Abstract
Aim:
To demonstrate the efficacy of a new novel anterior tonsillar fossa approach in management of elongated styloid process syndrome.
Material and Method:
We operated upon 20 patients with confirmed, symptomatic elongated styloid process. None of these patients gave a previous positive history of trauma or any other procedure relating to tonsillar area. All these patients had undergone treatment or were under treatment for neuralgia/TMJ dysfunction syndrome. Diagnosis was confirmed by clinical examination followed by radiological findings.
Results:
12 patients underwent bilateral styloidectomy (60%) and 8 patients, underwent unilateral styloidectomy (40%). The length of stolid process ranged from 34mm to 62mm (mean 44 mm). Post operative follow up period ranges from 6 months to 12 months.17 patients (85%) were asymptomatic & had complete remission of symptoms over a follow up period of 12 months. 2 patients had partial remission of symptoms & 1 patient was lost to follow-up.
Conclusion:
Our anterior tonsillar fossa approach to elongated styloid is safe & adequate in effective surgical management & more so with an additional advantage of not requiring tonsillectomy which is often performed in trans-pharyngeal technique.
Keywords: Dysphagia, Eagles syndrome, elongated styloid process, stylalgia, temporomandibular joint dysfunction syndrome
INTRODUCTION
Patients reporting with pharyngodynia and neck pain symptoms can lead to an extensive differential diagnosis.[1] The close proximity of the styloid process to many of the vital neurovascular structures in the neck makes it clinically significant; abnormal elongation of the styloid process may cause compression on a number of vessels and nerves with whom it shares close proximity often producing confusing signs and symptoms.[2] This elongation was first described in 1652 by an Italian surgeon Pietro Marchetti, who attributed it to an ossifying process of the stylohyoid ligament.[3] In 1937, Eagle, an otolaryngologist at Duke University, coined the term “stylalgia” to describe the pain associated with this abnormality.[4,5,6] Eagle postulated that there are two types of syndromes, which finally came to bear his name.[7]
Classic type
The classic type is characterized by pain secondary to stimulation of cranial nerves V, VII, IX, and X and is often seen following tonsillectomy.
Carotid artery type
Styloid process gets involved with carotid nerve plexuses causing foreign-body sensation in the pharynx and neck pain on rotation of the head.
There are three syndromes closely associated with styloid process syndrome: Costen's syndrome, Trotter's syndrome, and myofacial pain syndrome.[8] Weinlechner described the first surgical case in 1872.[9]
In this article of case series, we would like to demonstrate the successful management of elongated styloid process through a new novel intraoral surgical approach, which we would like to call as the anterior tonsillar fossa approach to elongated styloid.
Anatomical correlation and topographic characteristics of the styloid process
The name styloid is derived from the Greek word “Stylos” meaning a pillar. The styloid process is a thin, cylindrical, sharp osseous projection arising from the posterior lower surface of petrosal bone, just anterior to the stylomastoid foramen.[10] The process develops from the second branchial arch specifically from Reichert cartilage.[11] Reichert's cartilage is made up of four portions [Figures 1 and 2]:
Figure 1.
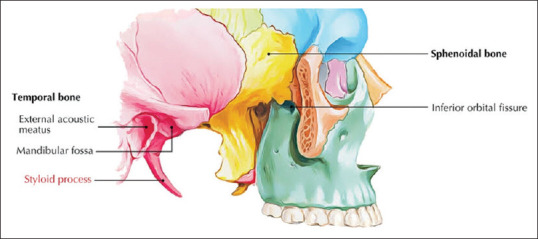
Topographic anatomy
Figure 2.
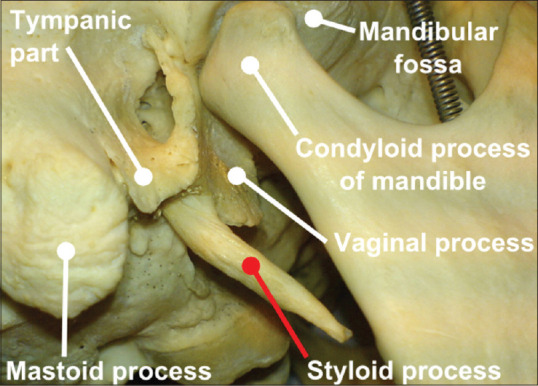
Topographic anatomy
The upper portion develops into the styloid process
The central portion forms stylohyoid ligament
Lower portion – lesser cornu of the hyoid bone
Basic portion – hyoid bone.
Its muscular attachments [Figures 3 and 4] include the stylohyoid, styloglossus, and stylopharyngeus. Together, they form the so-called “Riolano's Bouchet” as well as the stylohyoid and stylomandibular ligaments defined as Bouchets's white flower.[12]
Figure 3.
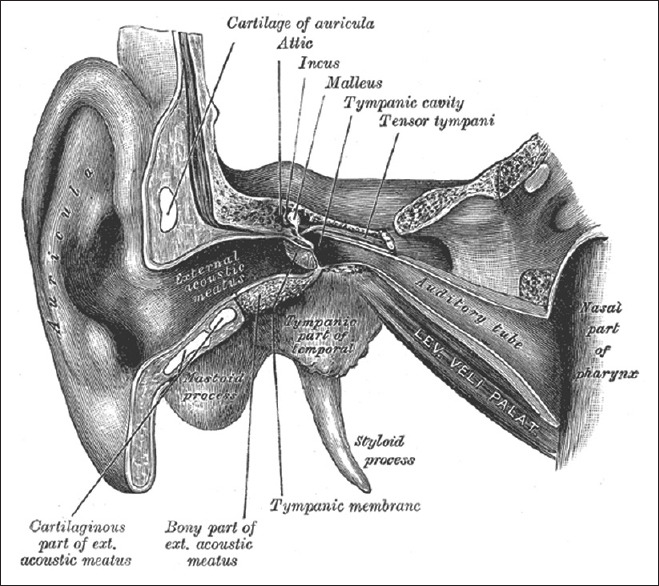
Muscular attachments
Figure 4.
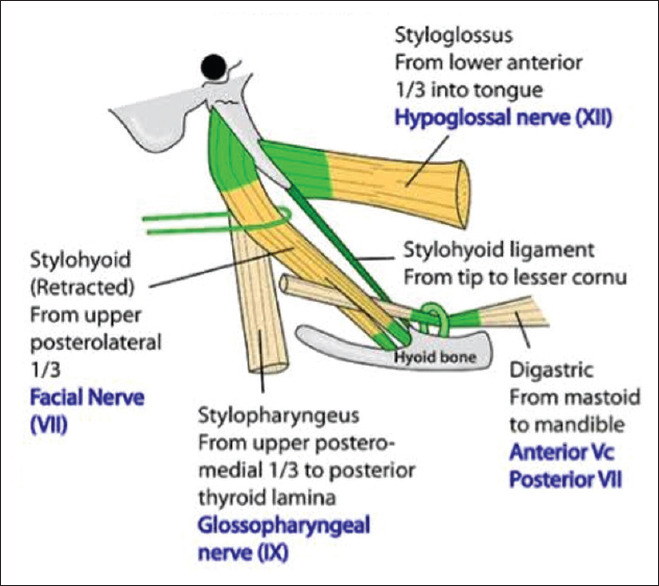
Muscular attachments
Stylohyoid connects the base of the styloid to hyoid bone near its greater horn and is innervated by the XII cranial nerve. The styloglossus arises from the anterior and lateral surface of the styloid process and descends forward between the internal and external carotid arteries and divides on the lateral side of the tongue to blend with the fibers of inferior linguae muscle and obliquely with the hyoglossus muscle and it is innervated by VII nerve. The stylopharyngeus traverses from the medial aspect of the styloid process to the lateral wall of the pharynx and is innervated by the IX nerve. The stylohyoid ligament connects the apex of the styloid and lesser horn of the hyoid bone, and the stylomandibular ligament extends from the styloid process to the parotid-masseteric fascia between the mandible and mastoid process.[3] Other structures relevant to the operative process include external and internal carotid arteries, internal jugular vein, VII, IX, X, XI, and XII cranial nerves.[3,12]
Studies have shown that normal average length of the styloid process is <3 cm, with a range of 1.52–4.77 cm.[3]
According to Motta et al. (1987): 1.52–4.77 cm[12]
Kaufman et al. (1978): <3 cm[13]
Lindeman (1985): 2–3 cm[14]
Less than 2.5 cm according to Correll et al. (1979), Langlais et al., and Montalbetti et al.[15,16]
Less than 4 cm according to Mansour and Young[17]
According to Balcioglu et al., the mean length of the styloid process among participants reporting with Eagle's syndrome is between 40 ± 4.72 mm[18]
Massey reported only 11 of 2000 cranial dissections detected a styloid process longer than 4 cm[19]
Härmä reported the incidence of elongated styloid is 4%–7%[20]
Murtagh et al. reported 4%–10.3% of patients experience pain with an elongated styloid process.[21]
However, it is found that the length of the styloid process does not correlate with the severity of pain, despite this, the literature still categorizes the patients into those with pain pattern following carotid artery distribution and those with a palpable (classical) mass in the tonsillar area.[22]
MATERIALS AND METHODS
Twenty patients were operated for the elongated styloid process
None of the patients gave any positive history of trauma or any other procedure relating to tonsillar area
All these patients had undergone or were under treatment for neuralgia/TMD for a period ranging from 3 to 5 years, with no resolution in symptoms Table 1
Our diagnosis of elongated styloid process was purely based on the history, clinical examination, and confirmatory radiological finding and CT findings [Figures 5–7]
In our series, 12 patients underwent bilateral styloidectomy, and 8 patients underwent unilateral styloidectomy.
Table 1.
Distribution of gender, age, chief symptoms, and remission status
| Patient | Gender | Age (years) | Chief symptoms | Results |
|---|---|---|---|---|
| 1 | Male | 37 | Dysphagia and foreign-body sensation | Complete remission |
| 2 | Male | 36 | Throat pain and otalgia | Complete remission |
| 3 | Male | 48 | Foreign-body sensation and pain on head rotation | Complete remission |
| 4 | Male | 24 | Dysphagia and persistent throat pain | Complete remission. Lost to follow-up after 6 months |
| 5 | Female | 35 | Dysphagia and throat pain | Partial remission |
| 6 | Female | 38 | Dysphagia and throat pain | Complete remission |
| 7 | Male | 36 | Dysphagia and throat pain | Complete remission |
| 8 | Male | 21 | Dysphagia and throat pain | Lost to follow-up |
| 9 | Male | 40 | Dysphagia and throat pain | Complete remission |
| 10 | Male | 50 | Dysphagia and throat pain | Complete remission |
| 11 | Female | 40 | Dysphagia and throat pain | Complete remission |
| 12 | Female | 40 | Dysphagia and throat pain | Complete remission |
| 13 | Male | 43 | Dysphagia and throat pain | Complete remission |
| 14 | Male | 62 | Dysphagia and throat pain | Complete remission |
| 15 | Male | 50 | Dysphagia and throat pain | Complete remission |
| 16 | Male | 38 | Dysphagia and throat pain | Complete remission |
| 17 | Male | 44 | Dysphagia and throat pain | Partial remission |
| 18 | Female | 48 | Dysphagia and throat pain | Complete remission |
| 19 | Female | 42 | Dysphagia and throat pain | Complete remission |
| 20 | Male | 44 | Dysphagia and throat pain | Complete remission |
Figure 5.

Intraoral clinical examination
Figure 7.
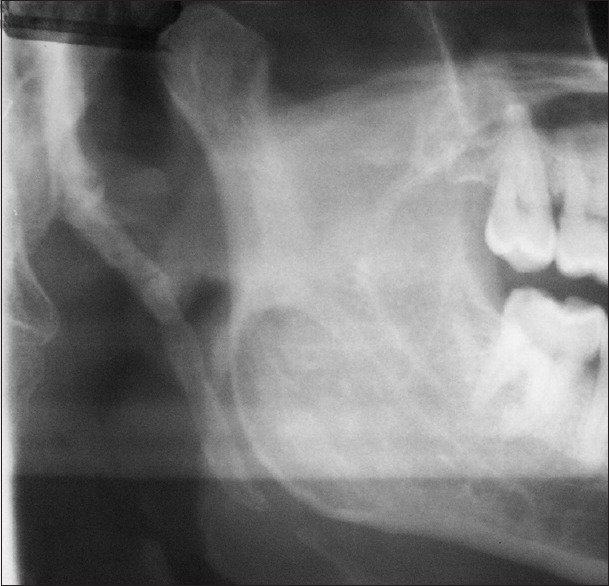
Radiological diagnosis: Lateral oblique
Figure 6.

Radiological diagnosis – OPG
RESULTS
In our series, 12 patients underwent bilateral styloidectomy (60%) and 8 patients, underwent unilateral styloidectomy (40%). The average length of stolid process ranged from 34 mm to 62 mm (mean 44 mm). Post operative follow up period ranges from 6 months to 12 months. 17 patients (85%) were asymptomatic and had complete remission of symptoms over a follow up period of 12 months. 2 patients had partial remission of symptoms and 1 patient was lost to follow-up.
Surgical anatomy
Palatine tonsil represents the largest collection of the lymphoid tissue in Waldeyer's lymphatic ring. Its capsule is regarded as a specialized portion of pharyngobasilar fascia, and its free surface is covered with the mucosa.[23] The triangular fold is a layer of mucosa and connective tissue that lies just behind the palatoglossal arch and is separated from the medial surface of the tonsil by the anterior tonsillar fossa.[24,25] In 40% of persons, there is a semilunar fold and a supratonsillar fossa at the upper pole of tonsil, at its deep surface, tonsil is held in place by fibers of the palatopharyngeus muscle that have been apparently termed as triangular ligament or retrotonsillar or transverse plica.[26] The large part of tonsillar bed is formed by the fibers of superior constrictor, and a variable posterior portion is formed by the fibers of palatopharyngeus muscle.[27] The muscular wall is thin and immediately against it on the outer wall of the pharynx is the glossopharyngeal nerve. Its other anatomical relations include stylopharyngeus and styloglossus muscle, stylohyoid ligament, styloid process, internal and external carotid arteries, and glossopharyngeal nerve. The five arteries supply the tonsil.[23,24]
Tonsillar artery from facial
Ascending pharyngeal from external carotid
Ascending palatine from facial
Descending palatine from the maxillary artery
Lingual artery and dorsal linguae.
The venous supply is from peritonsillar plexuses. Nerve supply is from the tonsillar branch of the maxillary nerve and glossopharyngeal nerve. Tonsils do not possess afferent lymphatics and efferent lymphatics drain directly into jugulodigastric nodes and upper deep cervical nodes and indirectly through retropharyngeal nodes [Figures 8 and 9].
Figure 8.
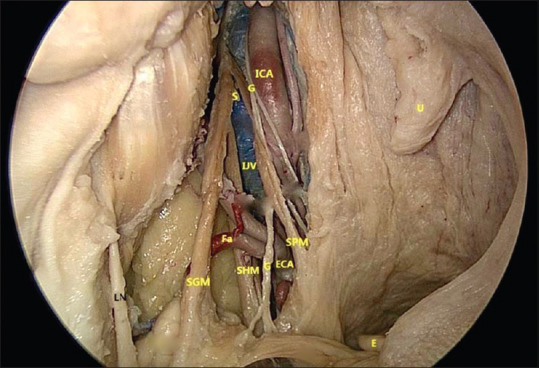
Surgical anatomy S-Styloid process. ICA: Internal carotid artery, G: Glossopharyngeal nerve, IJV: Internal jugular vein, ECA: External carotid artery, FA: Facial artery, SGM: Styloglossus muscle, SPM: Stylopharyngeus, SHM: Stylohyoid muscle E: Epiglottis, U: Uvalae
Figure 9.
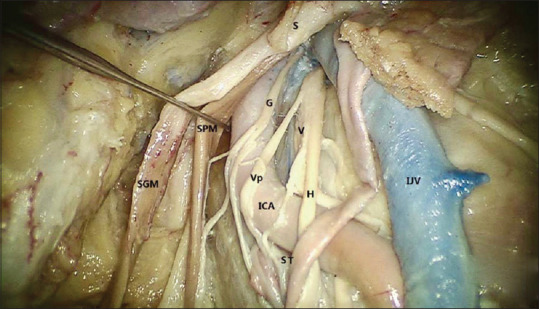
Surgical anatomy: Surgical anatomy S-Styloid process. ICA: Internal carotid artery, G: Glossopharyngeal nerve, IJV: Internal jugular vein, ECA: External carotid artery, H: Hypoglossal nerve, V: Vagus, SGM: Styloglossus muscle, SPM: Stylopharyngeus, ST: Sympathetic trunk, VP: Pharyngeal branch of the vagus
Surgical procedure
Under nasotracheal intubation, the patient is put on tonsillectomy position with Boyle Davis gag in place with the tongue blade being suspended depending on the height required on Draffin's bipod which is secured on McGauran's plate. Infiltration with 2% local anesthetic with adrenaline is given just medial to palatoglossal fold and anterior tonsillar space. A triangular fold is retracted by double-ended Freer's elevator, and a 0.5–1 cm submucosal incision is made in anterior tonsillar fossa; blunt dissection is carried through the loose areolar tissue which also contains paratonsillar vein which is lateralized. Dissection proceeds through the fascia to superior constrictor, which forms the bed of the tonsil. Once the bed is pierced and opened, care is taken not to damage the glossopharyngeal nerve, styloid process is identified through digital palpation, and dissection is carried around it exposing the tip. The tip of the styloid is engaged on a styloid ring (our modification of the sphenoid curette) once the elongated styloid tip is secure within the ring and sharp dissection is done over the styloid stripping it of its attachments. Using a kerrison punch, sufficient length of the elongated process is osteotomised and retrieved with a curved Kocher. Local hemostasis achieved and wound closed in layers [Figures 10–12].
Figure 10.
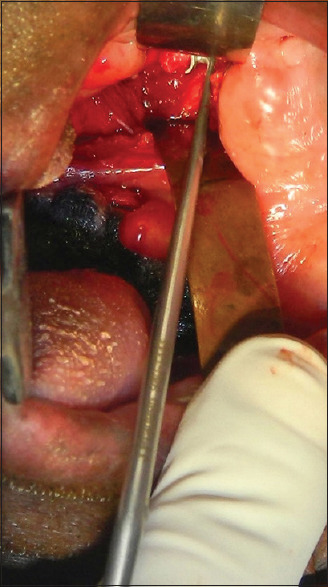
Intraoperative: Styloid tip secured on a styloid ring
Figure 12.
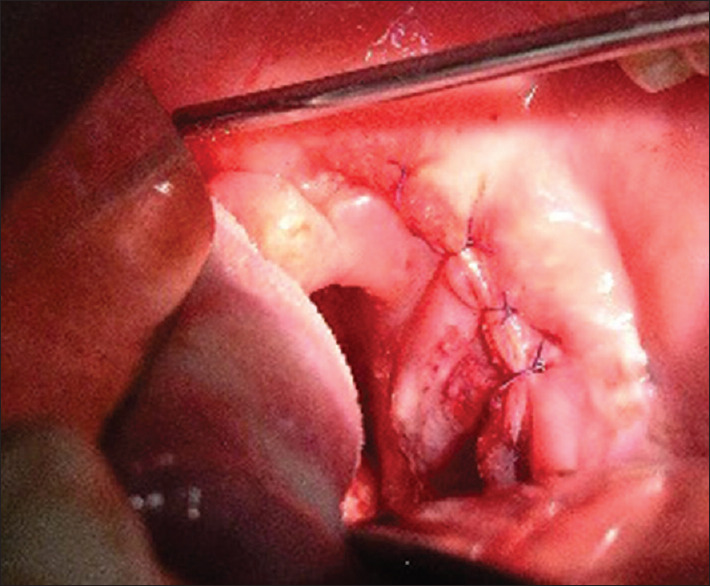
Final closure
Figure 11.

Resected specimen
DISCUSSION
Patients with vague head and neck pain symptoms can lead to an extensive differential diagnosis. A specific orofacial pain secondary to calcification of stylohyoid ligament or elongated styloid process has been known as Eagle's syndrome.[4] Elongated styloid or stylohyoid syndrome is the symptomatic elongation of styloid process or mineralization of the sylohyoid ligament complex.[17] Over a 20-year period, Eagle reported over 200 cases and explained that the normal styloid process is approximately 2.5–3.0 cm in length. Slight medial deviation of the styloid process could result in severe symptoms of atypical facial pain.[4] However, the mere presence of elongated styloid process or mineralization of the stylohyoid complex radiographically in the presence of pharyngeal pain does not automatically confirm a diagnosis of elongated styloid. Three reasons can be attributed to this as follows:
Many patients with an ossified stylohyoid complex are asymptomatic
There is no correlation between the severity of pain and extent of ossification of the stylohyoid complex
Majority of symptomatic patients have had no recent history of tonsillectomy or cervicopharyngeal trauma.[22]
The incidence of this syndrome varies between the populations.
Eagle[4,5] found a long styloid process in 4% of the participants he examined, whereas Kaufman et al. (1970)[13] found the incidence of 7%. In a review of 1771 panoramic radiographs, the incidence of mineralization of the styloid chain was found to be 18%–20%.[28] The incidence of elongated styloid was estimated at 33%, of which 55% of bilateral cases with a male-to-female ratio of 1/9. The average age was 43.35 ± 14.88 years, with no significant difference in the age of patients according to gender.[18] Despite these figures, only 1%–5% of patients are symptomatic.[15,29] Literature does not support the sexual dimorphism of elongated styloid. Wolrey stated that eagles syndrome occurs more frequently in women, while others do not support this theory.[30] The characteristic symptomatology is varied, with patients often complaining of pain in pharynx, foreign-body sensation, and pain on swallowing. The dull nagging pain of elongated styloid that becomes worse during the deglutition can be reproduced by palpation of the tonsillar fossa.[31] The duration of symptoms, in our case series, ranged from 8 months to 37 months with no significant sex predilection. The exact etiology is still being debated with Eagle[4,5] considering local trauma. Gli Aspetti[32] proposed the persistence of mesenchymal elements undergoing osseous metaplasia due to trauma or mechanical stress. Epifanio[33] suggested ossification related to endocrine disorders, which is more common in postmenopausal women. Gokce et al.[34] reported ectopic calcifications might have a role in elongation, especially in patients with abnormal calcium, phosphorous, and Vitamin D metabolism. Steinmann[35] proposed the following three theories to explain ossification:
Theory of reactive hyperplasia
Theory of reactive metaplasia
Theory of anatomic variance.
The pathophysiological mechanism for pain associated with elongated styloid is as follows:[36]
Compression of the neural elements, glossopharyngeal nerve, and branches of the trigeminal nerve or chorda tympani
Fracture of the ossified stylohyoid ligament, followed by the proliferation of granulation tissue that causes pressure on surrounding structures and resultant pain
Impingement on the carotid vessels by the styloid process, producing irritation of sympathetic nerves in the arterial sheath
Degenerative and inflammatory changes in the tendinous portion of the stylohyoid insertion, a condition called insertion tendinosis
Irritation of pharyngeal mucosa by direct compression by the styloid process
Stretching and fibrosis involving the fifth, seventh, ninth, and tenth cranial nerves in the posttonsillectomy period.
The diagnosis of elongated styloid must be based on sound clinical and radiological examination [Figure 13]. It is possible to feel an elongated styloid process by careful intraoral palpation in the tonsillar area.[16] Injection of local anesthetic relieves the pain and can be used as a diagnostic tool,[37] although a variety of head and neck conditions must, however, be considered in the differential diagnosis before concluding Eagle's syndrome and cervicopharyngeal pain. The clinical diagnosis should be confirmed and supported by imaging; several methods are available and vary in complexity, but CT is without doubt the best and most accurate and reliable.[21] The radiographic classification system includes three types of radiographic appearances:[15]
Figure 13.
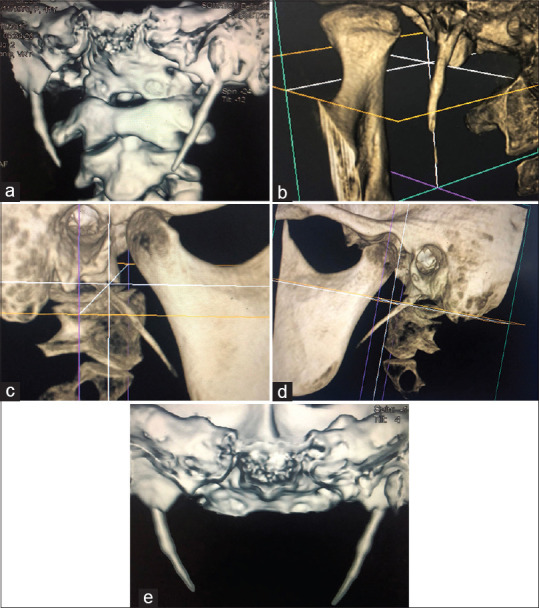
(a-e) Three-dimensional computed tomography images of the elongated styloid process
Type I: Uninterrupted, elongated styloid process
Type II: Styloid process apparently being joined to the stylohyoid ligament by a single pseudoarticulation
Type III: It consists of interrupted segments of the mineralized ligament creating the appearance of pseudoarticulation within the ligament.
In differential diagnosis, we need to consider several of these conditions,[20] including laryngopharyngeal dysesthesia, dental malocclusion, sphenopalatine ganglia neuralgia, trigeminal neuralgia, glossopharyngeal neuralgia, temporomandibular joint arthritis, chronic tonsillopharyngitis, hyoid bursitis, Sluder's syndrome, histamine cephalgia, cluster headache, esophageal diverticula, temporal arteritis, cervico vertebral arthritis, and benign or malignant pathologies.
The elongated styloid process can be treated either conservatively or surgically. Conservative management may include:
Transpharyngeal injection of steroids and lidocaine
Nonsteroidal anti-inflammatory drug
Local heat application
Traditional Chinese medicine
Transpharyngeal manipulation and fracturing of the styloid process.
The most satisfactory and effective treatment is surgical shortening either through an intraoral or external approach depending on the choice of surgeon, with each having its own advantages and disadvantages.[38,39,40,41,42]
In our experience involving 20 patients and 32 styloidectomies, we chose to operate through a new intraoral approach without performing tonsillectomy, which is the standard procedure in transpharyngeal approach to elongated styloid. Through this new approach, we were able to achieve good surgical exposure and adequate length reduction with no intraoperative hiccups. Postoperative recovery in all 20 patients was good and uneventful. During the 1-year follow-up period, patients were symptom-free and did not require any further medical or surgical intervention.
CONCLUSION
Elongated styloid process syndrome can be diagnosed by a detailed history, physical examination, and radiological investigation. It can often be confused or mistaken for conditions that must be excluded before reaching a confirmatory diagnosis. In our series, we could achieve favorable results through this new intraoral approach without performing tonsillectomy. Although surgical failures in both extraoral and intraoral techniques have been reported in the literature despite the removal of adequate length, we believe that these could be attributed to intraoperative injury, fibrous entrapment, and inadequate shortening assuming that the diagnosis was correct in the first place. Although the choice of surgical approach is purely based on surgeons comfort level and expertise, we through our experience believe and propose that this new intraoral technique is safe and adequate in effective surgical management more so with an additional advantage of not requiring tonsillectomy, which is often performed in transpharyngeal technique.
Based on anatomical relations/correlations and landmarks, we would like to call this approach as “Anterior tonsillar fossa approach to elongated styloid.”
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Mendelsohn AH, Berke GS, Chhetri DK. Heterogeneity in the clinical presentation of Eagle's syndrome. Otolaryngol Head Neck Surg. 2006;134:389–93. doi: 10.1016/j.otohns.2005.10.046. [DOI] [PubMed] [Google Scholar]
- 2.Prabhu LV, Kumar A, Nayak SR, Pai MM, Vadgaonkar R, Krishnamurthy A, et al. An unusually lengthy styloid process. Singapore Med J. 2007;48:e34–6. [PubMed] [Google Scholar]
- 3.Fini G, Gasparini G, Filippini F, Becelli R, Marcotullio D. The long styloid process syndrome or Eagle's syndrome. J Cranio Maxillofac Surg. 2000;28:123–7. doi: 10.1054/jcms.2000.0128. [DOI] [PubMed] [Google Scholar]
- 4.Eagle WW. Elongated styloid process. Report of two cases. Arch Otolaryngol. 1937;25:584–7. doi: 10.1001/archotol.1949.03760110046003. [DOI] [PubMed] [Google Scholar]
- 5.Eagle WW. Elongated styloid process; further observations and a new syndrome. Arch Otolaryngol. 1948;47:630–40. doi: 10.1001/archotol.1948.00690030654006. [DOI] [PubMed] [Google Scholar]
- 6.Eagle WW. Symptomatic elongated styloid process; report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol. 1949;49:490–503. doi: 10.1001/archotol.1949.03760110046003. [DOI] [PubMed] [Google Scholar]
- 7.Politi M, Toro C, Tenan G. A rare case of cervical pain: Eagle's syndrome. Int J Dent. 2009;2009:781297. doi: 10.1155/2009/781297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandev S, Sokler K. Styloid process syndrome. Acta Stomatol Croat. 2000;34:451–4. [Google Scholar]
- 9.Kelvin MM. Elongated styloid process: Their formation & clinical significance. Laryngoscope. 1930;40:907–9. [Google Scholar]
- 10.Magotra R, Razdan S. Elongated styloid process: Anatomical variations. Horiz JK Sci. 2008;10:203–5. [Google Scholar]
- 11.Fini G, Gasparini G, Filippini F, Beculli R, Marcotullio D. The long styloid process syndrome or Eagle's syndrome. J Maxillofac Surg. 2000;28:123–7. doi: 10.1054/jcms.2000.0128. [DOI] [PubMed] [Google Scholar]
- 12.Motta P, Randa T, Marrinozzi G. Anatomia umana. Edi Ermes Milano. 1987;11:209–16. [Google Scholar]
- 13.Kaufman SM, Elzay RP, Irish E. Styloid process variations: Radiologic & clinical study. Arch Otolaryngol. 1978;91:460–63. doi: 10.1001/archotol.1970.00770040654013. [DOI] [PubMed] [Google Scholar]
- 14.Lindeman P. The elongated styloid process as a cause of throat discomfort. Four case reports. J Laryngol Otol. 1985;99:505–8. doi: 10.1017/s0022215100097139. [DOI] [PubMed] [Google Scholar]
- 15.Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized stylohyoid ligament complex: A proposed classification and report of a case of Eagle's syndrome. Oral Surg Oral Med Oral Pathol. 1986;61:527–32. doi: 10.1016/0030-4220(86)90400-7. [DOI] [PubMed] [Google Scholar]
- 16.Montalbetti L, Ferrandi D, Pergami P, Savoldi F. Elongated styloid process and Eagle's syndrome. Cephalalgia. 1995;15:80–93. doi: 10.1046/j.1468-2982.1995.015002080.x. [DOI] [PubMed] [Google Scholar]
- 17.Monsour PA, Young WG. Variability of the styloid process and stylohyoid ligament in panoramic radiographs. Oral Surg Oral Med Oral Pathol. 1986;61:522–6. doi: 10.1016/0030-4220(86)90399-3. [DOI] [PubMed] [Google Scholar]
- 18.Balcioglu HA, Kilic C, Akyol M, Ozan H, Kokten G. Length of the styloid process and anatomical implications for Eagle's syndrome. Folia Morphol (Warsz) 2009;68:265–70. [PubMed] [Google Scholar]
- 19.Massey EW. Facial pain from an elongated styloid process (Eagle's syndrome) South Med J. 1978;71:1156–9. doi: 10.1097/00007611-197809000-00030. [DOI] [PubMed] [Google Scholar]
- 20.Härmä R. Stylalgia: Clinical experiences of 52 cases. Acta Otolaryngol. 1966;(Suppl 224):149. doi: 10.3109/00016486709123570. [DOI] [PubMed] [Google Scholar]
- 21.Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol. 2001;22:1401–2. [PMC free article] [PubMed] [Google Scholar]
- 22.Camarda AJ, Deschamps C, Forest D. I. Stylohyoid chain ossification: A discussion of etiology. Oral Surg Oral Med Oral Pathol. 1989;67:508–14. doi: 10.1016/0030-4220(89)90264-8. [DOI] [PubMed] [Google Scholar]
- 23.Kenna MA, Amin A. Anatomy & physiology of oral cavity. In: Snow JB, Wackym PA, editors. Ballenger's Otorhinolaryngology Head & Neck Surgery. 17th ed. Shelton: BC Decker Inc; 2009. pp. 769–74. [Google Scholar]
- 24.Susan S, Harold E, Jermiah CH, David J, Andrew W. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 39th ed. 35. Philadelphia: Elsevier; 2005. Pharynx; pp. 619–31. [Google Scholar]
- 25.Beasley BB. Anatomy of pharynx & oesophagus. In: Kerr AG, Gleeson M, editors. Scott-Browns Otorhinolaryngology. 6th ed. India: Butterworth-Hinemann Publications; 1997. [Google Scholar]
- 26.Wiatrak BJ, Woolley AL. Anatomy of pharynx & oesophagus. In: Cummings CW, Fredrikson JM, Harker LA, Crause CJ, Schuller DE, Richardson MA, editors. Otolaryngology Head & Neck Surgery. 3rd ed. London: Mosby; 1998. pp. 188–215. [Google Scholar]
- 27.William JL, Lawrence SS, Steven P, William JS. Human Embryology. 3rd ed. Philadelphia: Elsevier; 2001. pp. 375–6. [Google Scholar]
- 28.Correll RW, Jensen JL, Taylor JB, Rhyne RR. Mineralization of the stylohyoid-stylomandibular ligament complex. A radiographic incidence study. Oral Surg Oral Med Oral Pathol. 1979;48:286–91. doi: 10.1016/0030-4220(79)90025-2. [DOI] [PubMed] [Google Scholar]
- 29.Fini G, Gasparini G, Filippini F, Becelli R, Marcotullio D. The long styloid process syndrome or Eagle's syndrome. J Craniomaxillofac Surg. 2000;28:123–7. doi: 10.1054/jcms.2000.0128. [DOI] [PubMed] [Google Scholar]
- 30.Woolery WA. The diagnostic challenge of styloid elongation (Eagle's syndrome) J Am Osteopath Assoc. 1990;90:88–9. [PubMed] [Google Scholar]
- 31.Pierrakou ED. Eagle's syndrome. Review of the literature and a case report. Ann Dent. 1990;49:30–3. [PubMed] [Google Scholar]
- 32.Gli Aspetti LA. Clinici e radiologici delle anomalie dell' apparato stilo-joideo. Radiol Med. 1975;61:337–640. [Google Scholar]
- 33.Epifanio G. Processi stiloidea lunghi e ossificazione della catena stiloidea. Rad Prat. 1962;12:127–32. [Google Scholar]
- 34.Gokce C, Sisman Y, Sipahioglu M. Styloid process elongation or Eagle's syndrome: Is there any role for ectopic calcification? Eur J Dent. 2008;2:224–8. [PMC free article] [PubMed] [Google Scholar]
- 35.Steinmann EP. A new light on the pathogenesis of the styloid syndrome. Arch Otolaryngol. 1970;91:171–4. doi: 10.1001/archotol.1970.00770040241013. [DOI] [PubMed] [Google Scholar]
- 36.Ceylan A, Köybaşioǧlu A, Celenk F, Yilmaz O, Uslu S. Surgical treatment of elongated styloid process: Experience of 61 cases. Skull Base. 2008;18:289–95. doi: 10.1055/s-0028-1086057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prasad KC, Kamath MP, Reddy KJ, Raju K, Agarwal S. Elongated styloid process (Eagle's syndrome): A clinical study. J Oral Maxillofac Surg. 2002;60:171–5. doi: 10.1053/joms.2002.29814. [DOI] [PubMed] [Google Scholar]
- 38.Boedts D. Styloid process syndrome or stylohyoid syndrome? Acta Otorhinolaryngol Belg. 1978;32:273–8. [PubMed] [Google Scholar]
- 39.Zhang YL, Liao DM, Wei YG, Bai GR. Styloid process syndrome: Length and palpation of the styloid process. Chin Med J (Engl) 1987;100:56–7. [PubMed] [Google Scholar]
- 40.Chase DC, Zarmen A, Bigelow WC, McCoy JM. Eagle's syndrome: A comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986;62:625–9. doi: 10.1016/0030-4220(86)90253-7. [DOI] [PubMed] [Google Scholar]
- 41.Beder E, Ozgursoy OB, Karatayli Ozgursoy S. Current diagnosis and transoral surgical treatment of Eagle's syndrome. J Oral Maxillofac Surg. 2005;63:1742–5. doi: 10.1016/j.joms.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 42.Chrcanovic BR, Custódio AL, de Oliveira DR. An intraoral surgical approach to the styloid process in Eagle's syndrome. Oral Maxillofac Surg. 2009;13:145–51. doi: 10.1007/s10006-009-0164-6. [DOI] [PubMed] [Google Scholar]


