Supplemental Digital Content is available in the text.
Keywords: COVID-19, pandemic, South Carolina, stroke, thrombolysis
Background and Purpose:
The impact of the coronavirus disease 2019 (COVID-19) pandemic on stroke systems has not been systematically evaluated. Our study aims to investigate trends in telestroke consults during the pandemic.
Methods:
We did retrospective chart review of consecutive patients seen through a telestroke network in South Carolina from March 2019 to April 2020. We dichotomized patients to preCOVID-19 pandemic (March 2019 to February 2020) and during COVID-19 pandemic (March to April 2020).
Results:
A total of 5852 patients were evaluated during the study period, 613 (10.5%) were seen during the pandemic. The median number of weekly consults dropped from 112 to 77 during the pandemic, P=0.002. There was no difference in baseline features; however, Black patients were less likely to present with strokes during the pandemic (13.9% versus 29%, P≤0.002).
Conclusions:
The COVID-19 pandemic has led to a significant drop in telestroke volume. The impact seems to disproportionately affect Black patients.
The novel coronavirus disease 2019 (COVID-19) has rapidly spread since initial report in December 2019 to involve >200 countries, with over 300 000 deaths worldwide.1 While the hallmark of COVID-19 is respiratory insufficiency, up to 36% of patients with COVID-19 have neurological manifestations and ≈6% present with cerebrovascular diseases.2 Despite concern for increased risk of stroke, many centers reported a significant decline in number of patients presenting with strokes during the pandemic.3–5 This alarming drop raised concern that patients with stroke may be reluctant to seek medical care in the setting of the pandemic.6 Such abundance of caution has the potential to cause overall worse outcomes for those not presenting to a hospital for their health concerns, especially in acute stroke.7,8 Furthermore, recent studies have suggested a stronger impact of COVID-19 in Black patients, with 3-fold incidence in predominantly Black counties, and mortality rates rising to up to almost 6× those of White patients in some inner cities.9,10 With the higher risk seen in Black patients, concern arises that this fear of seeking care for acute medical problems, such as stroke, may disproportionately affect Black patients.
The Medical University of South Carolina is the hub for a large video-based telestroke network covering >38 hospitals throughout South Carolina.11 We sought to evaluate change in the volume of telestroke consults during COVID-19 pandemic. In addition, we sought to assess for racial disparities created by the pandemic.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request. We performed a retrospective review of the prospectively maintained telestroke registry at Medical University of South Carolina between March 2019 and April 2020. In this analysis, we included 27 centers that were in the telestroke network for the study duration. Collected data included baseline demographics, time from symptom-onset to presentation, baseline National Institutes of Health Stroke Scale, tPA (tissue-type plasminogen activator) administration, mechanical thrombectomy, door to needle time, and door in door out for transferred patients. Discharge outcomes included in-hospital mortality, National Institutes of Health Stroke Scale on discharge, and modified Rankin Scale on discharge. Patients were grouped by month during which consult occurred and then further grouped into those occurring before COVID-19 pandemic (March 1, 2019 to February 29, 2020) and during the pandemic (March 1, 2020 to April 30, 2020). Descriptive statistics were done using Mann-Whitney U test for continuous variables, and χ2 (or Fisher exact test for cells <5) for categorical variables. Alpha-level was set to 0.05 for significance, and all reported P values are 2-sided. Data analysis was done using SPSS version 25 (IBM, IL). Authors confirm that the study is an observational minimal risk study, and no consent is required per our institutional policy. Our study was approved by the institutional review board at our institution.
Results
Total of 5852 patients were evaluated in the telestroke network during the study period, of those, 5239 (89.5%) during the year preceeding the pandemic. The weekly number of patients presenting with stroke was lower during the pandemic (77 [interquartile range [IQR], 69–84] versus 112 [IQR, 102–120] before the pandemic, P=0.002) (Figure 1). Figure I in the Data Supplement shows the number of patients with stroke presenting directly to the thrombectomy-capable stroke center during the same time period. In addition, there was lower percentage of Black patients presenting during the pandemic (13.9% versus 29% before, P<0.001).
Figure 1.
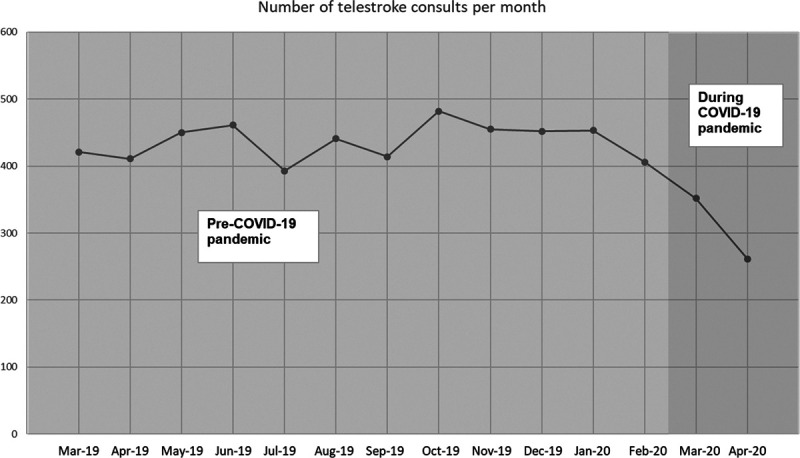
The number of monthly telestroke consults during study period. COVID-19 indicates coronavirus disease 2019.
The Table summarizes baseline characteristics and outcomes of patients in both groups. There was a higher percentage of patients receiving intravenous tPA during the pandemic (15.5% versus 12.5%, P=0.037), and the number of thrombectomies per week was lower during the pandemic (1 [IQR, 0.5–1] versus 3 [IQR, 1–4], P=0.022) (Figure 2); otherwise, there was no difference in baseline features between the 2 groups. Table I in the Data Supplement who presented during COVID-19 pandemic and those who presented during the same time of the year (March and April) of 2019.
Figure 2.

The number of monthly thrombectomies during study period. COVID-19 indicates coronavirus disease 2019.
Table.
Baseline Characteristics and Outcomes of Telestroke Patients Presenting Before and During COVID-19 Pandemic
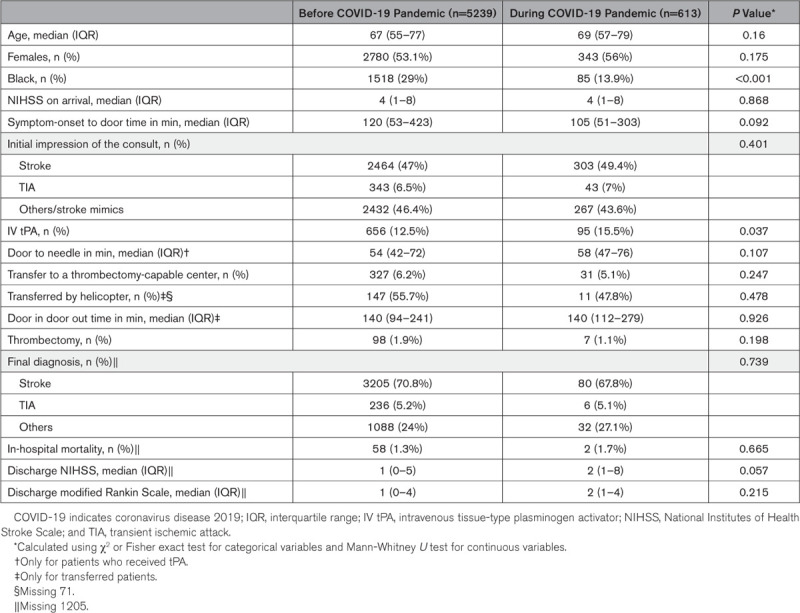
As summarized in Table II in the Data Supplement, there was higher rate of tPA in Black patients presenting during the pandemic compared with before (22.4% versus 13.5%, P=0.022). Otherwise, there was no difference in median age (72 [IQR, 60–82] versus 70 [IQR, 58–79], P=0.139), sex (49.4% versus 51.6% females, P=0.688), symptom-onset to presentation (85 [IQR, 50–209] versus 107 [IQR, 47–348], P=0.35), baseline National Institutes of Health Stroke Scale (4 [IQR, 1–10] versus 4 [IQR, 1–9], P=0.571), rate of transfer to a thrombectomy-capable stroke center (14.1% vs 10.2%, P=0.251), and rate of mechanical thrombectomy (3.5% versus 3.7%, P=1) between Black patients presenting during versus before COVID-19 pandemic.
Discussion
We evaluated the volume and outcomes of telestroke patients presenting during COVID-19 pandemic compared with patients presenting during the year prior. Our study shows an overall drop in the number of telestroke consults during the pandemic. Importantly, there was a disproportionately lower percentage of Black patients presenting during the pandemic.
Other studies have reported a decline in stroke presentations throughout the United States and the world during the COVID-19 pandemic.4,5 Our findings corroborate prior studies reporting falling stroke volume. However, our study is unique because it presents patient-level data in an area of high stroke rate and significant racial disparity.12,13 Interestingly, unlike previous studies, our study shows higher percentage of patients received tPA, without delay in treatment, and that similar percentages of patients received mechanical thrombectomy. One possible explanation to the higher rate of thrombolysis is that, while not statistically significant, there was a trend for shorter symptom-onset to hospital arrival time during COVID-19 pandemic by about 15 minutes which could be clinically significant.
An important finding in our study is that a lower percentage of Black patients presented with strokes during the pandemic. This finding is alarming, as many studies have highlighted existing racial disparities in stroke care, with Black patients having both higher risk factors as well as higher in-hospital mortality and burden of stroke disability.14 Black patients are also suffering from a higher incidence of COVID-19 infection, as well as an increased mortality rate.9,10 In this climate, Black patients may experience a stronger pull to avoid medical care, due to this harsh reality that their risk from COVID-19 is inherently higher than that facing other races. More concerning is the fact that the decline in number of Black patients presenting with stroke was not associated with an increased stroke severity in patients who presented, which might indicate that even patients with severe strokes did not present to emergency rooms for evaluation. If not addressed, this reluctance in seeking care may worsen the existing disparity in stroke outcome.
Limitations of our study include its retrospective nature and the uncertainty whether the decrease of patients with stroke presenting reflects a true decline in stroke rate as opposed to patients’ fear of presenting to medical facilities to avoid exposure to COVID-19. However, stroke rate is less likely to be affected by COVID-19 pandemic in South Carolina given the small number of cases (Table I in Data Supplement),15 and there is no strong data suggesting seasonal variation in stroke rate. Another limitation that we do not have the number of patients who had large artery occlusion which makes it difficult to know whether COVID-19 pandemic caused a higher rate of occlusions. However, we were able to show a stable rate of MTs performed during the pandemic.
Conclusions
There is a decrease in number of patients presenting with strokes during COVID-19 pandemic, which could be secondary to patients’ fear of exposure to COVID-19 in healthcare facilities. This concern is more alarming in Black patients. These results exemplify the crucial need for continued public health education about the importance of immediate stroke care.
Sources of Funding
None.
Disclosures
Dr Spiotta is a consultant for Penumbra, Stryker, Terumo, and Cerenovus, and receives research support from Penumbra. The other authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Supplementary Material
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
- tPA
- tissue-type plasminogen activator
For Sources of Funding and Disclosures, see page XXX.
Drs Cummings and Almallouhi contributed equally.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.120.031121.
References
- 1.Johns Hopkins University. COVID-19 dashboard by the center for systems science and engineering. https://coronavirus.jhu.edu/map.html. Accessed May 09, 2020.
- 2.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77:1–9https://jamanetwork.com/journals/jamaneurology/fullarticle/2764549. Accessed May,08, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babu Welch MD. Are stroke sufferers silent victims of COVID-19? https://utswmed.Org/medblog/covid19-stroke-volume-decrease/. Accessed May 09, 2020.
- 4.Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020; 29:104953.doi: 10.1016/j.jstrokecerebrovasdis.2020.104953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of covid-19 on stroke evaluation in the united states. N Engl J Med. 2020; 383:NEJMc2014816.https://www.nejm.org/doi/full/10.1056/NEJMc2014816. Accessed May 08, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yermal-Jr B. Amid pandemic, public wary of seeking non-coronavirus care from providers. 2020 https://morningconsult.Com/2020/05/04/coronavirus-health-care-providers-polling/. Accessed May 11, 2020.
- 7.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, et al. Stroke Thrombolysis Trialists’ Collaborative Group; Stroke Thrombolysis Trialists’ Collaborative Group Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384:1929–1935doi: 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, et al. DAWN Trial Investigators; DAWN Trial Investigators Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21doi: 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 9.Cw Y. COVID-19 and african americans. JAMA. 2020; 323:1891, 1892 [DOI] [PubMed] [Google Scholar]
- 10.Reyes CHN, Gutowski C, et al. Chicago’s coronavirus disparity: Black chicagoans are dying at nearly six times the rate of white residents, data show. https://www.chicagotribune.com/coronavirus/ct-coronavirus-chicago-coronavirus-deaths-demographics-lightfoot-20200406-77nlylhiavgjzb2wa4ckivh7mu-story.html. 2020. Accessed May 09, 2020. Chicago Tribune.
- 11.Almallouhi E, Holmstedt CA, Harvey J, Reardon C, Guerrero WR, Debenham E, Turner N, Aysse P, Al Kasab S. Long-term functional outcome of telestroke patients treated under drip-and-stay paradigm compared with patients treated in a comprehensive stroke center: a single center experience. Telemed J E Health. 2019; 25:724–729doi: 10.1089/tmj.2018.0137 [DOI] [PubMed] [Google Scholar]
- 12.Tabb LP, Ortiz A, Judd S, Cushman M, McClure LA. Exploring the spatial patterning in racial differences in cardiovascular health between blacks and whites across the United States: the REGARDS study. J Am Heart Assoc. 2020; 9:e016556.doi: 10.1161/JAHA.120.016556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ajinkya S, Almallouhi E, Turner N, Al Kasab S, Holmstedt CA. Racial/ethnic disparities in acute ischemic stroke treatment within a telestroke network. Telemed J E Health. 2019 [DOI] [PubMed] [Google Scholar]
- 14.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, et al. American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:2091–2116doi: 10.1161/STR.0b013e3182213e24 [DOI] [PubMed] [Google Scholar]
- 15.Sc testing data & projections (covid-19). https://scdhec.Gov/infectious-diseases/viruses/coronavirus-disease-2019-covid-19/sc-testing-data-projections-covid-19. Accessed June 20, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


