Abstract
目的
总结原发性椎管内脓肿的特点以及治疗方法,以期提高原发性椎管内脓肿的诊断与治疗水平.
方法
回顾性分析北京大学第三医院近20年来收治的13例原发性椎管内脓肿的病例,分别对其病史,病因,病原学,手术方式以及预后进行分析.
结果
所有病例病程从7 d到6个月不等,所有病例均以疼痛起病,有10例自觉肢体无力,有5例患者有发热史,8例血常规白细胞升高.13例中颈椎管内脓肿1例,颈胸段1例,胸段1例,胸腰段4例,腰骶段6例.病原学中,细菌培养阳性4例,病理学诊断结核3例,1例因发病前感染布氏杆菌(Brucella)按该细菌感染治疗,其余病例病原学结果均阴性.所有病例均行手术治疗,并获得组织病理学诊断.手术目的主要为清除病灶并减压,引流.术后根据病原学结果及临床经验予以抗感染及激素治疗.有2例术后形成切口脓肿再次行手术治疗,手术为清创及转移肌瓣修复.随访0.5~3.0年,平均1.8年.随访期1例术后复发并沿椎管扩散,再次手术治疗.所有病例最后炎症均完全恢复,神经系统体征较术前均有不同程度好转.
结论
原发性椎管内脓肿发病相对较急,主要以疼痛起病,腰骶部最好发,细菌培养多以阴性为主.建议早期手术,使用广谱,足量抗生素.术后如出现切口脓肿形成,宜在清创基础上转移肌瓣修复.术后为缓解脊髓和神经根水肿,可在抗生素保障下使用激素.
Keywords: 椎管内脓肿, 手术, 抗生素, 激素, 肌瓣修复
Abstract
Objective
To summarize the feature and treatment of the primary intraspinal abscess in order to improve the prognosis.
Methods
In the study, 13 cases of primary intraspinal abscess of the recent 20 years were retrospectively analyzed. The history, etiology, pathogen, surgical methods and prognosis were summarized.
Results
The course of the illness ranged from 7 days to 6 months. All the cases began with pain. Of the 13 patients, 10 had limb weakness. Five had a fever and 8 had increased white blood cells. As for distribution, 1 was in cervical vertebra, 1 in cervicothoracic junction, 1 in thoracic vertebra, 4 in thoracolumbar junction, and 6 in lumbosacral segment. The results of bacterial culture were positive in 4 cases, 3 cases were diagnosed as tuberculosis by pathological examination, and 1 case was recognized as infection of Brucella melitensis bacteria because of prior brucellosis. The pathogen of the remaining cases were unclear. All the cases received surgical treatment and pathology examination. The surgical aim was mainly removal of the lesion, decompression and drainage. Postoperatively anti-infection and glucocorticoid therapy were performed according to the pathogeny results and clinical experience. Incision abscesses were seen in 2 cases and reoperations including debridement and repair with transferred muscle flap were performed. Postoperative follow-up ranged from 6 months to 3 years (mean 1.8 years). One case suffered postoperative recurrence and the abscess spread along the vertebral canal. Reoperation was performed. Infections of all the cases were recovered completely and the nervous system signs were all improved in different degrees.
Conclusion
The onset of primary intraspinal abscess is relatively urgent, mainly with pain. The lumbar and sacral vertebra is the predilection site. The bacterial culture is mostly negative. Early operation and use of sufficient amount of broad-spectrum antibiotic are recommended. If the incision abscess forms after the operation, it is advisable to transfer the muscle flap to repair the coloboma on the basis of debridement. In order to relieve edema of spinal cord and nerve root, the glucocorticoid can be used in the escort of antibiotics.
Keywords: Intraspinal abscess, Surgery, Antibiotics, Glucocorticoid, Muscle flap
原发性椎管内脓肿罕见,但常常对神经系统造成严重损害[1].原发性椎管内脓肿的预后并不理想,而且治疗过程中容易出现各种严重并发症,既往文献报道只有不到半数的患者可完全恢复,病死率为13%~19%[2,3,4,5].原发性椎管内脓肿的预后与能否早期诊断密切相关,因此总结椎管内脓肿的特点及治疗过程中的经验教训,以提高早期诊断率和治疗水平,从而改善预后非常重要[6].北京大学第三医院自1997年1月至2017年1月收治了13例原发性椎管脓肿患者,经积极治疗,效果较为理想,现总结如下.
1. 资料与方法
1.1. 一般资料
本组共13例患者,其中男性5例,女性8例,年龄13~68岁,平均(40.85±19.34)岁,6例有感染危险因素,2例有感染史(表1).
1.
患者一般资料
General information of patients
| Case | Gender | Age | Predisposing factor | Course/d | Onset symptom | Temperature | Neurological signs |
| 1 | Female | 13 | Diabetes mellitus | 30 | Low back pain and lower extremity pain | Normal | Weakness of lower limb and loss of lower limb tendon reflex |
| 2 | Female | 15 | None | 180 | Right upper limb pain | Normal | Weakness and hypoesthesia in the right upper limb |
| 3 | Male | 18 | Malignancy | 7 | Low back pain and lower extremity pain | Fever | Local tenderness, hypoesthesia between T10 to L1 and hyperesthesia between L2-L5 |
| 4 | Female | 24 | Long term use of glucocorticoid | 7 | Low back pain | Fever | Weakness of lower limb, hypoesthesia below T12, hyporeflexiaof lower limb tendon reflex and relaxation of anal sphincter |
| 5 | Male | 30 | History of brucellosis | 20 | Neck pain | Normal | Weakness of right limb, positive right Babinski's sign and hypoesthesia at C2 |
| 6 | Female | 34 | None | 180 | Low back pain | Fever | Local tenderness, hypoesthesia of right lower limb, weakness of lower limb, hyporeflexia of lower limb tendon reflex and meningeal irritation sign |
| 7 | Female | 46 | Malignancy, Diabetes mellitus | 18 | Low back pain | Normal | Weakness of lower limb and hyporeflexia of lower limb tendon reflex |
| 8 | Female | 51 | Local dermal sinus | 15 | Low back pain | Normal | Weakness of lower limb, hyperreflexia of lower limb tendon reflex, hypermyotonia and hyperesthesia of lower limb |
| 9 | Male | 54 | Local dermal sinus | 10 | Low back pain | Normal | Weakness of lower limb, hyperreflexia of lower limb tendon reflex, hypermyotonia and hyperesthesia of lower limb |
| 10 | Male | 56 | None | 14 | Low back pain | Fever | Local tenderness, weakness of lower limb and meningeal irritation sign |
| 11 | Female | 58 | None | 20 | Chest back pain | Normal | Weakness of lower limb, hyperreflexia of lower limb tendon reflex, pathological signs and hypoesthesia below T6 |
| 12 | Female | 64 | None | 30 | Lumbosacral pain | Fever | Local tenderness, weakness of lower limb and hyporeflexia of lower limb tendon reflex |
| 13 | Male | 68 | Adjacent skin infection | 7 | Low back pain | Normal | Paralysis of lower limbs and relaxation of anal sphincter |
1.2. 临床表现
所有患者均有疼痛症状,10例自觉肢体无力,5例有大小便功能障碍,5例有体温升高,3例有肢体麻木.病史7 d到6个月,平均41 d(表1).
1.3. 辅助检查(表2)
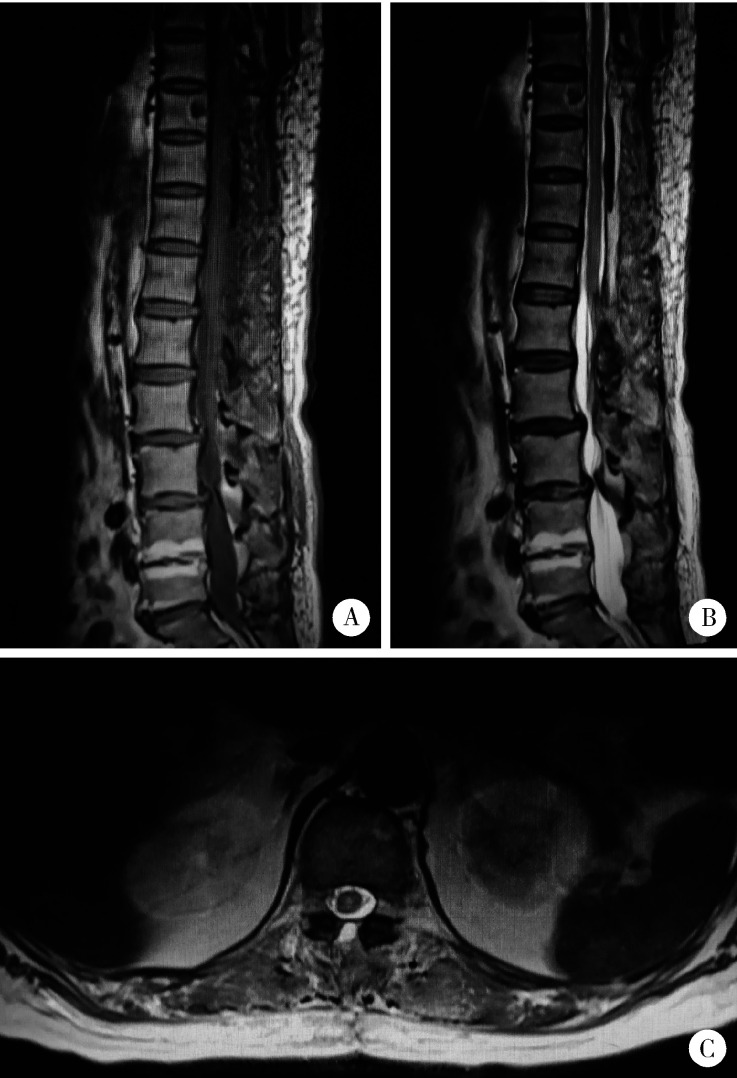
所有患者均行MRI检查,大多数表现为囊性病变,环形强化(图1).部分病变可无明显囊性表现,呈均匀强化.2例患者行CT检查,其中1例可见棘突及椎板骨质破坏,另1例未见明显异常表现.术后均复查磁共振以评估患者脓肿切除情况.
1.
胸腰段硬膜外脓肿患者的术前磁共振检查
Preoperative MRI in a patient with thoracolumbar epidural abscess
The sagittal (A) and axial (B) T2WI MRI showed a highsignal lesion in the epidural space, and the dural sac was obviously pressed. The sagittal (C) and axial (D) enhanced MRI showed a ring-enhancement lesion which extended to the intervertebral foramen, and the corresponding dura was thickened.
2.
患者术前辅助检查
Preoperative adjuvant examination
| Case | Inflammatory markers | MRI | ||
| WBC | ESR | CRP | ||
| WBC, white blood cell; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; NA: not applicable. | ||||
| 1 | Normal | High | NA | Subdural lesion between L4-S1 with significant enhancement |
| 2 | Normal | High | NA | Epidural lesion between C7-T3 with area of cystoid variation and necrosis and significant enhancement of solid area |
| 3 | High | NA | NA | Epidural lesion in the thoraco-lumbo-sacral spinal canal with posterior vertical spine muscle strip enhancement, posterior lamellar muscle enhancement |
| 4 | High | NA | NA | Epidural cystic lesion between T12-L2 with enhancement of cyst wall |
| 5 | Normal | Normal | High | Epidural lesion ventral to spinal cord between C2-C4 with significant homogeneous enhancement and edema of corresponding spinal cord |
| 6 | Normal | NA | NA | Multiple subdural lesions between T12-L3 with significant homogeneous enhancement |
| 7 | Normal | High | NA | Intraspinal cystic lesion between T8-L2 with ring enhancement of cyst wall |
| 8 | High | NA | NA | Intramedullary abnormal signal between L2-L3 with ring enhancement, dermal sinus at L4-L5 connected to the spinal canal with tethered cord |
| 9 | High | NA | NA | Intramedullary abnormal signal between L2-L3 with ring enhancement, dermal sinus at L2-L3 connected to the spinal canal |
| 10 | High | NA | NA | Intraspinal lesion between L3-L5 with ring enhancement |
| 11 | High | NA | NA | Extramedullary epidural lesion between T4-T5 with ring enhancement |
| 12 | High | High | High | Multiple intraspinal and paravertebral cystic lesions between S1-S3 with ring enhancement |
| 13 | High | NA | NA | Epidural cystic lesions between T9-L1 with ring enhancement |
1.4. 治疗方法
所有病例均接受手术治疗,手术均采取后正中入路,进行椎板切除减压.术前定位必须准确,椎板切除范围必须包括脓肿的上,下极.在显微镜下尽可能清除脓肿,术中用稀碘伏,双氧水和生理盐水反复冲洗,术后留置引流.
脓肿常规送病理诊断及细菌培养,术后如能根据组织病理学诊断及细菌培养结果确定病原菌,则根据病原菌给予相应治疗.如无明确病原菌,则给予广谱抗生素治疗,同时覆盖需氧菌和厌氧菌.对于脊髓和(或)神经受损较重者,可在使用抗生素治疗的同时,给予激素及甘露醇治疗.
2. 结果
治疗情况及术中情况见表3,脓肿大多位于腰椎和骶椎(6/13), 以硬膜外常见(7/13).
3.
治疗情况及术中所见
Treatment and intraoperative findings
| Case | Treatment | Location | Abscess character | |||
| Surgery | Antibacterials | Glucocorticoid | Mannitol | |||
| 1 | Yes | Yes(anti-TB) | No | No | L4-S1, epidural, ventral | Gelatinous and caseous |
| 2 | Yes | Yes(anti-TB) | No | No | C7-T3, epidural | Thinning pus and gray granuloma |
| 3 | Yes | Yes | No | No | L4-S1, epidural | Yellowish-white thinning pus |
| 4 | Yes | Yes | Yes | No | T12-L2, epidural | Beige pus |
| 5 | Yes | Yes | Yes | Yes | C3-C7, epidural, ventral | Purple-red granuloma |
| 6 | Yes | Yes | No | No | T12-L3,intra-extramedullary | Yellow sticky pus and granuloma |
| 7 | Yes | Yes | Yes | No | T8-L2, epidural | Much yellow pus with granuloma |
| 8 | Yes | Yes | Yes | Yes | L2-L3,intra-extramedullary | Yellowish-white pus with much pus mosses |
| 9 | Yes | Yes | Yes | Yes | L2-L3,subdural | Yellowish-white pus |
| 10 | Yes | Yes | No | No | L3-L5, epi-subdural | Yellowish-white pus with pus mosses and granuloma |
| 11 | Yes | Yes | Yes | Yes | T4-T5, intramedullary | Yellowish-white pus |
| 12 | Yes | Yes | No | No | S1-S3, epi-subdural and paravertebral | Yellowish-white pus with pale yellow granuloma |
| 13 | Yes | Yes | No | No | T9-L1, epidural | Beige pus with little granuloma and much pus mosses |
病原学检查及病理学检查结果见表4,有1例因病变位于脊髓腹侧且难以切除未做细菌培养,但该患者有布氏杆菌(Brucella)感染病史,故考虑脓肿亦为布氏杆菌导致.13例患者中有1例布氏杆菌感染,4例细菌感染,3例结核病,5例无明确病原菌.2例有窦道者感染途径考虑与窦道有关,其余11例均考虑为血行转移.
4.
患者术后情况
Postoperative situation
| Case | Pyoculture | Blood culture | Pathology | Possible way | Outcome |
| NA, not applicable. | |||||
| 1 | Negative | Negative | Tuberculosis | Hematogenous | Complete recovery |
| 2 | Negative | NA | Tuberculosis | Hematogenous | Complete recovery |
| 3 | Negative | NA | NA | Hematogenous | Complete recovery |
| 4 | Staphylococcus aureus | NA | Pus | Hematogenous | No abscess or pain, light hypoesthesia, muscle strength grade IV, occasional urine incontinence |
| 5 | NA | NA | NA | Hematogenous | No abscess or pain, euesthesia, muscle strength grade Ⅳ |
| 6 | Negative | NA | Pus | Hematogenous | Recurrence 1 year later, complete recovery finally |
| 7 | Negative | NA | Tuberculosis | Hematogenous | No abscess or pain, euesthesia, muscle strength grade Ⅳ |
| 8 | Enterococcus faecalis | NA | Dermal sinus, necrosis and granulation tissue |
Direct spread | Complete recovery |
| 9 | Escherichia coli | NA | Dermal sinus | Direct spread | Complete recovery |
| 10 | Negative | NA | Pus | Hematogenous | No abscess or pain, euesthesia, muscle strength grade Ⅳ |
| 11 | Negative | NA | Pus | Hematogenous | No abscess or pain, hypoesthesia, no provement in muscle strength |
| 12 | Negative | Negative | Pus | Hematogenous | Wound abscess which restored after debridement and repair with muscle flap, complete recovery finally |
| 13 | Staphylococcus aureus | NA | Pus | Hematogenous | Wound abscess which restored after debridement and repair with muscle flap. No abscess or pain, hypoesthesia, muscle strength grade Ⅳ, occasional urine incontinence finally |
术后有2例伤口脓肿形成,经清创及转移带蒂肌皮瓣至脓肿腔,消除死腔,术后继续抗炎等治疗,伤口愈合良好.随访0.5~3.0年,平均1.8年.有1例胸腰段脓肿患者,术后症状缓解且复查磁共振显示脓肿基本消失,约1年后又开始出现发热,左下肢无力及肢体抽搐,复查磁共振显示脓肿复发,再次行手术治疗,术后病理学诊断见真菌芽孢及菌丝,考虑为真菌性脓肿.规范抗真菌治疗3周,患者症状减轻,复查磁共振脓肿消失,在随访期内未再复发,至末次随访时,患者体温均恢复正常,疼痛消失,神经功能恢复情况见表4,复查磁共振均提示脓肿吸收(图2).
2.
胸腰段硬膜外脓肿患者的术后核磁
Postoperative MRI in a patient with a thoracolumbar epidural abscess
The sagittal T1WI(A) and sagittal T2WI(B) MRI showed that the abscess was cleared after the operation and the corresponding dural sac was relieved. The axial T2WI(C) MRI showed that the subarachnoid cavity was unblocked.
3. 讨论
原发性椎管内脓肿是指未对脊柱进行有创操作情况下出现的椎管内脓肿,该病罕见,但大多进展迅速,可能对神经系统造成严重损害[1].即使在发达国家,住院患者病死率也高达3.58%,且有8.51%的患者会发展为瘫痪[7].椎管内脓肿常位于硬膜外,其次为髓外硬膜下,位于髓内者极为罕见[8,9,10,11,12,13].可由邻近病变直接扩散而来,也可由血行播散而来,甚至是淋巴播散而来,其中血行播散是最常见的来源[5,6].由于椎管内空间有限,且无法扩张,脓肿形成后通过机械性压迫以及血管闭塞作用对脊髓等神经组织造成损害,严重者可导致脊髓梗塞[10,14].早期该病病死率高,而完全恢复者不足50%[2,3,4,5],这与诊断延迟有关.本组病例中,大多起病较急,尤其是伴有发热的病例,病史大多为1~2周,且脓肿部位和感染来源均与文献类似[2,3,4,5].早期诊断并手术的患者均取得了较好的疗效,包括一名完全截瘫的患者,术后恢复了大部分运动功能,也充分说明了早期诊断和早期手术的重要性,因此提高对椎管内脓肿的认识,尽早明确诊断,有助于改善患者预后[6].
尽早明确诊断需要结合患者的症状和影像学特征,原发性椎管内脓肿患者的临床症状包括疼痛,发热和神经功能障碍[15],但早期可能只有非特异性的疼痛,晚期才会出现神经根性疼痛或神经功能障碍,如无力,感觉减退,腱反射异常及大小便功能障碍等,严重者可能出现截瘫[5-6,16-18],只有部分患者伴有发热[6,16],结核性脓肿患者常没有明显的发热[5,17],这些均给早期诊断带来了困难.辅助检查中最有价值的是MRI[11,13,18-21],增强核磁上典型的脓肿呈环形强化,对诊断具有重要意义[11,14,21].
原发性椎管内脓肿的致病菌多种多样,最常见的致病菌是金黄色葡萄球菌,也有其他细菌,结核杆菌,真菌,布氏杆菌等[2,5,12-13,16-17,22-24].原发性椎管内脓肿的危险因素包括年龄,糖尿病,恶性肿瘤,酗酒,免疫抑制,全身性感染和静脉滥用药物等[5-6,25].抑制免疫力的因素包括HIV感染,器官移植,风湿,慢性肾衰竭或长期使用皮质醇药物等[5,22,25].在原发性椎管内脓肿中,非典型结核的患者值得引起重视,非典型脊柱结核可以只累及椎弓并引起椎管内脓肿[17,19],全椎管均可能受累,但更常见于胸椎管[19,20],这类结核脓肿可位于硬膜外或硬膜下,甚至位于髓内[11,17,20].硬膜外结核脓肿常导致椎板的破坏,并由结核肉芽组织代替;硬膜下结核脓肿的椎板破坏不明显,但也有结核肉芽组织的渗透,导致椎板变得薄弱[17,19].脓肿颜色可呈黄绿色或浅黄色,可呈稀薄,也可呈黏稠奶油状或牙膏状[17,20].部分标本能培养出结核杆菌,肉芽组织的病理学检查可见慢性炎性反应和干酪样坏死,包括典型的Langerhans细胞,上皮细胞和圆形细胞.本组病例可见3例结核性脓肿,均位于硬膜外,其中1例有棘突和椎板的骨质破坏.现在结核病虽然罕见,仍要警惕这类非典型结核的可能.
椎管内脓肿的治疗主要包括保守和手术治疗.有文献报道,保守治疗可取得与手术治疗相当甚至更好的预后[7],但通常是在没有或仅有轻微的神经功能障碍时,才选择保守治疗[2,10,22].由于本病进展快,多数学者支持进行手术治疗[5,7,14,21].当出现明显急性神经功能症状(如肌力下降,感觉障碍或大小便功能受限)时应该进行手术治疗,否则可能会引起不可逆的神经功能障碍[7,14,17-18].患者的预后和最终的神经功能与术前的神经功能情况有关,因此确诊后应尽早手术,早期手术能改善患者预后[5,7,15],而延迟手术者术后败血症及病死率均明显升高[7].手术目的在于清除脓肿,充分减压,同时获得病理和病原学检查标本[2,10,13].硬膜外和硬膜下脓肿可尽量清除,如为长节段脓肿可行部分椎板切除,进行脓肿灌洗和引流,髓内脓肿则主要进行充分引流[14,18],但要注意,手术充分减压即可,不必追求脓肿的全切,充分减压后,辅以术后药物治疗,大多预后较好.本组病例中有1例布氏杆菌脓肿位于脊髓腹侧且难以切除,仅行减压手术,术后给予针对性抗生素治疗,脓肿完全消失,恢复较好.对于伴有皮肤窦道等畸形者,应同期予以处理[13-14,21,24,26],但是需要注意,椎板可能已被脓肿尤其是硬膜外脓肿破坏,剥离椎旁肌肉时一定要小心,以防误入椎管内损伤硬脊膜和脊髓.本组患者就诊时均已出现不同程度的神经功能障碍,因此均进行了手术治疗,总体恢复情况较好.
本研究原发性椎管内脓肿细菌培养阳性率低,即便结合病理学检查,准确的病原学结果也非常有限.在没有病原学结果时,可给予广谱抗生素治疗,需注意选择可透过血脑屏障的抗生素,必要时给予抗结核治疗,且这类患者的抗生素治疗都要足量且足够疗程[6,17,22].在有病原学结果尤其是有药敏结果后,可根据病原种类选择敏感抗生素治疗[7],但要注意的是,脓液培养和血培养结果常呈阴性,因此应在诊断脓肿后就开始足量广谱抗生素治疗.在使用抗生素保护的前提下,使用激素和甘露醇,可以明显减轻脊髓和神经的水肿,有利于恢复[11,20].本研究有6例病例在使用抗生素的前提下使用了皮质类固醇激素治疗,无死亡病例,没有出现明显的并发症,大部分患者术后功能恢复良好,因此认为椎管内脓肿的患者,术后使用激素是有积极意义的.
由于椎管内脓肿手术切口为感染性伤口,术后可能出现伤口脓肿形成,伤口脓肿形成后传统的处理包括穿刺抽脓,换药或伤口再次清创缝合,但由于此类伤口是污染切口,同时清除脓液和坏死组织后形成脓肿残腔,术者需面临组织缺损的问题.无论是伤口加压包扎或局部松解缝合,都难以彻底消除死腔,且可能影响局部血运,导致伤口难以愈合,甚至脓肿反复形成.本研究有2例术后伤口脓肿形成的患者,在清创基础上转移带蒂肌瓣修复,术后不仅有效消除了死腔,而且由于肌肉血供丰富,愈合能力和抗感染能力都很强,伤口都愈合良好.因此,对于术后伤口脓肿形成的患者,转移肌瓣修补是一个值得推荐的办法.
综上所述,椎管内脓肿发病相对较急,主要以疼痛和肢体无力起病,以腰骶部为最好发,细菌培养多以阴性为主.为保障神经功能并缓解症状,需要快速给予处理,建议早期手术为宜,以防止永久性功能障碍的发生.抗生素使用建议广谱,足量.如能早期明确诊断,及早手术,并辅以足量抗生素治疗,效果多较好.术后足量的激素使用,有利于缓解脊髓和神经根的水肿.术后如出现伤口脓肿形成,在清创基础上转移肌瓣修复,一般能取得较好的效果.
Funding Statement
首都临床特色应用研究项目(Z171100001017120)
Supported by the Capital Foundation for Clinical Characteristics and Application Research(Z171100001017120)
References
- 1.Honig A, Or O, Barzilay Y, et al. Spinal epidural abscess with a rapid course in young healthy infantry recruits with multiple skin lacerations. J Clin Neurosci. 2016;31:127–132. doi: 10.1016/j.jocn.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 2.Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000;23(4):175–205. doi: 10.1007/pl00011954. [DOI] [PubMed] [Google Scholar]
- 3.Ersahin Y. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2001;24(2/3):156. doi: 10.1007/pl00014578. [DOI] [PubMed] [Google Scholar]
- 4.Karikari IO, Powers CJ, Reynolds RM, et al. Management of a spontaneous spinal epidural abscess: a single-center 10-year experience. Neurosurgery. 2009;65(5):919–924. doi: 10.1227/01.NEU.0000356972.97356.C5. [DOI] [PubMed] [Google Scholar]
- 5.Bartels RH, de Jong TR, Grotenhuis JA. Spinal subdural abscess. J Neurosurg. 1992;76(2):307–311. doi: 10.3171/jns.1992.76.2.0307. [DOI] [PubMed] [Google Scholar]
- 6.Kirzner H, Oh YK, Lee SH. Intraspinal air: a CT finding of epidural abscess. Am J Roentgenol. 1988;151(6):1217–1218. doi: 10.2214/ajr.151.6.1217. [DOI] [PubMed] [Google Scholar]
- 7.Farber SH, Murphy KR, Suryadevara CM, et al. Comparing outcomes of early, late, and non-surgical management of intraspinal abscess. J Clin Neurosci. 2017;36:64–71. doi: 10.1016/j.jocn.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 8.Kulkarni AG, Chu G, Fehlings MG. Pyogenic intradural abscess: a case report. Spine. 2007;32(12):E354–E357. doi: 10.1097/BRS.0b013e31805c0ab7. [DOI] [PubMed] [Google Scholar]
- 9.Thomé C, Krauss JK, Zevgaridis D, et al. Pyogenic abscess of the filum terminale. Case report. J Neurosurg. 2001;95(Suppl 1):100–104. doi: 10.3171/spi.2001.95.1.0100. [DOI] [PubMed] [Google Scholar]
- 10.Darouiche RO. Spinal epidural absces. N Engl J Med. 2006;355(19):2012–2020. doi: 10.1056/NEJMra055111. [DOI] [PubMed] [Google Scholar]
- 11.Hanci M, Sarioglu AC, Uzan M, et al. Intramedullary tuberculous abscess: a case report. Spine. 1996;21(6):766–769. doi: 10.1097/00007632-199603150-00023. [DOI] [PubMed] [Google Scholar]
- 12.Bingöl A, Yücemen N, Meço O. Medically treated intraspinal "Brucella" granuloma. Surg Neurol. 1999;52(6):570–576. doi: 10.1016/s0090-3019(99)00110-x. [DOI] [PubMed] [Google Scholar]
- 13.Kamat AS, Thango NS, Husein MB. Proteus mirabilis abscess involving the entire neural axis. J Clin Neurosci. 2016;30:127–129. doi: 10.1016/j.jocn.2015.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Al Barbarawi M, Khriesat W, Qudsieh S, et al. Management of intramedullary spinal cord abscess: experience with four cases, pathophysiology and outcomes. Eur Spine J. 2009;18(5):710–717. doi: 10.1007/s00586-009-0885-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hindy J, Shelef I, Slovik Y, et al. Late prevertebral and spinal abscess following chemoradiation for laryngeal squamous cell carcinoma. Case Rep Otolaryngol. 2014;2014:425724. doi: 10.1155/2014/425724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miyazaki M, Yoshiiwa T, Kodera R, et al. Clinical features of cervical pyogenic spondylitis and intraspinal abscess. J Spinal Disord Tech. 2011;24(7):E57–E61. doi: 10.1097/BSD.0b013e318227ed9d. [DOI] [PubMed] [Google Scholar]
- 17.Ur-rahman N, El-bakry A, Jamjoom AB, et al. Atypical forms of spinal tuberculosis: case report and review of the literature. Surg Neurol. 1999;51(6):602–607. doi: 10.1016/s0090-3019(98)00101-3. [DOI] [PubMed] [Google Scholar]
- 18.Khalil JG, Nassr A, Diehn FE, et al. Thoracolumbosacral spinal subdural abscess: magnetic resonance imaging appearance and limited surgical management. Spine. 2013;38(13):E844–E847. doi: 10.1097/BRS.0b013e31828d5f30. [DOI] [PubMed] [Google Scholar]
- 19.Narlawar RS, Shah JR, Pimple MK, et al. Isolated tuberculosis of posterior elements of spine: magnetic resonance imaging findings in 33 patients. Spine. 2002;27(3):275–281. doi: 10.1097/00007632-200202010-00015. [DOI] [PubMed] [Google Scholar]
- 20.Tanriverdi T, Kizilkiliç O, Hanci M, et al. Atypical intradural spinal tuberculosis: report of three cases. Spinal Cord. 2003;41(7):403–409. doi: 10.1038/sj.sc.3101463. [DOI] [PubMed] [Google Scholar]
- 21.Hung PC, Wang HS, Wu CT, et al. Spinal intramedullary abscess with an epidermoid secondary to a dermal sinus. Pediatr Neurol. 2007;37(2):144–147. doi: 10.1016/j.pediatrneurol.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 22.ter Avest E, Uyttenboogaart M, Dorgelo J, et al. A patient with neck pain and fever. Combined prevertebral and intraspinal abscess in a patient with a de novo HIV infection. Neth J Med. 2009;67(10):356–357. [PubMed] [Google Scholar]
- 23.Vajramani GV, Nagmoti MB, Patil CS. Neurobrucellosis presenting as an intramedullary spinal cord abscess. Ann Clin Microbiol Antimicrob. 2005;16(4):14. doi: 10.1186/1476-0711-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dev R, Husain M, Gupta A, et al. MR of multiple intraspinal abscesses associated with congenital dermal sinus. Am J Neuroradiol. 1997;18(4):742–743. [PMC free article] [PubMed] [Google Scholar]
- 25.Nagar VR, Springer JE, Salles S. Increased incidence of spinal abscess and substance abuse after implementation of state mandated prescription drug legislation. Pain Med. 2015;16(10):2031–2035. doi: 10.1111/pme.12810. [DOI] [PubMed] [Google Scholar]
- 26.Singh I, Rohilla S, Kumar P, et al. Spinal dorsal dermal sinus tract: An experience of 21 cases. Surg Neurol Int. 2015;6(Suppl 17):S429–434. doi: 10.4103/2152-7806.166752. [DOI] [PMC free article] [PubMed] [Google Scholar]