Abstract
Background:
Limited bone quality in the posterior maxilla results in low success rates for dental implants. Various bone augmentation methods have been described, yet most require two-step surgical procedures with relatively high rates of resorption and failure. An alternative for these patients is zygomatic implants. Zygomatic implants utilize the basal craniofacial bone.
Materials and Methods:
A retrospective study was conducted on 25 patients exhibiting ridges classified as V–VI according to the Cawood and Howell classification. Seventy-six extramaxillary zygomatic implants were placed. Immediate rehabilitation was performed with a mean follow-up of 18.6 months.
Results:
Three implants failed, and two were replaced successfully. No significant bone loss was observed in the rest of the implants. Soft tissue around the implant heads healed properly. All implants were prosthetically rehabilitated successfully.
Conclusions:
Zygomatic implants allow for immediate loading of an atrophic maxilla. The emergence of the implant is prosthetically correct compared to the intrasinus approach, leading to better dental hygiene and decreased mechanical resistance. 96.1% of the implants survived, with good anchorage and proper soft tissue healing and rehabilitation. We suggest using extramaxillary zygomatic fixture as the first line of treatment in severe atrophic maxilla.
Keywords: Atrophic, extramaxillary, implant, maxilla, zygomatic
INTRODUCTION
Increase in lifespan and overall quality of life in the western and eastern world created a demand for a permanent, fully functional dental rehabilitation. With the increase in the prevalence of dental implants, restoring the dental arch using a fixed nonremovable dental rehabilitation became common. Aging, maxillofacial trauma, periodontal disease, endodontic failure, cysts, lesions, and ablative surgery can result in decreased alveolar bone volume [Figure 1]. Loss of hard tissue in the maxillary region results in decreased bone volume and decreased support for the soft tissue, thus enhancing soft tissue volume loss, which affects the facial appearance dramatically and results in an older appearance. In the maxilla, limited bone quantity and quality, especially in the posterior region, results in low success rates for dental implants. For assessing the quality and quantity of the alveolar bone, many practitioners use the Cawood and Howell classification [Figure 2].[1]
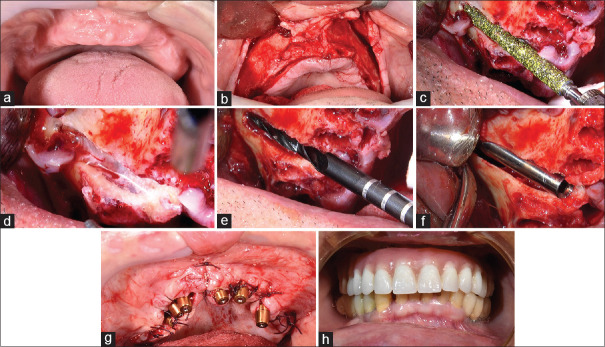
Figure 1.
A 43-year-old female suffering from total loss of dentition at a young age. The patient suffers from an atrophic maxilla secondary to the loss of teeth, resulting in an acquired maxilla–mandibular Class III relations, collapse of the lips, and an elderly appearance. Cone-beam computed tomography demonstrates the complete loss of maxillary alveolar bone. (a) Anterior view. (b) Three-dimensional reconstruction, anterior view. (c) Lateral view of the three-dimensional reconstruction
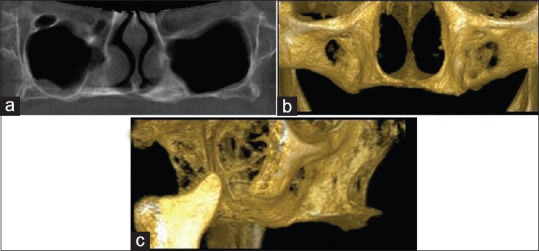
Figure 2.
Classification of bone resorption in the maxilla. (a) Anterior maxilla. (b) Posterior maxilla. Cawood and Howell
Various methods of bone augmentation have been described for reconstructing the atrophic maxilla. Among them autogenous block bone grafting; onlay and interpositional bone graft (smile osteotomy), guided bone regeneration (GBR) with a particulate graft, ridge splitting or expansion technique, osteotomies of the ridge or the jaws, distraction osteogenesis, microvascular free flaps and Le Fort I osteotomies combined with bone grafting.[2,3,4,5,6,7,8,9] Each of these methods has its advantages and disadvantages. Onlay bone graft is a simple procedure to master and the patient's own bone is used. Its disadvantages include a high rate of resorption, difficulty in obtaining soft tissue coverage and thus risk of premature bone exposure and failure of the graft and limitation in potential vertical bone augmentation, donor site morbidity, the need for vestibuloplasty, and plate removal. Interpositional bone grafts exhibit less resorption than onlay bone grafts, there is no need for vestibuloplasty, and implant placement is performed in the cortical bone. The disadvantages include donor site morbidity and limited vertical augmentation due to soft tissue closure. GBR includes no donor site morbidity, but is very limited in potential vertical bone gain. Microvascular free flaps result in proper skeletal and soft tissue coverage, and three-dimensional (3D) planning allows for accurate concomitant dental implant placement, yet requires extensive and prolonged operations with a second surgical site with increased morbidity and many times scars in the neck area and donor site. Distraction osteogenesis is not limited in vertical augmentation on account of soft tissue due to concomitant hard and soft tissue distraction. Distraction osteogenesis does not result in donor site morbidity, implants are placed in the cortical bone, minimal relapse is observed, and it results in increased attached mucosa. The disadvantages include the need of a second operation for device removal, difficulty in controlling the vector of bone augmentation, exposure of the bone and devices, and it is a technique-sensitive procedure which requires a learning curve.
An alternative approach for the reconstruction of an atrophic maxilla is zygomatic implants. These implants were first introduced by Brånemark at the late 1990s.[10] The concept behind the technique is bypassing the atrophic alveolar bone and using the strong, highly dense bone of the zygomatic complex as the anchoring unit for the implants.[11,12] The use of zygomatic implants increases treatment success and decreases the use of bone grafts, the number of surgical steps, and the length of the treatment.[13,14]
The method described by Brånemark, which is the most prevalent technique nowadays, is the intrasinus technique. This technique requires general anesthesia. The surgeon opens an elongated bone window starting in the alveolar crest and proceeding through the maxillary sinus to the zygomatic bone. The Schneiderian membrane is reflected. This technique may result in sinus pathologies and the emergence of the implants is usually located palatal to the alveolar crest.[15]
Lately, a new approach was introduced, the extramaxillary technique.[15] The extramaxillary technique is considered relatively new. The concept behind the method was to improve the previous techniques when addressing their disadvantages. The technique is based on longer implants, external to the maxillary sinus and anchored solely to the zygomatic bone.[15] We describe its advantages and the indications for placement and present our experience.
MATERIALS AND METHODS
This retrospective study included 76 zygomatic implants placed in 25 patients using the extramaxillary technique between 2014 and 2016, all performed by the same surgeon.
Inclusion criteria included patients who were not candidates/refused bone augmentation and dental implants. Inclusion criteria included maxillary sinus pathology, failure of previous sinus floor augmentation [Figure 3], alveolar ridges classified as Cawood and Howell V/VI [Figure 2], and patients status postmaxillectomy [Figure 4]. Exclusion criteria included patients with alveolar ridges classified as Cawood and Howell II–IV. Exclusion criteria included patients with alveolar ridges classified as Cawood and Howell II–IV [Figure 2].
Figure 3.

Maxillary sinus augmentation failure. Panoramic X-ray showing a zygomatic implant emerging in the right posterior maxilla. The zygomatic implant was inserted following failure of the right maxillary sinus augmentation
Figure 4.
Maxillary deficiency as a result from a maxillectomy. A 70-year-old female lacking the right maxilla. The patient underwent ablative surgery which included a right maxillectomy
All patients underwent cone-beam computed tomography preoperatively and panoramic imaging postoperatively.
All surgeries were performed using local anesthesia combined with intravenous sedation. A mucoperiosteal flap was elevated using a crestal incision from the maxillary tuberosity on one side to the contralateral side with two vertical releasing incisions. An additional incision is made in the buccal midline splitting the flap. Flap reflection allowed for infraorbital nerve identification and direct observation of the inferior edge of the zygomatic bone [Figure 5a and b]. Recontouring of the alveolar ridge was performed as needed. First, a tunnel is created through the residual alveolar ridge directing the diamond bur toward the center of ridge [Figure 5c]. The second stage includes creation of the elongated window lateral to the maxillary sinus, which enables the reflection of the Schneiderian membrane, exposing and marking the point of entry to the zygomatic bone [Figures 5c and d]. Next, drilling into the body of the zygomatic bone and preparation of the implant site is performed using two elongated drills, each with three different expanding diameters [Figure 5e]. During the drilling procedure, buccal palpitation of the zygomatic bone is important to assess buccal cortex penetration. Once the implant site is prepared, the zygomatic implant is inserted in a high torque, trying to establish bicortical stabilization sufficient for immediate loading. We used the Noris Medical zygomatic implants system (Haifa, Israel). The apical third of the implant contains threads which underwent surface treatment with alumina oxide, whereas the rest of the implant was only machine milled [Figure 5f]. It is structured this way because only the apical third is inserted into the bone. The manufactures claim that this design avoids soft tissue irritation. The buccal aspect of the occlusal half of the implant remains exposed and thus bone augmentation using a mixture of bovine bone (Cerabone®, Botiss biomaterials GmbH, Hauptstr, Germany) and alloplast graft (3D Bond™, Augma Biomaterials, Caesarea, Israel) is performed. Angulated multi-unit abutments were used in our cases to correct the angulation of the implants and to create an insertion path for an acrylic, screw-retained prosthesis [Figure 5g]. Closure of the flap is carried out using Vicryl and silk 3-0 sutures. Immediate rehabilitation was performed in all of our cases [Figure 5h]. Postoperative panoramic X-ray was obtained for all patients [Figure 6].
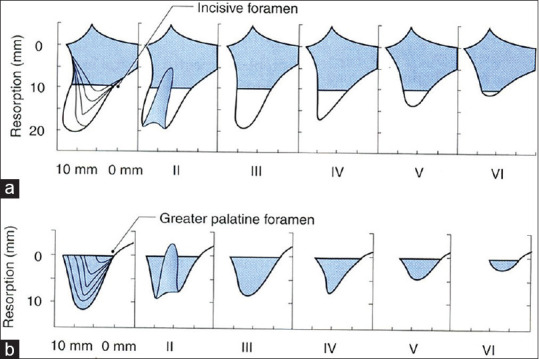
Figure 5.
Workflow of zygomatic implant insertion. (a) Deficient maxilla. (b) Mucoperiosteal flap. (c) Tunnel formation through the residual alveolar bone from the center of the ridge. (d) Elongated window lateral to the maxillary sinus and reflection of the Schneiderian membrane. (e) Marking the point of entry to the zygomatic bone and drilling into the zygoma. (f) The zygomatic implant is inserted in a high torque. Only the apical one third of the implant is inserted into the bone. (g) Angulated multi-unit abutments were used to correct the angulations. (h) Immediate prosthetic rehabilitation
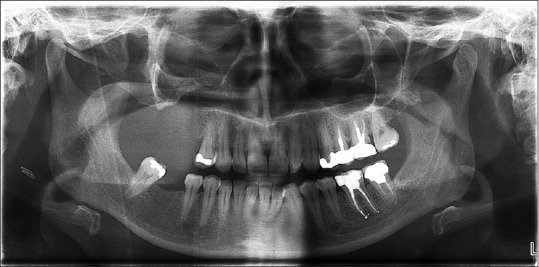
Figure 6.
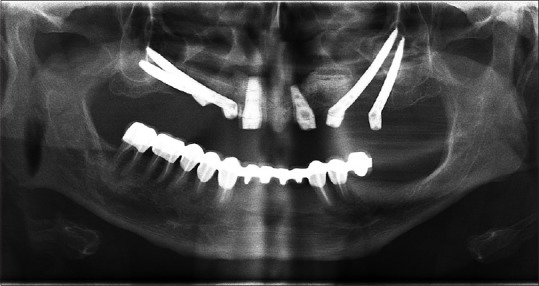
Postoperative panoramic X-ray. Two zygomatic implants can be observed on each side of the maxilla in addition to two regular endosseous dental implants in the anterior region
In every case, we aspired to place additional conventional dental implants in the anterior region. In cases of severe atrophy in the anterior region, two zygomatic implants were placed on each side or alternatively pterygoid implants were placed.
RESULTS
Twenty-five patients underwent insertion of seventy-six zygomatic implants and sixty-four conventional implants. Indications for zygomatic implants included severe bone deficiency and request for immediate loading in 76% of the patients, sinus floor augmentation failure in 12%, and one patient with each of the following: status postpartial maxillectomy, untreated cleft, and implant failure with severe bone deficiency. Eighty-eight percent of patients were healthy. One suffered from ischemic heart disease, one from cancer treated with partial maxillectomy and radiation, and one was a cleft palate patient.
Eighty-four percent of patients underwent insertion of conventional dental implants concomitantly with a minimum of two conventional dental implants. In 21 (84%) of patients, at least two zygomatic implants were inserted. Of the four who received only one zygomatic implant, one was rehabilitated following a partial maxillectomy and two underwent insertion of pterygoid implants apart from the zygomatic implant. A mean follow-up of 10.6 months was performed. In 18 (72%) of patients, a minimum follow-up of 8 months was performed.
All zygomatic implants were immediately rehabilitated. No failure of prosthetic rehabilitation was observed during the follow-up visits.
Three implants failed and were removed, and in two cases, new implants were inserted successfully. The results are summarized in Table 1.
Table 1.
Summarizing all zygomatic implants performed by us in the past 2 years
| Patient number | Health status | Indication | Number of zygomatic implants | Number of conventional implants | Follow-up duration (m) | Implant failure |
|---|---|---|---|---|---|---|
| 1 | - | Bone deficiency and request for immediate loading | 1+1 | 2+2 | 26 | - |
| 2 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 26 | - |
| 3 | - | Bone deficiency and request for immediate loading | 2+2 | - | 24 | 1 (redo) |
| 4 | - | Sinus floor augmentation failure | 1 | 2+2 | 22 | - |
| 5 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 22 | - |
| 6 | - | Bone deficiency and request for immediate loading | 2+1 | 1+2 | 22 | 1 |
| 7 | IHD | Bone deficiency and request for immediate loading | 1 | 2+3 | 22 | - |
| 8 | Cleft palate | Untreated cleft | 2+1 | 1+3 | 22 | - |
| 9 | - | Sinus floor augmentation failure | 1 | 3+5 | 22 | - |
| 10 | - | Bone deficiency and request for immediate loading | 1+1 | 2+2 | 20 | - |
| 11 | - | Implant failure and severe bone deficiency | 1+1 | 2+2 | 20 | - |
| 12 | S/P maxillectomy + radiation | Bone deficiency due to ablation surgery | 1 | 4 | 20 | - |
| 13 | - | Sinus floor augmentation failure | 1+1 | 1+1 | 20 | - |
| 14 | - | Bone deficiency and request for immediate loading | 1+1 | 2+2 | 19 | - |
| 15 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 17 | - |
| 16 | - | Bone deficiency and request for immediate loading | 2+2 | - | 17 | - |
| 17 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 16 | - |
| 18 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 16 | - |
| 19 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 14 | - |
| 20 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 14 | - |
| 21 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 14 | - |
| 22 | - | Bone deficiency and request for immediate loading | 2+2 | 1+1 | 14 | 1 (redo) |
| 23 | - | Bone deficiency and request for immediate loading | 2+2 | - | 12 | - |
| 24 | - | Bone deficiency and request for immediate loading | 2+2 | - | 12 | - |
| 25 | - | Bone deficiency and request for immediate loading | 2+2 | - | 12 | - |
The health status of the patients, indications for insertion of zygomatic implants, number of zygomatic and conventional implants inserted, follow-up duration, and failure rate. IHD=Ischemic heart disease; S/P=Status post
DISCUSSION
Dental implants for the rehabilitation of the edentulous maxilla are the standard of care nowadays, yet in some cases, achieving sufficient bone for their placement is very difficult or even impossible. In atrophic maxilla classified as Cawood and Howell V/VI, the 3D deficiency cannot be treated nowadays in one single procedure.
The vertical deficiency is large and requires extensive augmentation, which may require several procedures to achieve a favorable implant to crown ratio. Performing sinus floor augmentation to achieve an adequate bone volume for implant anchorage may be difficult. Using onlay bone augmentation requires soft tissue coverage, which may be hard to achieve in large deficiencies, and results in extensive resorption.[16] The buccopalatal deficiency which requires onlay bone augmentation is usually left unattended due to patient compliance and lack of soft tissue coverage and results in the need to angulate the implant for compensation. The improper angulation and cantilever of the prosthesis, results in shear forces on the implants and consequently high rates of failure in the long run.
In cases of severe maxillary atrophy, there is a reversal of the anteroposterior relations of the jaws. The sagittal anteroposterior deficiency requires a Le Fort I osteotomy and advancement.
In addition, patient compliance is difficult to achieve in all the above-mentioned procedures due to the need for long periods without applying pressure on the soft tissue and thus avoiding denture placement. Zygomatic implants are a simple, adequate solution for such cases. One procedure provides an adequate stable solution with the benefit of immediate loading. The extramaxillary technique was developed to address the disadvantages of the “classic” techniques, mostly the emergence of the implant head which is more prosthetically correct in the extramaxillary technique, thus leading to better dental hygiene, less disturbances to the tongue and thus better compliance, decreased mechanical resistance, and avoiding the disruption of the maxillary sinus, thus sparing possible pathologies.
We inserted 76 zygomatic implants in 25 patients, all in the extramaxillary technique. All of the implants were immediately rehabilitated. To date, three implants failed, and two were replaced at the time of implant removal. All of the surviving implants showed good stabilization and are functional, supporting prosthetic rehabilitation. Follow-up period ranged between 12 and 26 months, with a mean of 18.6 months. This period of follow-up is sufficient for short-term evaluation as immediate loading was performed, but is insufficient for long-term evaluation of stability and survival. Previous large-scale results showed most of the failures in zygomatic implants occurred in the 1st year following insertion (up to 9 months).[17] Maló et al. showed a cumulative success rate of 94.4% at 7 years.[17] Agliardi et al. showed 100% survival of 42 implanted zygomatic implants in an average period of 90.61 months.[18]
When adequate alveolar bone is present, we always place conventional dental implants in the anterior region for additional support. The zygomatic implant absorbs most of the posterior load, whereas the anterior conventional implants absorbed most of the anterior load.[19]
A disadvantage of this technique when comparing to the conventional intrasinus technique is the larger cantilever due to the anterior emergence of the implant in the arch. This effect can be reduced using a support system.[19]
Another disadvantage of this method is lack of support from the maxillary bone, yet current results in the literature[17] and our results show that anchorage is sufficient. Prolonged follow-ups are required for the evaluation of long-term stability and functionality.
CONCLUSIONS
We propose using zygomatic implants as the first choice of treatment for maxillary reconstruction in patients suffering from severe atrophy of the maxilla, following failure of sinus augmentation and postmaxillectomy. Demand of immediate loading without sufficient bony support for traditional dental implants is another indication for zygomatic implants. The extramaxillary technique addresses the disadvantages of the traditional techniques, thus decreasing the morbidity. Extramaxillary zygomatic implants provide an adequate stable solution with the benefit of immediate loading.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232–6. doi: 10.1016/s0901-5027(88)80047-x. [DOI] [PubMed] [Google Scholar]
- 2.Block MS, Haggerty CJ. Interpositional osteotomy for posterior mandible ridge augmentation. J Oral Maxillofac Surg. 2009;67:31–9. doi: 10.1016/j.joms.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Caplanis N, Sigurdsson TJ, Rohrer MD, Wikesjö UM. Effect of allogeneic, freeze-dried, demineralized bone matrix on guided bone regeneration in supra-alveolar peri-implant defects in dogs. Int J Oral Maxillofac Implants. 1997;12:634–42. [PubMed] [Google Scholar]
- 4.Jensen OT. Alveolar segmental “sandwich” osteotomies for posterior edentulous mandibular sites for dental implants. J Oral Maxillofac Surg. 2006;64:471–5. doi: 10.1016/j.joms.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 5.Jensen OT, Greer RO, Jr, Johnson L, Kassebaum D. Vertical guided bone-graft augmentation in a new canine mandibular model. Int J Oral Maxillofac Implants. 1995;10:335–44. [PubMed] [Google Scholar]
- 6.Nystrom E, Kahnberg KE, Gunne J. Bone grafts and Brånemark implants in the treatment of the severely resorbed maxilla: A 2-year longitudinal study. Int J Oral Maxillofac Implants. 1993;8:45–53. [PubMed] [Google Scholar]
- 7.Satow S, Slagter AP, Stoelinga PJ, Habets LL. Interposed bone grafts to accommodate endosteal implants for retaining mandibular overdentures. A 1-7 year follow-up study. Int J Oral Maxillofac Surg. 1997;26:358–64. doi: 10.1016/s0901-5027(97)80797-7. [DOI] [PubMed] [Google Scholar]
- 8.Triplett RG, Schow SR. Autologous bone grafts and endosseous implants: Complementary techniques. J Oral Maxillofac Surg. 1996;54:486–94. doi: 10.1016/s0278-2391(96)90126-3. [DOI] [PubMed] [Google Scholar]
- 9.Bottini GB, Brandtner C, Steiner C, Wittig J, Hartig F, List C, et al. Microvascular reconstruction and dental rehabilitation of benign severely atrophic jaws and defects of the alveolar ridge: Our philosophy in 2019. Br J Oral Maxillofac Surg. 2019;57:151–6. doi: 10.1016/j.bjoms.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Brånemark P. Surgery and Fixture Installation: Zygomaticus Fixture Clinical Procedures. 1st ed. Gothenburg, Sweden: Nobel Biocare; 1998. [Google Scholar]
- 11.Bedrossian E, Stumpel L, 3rd, Beckely ML, Indresano T. The zygomatic implant: Preliminary data on treatment of severely resorbed maxillae. A clinical report. Int J Oral Maxillofac Implants. 2002;17:861–5. [PubMed] [Google Scholar]
- 12.Pham AV, Abarca M, De Mey A, Malevez C. Rehabilitation of a patient with cleft lip and palate with an extremely edentulous atrophied posterior maxilla using zygomatic implants: Case report. Cleft Palate Craniofac J. 2004;41:571–4. doi: 10.1597/03-105.1. [DOI] [PubMed] [Google Scholar]
- 13.Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: A 6-48 months follow-up study. Clin Oral Implants Res. 2004;15:18–22. doi: 10.1046/j.1600-0501.2003.00985.x. [DOI] [PubMed] [Google Scholar]
- 14.Pi Urgell J, Revilla Gutiérrez V, Gay Escoda CG. Rehabilitation of atrophic maxilla: A review of 101 zygomatic implants. Med Oral Patol Oral Cir Bucal. 2008;13:E363–70. [PubMed] [Google Scholar]
- 15.Maló P, Nobre Mde A, Lopes I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: A pilot study. J Prosthet Dent. 2008;100:354–66. doi: 10.1016/S0022-3913(08)60237-1. [DOI] [PubMed] [Google Scholar]
- 16.von Arx T, Hardt N, Wallkamm B. The TIME technique: A new method for localized alveolar ridge augmentation prior to placement of dental implants. Int J Oral Maxillofac Implants. 1996;11:387–94. [PubMed] [Google Scholar]
- 17.Maló P, de Araújo Nobre M, Lopes A, Ferro A, Moss S. Extramaxillary surgical technique: Clinical outcome of 352 patients rehabilitated with 747 zygomatic implants with a follow-up between 6 months and 7 years. Clin Implant Dent Relat Res. 2015;17(Suppl 1):e153–62. doi: 10.1111/cid.12147. [DOI] [PubMed] [Google Scholar]
- 18.Agliardi EL, Romeo D, Panigatti S, de Araújo Nobre M, Maló P. Immediate full-arch rehabilitation of the severely atrophic maxilla supported by zygomatic implants: A prospective clinical study with minimum follow-up of 6 years. Int J Oral Maxillofac Surg. 2017;46:1592–9. doi: 10.1016/j.ijom.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 19.Ishak MI, Abdul Kadir MR, Sulaiman E, Abu Kasim NH. Finite element analysis of different surgical approaches in various occlusal loading locations for zygomatic implant placement for the treatment of atrophic maxillae. Int J Oral Maxillofac Surg. 2012;41:1077–89. doi: 10.1016/j.ijom.2012.04.010. [DOI] [PubMed] [Google Scholar]