Abstract
Aim:
The present study is designed to evaluate and compare the ability of serratiopeptidase and dexamethasone to control edema following the surgical removal of mandibular third molar.
Materials and Methods:
Two drugs, dexamethasone and serratiopeptidase, were compared for its efficacy in reducing the postoperative swelling. A total of 100 patients requiring the surgical removal of impacted mandibular third molar were randomly divided into two groups, consisting of 50 patients each. One group was administered 1 mg dexamethasone, one-half h preoperatively and every 8th hourly for 3 days postoperatively. The other group was given 10 mg serratiopeptidase every 8th hourly for 3 days postoperatively. The swelling was measured on 1st, 2nd, 5th, and 7th postoperative days. The results of this study showed that serratiopeptidase was effective in reducing swelling from 2nd to 5th postoperative day, and dexamethasone was effective in reducing swelling from 1st to 2nd postoperative day, further, it also reduced the swelling from 2nd to 5th postoperative day.
Results:
There was highly significant difference in the facial measurement between serratiopeptidase and dexamethasone group on postoperative day 2 (the mean difference was 62.5 with P < 0.001) and statistically significant difference on postoperative day 1, day 5, and day 7 (P < 0.01).
Conclusion:
It can be concluded that serratiopeptidase, a proteolytic enzyme and dexamethasone, a long-acting corticosteroid was effective in reducing the swelling, but dexamethasone was more effective than serratiopeptidase in reducing the swelling.
Keywords: Dexamethasone, impaction, serratiopeptidase
INTRODUCTION
The removal of impacted third molars involves trauma to soft and bony tissue, resulting in swelling.[1] It remains unclear as to why some of these surgical extractions are followed by considerable swelling, while others are affected to a much lesser degree.[2] The formation of postoperative edema, its complexities, and control has been the subject of perpetual interest to oral surgeons for many years. Therefore, its control has become a subject of scientific importance. Inflammatory response as a result of surgical trauma induced in oral surgical procedures is a normally expected phenomenon and is also a prerequisite for the subsequent healing process when present in the degree conducive to stimulate the process of repair. However, excessive postoperative edema is undesirable, as it adversely affects and delays the process of healing.[1]
When tissue damage occurs, large quantities of histamine, bradykinin, serotonin, and other substances are released into the surrounding area. These substances, especially histamine cause vasodilatation to occur, thereby increasing blood flow to the damaged area. The permeability of venous capillaries and venules is also increased. Leukocytes infiltrate into the damaged area and phagocytize invading microorganisms and debris. As a side effect of this process, there is an escape of fluid into interstitial spaces resulting in edema. The inflammatory process is necessary if healing is to occur, but often excessive inflammation causes edema leading to pain and trismus.[3]
Several types of medications such as antihistamines, enzymes, and steroids have been used to inhibit these postoperative sequelae. The principal effective physical method for relieving edema is the use of drains, while all the pharmacological agents tried, the anti-inflammatory steroids appear to be most successful and remain in common usage, even though its immunosuppressive effects are well recognized in medicine.[4] The use of corticosteroids to control inflammation following the third molar surgeries has been an area of dispute. Newer synthetic analogs of corticosteroids, with varying doses and different routes of administration, have been investigated over the years.[5] Dexamethasone is potent, highly selective long-acting, synthetic corticosteroids, which has anti-inflammatory action.[6] Previous studies on the use of dexamethasone to control postoperative edema have been concluded with an emphasis that there is a great need for well-designed clinical research to further evaluate protocols for corticosteroid use.[7] Serratiopeptidase, a proteolytic enzyme, decomposes bradykinin, thus producing anti-inflammatory action. Serratiopeptidase is promising from the knowledge of pharmacology of the enzymes and the pathology of the inflammatory edema. There is no sufficient evidence from the investigations regarding its efficacy in reducing postoperative edema, and hence, it can be investigated.[8]
The present study is designed to investigate, evaluate, and compare the ability of serratiopeptidase and dexamethasone to control edema following surgical removal of the mandibular third molar.
MATERIALS AND METHODS
The study was carried out on 100 patients, requiring surgical extraction of mandibular third molars from October 2004 to September 2006. Patients were enrolled for the study consecutively as and when they were presented. Selected patients were allocated to the dexamethasone group and serratiopeptidase group by randomization procedure, irrespective of age and sex. The following were the criteria for the selection of patients for the study.
Inclusion criteria
Bony impacted mandibular third molar
Routine blood and urine examination revealing no abnormal values
The first and second molar on the side of surgery must be present.
Exclusion criteria
The patients with systemic complications such as bleeding disorders
Recent swelling or infection in the area of surgery
Patients who took proteolytic drugs or steroids 1 day before surgery
Contraindication for the use of corticosteroids such as diabetes mellitus, active tuberculosis, ocular herpes, glaucoma, peptic ulceration, pregnancy, and hypertension.
Institutional ethical clearance was obtained for the study. Following informed consent of the patient and preoperative investigations, the patients were taken for surgery under local anesthesia. Dexamethasone group was given 1 mg of dexamethasone, one-half h before surgery and continued 1 mg, 8th hourly for 3 days postoperatively. Serratiopeptidase group was given 10 mg of serratiopeptidase, 8th hourly for 3 days postoperatively.
Preoperative measurements were taken by marking 7 points on the face with indelible ink on the following facial landmarks: mandibular angle, tragus, lateral canthus of the eye, alar base, lip commissure, pogonion, and the midpoint of the hyoid bone. With the mandibular angle as the base point and using 3-0 silk suture to follow the contour of the face, linear distances to the other landmarks were noted. The sum of all measurements was taken as the facial size. Cheek girth was measured by measuring the maximum width of the soft tissues in the anterior masseter region. It was measured in millimeters using calipers by keeping one of the limbs of the calipers intraorally in the embrasure between the first and second mandibular molars and the other limb extraorally, so as to touch approximately 1 cm above the anterior inferior border of the masseter [Figure 1].
Figure 1.
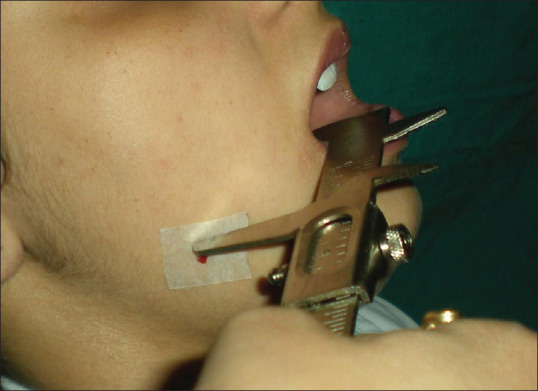
Cheek girth measurement
Standard surgical techniques and protocols were followed for surgical removal of the mandibular third molar. Amoxicillin, 500 mg and metronidazole, 400 mg were given orally, 8th hourly for 5 days, for prophylactic antibiotic coverage and diclofenac sodium 50 mg was given orally, 8th hourly for 3 days for management of postoperative pain. Facial size and cheek girth were measured on 1st, 2nd, 5th, and 7th postoperative days in the same manner, as preoperative facial measurements were recorded. The data were recorded for the statistical analysis. Paired Student's t-test was applied for intragroup comparison of facial measurement and cheek girth within the dexamethasone group and serratiopeptidase group. Unpaired Student's t-test was applied for intergroup comparison of facial measurement and cheek girth between the dexamethasone group and serratiopeptidase group.
RESULTS
The swelling was recorded on the 1st, 2nd, 5th and 7th postoperative days. The dexamethasone group consisted of 31 males and 19 females. The age range of the patients was 18–50 years with a mean age of 25.8 ± 7.1. The serratiopeptidase group consisted of 32 males and 18 females. The age ranges of the patients were 17–65 years with a mean age of 27.2 ± 9.8. Table 1 shows the changes in facial measurement in the serratiopeptidase group. It shows the mean difference in facial measurement on postoperative day 1, day 2, day 5, and day 7. There was highly significant reduction in facial measurement on the postoperative day 5 in the serratiopeptidase group.
Table 1.
Facial measurement (mm) of the serratiopeptidase group
| Time of assessment | Serratiopeptidase group | P* | ||
|---|---|---|---|---|
| Mean±SD | Difference from preoperative measurement (baseline) | Percentage increase from preoperative measurement (baseline) | ||
| Preoperative (baseline) | 475.6±73.4 | - | - | - |
| Postoperative (day 1) | 506.2±71.0 | 30.6±14.8 | 6.4 | <0.001 |
| Postoperative (day 2) | 508.8±70.9 | 33.2±12.6 | 7.0 | <0.001 |
| Postoperative (day 5) | 488.8±71.1 | 13.2±8.1 | 2.8 | <0.001 |
| Postoperative (day 7) | 476.3±72.9 | 0.7±3.1 | 0.1 | 0.11 (NS) |
*Paired Student’s t-test for intragroup comparison. SD: Standard deviation, NS: Not significant
Table 2 shows changes in the facial measurement in the dexamethasone group. It shows the mean difference in facial measurement on postoperative day 1, day 2, day 5, and day 7. There was highly significant reduction in facial measurement on the postoperative day 2 in dexamethasone. Figure 2 shows mean comparative efficacies of serratiopeptidase and dexamethasone in reducing facial swelling on postoperative day 1, day 2, day 5, and day 7. There was highly significant difference in facial measurement between the serratiopeptidase group and dexamethasone group on postoperative day 2 (mean difference was 62.5 with P < 0.001) and significant difference on postoperative day 1, day 5, and day 7 (P < 0.01).
Table 2.
Facial measurement (mm) of the dexamethasone group
| Time of assessment | Dexamethasone group | P* | ||
|---|---|---|---|---|
| Mean±SD | Difference from preoperative measurement (baseline) | Percentage increase from preoperative measurement (baseline) | ||
| Preoperative (baseline) | 431.6±83.7 | - | - | - |
| Postoperative (day 1) | 451.3±86.5 | 19.7±18.8 | 4.6 | <0.001 |
| Postoperative (day 2) | 446.3±87.4 | 14.7±20.5 | 3.4 | <0.001 |
| Postoperative (day 5) | 437.2±84.7 | 5.6±16.6 | 1.3 | <0.05 |
| Postoperative (day 7) | 430.1±84.4 | 1.5±14.3 | 0.3 | 0.45 (NS) |
*Paired Student’s t-test for intragroup comparison. SD: Standard deviation, NS: Not significant
Figure 2.
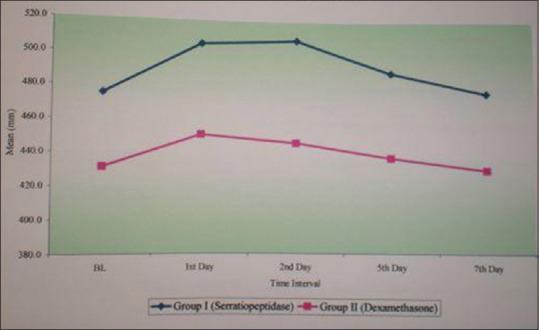
Graph showing the facial measurements
Table 3 shows changes in cheek girth in the serratiopeptidase group. It shows the mean difference in cheek girth on postoperative day 1, day 2, day 5, and day 7. There was a statistically significant reduction in cheek girth on postoperative day 5.
Table 3.
Cheek girth measurement (mm) of the serratiopeptidase group
| Time of assessment | Serratiopeptidase group | P* | ||
|---|---|---|---|---|
| Mean±SD | Difference from preoperative cheek girth (baseline) | Percentage increase from preoperative cheek girth (baseline) | ||
| Preoperative (baseline) | 29.8±4.3 | - | - | - |
| Postoperative (day 1) | 36.2±3.4 | 6.5±3.6 | 21.8 | <0.001 |
| Postoperative (day 2) | 37.4±4.9 | 7.6±3.7 | 25.5 | <0.001 |
| Postoperative (day 5) | 33.2±2.5 | 3.4±3.0 | 11.4 | <0.001 |
| Postoperative (day 7) | 29.7±4.3 | 0.01±0.05 | 0.03 | 0.29 (NS) |
*Paired Student’s t-test. SD: Standard deviation, NS: Not significant
Table 4 shows changes in cheek girth in the dexamethasone group. It shows the mean difference in cheek girth on postoperative day 1, day 2, day 5, and day 7. There was statistically significant reduction in cheek girth on postoperative day 2 and day 5. Figure 3 shows the mean comparative efficacies of dexamethasone and serratiopeptidase in the reduction of cheek girth. There was statistically significant mean difference between the serratiopeptidase group and dexamethasone group on postoperative day 2 (mean difference was 4.3 with P < 0.001).
Table 4.
Cheek girth measurement (mm) of the dexamethasone group
| Time of assessment | Dexamethasone group | P* | ||
|---|---|---|---|---|
| Mean±SD | Difference from preoperative cheek girth (baseline) | Percentage increase from preoperative cheek girth (baseline) | ||
| Preoperative (baseline) | 29.6±4.9 | - | - | - |
| Postoperative (day 1) | 35.1±5.3 | 5.4±1.5 | 18.2 | <0.001 |
| Postoperative (day 2) | 33.1±4.9 | 3.4±1.8 | 11.5 | <0.001 |
| Postoperative (day 5) | 31.6±4.8 | 2.0±1.8 | 6.8 | <0.001 |
| Postoperative (day 7) | 29.7±4.9 | 0.1±0.3 | 0.3 | 0.18 (NS) |
*Paired Student’s t-test. SD: Standard deviation, NS: Not significant
Figure 3.
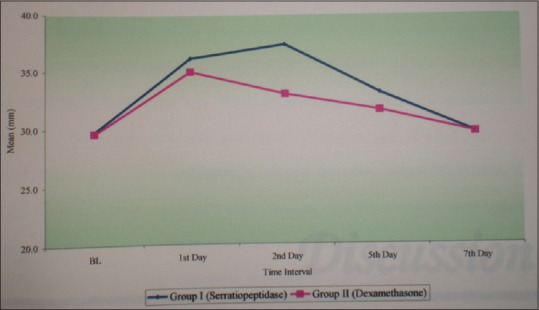
Graph showing cheek girth
DISCUSSION
Most surgical procedures result in a certain amount of postoperative edema. The swelling usually reaches its maximum within 48–72 h, after the surgical procedure. It begins to subside in the late postoperative phase. The operator can control the amount of postsurgical edema by performing surgery in a manner that minimizes the tissue damage. Some believe that ice applied to freshly wounded areas decreases the vascularity and thereby decreases transudation. However, no controlled study has verified this practice.[9]
Glucocorticoids are a group of steroids that possess anti-inflammatory properties. Perhaps, one of the most important actions of corticosteroids is the suppression or prevention of inflammation by interfering with capillary dilatation, edema formation, fibrin deposition, leucocyte migration, and phagocytosis.[10] Mechanism of the action of glucocorticoids are due to its effect on movement suppression and function of leukocytes, accumulation of macrophage at inflammatory site, and prevention of prostaglandin synthesis by inhibiting the arachidonic acid cascade. Lipocortin is an endogenous protein produced by steroids. It blocks the activity of phospholipase A2, thus inhibiting the release of arachidonic acid from cell membranes and the synthesis of prostaglandins, leukotrienes, and thromboxanes.[11]
During the selection of therapeutic regimen for glucocorticosteroid administration, a number of decisions must be made, including the type of steroid, the dosage, the route of administration, and, finally, the timing of the administration, related to the surgical procedure. In selecting the steroid, the major advantage is offered by the synthetic agents in use today and is the ones with longer duration of action and little or no mineralocorticoid activity.[12]
In a study on dexamethasone for reduction of swelling following extraction of the third molar teeth was conducted, and it was concluded that dexamethasone group had more patients with mild swelling and fewer patients with severe swelling.[13] Another study was conducted for establishing the anti-inflammatory effects of dexamethasone. It was concluded that the dexamethasone group had mean swelling volumes significantly lesser than the controls.[3]
A study conducted by Ware et al. used 1 mg dexamethasone by the oral route of administration, 8th hourly for 3 days beginning on the morning of the surgery. Lindberg used 1 mg oral dexamethasone, 8th hourly on the day of surgery and on 1st postoperative day, 1st dose taken, ½ h before the surgery. They reported a significant clinical improvement in postoperative swelling.[14]
Quantitative assessment of swelling represents a major difficulty. Evaluation of facial swelling resulting from surgical procedures has proven to be most problematic. Swelling involves a three-dimensional volumetric change at the tissue and cellular level. Methods used to evaluate swelling include photographic analysis, modified face bow, linear measurement, subjective assessment, and others.[4,15,16,17,18] No technique has been proved to be superior or more accurate in analyzing swelling. The desire to include a large number of patients and the practicality of a low-cost reliable technique made linear measurement a feasible choice. The swelling was also measured in terms of cheek girth, using calibrated slide calipers.
In the present study, the administration of dexamethasone resulted in significantly less degree of swelling on the 2nd postoperative day. There was further reduction of swelling by 7th postoperative day. The facial size reached the preoperative. In the present study, the oral route of drug administration was done. With respect to measurement by 7th-day routes of administration, virtually, all avenues of administration have been used with corticosteroids. However, onset, peak, and duration of action are dependent on the route of administration, the dosage, and the solubility of the agent. With the oral route, corticosteroids are rapidly and almost completely absorbed; hence, this route of administration is as effective as parenteral route. All studies using the oral route of administration reported a clinical reduction in swelling.[12]
In the present study, 1 mg of dexamethasone was given ½ h before the surgery and continued thrice daily for 3 postoperative days. The administration of the preoperative dose of dexamethasone maintains an adequate amount of drug in the blood before, during, and after the surgery, as dexamethasone is a long-acting corticosteroid. Since the appearance of swelling has been around 4–5 h after surgery, preoperative administration of the drug would be very effective in preventing swelling.
Dexamethasone has minimal or zero mineralocorticoid activity and is a long-acting corticosteroid with potent anti-inflammatory action.[12] In this study, dexamethasone was selected as prototype corticosteroid because it is desirable to use a steroid with minimal mineralocorticoid activity and a longer duration of action.
Enzymes are extremely potent substances. The possibility of their therapeutic application is attractive. Enzymes are derived from bacteria (streptokinase and streptodornase), plants (papase and bromelain), and animals (trypsin and chymotrypsin). The enzymes used therapeutically for reduction of edema are hyaluronidase, streptodornase, trypsin, chymotrypsin, alpha-chymotrypsin, and serratiopeptidase.
Various studies have been carried out to determine the efficacy of serratiopeptidase as an anti-inflammatory agent. A prospective study on serratiopeptidase for reduction of postoperative swelling after upper ankle joint surgery was conducted, and it was concluded that significant reduction in swelling was achieved with the use of serratiopeptidase.[19]
Another trial was conducted to investigate the clinical efficacy of the anti-inflammatory enzyme preparation, serratiopeptidase in patients who underwent Caldwell-Luc-antrostomy for chronic empyema and concluded that swelling was smaller in size in the serratiopeptidase treated group than in the placebo-treated group.[20]
Serratiopeptidase was the other drug, which was compared with dexamethasone for its efficacy to control postoperative edema. In the present study, administration of 10 mg of serratiopeptidase, thrice daily for 3 postoperative days resulted in the reduction of swelling on 5th postoperative day. The facial size reached the preoperative facial measurement by 7th postoperative day.
A study was conducted on prednisolone, a corticosteroid and papase, an enzyme as inhibitors of complications after the oral surgery. The conclusion of this study indicated that in comparing prednisolone and papase, prednisolone was more effective in reducing postsurgical sequel of trismus and pain, but no difference was found with regard to edema. This was probably because few moderate-to-severe cases of edema were observed in the first few postoperative days.[15]
In our study, on comparison between serratiopeptidase and dexamethasone, it was found that the swelling was less in the dexamethasone group on postoperative day 1, day 2, and day 5 compared to the serratiopeptidase group on day 1, day 2, and day 5. There was no difference in postoperative swelling on 7th day between dexamethasone and serratiopeptidase group. However, more studies need to be conducted prospectively with a large sample size with more variables comparing it with a control group.
CONCLUSION
Two different classes of drugs, serratiopeptidase, a proteolytic enzyme having anti-inflammatory action, and dexamethasone, a long-acting corticosteroid with minimum or zero mineralocorticoid activity having maximum anti-inflammatory action, were evaluated for its efficacy and compared with each other for its ability to reduce the postoperative swelling.
It appeared in this study that both serratiopeptidase and dexamethasone were effective in the reduction of swelling but in comparison with serratiopeptidase, dexamethasone was more effective in the reduction of swelling.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alexander RE, Throndson RR. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:406–15. doi: 10.1067/moe.2000.109778. [DOI] [PubMed] [Google Scholar]
- 2.Baxendale BR, Vater M, Lavery KM. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia. 1993;48:961–4. doi: 10.1111/j.1365-2044.1993.tb07474.x. [DOI] [PubMed] [Google Scholar]
- 3.Esch PM, Gerngross H, Fabian A. Reduction of postoperative swelling. Objective measurement of swelling of the upper ankle joint in treatment with serrapeptase – A prospective study. Fortschr Med. 1989;107:67. [PubMed] [Google Scholar]
- 4.Beirne OR, Hollander B. The effect of methylprednisolone on pain, trismus, and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol. 1986;61:134–8. doi: 10.1016/0030-4220(86)90173-8. [DOI] [PubMed] [Google Scholar]
- 5.Breytenvach HS. Objective measurement of postoperative swelling. Int J Oral Surg. 1979;7:386. doi: 10.1016/s0300-9785(78)80113-6. [DOI] [PubMed] [Google Scholar]
- 6.Cameron IW. An investigation into some of the factors concerned in the surgical removal of the impacted lower wisdom tooth, including a double blind trial of chymoral. Br J Oral Surg. 1980;18:112–24. doi: 10.1016/0007-117x(80)90027-x. [DOI] [PubMed] [Google Scholar]
- 7.Edilby GI, Gennit SP. A double blind placebo controlled trial on the effect of dexamethasone on post operative swelling. J Dent Res. 1982;62:556. [Google Scholar]
- 8.Caci F, Gluck GM. Double-blind study of prednisolone and papase as inhibitors of complications after oral surgery. J Am Dent Assoc. 1976;93:325–7. doi: 10.14219/jada.archive.1976.0484. [DOI] [PubMed] [Google Scholar]
- 9.ElHag M, Coghlan K, Christmas P, Harvey W, Harris M. The anti-inflammatory effects of dexamethasone and therapeutic ultrasound in oral surgery. Br J Oral Maxillofac Surg. 1985;23:17–23. doi: 10.1016/0266-4356(85)90074-9. [DOI] [PubMed] [Google Scholar]
- 10.Flower RJ, Blackwell GJ. Anti-inflammatory steroids induce biosynthesis of a phospholipase A2 inhibitor which prevents prostaglandin generation. Nature. 1979;278:456–9. doi: 10.1038/278456a0. [DOI] [PubMed] [Google Scholar]
- 11.Gilman AG, Rall TW, Nies AS. The Pharmacological Basis of Therapeutics. New York: Macmillan; 1990. p. 1436. [Google Scholar]
- 12.Holland CS. The development of a method of assessing swelling following third molar surgery. Br J Oral Surg. 1979;17:104–14. doi: 10.1016/s0007-117x(79)80037-2. [DOI] [PubMed] [Google Scholar]
- 13.Linenberg W. The clinical evaluation of dexamethasone in oral surgery. Oral Surg Oral Med Oral Pathol. 1965;20:6. [Google Scholar]
- 14.Milles M, Desjardins PJ, Pawel HE. The facial plethysmograph: A new instrument to measure facial swelling volumetrically. J Oral Maxillofac Surg. 1985;43:346–52. doi: 10.1016/0278-2391(85)90255-1. [DOI] [PubMed] [Google Scholar]
- 15.Montgomery MT, Hogg JP, Roberts DL, Redding SW. The use of glucocorticosteroids to lessen the inflammatory sequelae following third molar surgery. J Oral Maxillofac Surg. 1990;48:179–87. doi: 10.1016/s0278-2391(10)80207-1. [DOI] [PubMed] [Google Scholar]
- 16.Neupert EA, 3rd, Lee JW, Philput CB, Gordon JR. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg. 1992;50:1177–82. doi: 10.1016/0278-2391(92)90149-t. [DOI] [PubMed] [Google Scholar]
- 17.Peterson LJ, Ellis E, 3rd, Hupp JR, Tucker MR. Contemporary Oral and Maxillofacial Surgery. St Louis: Mosby; 2003. p. 47. [Google Scholar]
- 18.Satoskar RS, Bhandarkar SD, Ainapure SS. Pharmacology and Pharmacotherapeutics. Mumbai: Popular Prakashan Private Limited; 2003. pp. 1048–50. [Google Scholar]
- 19.Tachibana M, Mizukoshi O, Harada Y, Kawamoto K, Nakai Y. A multi-centre, double-blind study of serrapeptase versus placebo in post-antrotomy buccal swelling. Pharmatherapeutica. 1984;3:526–30. [PubMed] [Google Scholar]
- 20.Tripathi KD. Essentials of Medical Pharmacology. New Delhi: Jaypee Brothers Medical Publishers (p) Ltd; 2003. p. 261. [Google Scholar]


