Supplemental Digital Content is available in the text.
Keywords: cohort studies, coronavirus, inpatients, patient care, stroke
Background and Purpose:
Shelter-in-place (SIP) orders implemented to mitigate severe acute respiratory syndrome coronavirus 2 spread may inadvertently discourage patient care-seeking behavior for critical conditions like acute ischemic stroke. We aimed to compare temporal trends in volume of acute stroke alerts, patient characteristics, telestroke care, and short-term outcomes pre- and post-SIP orders.
Methods:
We conducted a cohort study in 21 stroke centers of an integrated healthcare system serving 4.4+ million members across Northern California. We included adult patients who presented with suspected acute stroke and were evaluated by telestroke between January 1, 2019, and May 9, 2020. SIP orders announced the week of March 15, 2020, created pre (January 1, 2019, to March 14, 2020) and post (March 15, 2020, to May 9, 2020) cohort for comparison. Main outcomes were stroke alert volumes and inpatient mortality for stroke.
Results:
Stroke alert weekly volume post-SIP (mean, 98 [95% CI, 92–104]) decreased significantly compared with pre-SIP (mean, 132 [95% CI, 130–136]; P<0.001). Stroke discharges also dropped, in concordance with acute stroke alerts decrease. In total, 9120 patients were included: 8337 in pre- and 783 in post-SIP cohorts. There were no differences in patient demographics. Compared with pre-SIP, post-SIP patients had higher National Institutes of Health Stroke Scale scores (P=0.003), lower comorbidity score (P<0.001), and arrived more often by ambulance (P<0.001). Post-SIP, more patients had large vessel occlusions (P=0.03), and there were fewer stroke mimics (P=0.001). Discharge outcomes were similar for post-SIP and pre-SIP cohorts.
Conclusions:
In this cohort study, regional stroke alert and ischemic stroke discharge volumes decreased significantly in the early COVID-19 pandemic. Compared with pre-SIP, the post-SIP population showed no significant demographic differences but had lower comorbidity scores, more severe strokes, and more large vessel occlusions. The inpatient mortality was similar in both cohorts. Further studies are needed to understand the causes and implications of care avoidance to patients and healthcare systems.
As of June 25, 2020, the severe acute respiratory syndrome coronavirus 2 has infected >2.37 million people in the United States and 9.47 million people worldwide. This new coronavirus has claimed >100 000 American lives and caused >450 000 deaths worldwide.1,2 The impact of coronavirus disease 2019 (COVID-19) extends beyond viral pneumonia and acute respiratory distress syndrome.3–5
California was the location of the second identified outbreak of the US COVID-19 pandemic, following Washington state. To control the spread of COVID-19, California introduced strong social distancing and then shelter-in-place (SIP) measures early in the pandemic.6 While these measures appear to have helped flatten the curve of COVID-19 spread,7 there is concern that social isolation and fear of acquiring the infection in a healthcare setting may have led some patients with acute medical conditions like stroke and myocardial infarction8 to avoid calling emergency medical services or presenting to an emergency department (ED).9–16 Given that there are effective, time-sensitive treatments for acute stroke, including intravenous thrombolytic and endovascular stroke therapy, both of which improve long-term outcomes, avoidance of seeking health care for stroke symptoms may lead to increased disability and death.
Kaiser Permanente Northern California (KPNC) provides care for one-third of the population in Northern California. We sought to determine whether a decrease in acute stroke presentations occurred during the early COVID-19 pandemic in Northern California and to assess differences in patient characteristics and hospital outcomes for those who presented for acute stroke evaluation during the pandemic compared with those who presented before the pandemic.
Methods
Data Source
This study was approved by the KPNC Institutional Review Board, and informed consent was waived by the Institutional Review Board. Data from the study are available for sharing upon reasonable request to the corresponding author. KPNC provides care at 21 medical centers serving a population of 4.4 million members, who are highly representative of the ethnic and socioeconomic diversity of the surrounding and statewide population.17 All 21 KPNC hospitals are Joint Commission Stroke certified—19 as primary stroke centers and 2 as comprehensive stroke centers. There are ≈1.3 million ED visits and 3500 ischemic stroke discharges per year. In 2016, we implemented the KPNC Stroke Expediting the Process of Evaluating and Stopping Stroke program. The program included immediate evaluation by a telestroke neurologist via video, expedited intravenous alteplase treatment, rapid computed tomography angiographic study, and expedited transfer and treatment for patients with large vessel occlusion (LVO).18
The study population included patients with suspected acute stroke who presented to KPNC facilities from January 1, 2019 to May 9, 2020. All stroke alerts were evaluated by a telestroke neurologist, and data were recorded in standardized stroke assessment, treatment, and clinical notes. For patients deemed not to be candidates for acute stroke treatment, the stroke alert was canceled, and the teleneurologist recorded the initial evaluation and reasons for canceling. The telestroke neurologist proceeded with full acute stroke workup for all noncanceled stroke alerts. Clinical and demographic data were available from electronic medical records.
Exposure
We evaluated trends in stroke alert volume, trends in ischemic stroke discharge volume, and acute stroke patient characteristics relative to regional and statewide SIP orders for COVID-19. For stroke alert and discharge volumes, data were available from January 1, 2019 to May 23, 2020. SIP orders began on March 16, 2020, for the 6 counties in the San Francisco Bay area and on March 19, 2020, for the state of California. For patient-specific data analysis, we selected the week beginning with March 15, 2020, as a cut point. In addition, mobility data from the Institute of Health Metrics and Evaluation also supported this selection.19 Stroke alert patients seen from January 1, 2019 to March 14, 2020, were defined as pre-SIP and those seen March 15, 2020 to May 9, 2020, were in the post-SIP cohort. On May 4, 2020, Governor Newsom announced plans for stage 2 gradual reopening for the State of California. Stage 2 began on May 8, 2020. We selected May 9, 2020 (the last day of that week), as the end of the post-SIP cohort because we were interested in comparing the patients who were presenting during the SIP order (between March 15, 2020, and May 9, 2020) to those seen pre-SIP.
Patient Characteristics and Outcomes
We compared the mean weekly number of stroke alerts and inpatient stroke discharges during the pre- and the post-SIP periods. To control for potential seasonal trend in stroke occurrence and potential temporal change due to annual health plan membership, we compared stroke alert volumes during the same months for 2019 versus 2020. All stroke alerts identified through teleneurology notes were included. Stroke discharges were defined as hospitalizations with a principal discharge diagnosis of ischemic stroke at KPNC facilities. Patient characteristics including age, race/ethnicity, sex, and method of arrival were collected for all stroke alerts. We included history of atrial fibrillation, myocardial infarction, and stroke within the prior 5 years. In addition, a longitudinal comorbidity score (Comorbidity Point Score, version 2),20 reflecting inpatient and outpatient diagnoses captured over the preceding 12 months, was calculated for each patient. Stroke mimics were defined as patients who had a principal discharge diagnosis other than cerebral infarction, nontraumatic intracerebral/subarachnoid hemorrhage, transient cerebral ischemic attack, hemiplegia, hemiparesis, or cerebral ischemia.
For noncanceled stroke alerts, patients underwent a complete evaluation to confirm eligibility for acute interventions with either alteplase or endovascular stroke therapy. More detailed information was collected including last time known well (LTKW), initial National Institutes of Health Stroke Scale (NIHSS) score, treatment with alteplase, and presence of LVO. Time to presentation was defined as time from LTKW-to-ED-arrival time. Door-to-needle time was the number of minutes from ED arrival until alteplase administration. Door-to-needle time was calculated for patients in the study without application of accepted exclusions from the American Heart Association Get With The Guidelines. Treatment time for inpatient stroke alerts was calculated from time of stroke alert to alteplase administration. Patient outcomes included length of stay in days, discharge status, and inpatient mortality.
Statistics
To assess for differences between the categorical and continuous variables, Pearson χ2 tests and Kruskal Wallis tests were used, respectively. t tests were used to assess differences in stroke volume for pre- and post-SIP periods. We performed a multivariate logistic regression to assess whether patients from the post-SIP period were more or less likely to be discharged home, adjusted for age, sex, race, Comorbidity Point Score, version 2, NIHSS score, and treatment with alteplase, along with taking into account clustering by facility. All analyses were conducted using SAS software, version 9.4 (SAS Institute, Cary, NC). With a sample size of 783 in the post-SIP cohort and a 2-sided α-level of 0.05, we had >90% power to detect differences in proportions of at least 0.11 between cohorts.
Results
Weekly Stroke Alert Volumes and Ischemic Stroke Discharges
Throughout the study period, 9120 adults received a stroke alert: 8337 in the pre-SIP and 783 in the post-SIP period (Table 1). From January to July 2019, weekly stroke alert volumes ranged from 120 to 160 alerts per week (Figure 1A). During January 5 to March 14, 2020, the average stroke alert volume was 136 cases per week (95% CI, 125–147). This was like the volume seen during the same period of 2019 (mean, 131 [95% CI, 126–137]; P=0.4). Overall, weekly stroke alert volume post-SIP (mean, 98 [95% CI, 92–104]) decreased significantly compared with the entire pre-SIP period (mean, 133 [95% CI, 130–136]; P<0.0001). It was also significantly lower than the volume for the preceding months in 2020 before SIP, as well as compared with the volume during the same period in 2019 (mean, 139 [95% CI, 124–154]; P<0.0001). After May 9, 2020, stroke alert volumes have returned to typical range for the region. The weekly ischemic stroke discharge volumes also decreased post-SIP (Figure 1B) and have increased after May 9, 2020, but not yet to the typical range. The percentage decrease in weekly stroke alert volumes varied across Northern California (Figure 2).
Table 1.
Patient Characteristics for All Stroke Alerts During Pre-SIP and Post-SIP Cohorts
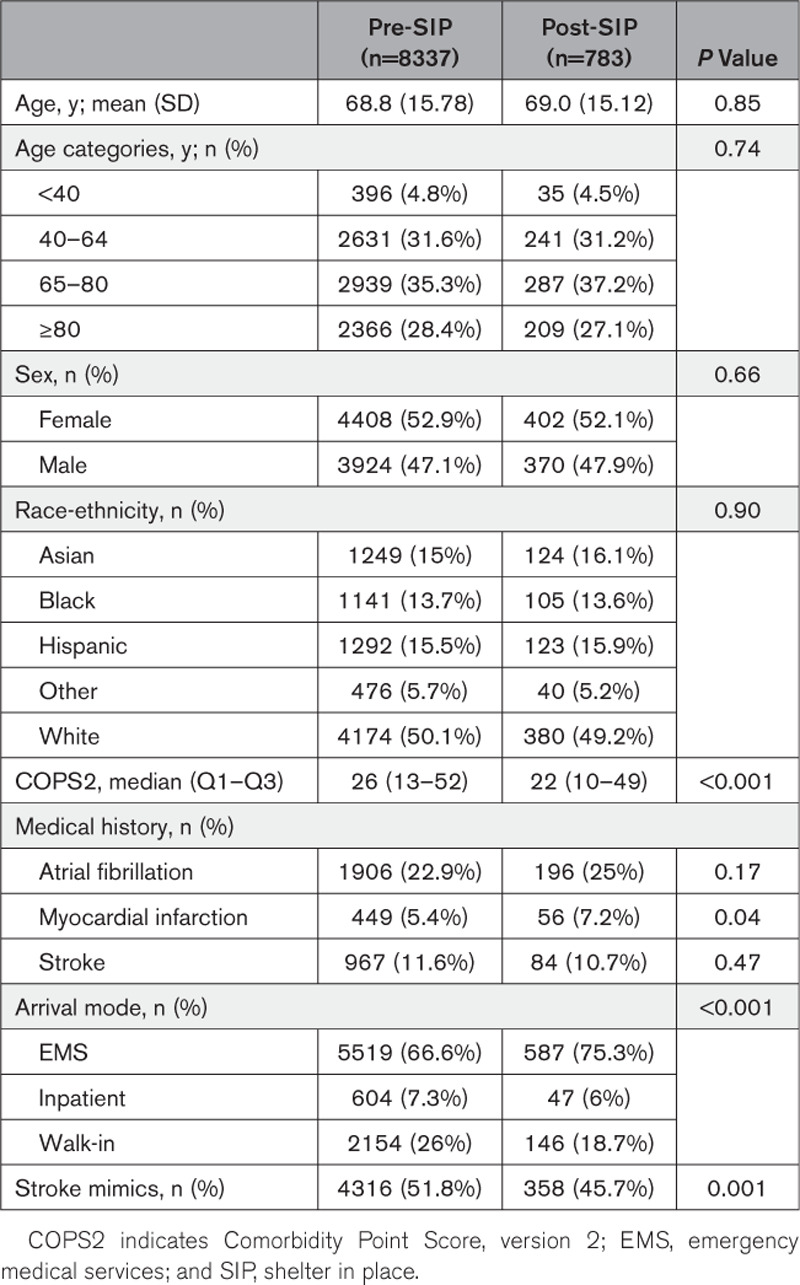
Figure 1.
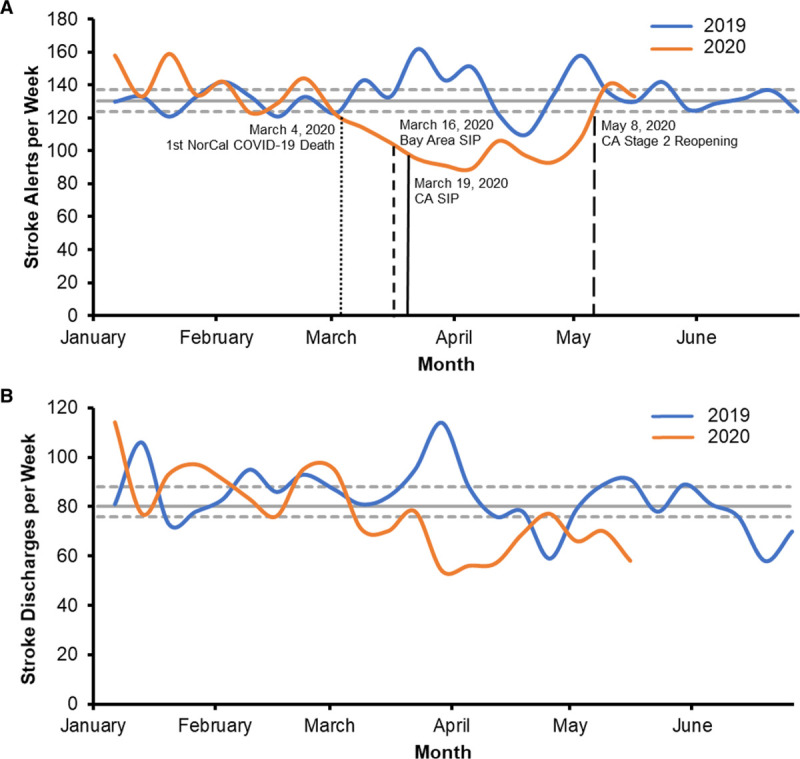
Stroke alert volumes and ischemic stroke discharges for 2019 and 2020.A, Weekly stroke alert volumes throughout the study period. B, Weekly ischemic stroke discharges in 2019 and 2020. On March 4, 2020, the first coronavirus disease 2019 (COVID-19)–related death was reported in Northern California (NorCal). On March 16, 2020, the Bay Area counties issued a shelter-in-place (SIP) order. On March 19, 2020, a SIP order was in effect for the state of California (CA). On May 8, 2019, CA moved into stage 2 of gradual reopening.
Figure 2.
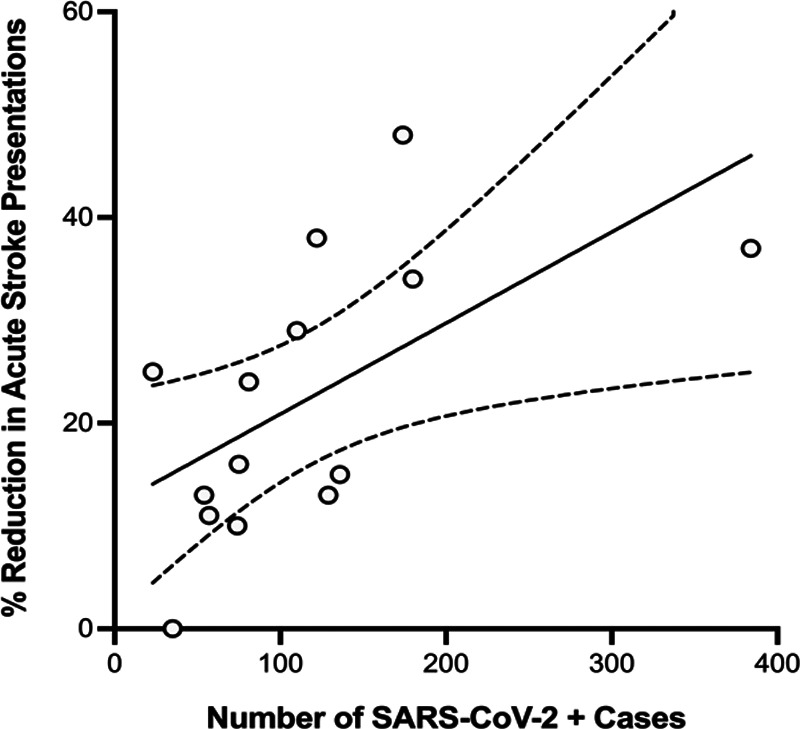
Percentage change in weekly stroke alert volume from the period of March 15, 2020 to April 18, 2020, compared with pre–shelter-in-place order cohort along with the total number of severe acute respiratory syndrome coronavirus 2–positive cases admitted during this time for each service area in Northern California. Slope, 0.09 (95% CI, 0.01–0.16); P=0.02 for deviation from zero. Goodness-of-fit R2, 0.36. SARS-CoV-2 indicates severe acute respiratory coronavirus 2.
Patient Characteristics of Pre- Versus Post-SIP Cohorts
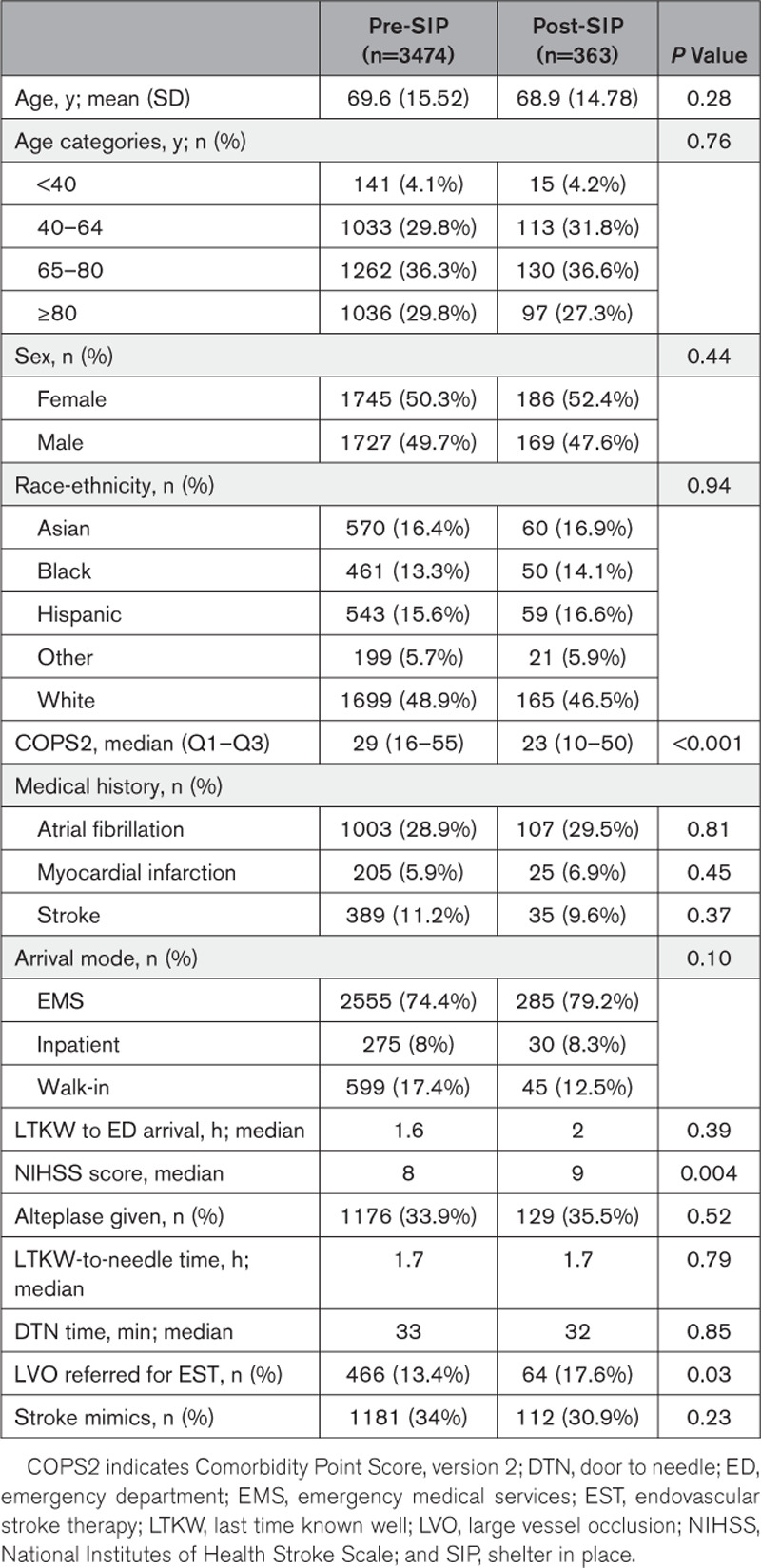
Patient demographics were similar in pre- and post-SIP cohorts among all stroke alerts and also noncanceled stroke alerts (Tables 1 and 2). There were statistically lower comorbidity scores in patients presenting with stroke symptoms post-SIP (Tables 1 and 2). In the post-SIP cohort among all stroke alerts (Table 1), more patients arrived at the ED by ambulance, and there were fewer stroke alert calls from walk-in or inpatient services (P<0.001). Noncanceled stroke alerts post-SIP had similar LTKW-to-ED-arrival time as pre-SIP (2 hours post-SIP and 1.6 hours pre-SIP, P=0.39). Post-SIP patients had higher NIHSS scores compared with the pre-SIP cohort (P=0.003). There were less stroke mimics seen as stroke alerts post-SIP (P=0.001). The percentage of patients receiving alteplase was not significantly different. Median door-to-needle time among noncanceled stroke alerts was unchanged during the study (34 minutes post-SIP versus 33 minutes pre-SIP, P=0.48). In addition, the median times from LTKW-to-needle time or alteplase treatment time were not significantly different between pre and post cohorts (1.7 hours, P=0.84; Table 2). Post-SIP, among noncanceled stroke alerts, more patients had LVO and were referred for endovascular stroke therapy (17.6% in post versus 13.4% in pre, P=0.03). Furthermore, patients presenting to the ED after May 9, 2020, were more similar to those in the pre-SIP cohort (January 1, 2019 to March 14, 2020) with regard to having a lower NIHSS score, higher percentage of stroke mimics, and fewer LVOs, but they were more similar to the post-SIP cohort (March 15, 2020 to May 9, 2020) with regard to arriving more by emergency medical services and having a lower Comorbidity Point Score, version 2, score (Tables I and II in the Data Supplement).
Table 2.
Patient Characteristics for Noncanceled Stroke Alerts During Pre-SIP and Post-SIP Cohorts
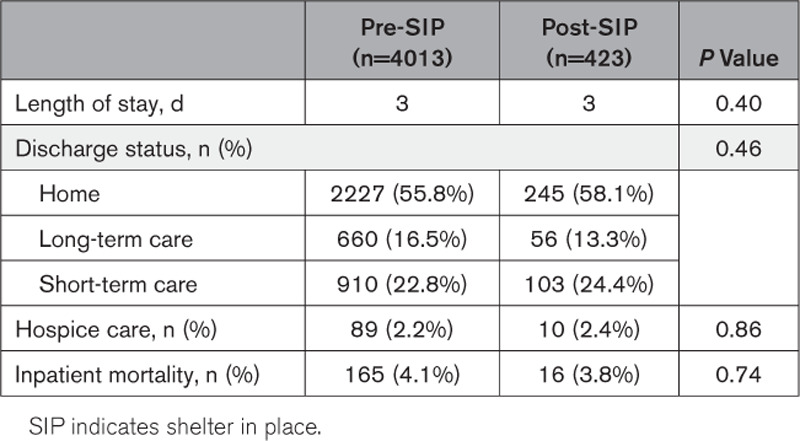
Hospitalization Outcomes
Removing stroke mimics, we examined hospital outcomes for those who were admitted after stroke alert (Table 3). Length of stay in hospital was similar between pre- and post-SIP cohorts (Table 3). The discharge status was similar for the pre- and post-SIP (P=0.44). In an adjusted multivariate model, patients from the post-SIP cohort were less likely to be discharged home (adjusted odds ratio, 0.67; P=0.04). There was no difference in inpatient mortality between the cohorts (P=0.75). In addition, none of the stroke alert patients had a positive severe acute respiratory syndrome coronavirus 2 test within 28 days of their index hospitalization.
Table 3.
Hospitalization Outcomes for Pre-SIP Compared With Post-SIP Cohorts Without Stroke Mimics
Discussion
It has been reported by mass media9,21–23 and medical journals8,24–28 that since the outbreak of COVID-19, non–COVID-19–related visits in both the ambulatory and emergency settings have been dramatically decreased. Our study revealed that stroke alert volumes and ischemic stroke discharges in Northern California started to decrease in early March 2020 and dropped significantly after the announcements of SIP orders. The stroke alert volumes have subsequently returned to the typical range since May 9, 2020. Post-SIP, telestroke evaluation and treatment times were similar before and after the pandemic. For those who were admitted, there was no difference in the inpatient mortality rate between the pre- and post-SIP cohorts or discharge disposition.
Declines in the number of outpatient visits were observed in all regions of the United States. Visits declined ≈60% in mid-March and remained low through mid-April.22 While some have reported a delay in presentation from stroke onset to arrival,15 others have not found that.12 Our data would suggest that potential stroke patients were not only missing the stroke alert window (up to 24 hours after LTKW) but they were not coming in at all for admission and evaluation, as our stroke discharge volume has also decreased significantly. For those who were still presenting for evaluation, they did not delay much, as their LTKW-to-ED-arrival time and thrombolytic time did not change significantly.
A national survey done by the American College of Emergency Physician reported that 80% of the surveyed adults said that they were concerned about contracting COVID-19 from another patient or visitor if they went to the ED. Twenty-nine percent had actively delayed or avoided seeking medical care due to concerns about contracting COVID-19. When considering a trip to ED, 73% were concerned about overstressing the healthcare system.29
Our study findings revealed that patients who presented to our regional telestroke team for acute stroke evaluation appeared to be those with lower comorbidity scores and higher NIHSS scores. Those with stroke symptoms and more comorbidities or with minor symptoms may have been more fearful to present to the ED. We also saw fewer stroke mimics presenting to the ED during the early pandemic. For those who did seek acute care, our study showed that it was possible to continue to treat acute strokes expeditiously during the pandemic. Post-SIP, door-to-needle time performance remained excellent as before the pandemic. With the announcement of stage 2 gradual reopening for California, we observed a significant increase in the stroke alert volume. This later cohort had milder strokes and more stroke mimics, but these patients were still more likely to come in via emergency medical services and had a lower comorbidity score than those in the pre-SIP cohort.
Examining stroke hospitalizations post-SIP, we did not find any severe acute respiratory syndrome coronavirus 2–positive cases among these acute stroke patients. However, there was somewhat limited COVID-19 testing during the study period due to more stringent criteria and less availability of testing kits. There was no change in in-hospital mortality between the pre- and post-SIP cohorts.4 It has been reported that COVID-19 is strongly associated with neurological presentations, including stroke,30 hypercoagulable state,31 and LVO in the young.32 We observed a higher percentage of patients in the post-SIP cohort with LVO and referral for endovascular stroke therapy. Our study, however, cannot tease out whether the observed increased rate of LVO in the post-SIP cohort reflected an actual increase in the incidence of LVO during COVID-19 pandemic or just a relative decrease in non-LVO presentations. Because of the retrospective nature of the study, we did not have direct data on stroke patients who were not presenting to the ED. However, given the consistent historical data from our telestroke program, we could gain some understanding of who may be staying home during the pandemic by examining the differences in patient characteristics between the 2 cohorts. In addition, we did not have data regarding changes in how our emergency medical services partners may have triaged potential stroke patients during the pandemic and whether this might explain the observed changes in volume of stroke presentation during the post-SIP period.
Stroke is the leading cause of long-term disability worldwide.33 Delay in seeking evaluation and treatment for acute stroke symptoms may lead to more stroke-related complications. It was reported that US deaths soared in the early weeks of the COVID-19 pandemic, far exceeding the number attributed to COVID-19.34 Some metropolitan areas have reported seeing an increase in mortality rates at home.35 The outcome of patients who did not seek acute care for stroke symptoms deserves further investigation.
Conclusions
We report a significant decrease in stroke alert volumes and ischemic stroke discharges in Northern California after middle of March 2020, with a return to normal volumes following the loosening of the initial SIP orders. The spreading COVID-19 pandemic, its related deaths, and public announcements of SIP orders may have contributed to these decreases. In addition, patients with stroke mimics or less severe stroke presentations and more comorbidities may be avoiding seeking ED evaluation and care. There was no increase in inpatient mortality for stroke patients who were admitted and treated during the pandemic. To reduce future potential complications from untreated strokes, clearer and more targeted communications may be needed to advise patients with stroke symptoms to present for workup and management. Further studies are needed to evaluate the potential unintended consequences to patient outcomes and to healthcare systems when patients with acute stroke avoid seeking emergent care.
Sources of Funding
None.
Disclosures
Drs Nguyen-Huynh and Vinson are partly supported by funding from the Permanente Medical Group Physician Researcher Program. Drs Nguyen-Huynh and Sidney receive grant funding from the National Institute of Neurological Disorders and Stroke. Dr Sidney receives grant funding from the National Heart Lung and Blood Institute. The other authors report no conflicts.
Supplementary Material
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
- ED
- emergency department
- KPNC
- Kaiser Permanente Northern California
- LTKW
- last time known well
- LVO
- large vessel occlusion
- NIHSS
- National Institutes of Health Stroke Scale
- SIP
- shelter in place
For Sources of Funding and Disclosures, see page XXX.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.120.031099.
References
- 1.Coronavirus Disease 2019 (COVID-19) - Cases in the US. Centers for Disease Control and Prevention; https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html#2019coronavirus-summary. Accessed June 25, 2020. [Google Scholar]
- 2.World Health Organization; WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/. Accessed June 25, 2020. [Google Scholar]
- 3.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [published online May 8, 2020]. N Engl J Med. 2020doi: 10.1056/NEJMc2014816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenbaum L. The untold toll - the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020; 382:2368–2371doi: 10.1056/NEJMms2009984 [DOI] [PubMed] [Google Scholar]
- 5.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77:1–9doi: 10.1001/jamaneurol.2020.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benade MM, Warlow CP. Cost of identifying patients for carotid endarterectomy. Stroke. 2002; 33:435–439doi: 10.1161/hs0202.102879 [DOI] [PubMed] [Google Scholar]
- 7.COVID-19 Statewide Update. California State. https://update.covid19.ca.gov/#top. Accessed April 12, 2020.
- 8.Solomon MD, NcNulty EJ, Rana JS, Leong T, Lee C, Sun SH, Ambrosy A, Sidney S, Go A. The Covid-19 pandemic and the incidence of acute myocardial infarction [published online May 19, 2020]. N Engl J Med. 2020doi: 10.1056/NEJMc2015630 [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM. Where have all the heart attacks gone? The New York Times. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html. 2020. Accessed April 12, 2020. [Google Scholar]
- 10.Bres Bullrich M, Fridman S, Mandzia JL, Mai LM, Khaw A, Vargas Gonzalez JC, Bagur R, Sposato LA. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 20201–4doi: 10.1017/cjn.2020.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, Zaino D, Michieletti E, Guidetti D. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020; 83:213–215doi: 10.1159/000507666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pop R, Quenardelle V, Hasiu A, Mihoc D, Sellal F, Dugay MH, Lebedinsky PA, Schluck E, La Porta A, Courtois S, et al. Impact of the Covid-19 outbreak on acute stroke pathways - insights from the Alsace region in France [published online May 12, 2020]. Eur J Neurol. 20201–5doi: 10.1111/ene.14316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schirmer CM, Ringer AJ, Arthur AS, Binning MJ, Fox WC, James RF, Levitt MR, Tawk RG, Veznedaroglu E, Walker M, et al. Endovascular Research Group (ENRG); Endovascular Research Group (ENRG) Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg. 2020; 12:639–642doi: 10.1136/neurintsurg-2020-016299 [DOI] [PubMed] [Google Scholar]
- 14.Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020; 29:104953.doi: 10.1016/j.jstrokecerebrovasdis.2020.104953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teo KC, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY, Kwok WM, Leung KK, Tse MY, Cheung RTF, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020; 51:2228–2231doi: 10.1161/STROKEAHA.120.030105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020; 51:1996–2001doi: 10.1161/STROKEAHA.120.030225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordon N, Lin T. The Kaiser Permanente Northern California adult member health survey. Perm J. 2016; 20:15–225doi: 10.7812/TPP/15-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen-Huynh MN, Klingman JG, Avins AL, Rao VA, Eaton A, Bhopale S, Kim AC, Morehouse JW, Flint AC. KPNC Stroke FORCE Team; KPNC Stroke FORCE Team Novel telestroke program improves thrombolysis for acute stroke across 21 hospitals of an integrated healthcare system. Stroke. 2018; 49:133–139doi: 10.1161/STROKEAHA.117.018413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.COVID-19 Projections. Institute for Health Metrics and Evaluation; https://covid19.healthdata.org/united-states-of-america/california. Accessed June 25, 2020. [Google Scholar]
- 20.Escobar GJ, Gardner MN, Greene JD, Draper D, Kipnis P. Risk-adjusting hospital mortality using a comprehensive electronic record in an integrated health care delivery system. Med Care. 2013; 51:446–453doi: 10.1097/MLR.0b013e3182881c8e [DOI] [PubMed] [Google Scholar]
- 21.McNamara D. COVID-19: Are Acute Stroke Patients Avoiding Emergency Care? Medscape; https://www.medscape.com/viewarticle/928337. 2020. Accessed April 12, 2020. [Google Scholar]
- 22.Mehrota A, Chernew M, Linetsky D, Hatch H, Cutler D. What Impact Has COVID-19 Had on Outpatient Visits? The Commonwealth Fund; https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. 2020. Accessed May 3, 2020. [Google Scholar]
- 23.Whiting S. A shelter-in-place side effect: Bay Area people are afraid to go to the hospital. San Francisco Chronicle. https://www.sfchronicle.com/bayarea/article/A-shelter-in-place-side-effect-Bay-Area-people-15219842.php. 2020. Accessed April 23, 2020. [Google Scholar]
- 24.Rodríguez-Leor O, Alvarez-Álvarez B, Ojeda S, Martín-Moreiras J, Rumoroso J, López-Palop R, Serrador A, Cequier Á, Romaguera R, Cruz I, et al. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC: Interventional Cardiology. 2020; 2:82–89 [Google Scholar]
- 25.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020; 369:m1401.doi: 10.1136/bmj.m1401 [DOI] [PubMed] [Google Scholar]
- 26.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020; 75:2871–2872doi: 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong LE, Hawkins JE, Langness S, Murrell KL, Iris P, Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catalyst. 2020doi: 10.1056/CAT.20.0193 [Google Scholar]
- 28.Naccarato M, Scali I, Olivo S, Ajčević M, Buoite Stella A, Furlanis G, Lugnan C, Caruso P, Peratoner A, Cominotto F, et al. Has COVID-19 played an unexpected “stroke” on the chain of survival? J Neurol Sci. 2020; 414:116889.doi: 10.1016/j.jns.2020.116889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kocher MS, Henley MB. It is money that matters: decision analysis and cost-effectiveness analysis. Clin Orthop Relat Res. 2003; 413:106–116doi: 10.1097/01.blo.0000079326.41006.4e [DOI] [PubMed] [Google Scholar]
- 30.Avula A, Nalleballe K, Narula N, Sapozhnikov S, Dandu V, Toom S, Glaser A, Elsayegh D. COVID-19 presenting as stroke. Brain Behav Immun. 2020; 87:115–119doi: 10.1016/j.bbi.2020.04.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spiezia L, Boscolo A, Poletto F, Cerruti L, Tiberio I, Campello E, Navalesi P, Simioni P. COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020; 120:998–1000doi: 10.1055/s-0040-1710018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020; 382:e60.doi: 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stroke Facts. Centers for Disease Control and Prevention; https://www.cdc.gov/stroke/facts.htm. Accessed April 12, 2020. [Google Scholar]
- 34.Brown E, Tran AB, Reinhard B, Ulmanu M. U.S. deaths soared in early weeks of pandemic, far exceeding number attributed to covid-19. The Washington Post. https://www.washingtonpost.com/investigations/2020/04/27/covid-19-death-toll-undercounted/?arc404=true. 2020. Accessed May 3, 2020. [Google Scholar]
- 35.Gillum J, Song L, Kao J. That Suggests Coronavirus Deaths Are Higher Than Reported. ProPublica; There’s Been a Spike in People Dying at Home in Several Cities. https://www.propublica.org/article/theres-been-a-spike-in-people-dying-at-home-in-several-cities-that-suggests-coronavirus-deaths-are-higher-than-reported. 2020. Accessed May 11, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


