Abstract
Background:
Oral implants are considered safe in the mandibular anterior region, but complications often occur if vital structures such as inferior alveolar nerve, mandibular incisive canal (MIC), anterior mental loop (AL), or mental foramen (MF) are not properly identified.
Aim:
The aim was to evaluate vital anatomical structures in the mandibular interforaminal region and to investigate sexual dimorphism and differences with respect to left and right side regions using cone-beam computed tomography (CBCT).
Materials and Methods:
Eighty CBCT scans (forty male and forty female) were analyzed for MF position and shape, presence and measurement of AL and MIC (both in mm), emergence patterns of mandibular canal, and symmetry of MF and AL. A pilot study was conducted on five patients to determine interobserver reliability among two oral and maxillofacial radiologists, considered for interpretation of CBCT images. All the scans were taken by CS 9300, CBCT machine adjusted at 80 kVp, 15 mA, voxel size 0.3 × 0.3 × 0.3, and field of view of 10 × 5 (mandible only). The acquired images were reconstructed into multiplanar views (axial, panoramic, and cross-sectional) for evaluation.
Results:
The mean age of the study population was 42.64 ± 16.22 years, with males noted with slightly higher age. Position 4 of MF (below the apex of the second premolar) was noted the most on the right side, whereas position 3 (between the first and second premolars) was noted on the left side, with 75% of symmetrical MF position. The oval-shaped MF was most common among both genders and sides. The prevalence of MIC was noted in 93.75% of patients with a mean length of 12.09 ± 5.95 mm. The prevalence of AL was 53.13%, with a mean length of 1.07 ± 1.42 mm. No statistically significant sexual dimorphism (P > 0.05) was found between genders or sides for all the evaluated interforaminal parameters.
Conclusion:
CBCT evaluation of vital anatomical structures needs to be elicited before planning an interforaminal placement of implants, and no sexual dimorphism was found regarding them.
Keywords: Anterior mental loop, inferior alveolar nerve, mandibular incisive canal, mental foramen
INTRODUCTION
Today, oral implants are routinely used in oral rehabilitation. Yet, the frequent placement of oral implants has raised the number of neurosensory disturbances and hemorrhages, even in the anterior mandible, which was previously considered as a safe region without vital neurovascular bundles.[1] These complications often occur if the vital structures such as inferior alveolar nerve (IAN), mandibular incisive canal (MIC), anterior mental loop (AL), or mental foramen (MF) are not properly identified.[2] These anatomical landmarks that are related with mandible are significant and can be damaged during oral and maxillofacial surgical procedures such as mandibular osteotomies, orthognathic surgeries, mandibular trauma managements, surgeries of benign and malignant lesions, and preprosthetic surgeries, and nerve damage is possible even during inferior mandibular nerve block.[3] The mandibular implant or orthognathic surgery-related three-dimensional (3D) radiographic anatomy needs to be carefully evaluated prior to treatment that will certainly decrease the chances of complications. Hence, the present study was conducted to add data regarding the same. During neurovascular path in mandibular bone, the IAN runs through the mandibular canal, and it is divided into two segments near the MF: the mental branch, which emerges in this foramen and supplies sensation to the skin and mucous membrane of the lower lip and chin together with adjacent buccal nerve, and the incisive branch, which continues intraosseous and runs through the MIC to innervate the anterior teeth including the first premolar. However, in some individuals, the terminal portion of the IAN may extend, passing below the inferior border of the MF and after giving off the incisive nerve branches, the main branch curves back to the MF, which emerges as the mental nerve. This section of the nerve in front of the MF can be described as the AL of the IAC.[2] Hence, the AL is an extension of the IAN, anterior to the MF, which loops back to exit the MF. Although it is a benign anatomical variation, its accurate identification is essential for surgical planning, particularly for dental implant placement, in order to prevent iatrogenic complications and to ensure the effectiveness of surgical procedures performed in the region.[4] The prevalence of AL has been reported to range from 28% to 71% in past studies.[5,6]
The MIC is described as a continuation of the IAC anterior to the MF and contains one of the terminal branches of the IAN, the incisive branch.[7] The MIC prevalence ranges from 15% in panoramic to 93% on cone-beam computed tomography (CBCT) scans.[8] The MIC becomes smaller while progressing from the distal to the most anterior part of the mandible to midline.[5] Because of decreased bone–implant contact, MICs with large diameters may play a negative role in the osseointegration of implants. Furthermore, a large MIC might be involved in postoperative sensory disturbance. A dental implant penetrating the MIC could result in a possible stretching of the mental nerve. Hence, the clinical significance can be realized through mapping of the MIC and its proximity relative to anatomical considerations during osseous grafting procedures, specifically when using the chin graft protocol for harvesting donor bone.[9] The MF is a funnel-like opening in the lateral surface of the body of the mandible at the terminus of the mental canal, which is the anterior limit of IAC.[10] Phillips et al.[6] reported that its average size was 4.6 mm horizontally and 3.4 mm vertically.[11] The knowledge of the position of MF is important in clinical dentistry when administering local or regional anesthesia, orthodontic tooth movement/surgery, periapical surgery, and implant placement in the mental region of the mandible. The MF is occasionally misdiagnosed as a radiolucent lesion in the periapical area of the mandibular premolar region.[12] The MF also aids in interpreting anatomical landmarks in oral and forensic pathology.[13] The MF has been reported to vary in its position in different genders and ethnic groups having different craniofacial skeletal and dental occlusion.[14] The wall of the MF is made up of cortical bone. The density of the foramen's image on radiographs varies, as does the shape and definition of its border.
The use of appropriate imaging techniques is, therefore, essential to enable the accurate identification and location of these vital structures. The digital two-dimensional (2D) intraoral and panoramic radiographies have been widely used by dentists in the last decade. However, 2D radiographic images are difficult to interpret because of the superimposition of complex osseous structures and inherent magnification distortion, typically 20%–30%.[7] Moreover, panoramic radiograph lacks spatial information concerning the buccolingual direction. The anatomical structures such as the lingual foramen, MIC, IAC can hardly be defined. In addition, the lingual cortical bone of the mandible and the width of the alveolar ridge cannot be accurately assessed. Hence, with the development of computed tomography (CT), 3D assessments of craniofacial structures have become a possible and widely available means for head-and-neck diagnosis and treatment planning. However, CT is still not ideal for particular diagnostic task in dental applications. The excessive radiation exposure, increased cost, and limited availability impede the routine use of this technology for dental applications. Now, CBCT offers a promising alternative approach because it provides submillimeter resolution images of high diagnostic quality with short time and reduced radiation dose of up to 15 times lower than that of multislice CT scans and produces images that demonstrate on different planes and real size of anatomical structures.[8] In recent years, several studies have analyzed the characteristics of anatomical landmarks in the mandibular anterior region in various populations around the world. Nevertheless, to date, few studies have evaluated CBCT in population from North-West India. With this background, the present study was conducted to evaluate the vital anatomical structures in the mandibular interforaminal region and to investigate the presence of sexual dimorphism and differences with respect to the left and right side regions using CBCT.
MATERIALS AND METHODS
This cross-sectional study was conducted on randomly selected eighty CBCT scans taken as a part of the planning procedure/diagnostic workup for implant placements, orthognathic surgeries, bone harvesting from the chin, and mandibular osteotomies. The study sample consisted of forty males and forty females, between the age of 20 and 70 years. The CBCTs were performed in a private maxillofacial radiology clinic. All the scans were taken by the same technologist, following a standardized protocol for patient positioning and exposure parameter settings. Informed written consent in both local and English language was taken for each patient. Institutional ethical committee clearance was obtained before the conduct of the study. The inclusion criteria consisted of (1) patients who are fully dentate in the posterior regions of both sides; (2) cone-beam CT scans displaying the entire mandibular bone of both sides, free of large pathologies; (3) absence of pathology that could affect the position of MF, AL, or MIC; and (4) CBCT images with high geometric resolution. The exclusion criteria considered were (1) CBCT of patients with a history of maxillofacial trauma, fracture, or supernumerary or impacted teeth in region of interest (ROI); (2) patients with a history of surgical intervention in the mandible, those with neurogenic disorders, or those with systemic diseases affecting bones; (3) syndromic patients; (4) pregnant females; (5) those with the presence of bifid mandibular canal or accessory MF; (6) scans with positioning errors that the inferior border of the mandible is not recorded well and images were not of perfect quality; and (7) presence of implants or metal artifacts in the mandibular interforaminal region.
The patients selected according to the inclusion and exclusion criteria were evaluated thoroughly by making them seated comfortably on the dental chair. Diluted 0.2% chlorhexidine gluconate mouthwash was given to rinse the oral cavity. A detailed case history including the individuals' demographic details (age, gender, address, etc.) and general and medical history followed by thorough clinical examination were carried out in a systematic manner. Then, hard tissue intraoral examination was carried out for each patient for the number of teeth present, presence or absence of dental caries, calculus, gingival recession, and periodontal pockets, and the findings were entered in a specially designed pro forma.
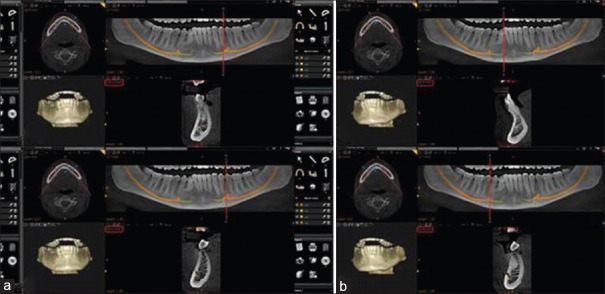
After the clinical examination, the CBCT scan of the selected patients was accomplished with a cone-beam volumetric tomography device CS 9300 (Carestream Dental Health Inc. 2012, Rochester, New york, USA) adjusted at 80 kVp, 15 mA and at voxel size of 0.3 × 0.3 × 0.3 [Figure 1]. The CBCT images were taken with a field of view of 10 × 5 (mandible only) and 17 × 13.5 (full mouth) and were used only if they cover the region of interest (ROI) and matched the inclusion criteria. Furthermore, the density and contrast of the images were adjusted using CS 3D imaging software version 3.71 (Carestream Dental Health Inc. 2012, Rochester, New York, USA) Care Stream Health Inc. software to assist the evaluators during identification and measurement procedures. The acquired images were reconstructed into multiplanar views (axial, panoramic, and cross-sectional) for evaluation of the following parameters:
Figure 1.

Cone-beam computed tomography machine (CS 9300 Care Stream) showing patient position
Mental foramen
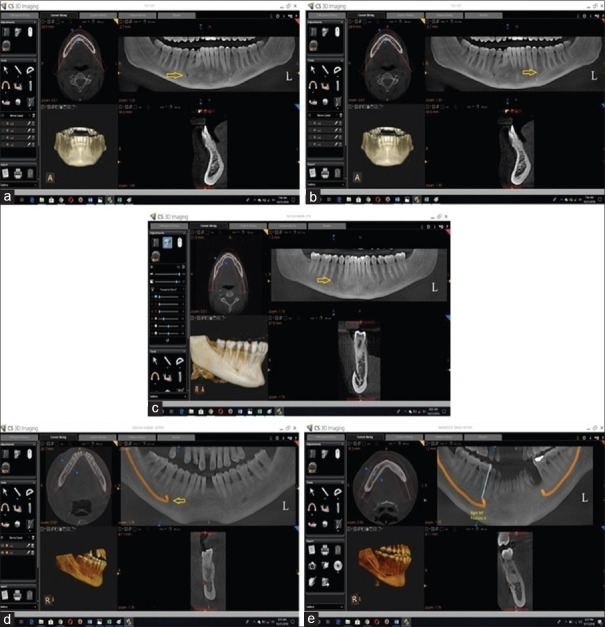
The MF position[9] was assessed relative to the adjacent mandibular teeth on the right and left sides as: position 1: between canine and first premolar; position 2: below the first premolar; position 3: between the first and second premolars; position 4: below the second premolar; position 5: between the second premolar and first molar; position 6: below the first molar [Figure 2].
Figure 2.
Different positions of mental foremen: (a) position 2: below the first premolar, (b) position 3: between the first and second premolars, (c) position 4: below the second premolar, (d) position 5: between the second premolar and first molar, (e) position 6: below the first molar
The position of MF was also recorded on the basis of gender and symmetry or asymmetry.
Symmetrical
Symmetrical was defined as MF on both sides with same anteroposterior position relative to the teeth.
Asymmetrical
Asymmetrical was defined as MF on both sides with different anteroposterior position relative to the teeth.
The shape of MF was recorded as oval, round, and irregular.
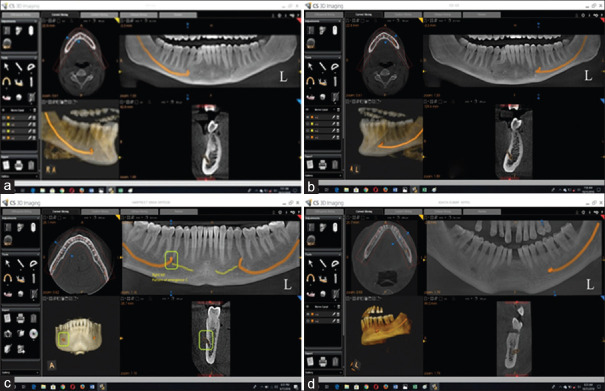
The emergence patterns of the mental canal (the anterior opening of the mandibular canal) and MF openings were assessed as follows: pattern A: superiorly, pattern B: posterosuperiorly, pattern C: labially, pattern D: mesially (anteriorly), and pattern E: posteriorly [Figure 3].
Figure 3.
Cone-beam computed tomography scans showing emergence patterns of the mental canal and normal foramen opening (a) superiorly, (b) posterosuperiorly, (c) labially, and (d) posteriorly
Anterior loop and mandibular incisive canal
The axial reconstruction image was initially used for the evaluation of AL and MIC. The volume was rotated toward the side being analyzed in order to position the long axis of the mandibular canal parallel to the sagittal plane and to position the coronal reconstruction perpendicular to the ROI. The coronal reconstruction images were then used, and immediately afterward, the most mesial point of MF was obtained in order to identify the presence or absence of an AL. In the coronal sections, it was possible to identify two basic types of images: one with an anterior extension represented by a single, round hypodense image and the other characterized by two round hypodense images. The AL was differentiated from the MIC based on the fact that the MIC has a diameter of <3 mm (according to Apostolakis and Brown). When only a single, round hypodense image was visualized, it was interpreted as the MIC if it exhibited a diameter <3 mm. If the diameter was >3 mm, the anterior extension of the mandibular canal was considered to be AL. An AL was also considered to be present when two round hypodense areas were observed, with one corresponding to the lumen of the mandibular canal that transverses the MF anteriorly and inferiorly and the other reflecting the doubling back (loop) of the mandibular canal, leading to the externalization of the IAN.
The length of AL was measured between the anterior border of the AL and the anterior margin of the MF. The vertical cursor in the panoramic image was positioned at the aforementioned sites respectively, and the site measurements indicated at the corner of the cross-sectional window were noted. The length of AL (in mm) was calculated by subtracting the measurements.
The MIC length was determined by measuring the distance in millimeter between the most anterior border of the MF and the most mesial slice where the canal was definitely visible in cross-sectional images [Figure 4].
Figure 4.
Cone-beam computed tomography showing measurement of anterior loop (a) of the mental nerve and mandibular incisive canal (b)
In addition, the differences with respect to the left and right sides and the presence of sexual dimorphism were also investigated. A pilot study was conducted on five CBCT scans to examine the interobserver reliability among the two considered trained maxillofacial radiologists. Both the examiners were asked to record the MF symmetry, MIC length, AL extent and emergence patterns of the mental canal on the same individuals. After recording the data of the respective parameters, the interobserver reliability was calculated among the two examiners. The data thus collected were tabulated and statistically analyzed using SPSS 18.0 (Microsoft Corporation Inc., Chicago, IL, USA) statistical software.
RESULTS
The overall mean age of the patients (forty males and forty females) was found to be 42.64 ± 16.22 years, with males having slightly more age than females although the difference was insignificant. A pilot study was conducted on five patients to examine the interobserver reliability among the two examiners. Both the examiners were asked to record the MF symmetry, MIC length, AL extent, and emergence patterns of the mental canal on the same patients. After recording the data of the respective parameters, the interobserver reliability was calculated among the two examiners, which was found to be 0.93, 0.91, 0.92, and 0.88 for MF symmetry, MIC length, AL extent, and emergence patterns of the mental canal, respectively. Interobserver values indicated a high degree of reliability [Table 1]. Therefore, for further statistical interpretation, any examiner recordings of the respective parameters can be used. In the present study, the most common positions noted for MF of the right side related to teeth on CBCT were position 4 (in line with the apex of the second premolar) and position 3 (between the apices of the first and second premolars) for males (for both position, n = 15; 37.5%), whereas for females, the corresponding was position 4 (n = 18; 45%). On the left side of the mandible, both the genders showed position 3 to be most common (males n = 18; 45% and females n = 22; 55%) [Table 2]. On applying Chi-square test, no association was found between genders and MF position for either side (P > 0.05). The position 1 (anterior to apex of the first premolar) of MF was not found in any of the CBCTs studied. Out of eighty CBCTs of the mandibles studied, sixty CBCTs showed symmetrical positions of MF, with the most common location being position 3, whereas the most common asymmetrical position (n = 20) noted was position 4. The majority of MF was oval in shape (n = 76), followed by round (n = 54), and the remaining were considered irregular (n = 30) in shape. Only the left side showed statistically significant differences between the shapes of MF and genders (P = 0.013).
Table 1.
Interobserver reliability
| Variables/parameters | Interobserver reliability | P |
|---|---|---|
| Mental foramen symmetry | 0.93 | <0.01* |
| Mandibular incisive canal length | 0.91 | <0.01* |
| Anterior loop extent | 0.92 | <0.01* |
| Emergence pattern of the mental canal | 0.88 | <0.01* |
*P<0.05 is statistically significant and P>0.05 is insignificant
Table 2.
Association between gender and position of right and left mental foramens
| Mental foramen position | Right | Left | Total | |||
|---|---|---|---|---|---|---|
| Male, n (%) | Female, n (%) | Male, n (%) | Female, n (%) | Right, n (%) | Left, n (%) | |
| Position 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Position 2 | 6 (15.0) | 2 (5) | 4 (10) | 0 | 8 (10) | 4 (5) |
| Position 3 | 15 (37.5) | 16 (40) | 18 (45) | 22 (55) | 31 (38.8) | 40 (50) |
| Position 4 | 15 (37.5) | 18 (45) | 13 (32.5) | 12 (30) | 33 (41.2) | 25 (31.2) |
| Position 5 | 3 (7.5) | 4 (10) | 4 (10) | 6 (15) | 7 (8.8) | 10 (12.5) |
| Position 6 | 1 (2.5) | 0 | 1 (2.5) | 0 | 1 (1.2) | 1 (1.2) |
| Total | 40 | 40 | 40 | 40 | 80 | 80 |
| χ2 | 3.448 | 5.840 | 4.107 | |||
| P | 0.486 | 0.21 | 0.392 | |||
n: Number of patients
Regarding the prevalence of various emergence patterns of mental canal from MF, the most common pattern noted on the right side was pattern B (posterosuperiorly) for both genders (males n = 18; females n = 21), whereas on the left side, males showed pattern B (n = 20) and females showed pattern A (superiorly; n = 21) to be most common. Overall, pattern B (n = 76) was noted most commonly in eighty CBCTs studied, and no association was found between genders and emergence patterns of mental canal for either side (P > 0.05) [Table 3].
Table 3.
Association between gender and emergence pattern of right and left mental foramens
| Emergence pattern of mental foramen | Right | Left | Total | |||
|---|---|---|---|---|---|---|
| Male, n (%) | Female, n (%) | Male, n (%) | Female, n (%) | Right, n (%) | Left, n (%) | |
| Pattern A | 15 (37.5) | 17 (42.5) | 17 (42.5) | 21 (52.5) | 32 (40) | 38 (47.5) |
| Pattern B | 18 (45.0) | 21 (52.5) | 20 (50.0) | 17 (42.5) | 39 (48.8) | 37 (46.2) |
| Pattern C | 1 (2.5) | 0 | 0 | 0 | 1 (1.2) | 0 |
| Pattern D | 0 | 0 | 0 | 0 | 0 | 0 |
| Pattern E | 6 (15) | 2 (5.0) | 3 (7.5) | 2 (5.0) | 8 (10) | 5 (6.2) |
| Total | 40 | 40 | 40 | 40 | 80 | 80 |
| χ2 | 3.356 | 0.864 | 2.259 | |||
| P | 0.340 | 0.649 | 0.520 | |||
n: Number of patients
Out of the total 160 ALs studied of both sides, at least one AL of the mandibular canal was visualized in 53.13% in our sample. The Chi-square test showed no statistically significant differences between the right and left sides in terms of the presence of AL (P = 0.87). Out of the eighty CBCTs images studied, 69 scans had bilateral AL (86.3%), whereas 11 had unilateral (13.7%). The mean length of AL noted on the right side for both genders was 1.22 ± 1.92 mm, whereas on the left side, it was 0.92 ± 1.14 mm. The overall mean length of AL for both sides was found to be 1.07 ± 1.42 mm. The findings of t-test did not show statistically significant differences between the mean lengths of AL in both sides and for both genders (P = 0.28) [Table 4].
Table 4.
Mean length of mandibular anterior loop
| Gender | Mean±SD | ||
|---|---|---|---|
| Right (in mm) | Left (in mm) | Total (in mm) | |
| Male | 0.96±1.36 | 1.08±1.32 | 1.02±1.10 |
| Female | 1.47±2.92 | 0.75±1.18 | 1.11±1.69 |
| Total | 1.22±1.92 | 0.92±1.14 | 1.07±1.42 |
| t-test | 1.01 | 1.18 | 0.28 |
| P | 0.32 | 0.24 | 0.78 |
SD: Standard deviation
The present study showed the existence of MIC in 93.75% of the patients. Three patients had symmetrical absence of MIC and four showed absence of either side only. The mean length of MIC noted on the right side for both genders was 12.90 ± 6.11 mm, whereas on the left side, it was 11.28 ± 6.17 mm. The overall mean MIC length for both sides was found to be 12.09 ± 5.95 mm. The findings of t-test did not show statistically significant differences between the mean lengths of MIC in both sides and for both genders (P = 0.35) [Table 5].
Table 5.
Mean length of mandibular incisive canal
| Gender | Mean±SD | ||
|---|---|---|---|
| Right (in mm) | Left (in mm) | Total (in mm) | |
| Male | 14.17±6.88 | 11.26±6.93 | 12.72±6.22 |
| Female | 11.62±6.07 | 11.30±6.86 | 11.46±5.66 |
| Total | 12.90±6.11 | 11.28±6.17 | 12.09±5.95 |
| t-test | 1.76 | 0.03 | 0.95 |
| P | 0.08 | 0.98 | 0.35 |
SD: Standard deviation
Moreover, no correlation was found between MF positions with emergence patterns of mental canal from MF for either side (P > 0.05) [Table 6].
Table 6.
Correlation of mental foramen positions with emergence patterns of mental canal
| Variables | R | P |
|---|---|---|
| Mental foramen right position with right emergence pattern of mental canal | −0.02 | 0.86 |
| Mental foramen left position with left emergence pattern of mental canal | −0.13 | 0.25 |
DISCUSSION
The planning of dental implants and curative interventions of the jaw require detailed anatomical knowledge of the exact position of the regional structures. In order not to cut or damage the branches of mental nerve, it is important for the operator to know the normal anatomy of mandibular intermental foraminal region.[10] The IAN is the most commonly injured nerve (64.4%), followed by the lingual nerve (28.8%) in oral surgery procedures. This could lead to permanent neurosensory disturbance to the lower lip after dental implant placement in the interforaminal region in 7%–10%.[11] Complications such as loss of the lip and chin sensation may result in lip biting, impaired speech, and diminished salivary secretion. Historically, it is believed that the course of IAN comes directly out of the MF in a straight horizontal projection from its posterior course. Medial to the MF, studies confirmed the existence of MIC, lingual foramen, and AL formation, and these structures contain some neurovascular bundle. The present study was conducted to evaluate these mandibular interforaminal structures in patients aged between 18 and 60 years using CBCT because variation in the position of these anatomical structures can occur due to aging.[12] Moreover, the mixed dentition and permanent tooth buds might obscure the view of these structures in early adolescent age.
Regarding imaging modality to be used for evaluating mandibular interforaminal region, periapical radiographs can produce image distortion due to angulation, and this may account for inability to detect the mandibular anterior interforaminal structures. Second, it can be difficult to record these structures when they are placed deep and inferiorly in the mandibular jaw. Third, in thin mandibular bone, these cannot be properly identified due to lack of radiographic contrast. In contrast, panoramic radiographs show average linear errors during routine assessments in 24% of films. The CBCT provides multiplanar reconstructions and true-to-size images at very low radiation dosage, which enables excellent resolutions and good contrast for the visualization of these dento-alveolar interforaminal structures compared to CT and conventional radiographic view.[13] The CT acquires image data using rows of detectors, whereas CBCT exposes the whole section of the patient over one detector.
In our series of eighty CBCTs scans, the most common position for the MF was between first and second premolars. Sexual dimorphism was not found (P > 0.05) regarding positions of MF in the studied population. The position was determined along the long axis of the teeth, considering the whole width of the teeth. Similar results were seen by Moiseiwitsch et al.[14] in a North American Caucasian population and also by Fishel et al.[15] and Olasoji et al.[16] in Northern Nigerian adults. In another similar study done on Punjabi Indians using orthopantomographs, MF was located mostly between the roots of the first and second premolars. On the contrary, few previous similar studies performed in other populations such as Malays, Asian Indians, Kenyan, Africans, and Moroccans found the most common position for the MF was found in line with the longer axis of mandibular second premolars. The difference in results could be due to genetics, which play an important role in determining the morphological characteristics of dental structures. According to Yesilyust et al.,[17] the position of MF may vary in different ethnic groups. It also depends on the imaging modality used for the evaluation of position, as according to Sonik et al.,[18] panoramic radiographs have average linear errors of 24% which may affect the positioning of MF.
The MF had similar bilateral positions in 75% of the patients, whereas past studies by Verma et al.[19] and Al-Khateeb et al.[20] reported similarities in 67%, 61.6%, 80%, and 84.4% of the cases. The difference in the bilateral positions of MF may occur if the MF is funnel shaped in the buccal cortex of the mandible. The mental canal passes from the posterior to the superior border of the mandible. In the present study, oval-shaped MF (47.5%) was most commonly reported. Very few were unidentified, which were excluded from the study. The literature also supports this finding.
Available date confirm our findings that the mental nerve most frequently emerges from a posterosuperior (position B; 47.5%) orientation without any significant difference between sides and gender. Warwick in 1950 first suggested that the posterior inclination of the MF was related to the development of the human chin. This view found support in the writing of Montagu[21] who suggested that the gradient of growth of the mandible was directed posterosuperiorly and hence the foramen would be expected to open in the same direction. De Villiers[22] showed that in young Negro skulls with unerupted first molars, the MF emerged with an anterior inclination. This changed to a posterior inclination with the eruption of second deciduous molar. Subsequently, it was argued that this change in orientation could be ascribed to the forward growth of the mandible, which dragged the neurovascular bundle along with it. Kjaer et al.[23] showed that the prenatal location of the MF is beneath the interdental septum between the primary canine and primary first molar teeth. From this, it was postulated that positional change in the orientation of the MF results from a combination of osseous growth and mesial drift of the dental anlagen. Other explanations might be that the shape and orientation of the mental canal opening is modified by soft-tissue factors such as the action and pull of the developing muscles of facial expression.
In our study, at least one AL of the mandibular canal was visualized in 53.13% of the patients. This is higher than the prevalence reported by Kuzmanovie et al., Kaya et al., and Ngeow et al.,[24] who conducted their studies using panoramic radiographic images. The relatively low prevalence rates reported in those studies may reflect the failure of panoramic radiography to detect the presence of the anterior loop, due to the limitations and disadvantages of radiography such as two dimensionality, distortion, the presence of overlapping structures, and calcification degree of the cortex, which appear radiopaque in radiographic images. Moreover, panoramic radiography can overestimate or underestimate the presence and extent of the AL and is not considered a reliable modality for evaluating the mandibular interforaminal anatomical variations. In contrast, studies using anatomical analysis or 3D images have demonstrated higher rates of prevalence for AL, with values ranging from 34% to 88%. Santos et al.,[25] even using CBCT, observed a prevalence of 22% and 28%. However, Jacobs et al.[26] reported the presence of AL in only 7% of the CT in Belgian patients, whereas Li et al. verified a prevalence of 83.1% of AL using spiral CT scans in the Chinese population. These differences could be explained by the fact that different radiographic techniques, different methods of measurements, and the inexistence of a specific definition of AL are recurrent in literature. In the present study, more than half of the patients had ALs bilaterally, followed by the left side and right side. These findings are similar to those reported by Apostolakis and Brown who observed an AL in approximately 57% of patients mostly bilaterally. In the survey conducted by Filo et al., a loop was identified in 78.84% of patients, with majority being bilateral, followed by being on the right and left sides.
ALs ranging from 0 to 9 mm have been reported. In our study, the mean value of the AL was 1.07 ± 1.42 mm, coinciding with the values found by other authors also using CBCT. However, in a study performed in South-Eastern Brazil, a mean 2.41 mm length of AL was found in the analyzed CBCT scans. These differences may be at least partly due to the racial influence. A safe distance anterior to the MF is required when performing surgery in the mandibular interforaminal region. About 6 mm safe distance anterior to the MF is frequently recommended especially when the AL of the mental nerve cannot be determined definitely or without the use of CBCT or CT. There are also other suggestions from 1 to 4 mm for the safe distance anterior to the MF. These diverse recommendations for the safe distance reflect the length variations of the AL in each patient, therefore a fixed distance anterior to the MF is not safe and the AL length should be determined for each patient to avoid injury to the mental nerve. In our study, the anterior limit of the AL was determined both based on the existence of two separate canals beyond the MF and by using its diameter in all the cross sections of CBCT scans. For this purpose, a minimum diameter of 3 mm was established, similar to the values used in other studies. In contrast, Santos et al. and Kaya et al.[27] did not measure the diameter of the canal and considered the AL to be present only in cross sections with two round hypodense images, with a structure that they referred to as “8 like.” This method would have underestimate the real AL length. In addition, no significant difference was found between the right and left sides in our studies; similar results were also noted in other studies. In contrast, some authors have found that the length of AL is significantly related to male gender, the right side, and the sixth decade of life.
MIC was first described by Olivier, who defined it as a continuation of the IAN, traveling through a canal or through vacuoles in spongy bone mesially from the MF. A relatively precise knowledge of the location of this anatomical structure is of extreme importance prior to any surgical procedure in the region in order to avoid potential neurovascular complications. In addition, the visibility of the MIC is poorly documented in panoramic images. In 1996, Rosenquist was the first to suggest that an implant placed in the MIC may fail to ossteointegrate and edema of the epineurium, caused by trauma, may spread to affect the nerve and cause neurosensory dysfunction of its main branch. The present study showed 93.75% visibility of the MIC by CBCTs, with a mean length of 12.09 ± 5.95 mm. The same results were found in the study by Pires A Carlos et al. and Jacobs et al.,[26] documenting 83% and 93% existence of MIC on CBCTs and spiral CTs, respectively. In contrast, in most of the cadaver dissection studies, it is possible to find 100% of existence of the MIC/nerve. The reason could be that the MIC becomes smaller while progressing from distal to the anterior part of the mandible to midline, so, sometimes, MIC narrows as it approaches the midline, and its visibility might be hindered by limited spatial and contrast resolution and by the partial volume-averaging effect inherent in the CBCT images. Further studies using 3 Tesla magnetic resonance imaging scanners that scan at a much higher resolution may show results of MIC that are similar to results from cadaver dissection studies. For all the CBCT images examined, the mean length of the MIC for the right side was 12.90 ± 6.11 mm and for the left side was 11.28 ± 6.17 mm. Despite the apparent difference between sides, there was no significant difference noted. There was also no significant difference between the genders. Similar lengths were obtained by Ross et al.[28] and Apostolakis and Brown, measuring 9.11 ± 3.00 mm and 8.9 mm, respectively. Pires et al.[29] verified MIC lengths of 7.14 ± 4 mm and 6.6 ± 3.7 mm for the right and left sides, respectively. The difference in the finding can be attributed to racial intrinsic differences existent in the bone structure of men and women (smaller mandible) on both sides. Bar-Ziv reported that sensory disturbance in the region of the mental nerve after implant placement was caused by damage to a “long MIC with a large diameter for orthognathic surgery. DICOM data from CBCT can be used to fabricate physical stereolithographic models or to generate virtual 3D models. Such 3D reconstructions are most useful for morphological analysis and finding the spatial relationship of the neighboring structures as well as for growth and developmental anomalies, gross tumor development, or fracture displacement.[30]
The main shortcoming of the present study is that it is a small sample sized study; hence, a large sample sized study needs to be conducted for substantiating the usefulness of the present study results.
CONCLUSION
It can be concluded that there may be large variations in the anatomical landmarks in the mandibular intermental foraminal region, therefore the concept of “a safe region” during surgical procedures in the interforaminal region should be questioned and a detailed study of the region must be performed using multiplanar images of CBCT during preoperative surgical planning. Our study showed that oral radiologist obtains high rates of identification of AL and MIC when CBCT images are used. The large variations in the lengths of AL and MIC were obtained, so it is suggested that preoperative radiographic evaluation of both should be carried out case by case, using CBCT scans which could clearly show the 3D structures. In addition, the most common horizontal location of MF was below the apex of second premolars, with its oval shape being noted more commonly while the posterosuperior emergence pattern of mental nerve from MF was maximally seen. In our study, no significant difference could be determined between sides and gender for any of the studied parameters of interforaminal region. The clinical significance of this study can be realized by doing thorough mapping of AL, MF, and MIC, specifically before implant placements and chin graft protocol for harvesting donor bone using CBCTs. Follow-up CBCT imaging is useful in evaluating the success of orthognathic surgery, as well as to measure the displacement of the surgical segments in all the three orientations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aglarci OS, Güngör E, Altunsoy M, Nur B, Ok E. Three-dimensional analysis of mandibular foramen location: A cone beam computed tomography study. OMICS J Radiol. 2015;4:179. [Google Scholar]
- 2.Greenstein G, Tarnow D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J Periodontol. 2006;77:1933–43. doi: 10.1902/jop.2006.060197. [DOI] [PubMed] [Google Scholar]
- 3.Uchida Y, Yamashita Y, Goto M, Hanihara T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the inter-foraminal region. J Oral Maxiilofac Surg. 2007;65:1772–9. doi: 10.1016/j.joms.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 4.Juodzbalys G, Wang HL, Sabalys G. Guidelines for the identification of the mandibular vital structures: Practical clinical applications of anatomy and radiological examination methods? J Oral Maxillofac Res. 2010;1:e2. doi: 10.5037/jomr.2010.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat. 2004;26:329–33. doi: 10.1007/s00276-004-0242-2. [DOI] [PubMed] [Google Scholar]
- 6.Phillips JL, Weller RN, Kulild JC. The mental foramen: 1.Size, orientation, and positional relationship to the mandibular second premolar. J Endod. 1990;16:221–3. doi: 10.1016/s0099-2399(06)81674-2. [DOI] [PubMed] [Google Scholar]
- 7.Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: A second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–50. doi: 10.1016/j.joms.2008.05.352. [DOI] [PubMed] [Google Scholar]
- 8.Mardinger O, Chaushu G, Arensburg B, Taicher S, Kaffe I. Anterior loop of the mental canal: An anatomical-radiologic study. Implant Dent. 2000;9:120–5. doi: 10.1097/00008505-200009020-00003. [DOI] [PubMed] [Google Scholar]
- 9.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of Cone Beam Computed Tomography (CBCT) and Multi-Slice CT (MSCT) Part I.On subjective image quality. Eur J Radiol. 2010;75:265–9. doi: 10.1016/j.ejrad.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 10.Al-Faleh W, Zahrani AA. Observer agreement in the radiographic assessment of mental foramen appearance on panoramic radiographs. Pakistan Oral Dent J. 2005;25:225–8. [Google Scholar]
- 11.Neo J. Position of the mental foramen in Singaporean Malays and Indians. Anesth Prog. 1989;36:276–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Baxmann M. Mental paresthesia and orthodontic treatment. Angle Orthod. 2006;76:533–7. doi: 10.1043/0003-3219(2006)076[0533:MPAOT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Robinson RC, Williams CW. Documentation method for inferior alveolar and lingual nerve paresthesias. Oral Surg Oral Med Oral Pathol. 1986;62:128–31. doi: 10.1016/0030-4220(86)90029-0. [DOI] [PubMed] [Google Scholar]
- 14.Moiseiwitsch DM, Gungor E, Guven S, Unal M. Evaluation of mental foramen location in the 10-70 years range using CBCT. Niger J Clin Pract. 2005;2:33–45. doi: 10.4103/1119-3077.178915. [DOI] [PubMed] [Google Scholar]
- 15.Fishel D, Buchner A, Hershkowith A, Kaffe I. Roentgenologic study of the mental foramen. Oral Surg Oral Med Oral Pathol. 1976;41:682–6. doi: 10.1016/0030-4220(76)90325-x. [DOI] [PubMed] [Google Scholar]
- 16.Olasoji HO, Tahir A, Ekanem AU, Abubakar AA. Radiographic and anatomic locations of mental foramen in northern Nigerian adults. Niger Postgrad Med J. 2004;11:230–3. [PubMed] [Google Scholar]
- 17.Yesilyust A, Udhaya K, Sridhar J. Morphometric analysis of the mental foramen in human dry mandibles: A study on the south Indian population. J Clin Diagn Res. 2013;7:1547–51. doi: 10.7860/JCDR/2013/6060.3207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sonik A, Abraham J, Faiella RA. A comparison of the accuracy of periapical panoramic and computerized tomographic radiograph in locating the mandibular canal. Int J Oral Maxillofac Implants. 1994;9:455–60. [Google Scholar]
- 19.Verma P, Bansal N, Khosa R, Sachdeva SK, Verma KG, Patwardhan N, et al. Correlation of radiographic mental foramen position and occlusion in three different Indian population. West Indian Med J. 2015;64:269–74. doi: 10.7727/wimj.2014.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Khateeb T, Al-Hadi Hamasha A, Ababneh KT. Position of the mental foramen in a Northern regional Jordanian population. Surg Radiol Anat. 2007;29:231–7. doi: 10.1007/s00276-007-0199-z. [DOI] [PubMed] [Google Scholar]
- 21.Montagu MF. The direction and position of the mental foramen in the great apes and man. Am J Phys Anthropol. 1954;12:503–18. doi: 10.1002/ajpa.1330120404. [DOI] [PubMed] [Google Scholar]
- 22.De Villiers H. The Skull of the South African Negro: A Biometrical and Morphological Study. Johannesburg: Witwatersrand University Press; 1968. [Google Scholar]
- 23.Kjaer I, Fink-Jensen M, Andreasen JO. Classification and sequelae of arrested eruption of primary molars. Int J Paediatr Dent. 2008;18:11–7. doi: 10.1111/j.1365-263X.2007.00886.x. [DOI] [PubMed] [Google Scholar]
- 24.Ngeow WC, Dionysius DD, Ishak H, Nambiar P. A radiographic study on the visualization of the anterior loop in dentate subjects of different age groups. J Oral Sci. 2009;51:231–7. doi: 10.2334/josnusd.51.231. [DOI] [PubMed] [Google Scholar]
- 25.Santos RO, Coutinho MR, Panzarella FK. Morphometric analysis of mental foramen using CBCT. Int J Dent. 2008;2:133–5. [Google Scholar]
- 26.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat. 2004;26:329–33. doi: 10.1007/s00276-004-0242-2. [DOI] [PubMed] [Google Scholar]
- 27.Kaya Y, Sencimen M, Sahin S, Okcu KM, Dogan N, Bahcecitapar M. Retrospective radiographic evaluation of the anterior loop of the mental nerve: Comparison between panoramic radiography and spiral computerized tomography. Int J Oral Maxillofac Implants. 2008;23:919–25. [PubMed] [Google Scholar]
- 28.Ross A, Spadola L, Ratib O. Accessory mental foramen assessment using CBCT. J Oral Med Oral Pathol Oral Radiol Oral Surg. 2009;107:289–94. doi: 10.1016/j.tripleo.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Pires L, Fuentes R. Prevalence and morphometric analysis of mental foramen in human dry skulls. Int J morphol. 2007;35:931–7. [Google Scholar]
- 30.Cavalcanti Mde G, Antunes JL. 3D-CT imaging processing for qualitative and quantitative analysis of maxillofacial cysts and tumors. Pesqui Odontol Bras. 2002;16:189–94. doi: 10.1590/s1517-74912002000300002. [DOI] [PubMed] [Google Scholar]