Abstract
The pandemic of severe acute respiratory syndrome coronavirus 2 has spread across the world, causing causalities and inflicting chronic complications in those who survive the infection. Disruptions in the immune system and lowered physical levels caused by quarantine protocols are the major causes of chronic dysfunction and impaired life independency, especially in elderly patients. Multiple exercise suggestions and novel program delivery methods, including telerehabilitation/tele-exercise programs, home-gym strategies, and exergames, have emerged. Patients with underlying obesity, diabetes mellitus, malnutrition, or binge-eating problems are at a high risk of serious infection and sequela. Adequate education and coping strategies can lessen the potential infection complications and improve the quality of life. Acknowledging the possible benefits and risks of nonsteroidal anti-inflammatory drug usage in chronic pain patients, and the supplementation of vitamin D may also aid in treating post-infected patients.
Keywords: Coronavirus disease, COVID-19, Exercise, Geriatric patients, Medication, Nutrition, SARS-CoV-2
1. INTRODUCTION
The global pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused serious decline in the world’s economic, health, and social parameters. As countries strive to withstand the catastrophes and consider to reopen businesses, further discussions about the long-term sequela of virus infection and associated management choices have emerged only recently.1 Prediction models show that about one-fourth to one-third of the patients suffering from COVID-19 will require further rehabilitation after curation, and the disability rates in high-risk populations, such as geriatric patients and those with predisposing diabetes mellitus or other co-morbidities, would be higher.2,3 The main cause of this phenomenon is the varied symptoms that the virus induce in the human body, including disruptions in heart and lung functions. Importantly, social distancing and quarantine protocols cause further deterioration of physical activity levels and quantity.
As healthcare providers, we must shed light on this ongoing trend of changing lifestyles and physical activity properties and provide our patients with comprehensive strategies to maintain fitness levels during the quarantine.4
2. EXERCISE/REHABILITATION
2.1. How physical activity function is affected by the SARS-COV-2
SARS-COV-2 is a single-stranded RNA virus that enters the human body by binding to angiotensin-converting enzyme 2 (ACE2) receptor. The most possible entry points for SARS-COV-2 are primarily the lungs and small intestines and correlate with the initial presentations of diarrhea, nausea, and cough. After entry, SARS-COV-2 affects the human body in various ways. The virus activates the antibody-secreting cells and follicular helper T cells. The associated cytokines, including monocyte chemoattractant protein (MCP)-1 (C-C motif chemokine ligand 2), show decreased concentration during acute infection.5 The elevated levels of other cytokines, including interleukin (IL)-1β, IL-8, IL-10, granulocyte colony-stimulating factor, interferon γ, MCP-1, platelet-derived growth factor subunit B, tumor necrosis factor (TNF) α, and vascular endothelial growth factor A, were noted in patients suffering from early cytokine storm, causing hyperacute immune response and eventually progressing into a more severe disease state.3 Peripheral neural inflammation is frequently induced by COVID-19 through the actions of local immune responses, thus contributing to focal pain-related symptoms which can hinder physical activity motives and lead to a sedentary lifestyle.
As the infection spreads, other organs become further involved, causing severe complications, including myocarditis, acute respiratory distress syndrome, and vasculitis,3 which demolish the heart and lung reserved functional capacity, and decreasing ADL independence and the quality of life. Studies have shown that 90% of patients have zero-to-mild symptoms, whereas 10% suffer from serious complications.6 Most patients in this 10% group include those with preexisting comorbidities or in their old age. Especially in the geriatric population, the virus produces acute geriatric symptoms, such as delirium, dehydration, and falls, owing to the predisposing comorbidities, including frailty, sarcopenia, and malnutrition.7 High levels of white blood cells, neutrophils, and C-reactive proteins (CRP) are also observed in elderly patients. Computed tomography is an efficient way of revealing lung involvement in SARS-COV-2. Multi-lobule lesions are frequently found in the elderly.8 Elevated intensive care unit hospitalization and mortality rate also occur among elderly patients.6,8
SARS-COV-2 infection spreads between individuals through contaminated surfaces in the environment. Thus, strategies, such as hand hygiene, wearing a mask, and maintaining social distances, became the top priority to prevent contagious spreading. The diagnosis can be made by real-time reverse transcription-polymerase chain reaction techniques, with samples acquired through nasal swabs, aspirates from trachea, or bronchoalveolar lavage. Although many medications, including chloroquine, monoclonal antibodies, and other antiviral agents, have been tested for their efficacy in treating COVID-19, no definite treatment has emerged yet.6
Geriatric patients residing in nursing homes generally suffer from comorbidities. The immune-compromised nature of the residents renders this kind of long-term care facility prone to viral infection spread.9 High rates of pneumonia were noted within these places before the COVID-19 epidemic. Specific measurements, including restriction or prescreening of visitors and avoidance of unnecessary transfer of patients, are needed to lessen the possibility of infection transmission.
2.2. How increasing physical activity can reduce viral burden and increase daily function
The human immune system can be enhanced by thorough nutrition intake and adequate physical activity.10 Physical activities have the long-term positive effects of alleviating stress, enhancing mood, and promoting long-term mental health. Resistance and flexibility exercises can promote muscular health and prevent ligamentous or tendinous injuries. Cardiovascular exercise, on the contrary, can benefit an individual by improving the heart and lung functional capacity, decreasing systemic inflammatory levels, and supporting the human body in combating viral infections and related sequela.
Disputes have arisen regarding the benefits of high-intensity interval exercises (HIIT) over moderate-intensity exercises to the immune system. HIIT exercises modulate systemic inflammatory responses, including reducing plasma alanine aminotransferase and aspartate aminotransferase levels; however, whether HIIT exercises provide more benefit than regular exercise is still under debate.11 In studies regarding exercise physiology and immunology, given that moderate exercise intensity can boost the exchange of immune cells between the tissue and the system, high-to-peak exercise intensities can cause systemic inflammation stress, oxidative stress, and muscular injuries, thus disrupting the immune system.12 Regular exercise training shows better anti-inflammatory properties than short bouts of non-regular exercises.
Increasing cardiorespiratory fitness in elderly patients is important because the benefits of physical activity extend to the prevention of age-related diseases, such as frailty, sarcopenia, dynapenia, cognitive decline, and self-esteem.13 Specific exercise recommendations for elder people generally follow the guidelines published by the American College of Sports Medicine,↱ with slight modifications in light of decreased physical activity during quarantine. The frequency of exercise is set at >5 times per week and the volume at 200–400 minutes per week, with 2–3 days per week of resistance exercise. Given that high-intensity exercises may have detrimental effects on the immune system, moderate exercise intensity is suggested for older people. Although the great variability of exercises can heighten motive, the goals of maintaining safety must not be undermined. Supervision is needed to ensure that the elders have company during exercises, and that emergent aid is within reach to prevent fall accidents.
Public gyms have been closed due to the stay-at-home policy. Thus, healthcare providers must focus on implementing strategies for patients to maintain adequate workout levels at home, with or without gym equipment. Easy exercises that can be performed at home without purchasing equipment include squatting while holding a chair, getting up from a chair, step ups and downs, and walking around the house or tracing a line on the floor with the feet, etc.13
Several apps with personalized training features have emerged, motivating people to reinforce their health. Other apps include a social connection function, benefiting those in need of social motivation.4 Other online classes, including cycling, yoga, and dance classes, can be broadcast by means of video conferences to allow clients to exercise in a safe and comfort environment.4 For those who insist on working out outdoors, personalized training videos focusing on improving the form and posture can be taught through virtual classes, thereby modifying the exercise form of the clients and reducing future injury risks when the quarantine policy is lifted. Overall, the goal is to provide patients with optimal choices that best suit their personal interests and individualized goals. Overtraining should also be avoided during this period given the limited access to healthcare.
When walking or running outdoors during social distancing, wearing a mask can cause extra resistance in breathing. The training intensity must be modified to a low level to balance this extra burden. Hyperventilation can be further prevented by avoiding shallow breathing and encouraging deep diaphragmatic breathing. Tracking each individual’s personal progress with a wearable device can also boost morale and self-confidence through progress visualization.
Moreover, if traditional exercises are unappealing, the newly growing trend of exergames can offer a novel and enjoyable exercise option. Exergames, including those related to dancing, boxing, and many other sports, can act as a moderate-intensity training; they not only offer the benefits of a traditional physical activity but also relieve anxiety to a great extent.14
Although telerehabilitation and tele-exercise show promise, other people are at risk to take part in regular, non-individualized programs. Those who have been infected with SARS-CoV-2 but showed no symptoms should continue their regular exercise protocols at a level similar to those free of disease. For symptomatic patients, further detailed evaluation of health status by a medical profession is crucial before commencing any form of training regime. Pre-exercise screening questionnaires may help in quick identification of individuals in need of medical attention and are unsuitable to take part in tele-exercise or telerehabilitation(Fig. 1).15
Fig. 1.
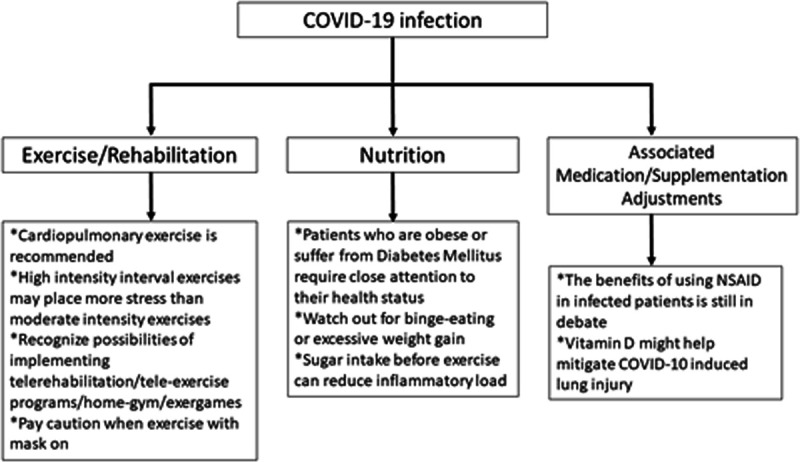
Summary of exercise, nutrition, and medication considerations regarding the COVID pandemic.
3. NUTRITION
Malnutrition and obesity, which are indicators of imbalanced nutrition status, can cause disruption in the immune system. Obesity can cause systemic metabolic dysfunction through inducing a chronic and low-grade systemic inflammation characterized by elevated CRP levels.16 Obese patients have high levels of leptin (a pro-inflammatory adipokine) and low levels of adiponectin (an anti-inflammatory adipokine). High levels of alpha-TNF, MCP-1, and IL-6, which are mainly produced by adipose tissue, cause innate immunity dysfunction and are also observed in obese patients.17 When obesity occurs in combination with diabetes mellitus, adaptive immunity may be further altered by impaired neutrophil function and T cell response on challenge and elevated macrophage levels in circulation. Patients with such condition must be identified and supported with a nutritional and physical activity strategy that is suitable to their individual needs.
The COVID-19 pandemic has caused additional stress to various individuals, and several people counter their stress with binge eating, which can result in regret, physical discomfort, and weight gain.4 Healthcare providers must encourage patients, especially those with chronic diabetes mellitus, to monitor their weight gains and losses and provide them with countermeasures when necessary.
Infections of the lungs or other organs can cause elevated blood sugar, which can impede infection control.8 However, a small amount of sugar intake before or during exercise can have anti-inflammatory, antioxidative, and immune cell signaling effects. The complex relationships between different blood sugar levels and the immune system must be considered, and patients must be provided with adequate blood sugar control medications, self-monitoring protocols, and other coping strategies(Fig).
4. ASSOCIATED MEDICATION/SUPPLEMENTATION ADJUSTMENTS
4.1. Non-steroidal anti-inflammatory drugs and corticosteroids
Many patients with chronic pain conditions rely on long-term prescriptions of Non-steroidal anti-inflammatory drugs (NSAIDs) to ease their pain. Several experts argue that taking NSAIDs can demolish the immune system and increase the susceptibility to viral infection. At present, no solid evidence indicates whether stopping NSAID medication affects susceptibility to viral infection.18 Studies have shown that NSAIDs can reduce viral replication,19 and corticosteroids can alleviate pulmonary inflammation, thus improve outcomes.20 However, other studies have shown that corticosteroids elevate the concentration of viral RNA, and that prolonged administration may enhance viral replication.21 Thus, short-term usage of NSAIDs is still recognized, but whether previous chronic NSAID prescriptions should be stopped still requires evidence to support the decision making.
4.2. Vitamin D
Vitamin D has multiple roles related to infection modulation,22,23 sleep–wake cycle,24 depression management,25 and chronic pain control.26 Decreased serum vitamin D levels are observed with aging due to the lack of sun exposure and skin synthesis. In countries with low latitude, people prefer staying in the shade than under the sun, thus implying a low serum vitamin D level in their body and resulting in high COVID-19 infection and mortality rates.22 Vitamin D has a promising role in treating elderly patients with chronic pain issues, and its supplementation might mitigate the acute lung injury caused by COVID-19. The possible mechanism is that COVID-19 infection is mediated by the ACE2 receptor, and calcitriol (1,25-dihydroxyvitamin D3) can enhance the ACE2 expression.27 The current studies regarding vitamin D focus more on the deficiency causing the symptoms rather than the supplementations that relieve them. Thus, well-coordinated vitamin D supplementation studies should be carried out to further confirm the routine use of vitamin D in chronic pain geriatric patients with high risk of COVID-19 (Fig).
In conclusion, the immune reactions and decreased physical activity levels caused by SARS-COV-2 are the primary reasons for the disabilities appearing in the post-infection stages, especially in the geriatric population. Multiple counter-strategies, including physical activity modification, nutritional consultations, and medication/supplement refinement, must be implemented to strengthen the person’s resistance against the ongoing global threat. Although cardiovascular exercises can improve heart and lung functional capacity, exercises with moderate intensities can boost an individual’s immune health and at the same time maintain safety compared with high-exertion exercises. Tele-exercise and home-gym programs which implement tailored apps or wearable devices can provide easy-accessible exercise programs and allow healthcare providers to achieve improved, real-time insights into the training status of patients and share professional opinions with a focus on the patients’ strengths and weaknesses. Identifying patients with underlying obesity, diabetes mellitus conditions, malnutrition, or binge-eating problems and providing them with lifestyle modification methods can have a key role in their fight against COVID-19. NSAID and vitamin D usage in infected patients or patients with high risk should also be seriously considered, including their possible benefits and risks. This study has several limitations. We attempted to enroll as many articles regarding chronic care of COVID-19-affected patients as possible, but other papers might have been missed. We also failed to gain access to several articles with fully relatable titles and abstract. Future studies should focus on the possibility of implementing telerehabilitation and tele-health programs in a greater degree in the light of social-distancing and quarantine28 to investigate the optimal prescription of chronic medications and other supplementations in COVID-19 patients.
ACKNOWLEDGMENTS
This study was funded by the Ministry of Science and Technology (MOST 108-2314-B-010-042-MY3), Taipei Veterans General Hospital (V109C-072) and Taipei Veterans General Hospital –National Taiwan University Hospital Joint Research Program (TVGH-NTUH VN109-11).
Footnotes
Conflicts of interest: The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
REFERENCES
- 1.Altmann DM, Douek DC, Boyton RJ. What policy makers need to know about COVID-19 protective immunity. Lancet. 2020; 395:1527–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith SR, Jenq G, Claflin T, Magnant C, Haig AJ, Hurvitz E. Proposed workflow for rehabilitation in a field hospital setting during the COVID-19 pandemic PM R. 2020Doi: 10.1002/pmrj.12405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nanda A, Vura NVRK, Gravenstein S. COVID-19 in older adults. Aging Clin Exp Res. 2020; 32:1199–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nyenhuis SM, Greiwe J, Zeiger JS, Nanda A, Cooke A. Exercise and fitness in the age of social distancing during the COVID-19 pandemic J Allergy Clin Immunol Pract. 2020; 8:2152–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thevarajan I, Nguyen THO, Koutsakos M, Druce J, Caly L, van de Sandt CE, et al. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat Med. 2020; 26:453–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pascarella G, Strumia A, Piliego C, Bruno F, Del Buono R, Costa F, et al. COVID-19 diagnosis and management: a comprehensive review J Intern Med. 2020Doi: 10.1111/joim.13091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olde Rikkert MGM, Vingerhoets RW, van Geldorp N, de Jong E, Maas H. Atypical clinical picture of COVID-19 in older patients Ned Tijdschr Geneeskd. 2020; 164:D5004. [PubMed] [Google Scholar]
- 8.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients J Infect. 2020; 80:e14–e18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan LF, Seetharaman S. Preventing the spread of COVID-19 to nursing homes: experience from a Singapore Geriatric Centre. J Am Geriatr Soc. 2020; 68:942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahmati-Ahmadabad S, Hosseini F. Exercise against SARS-CoV-2 (COVID-19): does workout intensity matter? (a mini review of some indirect evidence related to obesity). 2020; 19:100245.Doi: 10.1016/j.obmed.2020.100245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khaleghzadeh H, Afzalpour ME, Ahmadi MM, Nematy M, Sardar MA. Effect of high intensity interval training along with Oligopin supplementation on some inflammatory indices and liver enzymes in obese male Wistar rats with non-alcoholic fatty liver disease Obesity Medicine. 2020; 17:100177 [Google Scholar]
- 12.Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Health Sci. 2019; 8:201–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jimenez-Pavon D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people Prog Cardiovasc Dis. 2020. March 24S0033-0620(20)30063-3. Doi: 10.1016/j.pcad.2020.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Viana RB, de Lira CAB. Exergames as coping strategies for anxiety disorders during the COVID-19 quarantine period. Games Health J. 2020; 9:147–9 [DOI] [PubMed] [Google Scholar]
- 15.de Oliveira Neto L, de Oliveira Tavares VD, Schuch FB, Lima KC. Coronavirus pandemic (SARS-COV-2): Pre-Exercise Screening Questionnaire (PESQ) for telepresential exercise. Front Public Health. 2020; 8:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luzi L, Radaelli MG. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020; 57:759–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richard C, Wadowski M, Goruk S, Cameron L, Sharma AM, Field CJ. Individuals with obesity and type 2 diabetes have additional immune dysfunction compared with obese individuals who are metabolically healthy. BMJ Open Diabetes Res Care. 2017; 5:e000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russell B, Moss C, Rigg A, Van Hemelrijck M. COVID-19 and treatment with NSAIDs and corticosteroids: should we be limiting their use in the clinical setting? Ecancermedicalscience. 2020; 14:1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amici C, Di Caro A, Ciucci A, Chiappa L, Castilletti C, Martella V, et al. Indomethacin has a potent antiviral activity against SARS coronavirus. Antivir Ther. 2006; 11:1021–30 [PubMed] [Google Scholar]
- 20.Hao D, He LX, Qu JM, Pan J, Hu BJ, Zhang J, et al. [A study of pulmonary inflammatory reaction induced by N-protein of SARS-CoV in rat models and effects of glucocorticoids on it]. Zhonghua Nei Ke Za Zhi. 2005; 44:890–3 [PubMed] [Google Scholar]
- 21.Zhang X, Alekseev K, Jung K, Vlasova A, Hadya N, Saif LJ. Cytokine responses in porcine respiratory coronavirus-infected pigs treated with corticosteroids as a model for severe acute respiratory syndrome. J Virol. 2008; 82:4420–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality Aging Clin Exp Res. 2020; 32:1195–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017; 356:i6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Oliveira DL, Hirotsu C, Tufik S, Andersen ML. The interfaces between vitamin D, sleep and pain. J Endocrinol. 2017; 234:R23–36 [DOI] [PubMed] [Google Scholar]
- 25.Abdul-Razzak KK, Mayyas FA, Al-Farras MI. Vitamin D as potential antidepressant in outpatients with musculoskeletal pain. Int J Clin Pharmacol Ther. 2018; 56:400–10 [DOI] [PubMed] [Google Scholar]
- 26.Wu Z, Malihi Z, Stewart AW, Lawes CM, Scragg R. The association between vitamin D concentration and pain: a systematic review and meta-analysis. Public Health Nutr. 2018; 21:2022–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cui C, Xu P, Li G, Qiao Y, Han W, Geng C, et al. Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: role of renin-angiotensin system. Redox Biol. 2019; 26:101295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Middleton A, Simpson KN, Bettger JP, Bowden MG. COVID-19 pandemic and beyond: considerations and costs of telehealth exercise programs for older adults with functional impairments living at home-lessons learned from a pilot case study Phys Ther. 2020Doi: 10.1093/ptj/pzaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]


