales in the Health and Daily Living Questionnaire Older Persons Pleasant Events Schedule |
|
| Notes | We extracted data mainly from Thompson 1987 and Gallagher‐Thompson 1990. Outcomes of groups 1, 2 and 3 were analysed Investigators re‐randomly assigned participants who were originally allocated to "delayed‐treatment condition (DTC)" into therapy groups after 6 weeks and reported only combined outcomes However, the proportion of re‐randomly assigned participants was less than 20% of the whole randomly assigned sample (20 of 115), and we concluded this study was eligible |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants who dropped out from the study excluded from the analysis. Only completer analysis performed on 91 of 115 randomly assigned participants |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Researcher allegiance and other conflicts of interest (financial or other) | High risk | Manuarl of behavioural therapy written by the authors (Gallagher and Thompson) |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | Therapists qualified: unclear Received specialist training: yes "All were doctoral level psychologists with at least 1 year of specialised training in the modality they used "—page 385, right column, 3rd paragraph, Thompson 1987 |
| Treatment fidelity | Low risk | Monitored against a manual: unclear Monitored with a scale: yes Sessions audiotaped: yes "At least one videotaped treatment session per patient (selected from near the midpoint of therapy) was evaluated by raters at the centres of origination of each therapy modality"—page 386, left column, 1st paragraph, Thompson 1987 |
| Other bias | High risk | Neither number of participants originally allocated to each treatment first, nor number later re‐randomly assigned from the waiting list into treatment groups was reported |
Comas‐Diaz 1981.
| Methods | Design: RCT Study duration: 4 weeks Follow‐up: 5 weeks | |
| Participants |
Sample size: 26 individuals eligible and randomly assigned into three groups Recruitment: referred by local community agencies Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: BDI and HAM‐D. Threshold unclear Included disorders: stated as “Depression” only Gender: 26 women Mean age: 38 years Country/Ethnicity: USA/Puerto Rican woman Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐Lewinsohn's behavioural activation
Group 3: waiting list n = 10 |
|
| Outcomes | BDI HAM‐D Depression Behavior Rating Scale (developed for this study) |
|
| Notes | We analysed outcomes only for groups 1 and 2 of this trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated how incomplete outcome data were treated |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | Therapists qualified: unclear Received specialist training: unclear |
| Treatment fidelity | Low risk | Monitored against a manual: yes Monitored with a scale: yes Sessions audiotaped: yes "Potential experimenter bias was evaluated by rating 30 3 minute randomly selected segments from the audio‐taped sessions"—page 629, 2nd paragraph "Results suggests that the therapists followed the treatment protocol" "The sessions were distinguishable by an observer familiar with the written treatment manual"—page 629, 2nd paragraph |
| Other bias | Unclear risk | Not enough information provided |
Gallagher 1979.
| Methods | Design: RCT Study duration: 5 weeks Follow‐up: 5 weeks | |
| Participants |
Sample size: 28 individuals eligible and randomly assigned into two groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: Minnesota Multiphasic Personality Inventory–Depression (MMPI‐D) scale at least two SD above the mean Included disorders: major depressive disorder Gender: unclear Mean age: 67.65 (SD 5.84) years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: BT‐Lewinsohn's behavioural activation
Group 2: humanistic‐non‐directive/supportive therapies
|
|
| Outcomes | MMPI‐D BDI Zung Self‐rating Depression Scale Depression Scale of the Symptom Checklist (SCL)‐90 Dysfunctional Attitude Scale Cognitive Distortion Vignettes Interpersonal Events Schedule |
|
| Notes | Measured outcomes not reported by authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | Observer‐rated outcomes not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number of dropouts in each group and how incomplete outcome data were treated not stated |
| Selective reporting (reporting bias) | High risk | Mean and SD in each scale not reported |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Low risk | Therapists qualified: yes Received specialist training: yes "The therapy were conducted by two therapists.....They had been practicing clinical psychologists for over 10 years"—page 37, last paragraph "In addition, several training sessions were held in advance of the project to clarify their specific questions"—page 38, 1st paragraph |
| Treatment fidelity | Unclear risk | Monitored against a manual: yes Monitored with a scale: yes Sessions audiotaped: no "Three undergraduate students at the University of Southern California were recruited and trained to rate various aspects of therapist"—page 39, second paragraph "Observation[s] were obtained from behind one‐way mirror"—page 40, 1st paragraph "In addition, to measure the extent to which therapists were following the specific treatment protocols, observer counted specific therapist behaviours...."—page 53, 1st paragraph |
| Other bias | Unclear risk | Not enough information provided |
Gardner 1981.
| Methods | Design: RCT Study duration: 6 weeks Follow‐up: 5 weeks | |
| Participants |
Sample size: 17 individuals eligible and randomly assigned into two groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: BDI. Threshold not described Included disorders: stated as "Depression" only Gender: 7 men and 9 women Mean age: unclear Country/Ethnicity: Australia/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: BT‐other behaviour therapies
Group 2: CBT‐rational emotive behaviour therapy
|
|
| Outcomes | BDI Zung Self‐rating Depression Scale Tennessee Self‐concept |
|
| Notes | Unpublished data: pretreatment mean and SD | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | Unclear risk | Not enough information provided |
Jacobson 1996.
| Methods | Design: RCT Study duration: 16 weeks Follow‐up: 6, 12, 18, 24 weeks | |
| Participants |
Sample size: 152 individuals eligible and 149 individuals randomly assigned into three groups Recruitment: media advertisement and other (health maintenance organisation) Inclusion criteria: diagnostic classification criteria:DSM‐III‐R Inclusion criteria: rating scales: scores of 20 or higher on BDI, and scores of 14 or higher on 17‐item HAM‐D Included disorders: major depressive disorder and dysthymia Gender: 38 men and 113 women Mean age: 38.0 years Country/Ethnicity: USA/Among 151 participants, 128 (84.7%) were Caucasian, 6 (3.9%) were Native American, 4 (3.1%) were African American, 3 (2.3%) were Hispanic and 3 (2.3%) were Asian Pharmacotherapy allowed during the study: unclear |
|
| Interventions |
Group 1: BT‐Jacobson's behavioural activation
Group 2: CBT‐other cognitive‐behavioural therapies
Group 3: CBT‐cognitive therapy
|
|
| Outcomes | BDI HAM‐D |
|
| Notes | We extracted data mainly from Jacobson 1996 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Outcome assessors blind "Raters were also not informed of the treatment condition of the participant"—page 296, right column 1st paragraph |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 149 of 152 participants analysed; low attrition rate |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | High risk | Apparent allegiance of researcher for behavioural activation therapy because therapy manual was developed by first author, Jacobson |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Low risk | Therapists qualified: yes Received specialist training: yes "Three licensed clinical psychologists and one licensed social worker served as therapists" " All therapists participated previously in controlled trials of CBT and each underwent a pilot training period for the current study"—page 317, 3rd paragraph, Addis 2000 |
| Treatment fidelity | Low risk | Monitored against a manual: yes Monitored with a scale: yes Sessions audiotaped: yes "The measure of treatment integrity used in the present study was a modified version of the National Institute of Mental Health Collaborative Study Psychotherapy Rating Scale (CSPRS; Hollon, Evans, Elkin, Lowery, 1984). Items included both techniques designated by the treatment manual and those prohibited or proscribed [by] it"—page 298, right column, 1st paragraph "Raters listened to a tape of the therapy sessions..."—page 298, right column, 2nd paragraph |
| Other bias | High risk | Number of people included in the analysis different from paper to paper |
Kelly 1982.
| Methods | Design: RCT Study duration: 6 weeks Follow‐up: not stated | |
| Participants |
Sample size: 24 individuals eligible and randomly assigned into three groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria:DSM‐III Inclusion criteria: rating scales: scores of 15 or higher on BDI Included disorders: major depressive disorder Gender: 4 men and 16 women Mean age: 33.9 years Country/Ethnicity: Greece/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: Lewinsohn's behavioural activation
Group 2: CBT‐rational emotive behaviour therapy
Group 3: control‐psychological placebo
|
|
| Outcomes | BDI Social Avoidance and Scale DSM‐III Checklist Irrational Beliefs Test Pleasant Event Schedule |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate (4 of 24) but only completer analysis performed by authors |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Low risk | Investigators checked therapist expectancy for improvement of symptoms and reported that ratings were similar across groups "The second category of ratings involved the consistency of therapist across group, empathy, therapist expectancy for improvement and therapist credibility"—page 44, 3rd paragraph |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: no "Two masters level clinical psychology graduate students served as therapists"—page 36, 2nd paragraph |
| Treatment fidelity | Unclear risk | Monitored against a manual: yes Monitored with a scale: yes Sessions audiotaped: unclear "As a check on the manipulation of the investigation, several ratings were obtained..."—page 41, 4th paragraph |
| Other bias | Unclear risk | Not enough information provided |
Kelly 1983.
| Methods |
Design: RCT. Cross‐over design
Study duration: 10 weeks. Although the total intervention lasted 10 weeks, researchers switched the content of two interventions at the beginning of week 7. Therefore we extracted only data until the end of week 6 Follow‐up: not stated |
|
| Participants |
Sample size: 16 individuals eligible and randomly assigned into two groups Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: scores of 10 or higher and 40 or lower on BDI Included disorders: stated as “Depression” only Gender: 5 men and 11 women Mean age: not stated Country/Ethnicity: USA/unclear Pharmacotherapy during the study: not allowed |
|
| Interventions |
Group 1: Lewinsohn's behavioural activation
Group 2: CBT‐cognitive therapies
|
|
| Outcomes | BDI | |
| Notes | This is a study of cross‐over design; we extracted data only from the first CBT or BT therapy term | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "Therapists for this study were six doctoral students in the Counseling and Human Systems Program at Florida State University. They all received academic training in models... in the therapeutic approach being employed in this study"—page 53, 2nd paragraph |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | Unclear risk | Not enough information provided |
Lapointe 1980.
| Methods | Design: cluster RCT Study duration: 6 weeks Follow‐up: 2 weeks | |
| Participants |
Sample size: 41 individuals eligible and randomly assigned into three groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: scores between 15 and 31 on BDI Included disorders: stated as “Depression” only Gender: 33 (100%) women Mean age: 35.1 years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: BT‐social skills training/assertiveness training
Group 2: psychodynamic‐other psychodynamic therapies
Group 3: CBT‐cognitive therapy
|
|
| Outcomes | BDI Personality Data Form Rathus Assertiveness Schedule |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Cluster randomisation trial; allocation determined on the basis of available time "In both cases, groups are formed on the basis of available times and treatment conditions randomly assigned to groups"—page 314, right column, 3rd paragraph |
| Allocation concealment (selection bias) | High risk | Allocation apparently not concealed because allocation was determined on the basis of available time "In both cases, groups are formed on the basis of available times and treatment conditions randomly assigned to groups"—page 314, right column, 3rd paragraph |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychotherapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of 41 participants, 33 participants completed; completer analysis performed for only 33 completers |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information about therapist allegiance |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "At the end of four weeks...groups which were led by a female intern who had had 190 hours of individual and 100 hours of group therapy experience" "After four additional weeks,...the second set of groups led by the author who had had 105 hours of individual and 120 hours of group therapy experience"—page 314, right column, 3rd paragraph |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | Unclear risk | Not enough information provided |
Maldonado 1982.
| Methods | Design: RCT Study duration: unclear Follow‐up: 3 months | |
| Participants |
Sample size: 24 individuals randomly assigned into three groups Recruitment: self‐referral Inclusion criteria: diagnostic classification criteria: other ("neurotic depression") Inclusion criteria: rating scales: not stated Included disorders: stated as “Depression” only Gender: unclear Mean age: unclear Country/Ethnicity: Spain/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐social skills training/assertiveness training
Group 3: others‐drug only n = 8 |
|
| Outcomes | BDI HAM‐D Zung Self‐rating Depression Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear whether ITT or completer analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | Unclear risk | Not enough information provided |
Maldonado 1984.
| Methods | Design: RCT Study duration: unclear Follow‐up: 3 months | |
| Participants |
Sample size: 24 individuals randomly assigned into three groups Recruitment: self‐referral Inclusion criteria: diagnostic classification criteria: other ("neurotic depression") Inclusion criteria: rating scales: score ≤ 20 on BDI and HAM‐D, score ≤ 40 on Zung Self‐Rating Depression Scale Included disorders: stated as “Depression” only Gender: unclear Mean age: unclear Country/Ethnicity: Spain/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: CBT‐other cognitive‐behavioural therapy
Group 2: BT‐social skills training/assertiveness training
Group 3: others‐drug only n = 8 |
|
| Outcomes | BDI HAM‐D Zung Self‐rating Depression Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear whether ITT or completer analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | Unclear risk | Not enough information provided |
McNamara 1986.
| Methods | Design: RCT Study duration: 8 or 10 weeks Follow‐up: 2 months | |
| Participants |
Sample size: 50 individuals eligible and randomly assigned into four groups Recruitment: other (counselling centre of a large southwestern university) Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: BDI score of 18 or higher at intake and 16 or lower at pretest, and HAM‐D score of 20 or higher at pretest Included disorders: stated as “Depression” only Gender: 11 men and 29 women Mean age: 23 years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐Lewinsohn's behavioural activation
Group 3: CBT‐other cognitive‐behavioural therapies
Group 4: humanistic‐person‐centred therapy (Rogerian)
|
|
| Outcomes | BDI HAM‐D Automatic Thoughts Questionnaire Cognitive Scale Recalled Cognitions Self‐evaluated Social Skills Pleasant Events Schedule Behavioral Scale Observer‐evaluated Social Skills |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No information provided about the level of attrition in each group or how this was treated |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention because treatments were not developed by the authors "This condition was derived from the work of Lewinsohn and his associates"—page 26, left column, 6th paragraph "This condition was derived from the work of Lewinsohn and his associates"—page 26, left column, 1st paragraph "All counsellors were instructed to adhere carefully to Chapter 2 of Client‐Centered Therapy (Rogers 1951)"—page 26, right column, 3rd paragraph |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | Therapists had interest in specific treatment but declared that they would follow treatment procedures "At the time of recruitment, seven counsellors were self‐described as 'cognitive‐behavioural' in orientation; the eighth preferred the term "interpersonal" (cf. Strong 1968). All counsellors had expressed complete willingness to follow the exact procedures required by this study, despite any idiosyncratic preferences that might occur"—page 25, left column, 4th paragraph |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "Seven doctoral interns in clinical and counselling psychology and one master's level social worker (4 men and 4 women) served as counsellors"—page 25, left column, 4th paragraph |
| Treatment fidelity | Low risk | Monitored against a manual: yes Monitored with a scale: unclear Sessions audiotaped: yes "They were also provided with treatment manuals and were closely monitored (via audiotapes) for adherence to the appropriate intervention throughout the course of the study"—page 25, 4th paragraph |
| Other bias | Unclear risk | Not enough information provided |
Pace 1977.
| Methods | Design: RCT Study duration: 3.5 weeks Follow‐up: 4, 8, 13 weeks and 10 months | |
| Participants |
Sample size: 18 individuals randomly assigned into three groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: scores higher than 20 on BDI Included disorders: stated as “unipolar depression” only Gender: 18 women Mean age: 38.4 years Country/Ethnicity: Australia/unclear Pharmacotherapy during the study: not allowed |
|
| Interventions |
Group 1: control‐psychological placebo
Group 2: BT‐relaxation therapy
Group 3: integrative‐other integrative therapy approaches
|
|
| Outcomes | Zung Self‐rating Depression Scale Depression Adjective Checklist Abbreviated version of Sentence Completions Method State‐Trait‐ Anxiety Inventory Sleep Measure Block Design section (B‐D) of the Wechsler Adult Intelligence Scale Edwards Personal Preference Schedule (EPPS) |
|
| Notes | Pace 1977 included three trials. We extracted data from one of the trials in the dissertation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychotherapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome of our interest reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropping out of 2 of 18 participants by end of treatment; only the data of completers analysed |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | High risk | Apparent allegiance of author for BT‐relaxation therapy Manual for both treatments written by the author, but integrative therapy stated to be used as a control "SAT and RT were compared to a control treatment called 'Cognitive‐ernotional therapy' (CET)"—page 95, 3rad paragraph "The aim of CET was to provide a treatment which would have face validity and which would control for the non‐specific effects of therapy (e.g. support and understanding)"—page 98, 3rd paragraph |
| Therapist allegiance and other conflicts of interest (financial or other) | High risk | Therapy provided by he author. Reasons for allegiance of therapist to BT‐relaxation therapy similar to reasons for researcher allegiance |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: no "All three treatments were conducted by two therapists, namely the experimenter and the co‐researcher who had assisted in the subject selection process"—page 102, 3rd paragraph |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | Unclear risk | Not enough information provided |
Padfield 1975.
| Methods | Design: RCT Study duration: 12 weeks Follow‐up: not stated | |
| Participants |
Sample size: 24 eligible individuals randomly assigned into two groups Recruitment: referred by GP or GP surgery, media advertisement and other Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: Zung Self‐Rating Depression Scale (no information about threshold). Scores above cut‐off score for mild depression (1.50) on Grinker Interview Checklist Included disorders: stated as “Depression” only Gender: 24 (100%) women Mean age: unclear Country/Ethnicity: USA/unclear Pharmacotherapy during the study: not allowed |
|
| Interventions |
Group 1: humanistic‐non‐directive/supportive therapies
Group 2: BT‐Lewinsohn's behavioural activation
|
|
| Outcomes | Zung Self‐rating Depression Scale Grinker Interview Checklist Pleasant Events Schedule Self‐reported Daily Mood Tracking |
|
| Notes | We extracted data mainly from the dissertation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequence adequately generated "After the women had volunteered for participants ....every two clients in order of appearance were randomly assigned to counselling with the relationship model (group A) or the relationship model plus the behavioral model (Group B) by flipping a coin"—page 36, 2nd paragraph |
| Allocation concealment (selection bias) | High risk | Allocation of the next woman suspected by investigators "After the women had volunteered for participants....every two clients in order of appearance were randomly assigned to counselling with the relationship model (group A) or the relationship model plus the behavioral model (Group B) by flipping a coin"—page 36, 2nd paragraph |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial. |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Outcome assessors blind "A psychiatric nurse, after listening to the tape without knowing which counselling approach the woman was receiving, made her assessment"—page 46, 1st paragraph |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data for only one of 24 "Posttesting was completed in entirety with 23 women"—page 210, Padfield 1976 |
| Selective reporting (reporting bias) | High risk | Detail of suicide attempts during the study not reported "Two of these attempts (suicide attempt) took place during the time of study"—page 35, 1st paragraph |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | No information about qualification or training provided |
| Treatment fidelity | Low risk | Monitored against a manual: unclear Monitored with a scale: yes Sessions audiotaped: yes "There were 203 counselling sessions and all except two were recorded"—page 47, 4th paragraph "To check on the possibility of experimenter bias 11 rating scale focusing on relevant treatment variables were devised"—page 48, 1st paragraph |
| Other bias | Unclear risk | Not enough information provided |
Rehm 1979.
| Methods | Design: RCT Study duration: 6 weeks Follow‐up: 6 weeks | |
| Participants |
Sample size: 27 individuals eligible and randomly assigned into two groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: MMPI scale score of F 80 or less, L 60 or less, D 70 or more, D > Hy, D > Pt and D among the highest two elevations on the profile Included disorders: stated as “Depression” only Gender: 27 women Mean age: unclear Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐self‐control therapy
Group 2: BT‐social skills training/assertiveness training
|
|
| Outcomes | BDI MMPI–Depression Pleasant Events Schedule Self‐evaluation Questionnaire Common Associates Test Concepts Test Wolpe‐Lazarus Assertion Scale |
|
| Notes | Unpublished data: mean and SD on MMPI‐D and BDI at pretreatment and post‐treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome of our interest reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates different between groups (none of 14 in CBT group, 3 of 13 in BT group) but only the data of completers analysed |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | High risk | Apparent allegiance of researcher for self‐control therapy because authors developed this intervention "Fuchs and Rehm (1977) developed and evaluated a group administered self‐control behavior therapy programme designed to remediate deficits in self‐control identified with depression"—page 429, 1st paragraph |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: unclear "All four therapists were graduate students in a Ph.D. programme in Clinical Psychology"—page 431, 2nd paragraph |
| Treatment fidelity | Unclear risk | No information provided about monitoring |
| Other bias | Unclear risk | Not enough information provided |
Rehm 1984.
| Methods | Design: RCT Study duration: 10 weeks Follow‐up: 6 months | |
| Participants |
Sample size: 149 individuals eligible, and 147 individuals randomly assigned into three groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: Research Diagnostic Criteria Inclusion criteria: rating scales: MMPI‐D 70 or higher; BDI scores 20 or higher Included disorders: major depressive disorder Gender: 104 women Mean age: 38.6 years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: BT‐other
Group 2: CBT‐other
Group 3: CBT‐self‐control
|
|
| Outcomes | BDI MMPI‐D 21‐Item HAM‐D Raskin Three‐item Depression Scale (RDS)–Interviewer Rating Brief Hopkins Psychiatric Rating Scale Revised Symptom Checklist Social Adjustment Scale–Self‐report Self‐control Questionnaire Self‐control Schedule Dysfunctional Attitude Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random sequence generation not adequately conducted "Assignments of groups were made to balance the order with which therapists began groups in different conditions with meeting time"—page 61, right column, 3rd paragraph |
| Allocation concealment (selection bias) | High risk | Allocation apparently not concealed "Assignments of groups were made to balance the order with which therapists began groups in different conditions with meeting time"—page 61, right column, 3rd paragraph |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Raters blind to the allocation "Interviewers were blind to all test results and to subjects' experimental conditions"—page 61, right column, 2nd paragraph |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis performed by authors although 43 of 147 dropped out |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "Three therapists were doctoral‐level psychologists and one was an advanced clinical psychology graduate student"—page 61, right column, 3rd paragraph |
| Treatment fidelity | Unclear risk | Monitored against a manual: unclear Monitored with a scale: no Sessions audiotaped: yes "We randomly selected 72 tape segments by therapy tape‐numbers and by tape recorder counter‐settings"—page 62, right column, 4th paragraph |
| Other bias | Unclear risk | Not enough information provided |
Rude 1986.
| Methods | Design: cluster RCT. Cross‐over design Study duration: 6 weeks Follow‐up: 2 to 3 months | |
| Participants |
Sample size: 51 individuals eligible and 32 individuals assigned to eight groups of four members each; each group assigned to CBT or BT Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: Research Diagnostic Criteria Inclusion criteria: rating scales: BDI score 14 or higher; MMPI‐Depression scale score 70 or higher and one of the two highest scores on the profile; Depression score > Hysteria and Psychasthenia scores; Lie and Validity scores < 70 Included disorders: major depressive disorder, depressive disorder not otherwise specified (including minor depression) Gender: 48 women Mean age: 40 years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐self‐control therapy (followed by BT‐assertiveness training)
Group 2: BT‐social skills training/assertiveness training (followed by CBT‐self‐control therapy)
|
|
| Outcomes | BDI Rathus Assertiveness Schedule Self‐control Schedule Self‐control Questionnaire Cognitive Self‐management |
|
| Notes | This is a study of cross‐over design, and we extracted data only from the first CBT or BT therapy term | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome of our interest reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In both groups, 2 of 16 individual outcomes missing. Proportion apparently equal and relatively low |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: unclear "Four doctoral level counselling psychology students were to instruct two groups each"—page 31, 2nd paragraph |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | High risk | Cluster‐randomised trial, but intracluster correlation between therapists not reported for the outcome |
Sanchez 1980.
| Methods | Design: RCT. Study duration: 5 weeks Follow‐up: 1 month | |
| Participants |
Sample size: 32 individuals randomly assigned into two groups Recruitment: referred from outpatient setting Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales:
Included disorders: major depressive disorder (MDD), depressive disorder NOS (including minor depression) Gender: 11 men and 21 women Mean age: unclear Country/Ethnicity: USA/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: BT‐social skills training/assertiveness training
Group 2: psychodynamic‐other psychodynamic therapies
|
|
| Outcomes | BDI MMPI‐D Index of General Affect Domains of Satisfaction Assertive Inventory: Inventory Discomfort, Response Probability |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcomes reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only data of completers analysed, although 5 of 16 dropped out of both groups |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "Each of the four groups was led by a different therapist, each an advanced graduate student in clinical psychology"—page 527, 5th paragraph |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | High risk | More than half of participants in the psychodynamic therapy group placed on medication after start of treatment |
Schmitt 1988.
| Methods | Design: RCT Study duration: 12 weeks Follow‐up: 3 and 6 months | |
| Participants |
Sample size: 40 individuals eligible and randomly assigned into three groups Recruitment: media advertisements Inclusion criteria: diagnostic classification criteria: Research Diagnostic Criteria Inclusion criteria: rating scales: 14 or greater on HRDS; 14 and above on BDI Included disorders: major depressive disorder Gender: 11 men and 29 women Mean age: 46.24 years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐problem‐solving therapy
Group 2: BT‐social skills training/assertiveness training
Group 3: waiting list n = 11 |
|
| Outcomes | BDI HAM‐D Automatic Thoughts Questionnaire Problem Solving Inventory Pleasant Events Schedule Rathus Assertiveness Scale Self‐control Schdule Attributional Style Questionnaire |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates different between groups (1 of 15 in problem solving, 4 of 14 in social skills training); only the data of completers analysed by authors |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "Therapists underwent extensive training procedures"—page 40, 2nd paragraph "Therapy was conducted four doctoral students (two advanced doctoral candidates with approximately three years of supervised psychotherapy experience and two first year doctoral students)"—page 40, 2nd paragraph |
| Treatment fidelity | Unclear risk | No information provided about monitoring |
| Other bias | Unclear risk | Not enough information provided |
Shaw 1977.
| Methods | Design: RCT Study duration: 4 weeks Follow‐up: 1 month | |
| Participants |
Sample size: 32 individuals eligible and randomly assigned into four groups Recruitment: self‐referral and other (referral from university's student health service) Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales
Gender: 10 men and 22 women Mean age: 20.1 years Country/Ethnicity: Canada/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐Lewinsohn's behavioural activation
Group 3: attention placebo
Group 4: waiting list n = 8 |
|
| Outcomes | BDI HAM‐D Visual Analogue Scale |
|
| Notes | We extracted the data only from trial groups 1 and 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Assessors blinded "The raters were blinded to the subjects’ treatment group assignment"—page 545, right column, 5th paragraph |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants for whom data were analysed not reported |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of the researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | High risk | Apparent allegiance of therapists for BT‐Lewinsohn’s behavioural activation "The theoretical orientation of his training was strongly behavioral with the result that he was most experienced with behavior therapy"—page 546, left column, 4th paragraph |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: unclear "The therapist (experimenter) was a doctoral‐level clinical psychology graduate student"—page 546, left column, 4th paragraph |
| Treatment fidelity | Low risk | Monitored against a manual: yes Monitored with a scale: yes Sessions audiotaped: yes "All session[s] were audio taped for later evaluation"—page 546, left column, 2nd paragraph "Also, the therapist's behavior and adherence to the treatment protocols were monitored and rated by a third independent rater"—page 546, left column, 3rd paragraph |
| Other bias | Unclear risk | Not enough information provided |
Skinner 1983.
| Methods | Design: RCT Study duration: 4 weeks Follow‐up: not stated | |
| Participants |
Sample size: 50 individuals eligible and randomly assigned into four groups Recruitment: media advertisements Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: scores of 13 or higher on BDI Included disorders: stated as “Depression” only Gender: 13 men and 27 women Mean age: 34 (SD 11.22) years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐Lewinsohn's behavioural activation
Group 3: others
Group 4: attention placebo
|
|
| Outcomes | BDI Pleasant Event Schedule (PES) |
|
| Notes | We extracted data only from trial groups 1 and 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated scale used |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate (10 of 50 randomly assigned participants withdrew); only the data of completers analysed by authors |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes All therapy conducted by one experimenter who had been trained; experimenter apparently the author—a doctoral level psychological student |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | Unclear risk | Not enough information provided |
Taylor 1977.
| Methods | Design: RCT Study duration: 4 weeks Follow‐up: 5 weeks | |
| Participants |
Sample size: 28 individuals eligible and randomly assigned into four groups Recruitment: media advertisements Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: scores of 13 or higher on BDI, T scores not less than 70 on D‐30 scale; 30 of original 60 items of MMPI‐D scale taken by Dempsey (1964) Included disorders: stated as “Depression” only Gender: 8 men and 20 women Mean age: 22.4 (SD 2.6) years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: not allowed |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐Lewinsohn's behavioural activation
Group 3: CBT‐other cognitive‐behavioural therapies
Group 4: waiting list n = 7 |
|
| Outcomes | BDI Visual Analogue Scale Self‐acceptance and Self‐esteem |
|
| Notes | Unpublished data: dropouts | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Unclear risk | No observer‐rated outcome reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Treatment completed by all participants; no missing data |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: unclear "All treatments (six 40‐min sessions) were administered individually by a single therapist (the senior author)"—page 62, 6th paragraph |
| Treatment fidelity | Unclear risk | No information provided about monitoring |
| Other bias | Unclear risk | Not enough information provided |
Wetzel 1992.
| Methods | Design: RCT Study duration: 16 weeks Follow‐up: not stated | |
| Participants |
Sample size: 43 individuals eligible and 37 individuals randomly assigned into three groups Recruitment: media advertisement Inclusion criteria: diagnostic classification criteria: Feighner criteria Inclusion criteria: rating scales: scores of 14 or higher on BDI; scores of 10 or higher on 17‐item HAM‐D Included disorders: stated as “unipolar depression” only Gender: 11 men and 26 women Mean age: 39.4 (SD 10.9) years Country/Ethnicity: USA/36 white, 1 black Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: CBT‐cognitive therapy
Group 2: BT‐relaxation therapy
Group 3: other‐drug only
|
|
| Outcomes | BDI HAM‐D |
|
| Notes | We extracted the data only from trial groups 1 and 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequence adequately generated "Patients were randomly assigned to one of the three treatments according to a table of random numbers generated for that purpose"—page 406, 3rd paragraph |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | High risk | Outcome assessors not blind "The research coordinator... administered the Hamilton Scale. She was not blind to treatment assignment"—page 406, 5th paragraph |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates different between interventions (none of 12 in CBT, 3 of 14 in BT); only completer analysis performed by author |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Low risk | Therapists qualified: yes Received specialist training: yes "Therapists were six psychologists, one social worker, and one psychiatrist"—page 406, 6th paragraph "The psychologists had at least three years of supervised clinical experience, were doctoral candidates...or held a Ph.D. degree"—page 407, 1st paragraph |
| Treatment fidelity | Unclear risk | Monitored against a manual: unclear Monitored with a scale: unclear Sessions audiotaped: yes "Cognitive behavioral therapy therapists received pretreatment supervision and training in the theory and practice of cognitive therapy to Beck's model of cognitive behavioral therapy"—page 407, 4th paragraph "Therapists were trained in progressive muscle relaxation using the format described by Bernstein and Borkovec (1973)"—page 407, 5th paragraph "All therapeutic sessions were audio taped"—page 408, 1st paragraph |
| Other bias | Unclear risk | Not enough information provided |
Wilson 1983.
| Methods | Design: RCT Study duration: 8 weeks Follow‐up: 5 months | |
| Participants |
Sample size: 29 individuals eligible and 25 individuals randomly assigned into 3 groups Recruitment: media advertisements Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales: scores of 17 or higher on BDI Included disorders: stated as “Depression” only Gender: 5 men and 20 women Mean age: 39.5 years Country/Ethnicity: Australia/unclear Pharmacotherapy during the study: allowed |
|
| Interventions |
Group 1: BT‐ Lewinsohn's behavioural activation
Group 2: CBT‐cognitive therapy
Group 3: waiting list n = 9 |
|
| Outcomes | BDI Irrational Beliefs Test Mood Ratings 17‐Item Hamilton Depression Rating Scale Pleasant Events Schedule Cognition Schedule |
|
| Notes | Dropouts were replaced. However, less than 20% of participants were replaced, so this study was included in our analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Assessor blinded "Interviews were tape‐recorded and independently assessed by one rater who was blind to both treatment condition and assessment occasion"—page 115, 4th paragraph |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts (4 of 25 randomly assigned sample) replaced by new participants |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of the researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | No information about qualifications or training provided |
| Treatment fidelity | Unclear risk | No information about monitoring or supervision provided |
| Other bias | High risk | During treatment, dropouts replaced "Three subjects in the cognitive therapy condition and 1 subject in the behavior therapy condition discontinued treatment. These subjects were replaced in order to maintain equivalent cell frequencies"—page 114, 3rd paragraph |
Zeiss 1979.
| Methods | Design: RCT Study duration: 16 weeks Follow‐up: not stated | |
| Participants |
Sample size: 66 individuals eligible and randomly assigned to 3 groups, and again randomly assigned to 2 groups (immediate therapy or delayed therapy) Recruitment: announcement at University of Oregon and in surrounding metropolitan area Inclusion criteria: diagnostic classification criteria: unclear Inclusion criteria: rating scales
Included disorders: major depressive disorder Gender: 20 men and 46 women Mean age: 33.9 years Country/Ethnicity: USA/unclear Pharmacotherapy during the study: unclear |
|
| Interventions |
Group 1: BT‐social skills training/assertiveness training
Group 2: waiting list
Group 3: CBT‐other cognitive‐behavioural therapies
Group 4: waiting list
Group 5: BT‐Lewinsohn's behavioural activation
Group 6: waiting list
|
|
| Outcomes | MMPI‐D Interpersonal Events Schedule Social Skill Measures Based on Group Interaction Coder Ratings of Social Skill, Peer Ratings of Social Skill Pleasant Events Schedule Cognitive Events Schedule Personal Beliefs Inventory Subjective Probability Questionnaire Corder Ratings of Cognitive Style, Peer Ratings of Cognitive Style |
|
| Notes | We extracted the data only from trial groups 1, 3 and 5 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Impossible to blind participants in a psychological therapy trial |
| Blinding of outcome assessment for the OBSERVER‐RATED scale (detection bias) | Low risk | Assessors were blinded "Verval coders were blind to the experimental condition of participants"—page 431, left column, 3rd paragraph |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate (22 of 66); number of dropouts in each group not reported; data of completers analysed by author |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Researcher allegiance and other conflicts of interest (financial or other) | Low risk | No apparent allegiance of researcher for any intervention |
| Therapist allegiance and other conflicts of interest (financial or other) | Unclear risk | No information provided |
| Therapist qualifications | High risk | Therapists qualified: no Received specialist training: yes "Therapists for this study were six graduate students in counselling psychology and two counselling psychologists with master's degrees"—page 432, left column, 6th paragraph |
| Treatment fidelity | Unclear risk | No information about monitoring provided |
| Other bias | Unclear risk | Not enough information provided |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Barrera 1979 | This study compared BT with waiting list |
| Bowers 1990 | Quasi‐randomisation was used |
| Brand 1992 | Participants were inpatients |
| Broota 1990 | This study compared BT with no treatment |
| Cullen 2002 | This study compared BT with waiting list |
| Gallagher 1982 | The author added non‐randomly assigned members to supplement the dropouts (8 of 30) |
| Hayman 1980 | This study compared BT with waiting list |
| Hopko 2003b | Participants were inpatients |
| Losada 2011 | No threshold for baseline depression severity was noted |
| Mclean 1979 | The author replaced participants to supplement the dropouts (37 of 154), and it was unclear whether those participants were randomly assigned |
| Reynolds 2011 | Mean depression score at baseline assessment was in the normal range |
| Rokke 1999 | Not all participants were randomly assigned to treatment |
| Snarski 2011 | Participants were elderly inpatients with mild to moderate cognitive impairment |
| Turner 1979 | Quasi‐randomisation was used |
| Wilson 1982 | This study compared BT with psychological placebo |
Contributions of authors
Kiyomi Shinohara extracted the data, contributed to development of the revised data extraction form, brought together the evidence for this review and analysed the data and wrote the first draft of the present review.
Mina Honyashiki and Hissei Imai extracted the data, contributed to the development of the revised data extraction and summary form and managed and organised the data extraction and summary process.
Rachel Churchill conceived, designed, secured funding for and is managing this programme of linked reviews. She worked on all aspects of development of this project, including building and managing the review team, developing the protocol, devising a search strategy, compiling data extraction forms and compiling the overall dataset. Along with Dr Vivien Hunot, she conducted the original review on which this programme is based and has directly contributed to all aspects of drafting this manuscript. She is the guarantor of the individual reviews in this programme of work.
Vivien Hunot provided theoretical and clinical expertise for designing this programme of linked reviews, drawing from her training and clinical practice as a psychotherapeutic counsellor and a cognitive‐behavioural therapist in NHS primary care settings. She worked on protocol development, developed a search strategy, compiled data extraction forms, wrote the protocol for each review and contributed to the draft of this manuscript. Along with Dr Rachel Churchill, she conducted the original review on which this programme is based.
Deborah Caldwell provided methodological and statistical advice for each of 12 linked protocols assessing the effects of different psychotherapies for depression. She contributed to the design of the data extraction form, drafted some sections of the protocols and commented on the protocol manuscripts.
Philippa Davies contributed to the design of the review and to development of the protocol.
Theresa HM Moore managed the organisation of data for the 12 linked reviews of psychotherapies for depression, including search results, tracked papers, and managed references for the project. She developed the original data extraction form, contributed to writing sections of the protocols and commented on the text of the protocols.
Toshi A Furukawa provided theoretical and clinical expertise for this programme of linked reviews. He is a Diplomate of the Academy of Cognitive Therapy (Philadelphia). He commented on the protocol manuscripts, helped revise the data extraction and summary forms, extracted data and contacted the original authors of relevant studies. He supervised the writing and preparing of this review.
All of the review authors have seen, commented on and approved the final manuscript.
Sources of support
Internal sources
University of Bristol, UK.
External sources
-
Department of Health, UK.
NIHR Programme Grant
Declarations of interest
TAF has received honoraria for speaking at CME meetings sponsored by Asahi Kasei, Eli Lilly, GlaxoSmithKline, Mochida, MSD, Otsuka, Pfizer, Shionogi and Tanabe‐Mitsubishi. He is a diplomate of the Academy of Cognitive Therapy. He has received royalties from Igaku‐Shoin, Seiwa‐Shoten and Nihon Bunka Kagaku‐sha. He serves on advisory boards for Sekisui Chemicals and Takeda Science Foundation. The Japanese Ministry of Education, Science, and Technology, the Japanese Ministry of Health, Labor and Welfare and the Japan Foundation for Neuroscience and Mental Health have funded his research projects.
RC leads and has responsibility for the Cochrane Depression, Anxiety and Neurosis Group which has supported parts of the review process and is funded by a grant from the National Institute of Health and Research (NIHR) in the UK.
All of the other review authors have no conflicts of interest to declare.
New
References
References to studies included in this review
Bellack 1981 {published data only}
- Bellack AS, Hersen M, Himmelhoch J. Social skills training compared with pharmacotherapy and psychotherapy in the treatment of unipolar depression. American Journal of Psychiatry 1981;138(12):1562‐7. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Hersen M, Himmelhoch JM. A comparison of social‐skills training, pharmacotherapy and psychotherapy for depression. Behaviour Research and Therapy 1983;21(2):101‐7. [DOI] [PubMed] [Google Scholar]
- Hersen M, Bellack AS, Himmelhoch JM. A comparison of solicited and nonsolicited female unipolar depressives for treatment outcome research. Journal of Consulting and Clinical Psychology 1981;49(4):611‐3. [DOI] [PubMed] [Google Scholar]
- Hersen M, Bellack AS, Himmelhoch JM, Thase ME. Effects of social skill training, amitriptyline, and psychotherapy in unipolar depression women. Behavior Therapy 1984;15:21‐40. [Google Scholar]
- Last CG, Thase ME, Hersen M, Bellack AS, Himmelhoch JM. Treatment outcome for solicited versus nonsolicited unipolar depressed female outpatients. Journal of Consulting and Clinical Psychology 1984;52(1):134. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Thase ME, Hersen M, Himmelhoch JM, Bellack AS. Life events and the endogenous‐nonendogenous distinction in the treatment and posttreatment course of depression. Comprehenxive Psychiatry 1985;26(2):175‐86. [DOI] [PubMed] [Google Scholar]
Breckenridge 1985 {published data only (unpublished sought but not used)}
- Breckenridge JS, Zeiss AM, Breckenridge JN, Gallagher D, Thompson LW. Solicitation of elderly depressives for treatment outcome research: a comparison of referral sources. Journal of Consulting and Clinical Psychology 1985;53(4):552‐4. [DOI] [PubMed] [Google Scholar]
- Gallagher D, Thompson LW. Efficacy of psychotherapy in the treatment of late‐life depression. Advances in Behaviour Research and Therapy 1984;6:127‐39. [Google Scholar]
- Gallagher‐Thompson D, Hanley‐Peterson P, Thompson LW. Maintenance of gains versus relapse following brief psychotherapy for depression. Journal of Consulting and Clinical Psychology 1990;58(3):371‐4. [DOI] [PubMed] [Google Scholar]
- Gaston L, Gallagher D, Marmar CR, Thompson LW. Impact of confirming patient expectations of change processes in behavioral, cognitive, and brief dynamic psychotherapy. Psychotherapy 1989;26(3):296‐302. [Google Scholar]
- Gaston L, Marmar CR, Thompson LW, Gallagher D. Relation of patient pretreatment characteristics to the therapeutic alliance in diverse psychotherapies. Journal of Consulting and Clinical Psychology 1988;56(4):483‐9. [DOI] [PubMed] [Google Scholar]
- Gaston L, Thompson L, Gallagher D, Cournoyer LG, Gagnon R. Alliance, technique, and their interactions in predicting outcome of behavioral, cognitive, and brief dynamic therapy. Psychotherapy Research 8;2(190‐209):1998. [Google Scholar]
- Marmar CR, Gaston L, Gallagher D, Thompson LW. Alliance and outcome in late‐life depression. The Journal of Nervous Mental Disease 1989;177(8):464‐72. [DOI] [PubMed] [Google Scholar]
- Smith CA. The comparative effectiveness of psychotherapies for depressed elders: interaction between individual attributes and therapeutic models. A dissertation presented to the faculty of the California School of Professional Psychology, Alameda, CA, 1995.
- Thompson LW, Gallagher D, Breckenridge JS. Comparative effectiveness of psychotherapies for depressed elders. Journal of Consulting and Clinical Psychology 1987;55(3):385‐90. [DOI] [PubMed] [Google Scholar]
Comas‐Diaz 1981 {published data only (unpublished sought but not used)}
- Comas‐Díaz L. Effects of cognitive and behavioral group treatment on the depressive symptomatology of Puerto Rican women. Journal of Consulting and Clinical Psychology 1981;49(5):627‐32. [DOI] [PubMed] [Google Scholar]
Gallagher 1979 {published data only}
- Gallagher DE. Comparative effectiveness of group psychotherapies for reduction of depression in elderly outpatients. A dissertation presented to the faculty of the Graduate School, University of Southern California, Los Angeles, 1979.
Gardner 1981 {published and unpublished data}
- Gardner P, Oei TP. Depression and self‐esteem: an investigation that used behavioral and cognitive approaches to the treatment of clinically depressed clients. Journal of Clinical Psychology 1981;37(1):128‐35. [DOI] [PubMed] [Google Scholar]
Jacobson 1996 {published data only}
- Addis ME, Jacobson NS. A closer look at the treatment rationale and homework compliance in cognitive‐behavioral therapy for depression. Cognitive Therapy and Research 2000;24(3):313‐26. [Google Scholar]
- Addis ME, Jacobson NS. Reasons for depression and the process and outcome of cognitive‐behavioral psychotherapies. Journal of Consulting and Clinical Psychology 1996;64(6):1417‐24. [DOI] [PubMed] [Google Scholar]
- Gollan J, Raffety B, Gortner E, Dobson K. Course profiles of early‐ and adult‐onset depression. Journal of Affective Disorders 2005;86(1):81‐6. [DOI] [PubMed] [Google Scholar]
- Gollan JK, Gortner ET, Dobson KS. Predictors of depressive relapse during a two year prospective follow‐up after cognitive and behavioral therapies. Behavioural and Cognitive Psychotherapy 2006;34:397‐412. [Google Scholar]
- Gortner ET, Gollan JK, Dobson KS, Jacobson NS. Cognitive‐behavioral treatment for depression: relapse prevention. Consulting and Clinical Psychology 1998;66(2):377‐84. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive‐behavioral treatment for depression. Journal of Consulting and Clinical Psychology 1996;64(2):295‐304. [DOI] [PubMed] [Google Scholar]
- McGlinchey JB, Atkins DC, Jacobson NS. Clinical significance methods: which one to use and how useful are they?. Behavior Therapy 2002;33:529‐50. [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions, and sudden gains in cognitive‐behavioral therapy for depression. Journal of Consulting and Clinical Psychology 2005;73(1):168‐72. [DOI] [PubMed] [Google Scholar]
Kelly 1982 {published data only}
- Kelly LM. Rational emotive therapy versus Lewinsohnian based approaches to the treatment of depression. Dissertation Abstracts International 1982; Vol. 43, issue 6‐B.
Kelly 1983 {published data only (unpublished sought but not used)}
- Kelly FD, Dows ET, Duffey DK. A comparison of cognitive and behavioural intervention strategies in the treatment of depression. British Journal of Cognitive Psychotherapy 1983;1(2):51‐8. [Google Scholar]
Lapointe 1980 {published data only (unpublished sought but not used)}
- LaPointe KA. Cognitive therapy versus assertive training in the treatment of depression. A dissertation submitted to Department of Psychology at the Graduate School, Southern Illinois University, Carbondale, Illinois, 1976.
- LaPointe KA, Rimm DC. Cognitive, assertive, and insight‐oriented group therapies in the treatment of reactive depression in women. Psychotherapy: Theory, Research and Practice 1980;17(3):312‐21. [Google Scholar]
Maldonado 1982 {published data only}
- Maldonado A. Behavioral therapy and depression: an experimental analysis of the behavioral and cognitive models [Terapia de conducta y depresion: un analisis experimental de los modelos conductual y cognitivo]. Revista de Psicologia General y Aplicada 1982;37(1):31‐56. [Google Scholar]
Maldonado 1984 {published data only (unpublished sought but not used)}
- Maldonad A. Behavioral therapy and depression: an experimental analysis of interactions between cognitive and behavioral treatments with pharmacological treatments in depressed subjects [Terapia de conducta y depresion: un analisis experimental de las interacciones entre tratamientos cognitivos y conductuales con tratamientos farmacologicos en sujetos depresivos]. Revista de Psicologia General y Aplicada 1984;39(3):517‐35. [Google Scholar]
McNamara 1986 {published data only (unpublished sought but not used)}
- McNamara K, Horan JJ. Experimental construct validity in the evaluation of cognitive and behavioral treatments for depression. Journal of Counseling Psychology 1986;33(1):23‐30. [Google Scholar]
Pace 1977 {published data only}
- Pace FR. Behavioral techniques in the treatment of depression. A dissertation submitted to School of Psychology, University of New South Wales, Sydney, Australia, 1977.
Padfield 1975 {published data only}
- Padfield M. The comparative effects of two counseling approaches on the intensity of depression among low socioeconomic status rural women. A dissertation submitted to Department of Counselling and Guidance, University of Arizona, Tucson, 1975.
- Padfield M. The comparative effects of two counseling approaches on the intensity of depression among rural women of low socioeconomic status. Journal of Counseling Psychology 1976;23(3):209‐14. [Google Scholar]
Rehm 1979 {published and unpublished data}
- Rehm LP, Fuchs CZ, Roth DM, Kornblith SJ, Romano JM. A comparison of self‐control and assertion skills treatments of depression. Behavior Therapy 1979;10:429‐42. [Google Scholar]
Rehm 1984 {published data only (unpublished sought but not used)}
- Rabin AS, Kaslow NJ, Rehm LP. Changes in symptoms of depression during the course of therapy. Cognitive Therapy and Research 1984;8(5):479‐88. [Google Scholar]
- Rehm LP, Kaslow NJ, Rabin AS. Cognitive and behavioral targets in a self‐control therapy program for depression. Journal of Consulting Clinical Psychology 1987;55(1):60‐7. [DOI] [PubMed] [Google Scholar]
Rude 1986 {published data only}
- Rude SS. An investigation of differential response to two treatments for depression. A dissertation submitted to the School of Education and the Committee on Graduate Studies of Stanford University, Stanford, California, 1983.
- Rude SS. Relative benefits of assertion or cognitive self‐control treatment for depression as a function of proficiency in each domain. Journal of Consulting and Clinical Psychology 1986;54(3):390‐4. [DOI] [PubMed] [Google Scholar]
Sanchez 1980 {published data only (unpublished sought but not used)}
- Sanchez VC, Lewinsohn PM, Larson DW. Assertion training: effectiveness in the treatment of depression. Journal of Clinical Psychology 1980;36(2):526‐9. [DOI] [PubMed] [Google Scholar]
Schmitt 1988 {published data only}
- Schmitt SG. Clinical depression: a comparative study of two treatment approaches. A dissertation submitted to College of Liberal Arts Fairleigh Dickinson University, Florham, Madison, New Jersey, 1988.
Shaw 1977 {published data only (unpublished sought but not used)}
- Shaw BF. Comparison of cognitive therapy and behavior therapy in the treatment of depression. Journal of Consulting and Clinical Psychology 1977;45(4):543‐51. [DOI] [PubMed] [Google Scholar]
Skinner 1983 {published data only}
- Skinner DA. Self‐ control of depression: a comparison of behavior therapy and cognitive behavior therapy. A dissertation presented to the Graduate Faculty of the School of Human Behavior, United States International University, San Diego, California, 1984.
Taylor 1977 {published and unpublished data}
- Taylor FG, Marshall WL. Experimental analysis of a cognitive‐behavioral therapy for depression. Cognitive Therapy and Research 1977;1(1):59‐72. [Google Scholar]
Wetzel 1992 {published data only}
- Murphy GE, Carney RM, Knesevich MA, Wetzel RD, Whitworth P. Cognitive behavior therapy, relaxation training, and tricyclic antidepressant medication in the treatment of depression.. Psychological Reports 1995;77(2):403‐20. [DOI] [PubMed] [Google Scholar]
- Wetzel RD, Murphy GE, Carney RM, Whitworth P, Knesevich MA. Prescribing therapy for depression: the role of learned resourcefulness, a failure to replicate. Psychological Reports 1992;70(3 Pt 1):803‐7. [DOI] [PubMed] [Google Scholar]
Wilson 1983 {published data only}
- Wilson PH, Goldin JC, Charbonneau‐Powis M. Comparative efficacy of behavioral and cognitive treatments of depression. Cognitive Therapy and Research 1983;7(2):111‐24. [Google Scholar]
Zeiss 1979 {published data only (unpublished sought but not used)}
- Lewinsohn PM, Larson DW. The measurement of expectancies and other cognitions in depressed individuals. Cognitive Therapy and Research 1982;6(4):437‐46. [Google Scholar]
- Zeiss AM. Interpersonal behavior problems of the depressed: a study of outpatient treatment. A dissertation presented to the Department of Psychology and the Graduate School of the University of Oregon, Eugene, Oregon, 1977.
- Zeiss AM, Lewinsohn PM. Enduring deficits after remissions of depression: a test of the scar hypothesis. Behaviour Research and Therapy 1988;26(2):151‐8. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM, Muñoz RF. Nonspecific improvement effects in depression using interpersonal skills training, pleasant activity schedules, or cognitive training. Journal of Consulting and Clinical Psychology 1979;47(3):427‐39. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Barrera 1979 {published and unpublished data}
- Barrera M Jr. An evaluation of a brief group therapy for depression. Journal of Consulting and Clinical Psychology 1979 Apr;47(2):413‐5. [DOI] [PubMed] [Google Scholar]
Bowers 1990 {published data only}
- Bowers WA. Treatment of depressed in‐patients. Cognitive therapy plus medication, relaxation plus medication, and medication alone. British Journal of Psychiatry 1990;156:73‐8. [DOI] [PubMed] [Google Scholar]
Brand 1992 {published data only}
- Brand E. Group behavioral therapy with depressed geriatric inpatients: an assessment of incremental efficacy. Behavior Therapy 1992;23:475‐82. [Google Scholar]
Broota 1990 {published data only}
- Broota A, Dhir R. Efficacy of two relaxation techniques in depression. Journal of Personality and Clinical Studies 1990;6(1):83‐90. [Google Scholar]
Cullen 2002 {unpublished data only}
- Cullen JM. Testing the effectiveness of behavioral activation therapy in the treatment of acute unipolar depression. A dissertation submitted to the faculty of the Graduate College Western Michigan University, Kalamazoo, Michigan 2002.
Gallagher 1982 {published data only}
- Gallagher D, Thompson LW. Treatment of major depressive disorder in older adult outpatients with brief psychotherapies. Psychotherapy: Theory, Research & Practice 1982;19(4):482‐90. [Google Scholar]
Hayman 1980 {published and unpublished data}
- Hayman PM, Cope CS. Effects of assertion training on depression. Journal of Clinical Psychology 1980;36(2):534‐43. [DOI] [PubMed] [Google Scholar]
Hopko 2003b {published data only}
- Hopko DR, Lejuez CW, LePage JP, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression. A randomized pilot trial within an inpatient psychiatric hospital. Behavior Modification 2003;27(4):458‐69. [DOI] [PubMed] [Google Scholar]
Losada 2011 {published data only}
- Losada A, Marquez‐Gonzalez M, Romero‐Moreno R. Mechanisms of action of a psychological intervention for dementia caregivers: effects of behavioral activation and modification of dysfunctional thoughts. Geriatric Psychiatry 2011;26:1119‐27. [DOI] [PubMed] [Google Scholar]
Mclean 1979 {published data only}
- McLean PD, Hakstian AR. Clinical depression: comparative efficacy of outpatient treatments. Journal of Consulting and Clinical Psychology 1979;47(5):818‐36. [DOI] [PubMed] [Google Scholar]
Reynolds 2011 {published data only}
- Reynolds EK, Macpherson L, Tull MT, Baruch DE, Lejuez CW. Integration of the brief behavioral activation treatment for depression (BATD) into a college orientation program: depression and alcohol outcomes. Journal of Counseling Psychology 2011;58(4):555‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rokke 1999 {published data only}
- Rokke PD, Tomhave JA, Jocic Z. The role of client choice and target selection in self‐management therapy for depression in older adults. Psychology and Aging 1999;14(1):155‐69. [DOI] [PubMed] [Google Scholar]
Snarski 2011 {published data only}
- Snarski M, Scogin F, DiNapoli E, Presnell A, McAlpine J, Marcinak J. The effects of behavioral activation therapy with inpatient geriatric psychiatry patients. Behavior Therapy 2011;42(1):100‐8. [DOI] [PubMed] [Google Scholar]
Turner 1979 {published data only}
- Turner RW, Ward MF, Turner DJ. Behavioral treatment for depression: an evaluation of therapeutic components. Journal of Clinical Psychology 1979;35(1):166‐75. [DOI] [PubMed] [Google Scholar]
Wilson 1982 {published data only}
- Wilson PH. Combined pharmacological and behavioural treatment of depression. Behaviour Research and Therapy 1982;20(2):173‐84. [DOI] [PubMed] [Google Scholar]
Additional references
APA 1980
- American Psychiatric Association. Diagnostical and Statistical Manual of Mental Disorders (DSM‐III). 3rd Edition. Washington, DC: American Psychiatric Association, 1980. [Google Scholar]
APA 1987
- American Psychiatric Association. Diagnostical and Statistical Manual of Mental Disorders (DSM‐III‐R). 3rd edition, revised. Washington, DC: American Psychiatric Association, 1987. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV). 4th Edition. Washington,DC: American Psychiatric Association, 1994. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostical and Statistical Manual of Mental Disorders (DSM‐IV‐TR). 4th edition, text revision. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
Arroll 2009
- Arroll B, Elley CR, Fishman T, Goodyear‐Smith FA, Kenealy T, Blashki G, et al. Antidepressants versus placebo for depression in primary care. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007954] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barbato 2006
- Barbato A, D'Avanzo B. Marital therapy for depression. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD004188.pub2] [DOI] [PubMed] [Google Scholar]
Barrett‐Lennard 1986
- Barrett‐Lennard GT. The relationship inventory now: Issues and advances in theory, method and use. In: Greenberg LS, Pinsof W editor(s). The Psychotherapeutic Process: A Research Handbook. New York: Guildford Press, 1986. [Google Scholar]
Bayer 2000
- Bayer A, Tadd W. Unjustified exclusion of elderly people from studies submitted to research ethics committee for approval: descriptive study. BMJ 2000;321(7267):992‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelsohn M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Beck 1979
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guildford Press, 1979. [Google Scholar]
Beck 1988
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1988;56(6):893‐7. [DOI] [PubMed] [Google Scholar]
Beck 1996
- Beck AT, Steer RA, Brown GK. BDI‐II: Beck Depression Inventory. 2nd Edition. San Antonio, Texas: The Psychological Corporation, Harcourt Assessment, Inc., 1996. [Google Scholar]
Bellack 1980
- Bellack AS, Hersen M, Himmelhock JM. Social skills training for depression: a treatment manual. JSAS Catalogue of Select Documents 1980;10(92 Ms No 21964):25. [Google Scholar]
Bennett‐Levy 2004
- Bennett‐Levy J, Butler G, Fennell M, Hackmann A, Mueller M, Westbrook D. Oxford Guide to Behavioural Experiments in Cognitive Therapy. Oxford: Oxford University Press, 2004. [Google Scholar]
Bernstein 1973
- Bernstein DA, Borkovec TD. Progressive Relaxation Training. Champaign, Illinois: Research Press, 1973. [Google Scholar]
Bowlby 1980
- Bowlby J. Loss: sadness & depression. Attachment and Loss (Vol 3). London: Hogarth Press, 1980. [Google Scholar]
Cain 2002
- Cain DJ, Seeman J. Humanistic Psychotherapies: Handbook of Research and Practice. Washington, DC: American Psychological Association, 2002. [Google Scholar]
Chen 2001
- Chen YF, Dewey ME, Avery AJ. Self‐reported medication use for older people in England and Wales. Journal of Clinical Pharmacy and Therapeutics 2001;26(2):129‐40. [DOI] [PubMed] [Google Scholar]
Churchill 2000
- Churchill R, Khaira M, Gretton V, Chilvers C, Dewey M, Duggan C, et al. Treating depression in general practice: factors affecting patients' treatment preferences. British Journal of General Practice 2000;50(460):905‐6. [PMC free article] [PubMed] [Google Scholar]
Churchill 2001
- Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al. A systematic review of controlled trials of the effectiveness and cost‐effectiveness of brief psychological treatments for depression. Health Technology Assessment 2001;5(35):1‐173. [DOI] [PubMed] [Google Scholar]
Churchill 2010
- Churchill R, Caldwell D, Moore T, Davies P, Jones H, Lewis G, et al. Behavioural therapies versus other psychological therapies for depression. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD008696] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cipriani 2005
- Cipriani A, Brambilla P, Furukawa T, Geddes J, Gregis M, Hotopf M, et al. Fluoxetine versus other types of pharmacotherapy for depression. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD004185.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cipriani 2009
- Cipriani A, Santilli C, Furukawa TA, Signoretti A, Nakagawa A, McGuire H, et al. Escitalopram versus other antidepressive agents for depression. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006532.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cipriani 2009a
- Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, et al. Comparative efficacy and acceptability of 12 new‐generation antidepressants: a multiple‐treatments meta‐analysis. Lancet 2009;373(9665):746‐58. [DOI] [PubMed] [Google Scholar]
Cipriani 2009b
- Cipriani A, Ferla T, Furukawa TA, Signoretti A, Nakagawa A, Churchill R, et al. Sertraline versus other antidepressive agents for depression. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006117.pub4] [DOI] [PubMed] [Google Scholar]
Cuijpers 2002
- Cuijpers P, Smit F. Excess mortality in depression: a meta‐analysis of community studies. Journal of Affective Disorders 2002;72:227‐36. [DOI] [PubMed] [Google Scholar]
Cuijpers 2007
- Cuijpers P, Straten A, Warmerdam L. Behavioral activation treatments of depression: a meta‐analysis. Clinical Psychology Review 2007;27(3):318‐26. [DOI] [PubMed] [Google Scholar]
da Costa 2012
- Costa BR, Rutjes AW, Johnston BC, Reichenbach S, Nuesch E, Tonia T, et al. Methods to convert continuous outcomes into odds ratios of treatment response and numbers needed to treat: meta‐epidemiological study. International Journal of Epidemiology 2012;41:1445‐59. [DOI] [PubMed] [Google Scholar]
de Shazer 1988
- Shazer S. Clues: Investigating Solutions in Brief Therapy. New York, NY: WW Norton & Co, 1988. [Google Scholar]
Deeks 1997
- Deeks JJ. Are you sure that's a standard deviation? (part 1). Cochrane News 1997;10:11‐2. [Google Scholar]
Deeks 2008
- Deeks JJ, Higgins JPT, Altman DG, on behalf of the CSMG. Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. [Google Scholar]
Dimidjian 2006
- Dimidjian S. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology 2006;74(4):658‐70. [DOI] [PubMed] [Google Scholar]
Dimidjian 2011
- Dimidjian S, Barrera M Jr, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annual Review of Clinical Psychology 2011;7:1‐38. [DOI] [PubMed] [Google Scholar]
Ekers 2008
- Ekers D, Richards D, Gilbody S, Ekers D, Richards D, Gilbody S. A meta‐analysis of randomized trials of behavioural treatment of depression. Psychological Medicine 2008;38(5):611‐23. [DOI] [PubMed] [Google Scholar]
Ellis 2004
- Ellis P. Australian and New Zealand clinical practice guidelines for the treatment of depression. Australian and New Zealand Journal of Psychiatry 2004;38(6):389‐407. [DOI] [PubMed] [Google Scholar]
ESEMeD/MHEDEA 2004
- ESEMeD/MHEDEA 2000 Investigators, Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica Suppl 2004;190(420):21‐7. [DOI] [PubMed] [Google Scholar]
Eysenck 1960
- Eysenck HJ. Behavior Therapy and the Neuroses. Oxford: Pergamon, 1960. [Google Scholar]
Freud 1949
- Freud S. An outline of psychoanalysis. London: Hogarth Press, 1949. [Google Scholar]
Fuchs 1977
- Fuchs CZ, Rehm LP. Self‐control behavior—therapy program for depression. Journal of Consulting and Clinical Psychology 1977;45(2):206‐15. [DOI] [PubMed] [Google Scholar]
Furukawa 2005
- Furukawa TA, Cipriani A, Barbui C, Brambilla P, Watanabe N. Imputing response rates from means and standard deviations in meta‐analysis. Internal Clinical Psychopharmacology 2005;20:49‐52. [DOI] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta‐analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59:7‐10. [DOI] [PubMed] [Google Scholar]
Guaiana 2007
- Guaiana G, Barbui C, Hotopf M. Amitriptyline for depression. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD004186.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guy 1976
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs, 1976:218‐22. [Google Scholar]
Hamilton 1959
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology 1959;32(1):50‐5. [DOI] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2006
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy 2006;44(1):1‐25. [DOI] [PubMed] [Google Scholar]
Henken 2007
- Henken HT, Huibers MJ, Churchill R, Restifo K, Roelofs J. Family therapy for depression. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD006728] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Deeks JJ, Altman DG, on behalf of the CSMG. Special topics in statistics. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. [Google Scholar]
Higgins 2008a
- Higgins JPT, Altman DG. Assessing risk of bias in included studies. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. www.cochrane‐handbook.org.
Hobson 1985
- Hobson RF. Forms of Feeling: The Heart of Psychotherapy. London: Tavistock Publications, 1985. [Google Scholar]
Hofmann 2008
- Hofmann SG, Asmundson GJG. Acceptance and mindfulness‐based therapy: new wave or old hat?. Clinical Psychology Review 2008;28(1):1‐16. [DOI] [PubMed] [Google Scholar]
Hopko 2003a
- Hopko DR, Lejuez CW, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: procedures, principles, and progress. Clinical Psychology Review 2003;23(5):699‐717. [DOI] [PubMed] [Google Scholar]
Horvath 1986
- Horvath AO, Greenberg L. The development of the Working Alliance Inventory: a research handbook. In: Greenberg L, Pinsoff W editor(s). Psychotherapeutic Processes: A Research Handbook. New York: Guildford Press, 1986. [Google Scholar]
Horvath 2011
- Horvath AO, Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy 2011;48(1):9‐16. [DOI] [PubMed] [Google Scholar]
Hunot 2007
- Hunot VM, Horne R, Leese MN, Churchill RC. A cohort study of adherence to antidepressants in primary care: the influence of antidepressant concerns and treatment preferences. Primary Care Companion to the Journal of Clinical Psychiatry 2007;9(2):91‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunot 2010
- Hunot V. Mindfulness‐based 'third wave' cognitive and behavioural therapies versus treatment as usual for depression. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD008705] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ivnik 1992
- Ivnik RJ, Malec JF, Smith GE, Tangalos EG, Petersen RC, Kokmen E, et al. Mayo's older Americans normative studies: updated AVLT norms for ages 56 to 97. The Clinical Neuropsychologist 1992;6(1 Suppl 1):83‐104. [Google Scholar]
Jackson 1985
- Jackson HJ, Moss JD, Solinski S. Social skills training—an effective treatment for unipolar nonpsychotic depression. Australian and New Zealand Journal of Psychiatry 1985;19(4):342‐53. [DOI] [PubMed] [Google Scholar]
Jacobson 2001
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: returning to contextual roots. Clinical Psychology: Science and Practice 2001;8(3):255‐70. [Google Scholar]
Jung 1963
- Jung CG, Jaffe A, Winston C. Memories, Dreams, Reflections. New York: Pantheon Books, 1963. [Google Scholar]
Kanter 2010
- Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC. What is behavioral activation? A review of the empirical literature. Clinical Psychology Review 2010;30(6):608‐20. [DOI] [PubMed] [Google Scholar]
Klein 1960
- Klein M. Our Adult World and Its Roots in Infancy. London: Tavistock, 1960. [Google Scholar]
Klerman 1984
- Klerman GL, Weissman MM, Rousaville BJ, Chevron ES. Interpersonal Psychotherapy for Depression. New York: Basic Books, 1984. [Google Scholar]
Lambert 2013
- Lambert MJ. Handbook of Psychotherapy and Behavior Change. 6th Edition. New York, NY: John Wiley & Sons, Inc., 2013. [Google Scholar]
Law 2003
- Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD004110] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lazarus 1971
- Lazarus AA. Behavior Therapy and Beyond. New York, NY: McGraw‐Hill, 1971. [Google Scholar]
Lewinsohn 1972
- Lewinsohn PM, Libet J. Pleasant events, activity schedules, and depressions. Journal of Abnormal Psychology 1972;79(3):291‐5. [DOI] [PubMed] [Google Scholar]
Lewinsohn 1974
- Lewinsohn PM. A behavioural approach to depression. In: Friedman RJ, Katz MM editor(s). The Psychology of Depression: Contemporary Theory and Research. Washington, DC: Winston, 1974:157‐78. [Google Scholar]
Lewinsohn 1984
- Lewinsohn PM. The Coping With Depression Course: A Psychoeducational Intervention for Unipolar Depression. Eugene, OR: Castalia Publishing Company, 1984. [Google Scholar]
Luborsky 1962
- Luborsky L. Clinician's judgments of mental health. Archives of General Psychiatry 1962;7:407‐17. [DOI] [PubMed] [Google Scholar]
Malan 1963
- Malan DH. A Study of Brief Psychotherapy. London: Tavistock, 1963:xiv‐312. [Google Scholar]
Mann 1973
- Mann J. Time‐Limited Psychotherapy. Cambridge, MA: Havard University Press, 1973. [Google Scholar]
Martell 2001
- Martell CR, Addis ME, Jacobson NS. Depression in Context: Strategies for Guided Action. New York: WW Norton, 2001. [Google Scholar]
Maslow 1943
- Maslow AH. A theory of human motivation. Psychological Review 1943;50:270‐96. [Google Scholar]
May 1961
- May R. Existential Psychology. New York: Random House, 1961. [Google Scholar]
McLeod 2011
- McLeod BD. Relation of the alliance with outcomes in youth psychotherapy: a meta‐analysis. Clinical Psychology Review 2011;31(4):603‐16. [DOI] [PubMed] [Google Scholar]
McMurdo 2005
- McMurdo ME, Witham MD, Gillespie ND. Including older people in clinical research. BMJ 2005;331(7524):1036‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2009
- Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: a meta‐analysis. The Lancet 2009;374(9690):609‐19. [DOI] [PubMed] [Google Scholar]
Montgomery 1979
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry 1979;134:382‐9. [DOI] [PubMed] [Google Scholar]
Mykletun 2009
- Mykletun A, Bjerkeset O, Øverland S, Prince M, Dewey M, Stewart R. Levels of anxiety and depression as predictors of mortality: the HUNT study. British Journal of Psychiatry 2009;195:118‐25. [DOI] [PubMed] [Google Scholar]
Nelson‐Jones 1990
- Nelson‐Jones R. The Theory and Practice of Counselling Psychology. London: Cassell, 1990. [Google Scholar]
Nezu 1986
- Nezu AM. Efficacy of a social problem‐solving therapy approach for unipolar depression. Journal of Consulting and Clinical Psychology 1986;54(2):196‐202. [DOI] [PubMed] [Google Scholar]
NICE 2009
- NICE. Depression: treatment management of depression in adults, including adults with a chronic physical health problem. Clinical Guidelines 09 and 91. London: National Institute for Clinical Excellence, 2009. [Google Scholar]
O'Connell 2007
- O'Connell B. Solution‐focused therapy. In: Dryden W editor(s). Dryden's Handbook of Individual Therapy. London: Sage, 2007. [Google Scholar]
Pilgrim 2002
- Pilgrim D. The cultural context of British psychotherapy. In: Dryden W editor(s). The Handbook of Individual Psychotherapy. 4th Edition. London: Sage, 2002. [Google Scholar]
Rachman 1997
- Rachman SJ. The evolution of cognitive behaviour therapy. In: Clark DM, Fairburn CG editor(s). Science and Practice of Cognitive Behaviour Therapy. Oxford: Oxford University Press, 1997:2‐26. [Google Scholar]
Rait 2005
- Rait G, Fletcher A, Smeeth L, Brayne C, Stirling S, Nunes M, et al. Prevalence of cognitive impairment: results from the MRC trial of assessment and management of older people in the community. Age and Ageing 2005;34(3):242‐8. [DOI] [PubMed] [Google Scholar]
Rait 2009
- Rait G, Walters K, Griffin M, Buszewicz M, Petersen I, Nazareth I. Recent trends in the incidence of recorded depression in primary care. The British Journal of Psychiatry 2009;195(6):520‐4. [DOI] [PubMed] [Google Scholar]
Rehm 1977
- Rehm LP. Self‐control model of depression. Behavior Therapy 1977;8(5):787‐804. [Google Scholar]
Riedel‐Heller 2005
- Riedel‐Heller SG, Matschinger H, Angermeyer MC. Mental disorders—who and what might help? Help‐seeking and treatment preferences of the lay public. Social Psychiatry and Psychiatric Epidemiology 2005;40(2):167‐74. [DOI] [PubMed] [Google Scholar]
Roca 2009
- Roca M, Gili M, Garcia‐Garcia M, Salva J, Vives M, Garcia Campayo J, et al. Prevalence and comorbidity of common mental disorders in primary care. Journal of Affective Disorders 2009;119(1‐3):52‐8. [DOI] [PubMed] [Google Scholar]
Rogers 1951
- Rogers C. Client‐centered therapy: its current practice, implications and theory. London: Constable, 1951. [Google Scholar]
Ryle 1990
- Ryle A. Cognitive‐Analytic Therapy—Active Participation in Change: New Integration in Brief Psychotherapy. Chichester: John Wiley & Sons, 1990. [Google Scholar]
Shapiro 1990
- Shapiro DA, Startup MJ. Raters' Manual for the Sheffield Psychotherapy Rating Scale. Sheffield: MRC/ESRC Social and Applied Psychology Unit, University of Sheffield, 1990. [Google Scholar]
Skinner 1953
- Skinner BF. Science and Human Behaviour. New York: Free Press, 1953. [Google Scholar]
Spielberger 1983
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State‐Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, 1983. [Google Scholar]
Steer RA 2001
- Steer RA, Brown GK, Beck AT, Sanderson WC. Mean Beck Depression Inventory‐II scores by severity of major depressive episode. Psychological Reports 2001;88(3 Pt 2):1075‐6. [DOI] [PubMed] [Google Scholar]
Stiles 2008
- Stiles WB, Barkham M, Mellor‐Clark J, Connell J. Effectiveness of cognitive‐behavioural, person‐centred, and psychodynamic therapies in UK primary‐care routine practice: replication in a larger sample. Psychological Medicine 2008;38(5):677‐88. [DOI] [PubMed] [Google Scholar]
Strupp 1984
- Strupp H, Binder J. Psychotherapy in a New Key: A Guide to Time‐Limited Dynamic Psychotherapy. New York: Basic Books, 1984. [Google Scholar]
Ustun 2004
- Ustun TB, Ayuso‐Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. British Journal of Psychiatry 2004;184:386‐92. [DOI] [PubMed] [Google Scholar]
van Geffen 2009
- Geffen EC, Gardarsdottir H, Hulten R, Dijk L, Egberts AC, Heerdink ER. Initiation of antidepressant therapy: do patients follow the GP's prescription?. British Journal of General Practice 2009;59(559):81‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health Survey: Manual and Interpretation Guide. Boston, MA: Health Institute, New England Medical Center, 1993. [Google Scholar]
Watanabe 2004
- Watanabe N, Churchill R, Hunot V, Furukawa TA. Psychotherapy for depression in children and adolescents (Protocol). Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD005334] [DOI] [Google Scholar]
Watson 1924
- Watson JB. Behaviorism. New York: WW Norton, 1924. [Google Scholar]
Watzlavick 1974
- Watzlavick P, Weakland J, Fisch R. Brief Problem SolvingChange: principles of problem formation and problem resolution. New York: W W Norton. Change: Principles of Problem Formation and Problem Resolution. New York: WW Norton, 1974. [Google Scholar]
Weissman 2007
- Weissman MM, Markowitz JC, Klerman GL. Clinician's Quick Guide to Interpersonal Psychotherapy. Oxford: Oxford University Press, 2007. [Google Scholar]
WHO 1978
- World Health Organisation (WHO). The Ninth Revision of the International Classification of Diseases and Related HealthProblems (ICD‐9). Geneva: WHO, 1978. [Google Scholar]
WHO 1992
- World Health Organisation. The ICD‐10 Classification of Mental and Behavioural Disorders. Geneva: WHO, 1992. [Google Scholar]
WHO 1998
- WHO. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Social Science and Medicine 1998;46(0277‐9536 (Print), 0277‐9536 (Linking), 12):1569‐85. [DOI] [PubMed] [Google Scholar]
WHO 2004
- WHO. The Global Burden of Disease: 2004 Update. Geneva: WHO, 2004. [Google Scholar]
WHO 2008
- WHO. The World Health Report—Primary Health Care (Now More Than Ever). http://www.who.int/healthinfo/global_burden_disease/projections/en/index.html.
Williams 1997
- Williams JMG. Specific problems and disorders: depression. In: Clark DA, Fairburn Christopher G editor(s). Science and Practice of Cognitive Behaviour Therapy. Oxford: Oxford University Press, 1997. [Google Scholar]
Wilson 2008
- Wilson K, Mottram PG, Vassilas C. Psychotherapeutic treatments for older depressed people. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD004853.pub2] [DOI] [PubMed] [Google Scholar]
Wing 1994
- Wing J. Measuring Mental Health Outcomes: A Perspective From the Royal College of Psychiatrists: Outcomes Into Clinical Practice. London: BMJ Publishing, 1994. [Google Scholar]
Wolpe 1958
- Wolpe J. Psychotherapy by Reciprocal Inhibition. Stanford, CA: Stanford University Press; Johannesburg, South Africa: Witwatersrand University Press, 1958. [Google Scholar]


