Abstract
Lung cancer is the most common cause of cancer death in the world. However, recent studies have found that patients with pulmonary ground-glass opacity (GGO) have a better prognosis. Considering its low invasiveness, sublobar resection may be an appropriate treatment of choice. Low-dose computed tomography (CT) is recommended for the high-risk groups of lung cancer. Patients with nonsolid nodule are suggested to take annual low dose CT following-up. For part-solid or solid nodules, the solid component size less or more than 8 mm is the watershed of surgical treatment. Increasing tumor size is a hint of malignancy. Biopsy can be performed for clinically highly suspected malignant nodules. The endobronchial ultrasound biopsy, CT-guide biopsy, or surgical excision are the mainstream for the diagnosis of lung nodules. But for treatment, the sublobar resection is the mainstream of pulmonary GGO. A precise localization technique makes surgeons get enough resection margin and preserve more pulmonary function of the patients. The different localization technique is suitable for different kind nodular position. For patients with pure pulmonary GGO, annual low dose CT checkup is suitable. If the tumor size or solid part of the tumors increased gradually, adequate sublobar resection after tumor localization technique may provide good prognosis and preserve more pulmonary function of the patients.
Keywords: Chest computed tomography, Ground Glass Opacity, Lung cancer, Screening
1. INTRODUCTION
Lung cancer is the most common cause of cancer death in the world, causing approximately 1.6 million deaths each year.1 With the development of low-dose computer tomography (CT), more and more people are being screened for lung cancer in anticipation of early diagnosis.2 Studies revealed that the main risk factors affecting lung cancer are air pollution and smoking.1,3 However, other studies presented that women and Asian ethnic groups are also risk factors for lung cancer.3,4 The standard treatment for early lung cancer is lobectomy plus radical lymph node dissection.5 However, recent studies have found that lung cancer with ground-glass component has a better prognosis.6–8 Many studies believe that the treatment of ground-glass opacity (GGO) should be different from traditional lobectomy.6,8 Considering its low invasiveness, sublobar resection or even observation are appropriate treatment methods.5,9,10 For this lung cancer with a good prognosis, there should be a review to unify its screening, diagnosis, and treatment.
2. SCREENING
In the National Comprehensive Cancer Network (NCCN) guideline, it is recommended that high-risk groups of lung cancer undergo low-dose chest computed tomography (CT) for early screening.11 Among them, smoking history is one of the most influential risk factors. People with a history of smoking for more than 20 pack-year will be classified as a high-risk group and recommended to undergo a low dose CT test.11 In addition to smoking, second-hand smoke, air pollution, work environment, family history, etc. are also risk factors for lung cancer.11 People with multiple risk factors should undergo lung cancer screening for early detection. In CT examination, these nodules can be divided into three categories: nonsolid nodule, part-solid nodule, and solid nodule according to their GGO component (Fig. 1). Nonsolid nodule represents 100% GGO component. Since the pathological types of these patients are mostly low-invasive lung adenocarcinomas such as adenocarcinoma in situ, minimally invasive adenocarcinoma, or lepidic-predominant adenocarcinoma, NCCN guideline recommends that nonsolid nodule less than 2 cm be subject to annual low dose CT following-up.11 For nonsolid nodule larger than 2 cm, it is recommended to receive another CT after 6 months. If the nodule disappeared or stable, it should be checked once a year; if the tumor volume increases or changes into a part-solid nodule, it is recommended to accept biopsy or surgical excision.11 Screening found solid or part-solid nodule needs to check its solid component size. If the solid component size is less than 8 mm, the malignancy degree of the tumor is low and it is recommended to perform CT follow-up after 3–6 months. If the Solid component is greater than 8 mm, it is recommended to undergo further Positron emission tomography(PET)/CT examination to clarify the need for sectioning or surgical resection.11 If PET/CT is suspected of being highly malignant, or following CT scan shows that the tumor size has increased by more than 1.5 mm, it is recommended that patients undergo biopsy or surgical resection11 (Fig. 2).
Fig. 1.
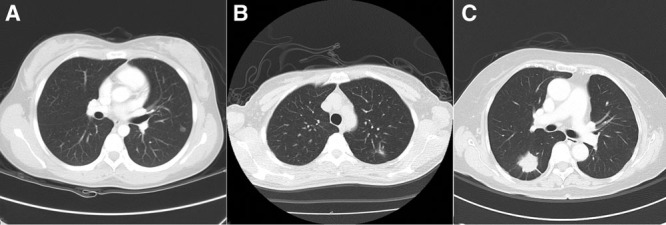
The common nodule appearance under chest computed tomography. (A) Nonsolid nodule over left upper lobe; (B) part-solid nodule over left lower lobe; C: Solid nodule over right lower lobe.
Fig. 2.
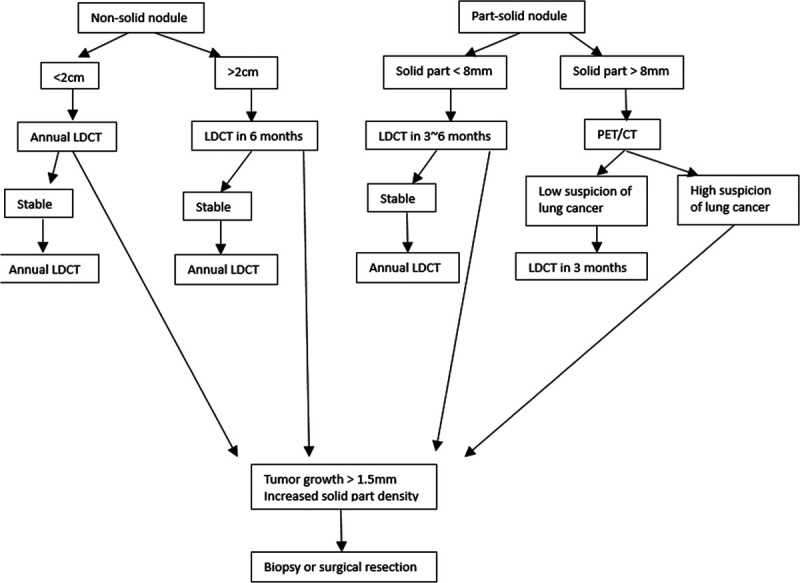
Nonsolid and part-solid nodule screening protocol. LDCT, low-dose computed tomography; PET/CT, positron emission tomography/computed tomography (Adapted from National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology, Lung Cancer Screening, Version 1 2020).
3. DIAGNOSIS
Lung nodules may be infection, benign nodules, intrapulmonary lymph nodes, or malignant tumors.7 Different types of nodules have different treatment methods, and correct diagnosis is important for clinical treatment. Clinically, low-malignant nodules can be treated with conservative treatment of regular CT follow-up. If the nodules are increased in size or solid component, more invasive therapy is suggested.11 Infections, benign nodules, and intrapulmonary lymph nodes often resolve or become stationary after regular follow-up. It is recommended to take biopsy for nodules that are clinically suspected of high malignancy or found to increase in size after follow-up.11 Fukui et al. reported that there was no difference in the pathological stage between patients who had surgery at the beginning and those who had surgery after the tumor size increased.10 For clinical stage IA lung cancer, patients do not need to worry about follow-up leads to tumor progression.12
The current diagnostic methods for pulmonary nodules are mainly divided into the following: (1) Endobronchial ultrasound (EBUS) biopsy, (2) CT-guide biopsy, and (3) surgical excision. The pooled sensitivity of real-time EBUS in lung cancer is 90% but the false-negative rate is 20%.13 EBUS has a higher diagnosis rate for nodules near the bronchial wall, but a lower diagnosis rate for peripheral type nodule.13 Shimizu reported that the accuracy rate of CT-guide biopsy for small pulmonary nodules is about 64.6%, and it has a higher diagnosis rate (75.6%) for solid-dominant lesions.14 CT-guide biopsy has less discomfort than EBUS biopsy. However, patients need to receive more radiation exposure, and the diagnosis rate of central type nodules is lower.13,14 Surgical excision has the highest diagnosis rate, but it is accompanied by the cost of pulmonary function decreasing and longer recovery period. It is not recommended to use surgical excision as a diagnostic tool for nodules with low clinical malignancy. However, Huang et al. reported that for patients with stage-I lung cancer, preoperative biopsy may increase the risk of tumor recurrence.15 For clinical nodules with high malignancy, direct surgical resection is also a suitable treatment method. Patients can discuss the malignancy of nodules with clinicians and choose proper treatment strategies such as regular CT follow-up, biopsy, or surgical resection.
4. TREATMENT
Patients who are clinically highly suspected or diagnosed as early lung cancer are recommended to receive surgical treatment.5 According to the NCCN guideline, the standard treatment for lung cancer is lobectomy plus radical lymph node dissection.5
However, in recent years, there have been many research reports that the nodules with GGO component have low malignancy and low lymph node metastasis rate.6–8,16,17 For low-grade malignant GGO, lobectomy plus radical lymph node dissection do not provide a better prognosis, on the contrary, it loses more pulmonary function and has a higher complication rate.9,16–19 The current NCCN guideline recommends that if the patient’s nodules are less than 2 cm and meet one of the following conditions: (1) pure adenocarcinoma in situ histology, (2) GGO component is greater than 50%, and (3) tumor doubling time is greater than 400 days, patient can consider taking sublobar resection (segmentectomy or wedge resection).5
Sublobar resection requires a balance between preserving pulmonary function and achieving safe resection margin.5 It is clinically recommended that the safety margin should be more than the nodule size or at least 2 cm.5 In order to achieve a better safety margin and retain more lung function, it is important to accurately locate the tumor. Traditionally, the surgeon used visual and finger touch to determine the location of the tumor. However, vision and touch may be interfered by normal lung tissues, such as vessels, bronchus, and lymph nodes, resulting in a decrease in the diagnosis rate (54% failure rate).20 Difficult precise localization often leads to patients having to sacrifice larger lung tissue or even operation failure. To improve the localization technology, in recent years, scholars have successively published bronchoscopy-guide localization, ultrasound localization, CT-guide localization, and electromagnetic navigation bronchoscopy (ENB) localization technology.21 The materials used for localization include methylene blue dye, hook wire, and mircocoil.
Methylene blue dye localization is to inject the dye near the lesion, and the surgeon can directly observe the lesion in video-assisted thoracoscopic surgery (VATS) and perform surgical resection.21 After localization, the patient had only slight discomfort, but as time passes, the dye will gradually spread and make the localization effect worse.21 Meanwhile, methylene blue dye will also stain the tumor, making it difficult to differentiate the tumor margin from normal lung parenchyma grossly. Hook wire localization needs to puncture the hook wire from the chest wall to the lesion. After localization, the patient must maintain a fixed posture until the operation. Although the patient has a high degree of discomfort, the surgeon can directly find the hook wire and remove the lesion during VATS operation. Microcoil localization has less discomfort than hook wire. However, fluroscopic guidance is needed to determine the location of the lesion during VATS operation.22
The bronchoscopy-guide technique can only use bronchoscopy to inject methylene blue dye to locate the lesion. Patients need to receive bronchoscopy-guide localization before surgery, and this technique is only suitable for central type nodules. Ultrasound localization can use methylene blue, hook wire, and microcoil material for localization. However, it is mainly performed in peripheral nodules, and it is less effective for nodule localization with GGO-predominant nodules.23 CT-guide localization is divided into CT room localization and Hybrid room localization.21 CT room localization needs to be done in the CT room, while hybrid room localization is done in the hybrid operation room. Patients have a short waiting time in hybrid room localization, but because of the limitations of equipment, hybrid room localization technology has not been popularized.21,22 CT-guide localization can use methylene blue dye, hook wire, and microcoil material for localization. ENB localization needs to receive electromagnetic localization before surgery. Real-time localization is an advantage of this technique. According to the location of the nodules and the habits of clinicians, different nodules are suitable for different localization methods.21,22 It is up to the surgeon to decide which localization method the patient needs to accept (Table 1).
Table 1.
Localization technology, suitable location and materials
| Technique | Suitable location | Materials |
|---|---|---|
| Bronchoscopy-guide | Central | Methylene blue dye |
| Ultrasound | Peripheral | Methylene blue dye, hook wire, microcoil |
| CT-guide | Central, peripheral | Methylene blue dye, hook wire, microcoil |
| ENB | Central, peripheral | Methylene blue dye, hook wire, microcoil |
Central: inside two-third of lung parenchyma; peripheral: outside one-third of lung parenchyma; ENB = electromagnetic navigation bronchoscopy.
In addition to tumor resection, lymph node dissection is also an important part of lung cancer surgery. Lymph node metastasis or not affects the stage and treatment of lung cancer.5,24 Accurate lymph node clearance has a better prognosis for patients. Despite the PET/CT examination before surgery, it is inevitable that there will be false negatives.25 Lymph node dissection during surgery is still considered an appropriate treatment.5 However, lymph node dissection may cause complications such as chylothorax, bleeding, and nerve or blood vessel injury. Recent studies have pointed out that GGO-predominant nodules have a lower lymph node metastasis rate than solid nodule.6,16,17 Some scholars proposed GGO patients only need lymph node sampling, even need not harvest lymph nodes.6,17 GGO patients do not need to accept extended lymph node dissection has been gradually accepted by chest surgeons.16,17
Patients with poor cardiopulmonary function or unwillingness to undergo surgical resection can be treated with alternative therapies such as stereotactic body radiation therapy, chemotherapy, or target therapy.5 Although the survival rate of alternative therapy is lower than that of surgical resection for early lung cancer, patients do not need to bear the risks of wound pain, postoperative pulmonary function loss and surgical complications.5
In conclusion, GGO is regarded as the appearance of early lung cancer under chest CT. The characteristics of low invasiveness, low metastasis rate, and long tumor doubling time make these patients have a better prognosis. Tumors less than 0.8 cm or GGO-predominant nodules can be followed up for a period, without immediate surgery. In the past, lobectomy was regarded as the standard treatment for early lung cancer, but for low-invasive GGO, sublobar resection can get equal treatment results. Tumor localization technology is widely used in patients with GGO to retain more lung parenchyma and get an appropriate section margin. Nodules in different locations are suitable for different positioning methods, depending on the decision of the surgeon. GGO patients can get a good prognosis after surgical treatment, and the decline of pulmonary function is also less than traditional surgery.
Footnotes
Conflicts of interest: The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
Conflicts of interest: The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
REFERENCES
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;6587–108. [DOI] [PubMed] [Google Scholar]
- 2.Migliore M, Fornito M, Palazzolo M, Criscione A, Gangemi M, Borrata F, et al. Ground glass opacities management in the lung cancer screening era. Ann Transl Med. 2018;6:90 Doi: 10.21037/atm.2017.07.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of lung cancer: Diagnosis and management of lung cancer Chest. 2013;143(3rd ed5 Suppl):e1S–e29S.American College of Chest Physicians evidence-based clinical practice guidelines. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Groot PM, Wu CC, Carter BW, Munden RF. The epidemiology of lung cancer. Transl Lung Cancer Res. 2018;7:220–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Network NCC 2019. (Accessed June 7 2019 Available at https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf).
- 6.Matsuguma H, Yokoi K, Anraku M, Kondo T, Kamiyama Y, Mori K, et al. Proportion of ground-glass opacity on high-resolution computed tomography in clinical T1 N0 M0 adenocarcinoma of the lung: a predictor of lymph node metastasis. J Thorac Cardiovasc Surg. 2002;124:278–84. [DOI] [PubMed] [Google Scholar]
- 7.Seidelman JL, Myers JL, Quint LE. Incidental, subsolid pulmonary nodules at CT: etiology and management. Cancer Imaging. 2013;13:365–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hattori A, Matsunaga T, Takamochi K, Oh S, Suzuki K. Importance of ground glass opacity component in clinical stage IA radiologic invasive lung cancer. Ann Thorac Surg. 2017;104:313–20. [DOI] [PubMed] [Google Scholar]
- 9.Altorki NK, Yip R, Hanaoka T, Bauer T, Aye R, Kohman L, et al. Sublobar resection is equivalent to lobectomy for clinical stage 1A lung cancer in solid nodules. J Thorac Cardiovasc Surg. 2014;147754–62. [DOI] [PubMed] [Google Scholar]
- 10.Fukui M, Suzuki K, Matsunaga T, Oh S, Takamochi K. Surgical intervention for ground glass dominant lesions: observation or outright resection? Jpn J Clin Oncol. 20171–6. Doi: 10.1093/jjco/hyx053. [DOI] [PubMed] [Google Scholar]
- 11.Network NCC Lung Cancer Screening Version1.2020. NCCN.org, 2020. (Accessed May 14 2019, Available at https://www.nccn.org/professionals/physician_gls/pdf/lung_screening.pdf).
- 12.Walter JE, Heuvelmans MA, Yousaf-Khan U, Dorrius MD, Thunnissen E, Schermann A, et al. New subsolid pulmonary nodules in lung cancer screening: The NELSON Trial. J Thorac Oncol. 2018;13:1410–4. [DOI] [PubMed] [Google Scholar]
- 13.Anantham D, Koh MS, Ernst A. Endobronchial ultrasound. Respir Med. 2009;103:1406–14. [DOI] [PubMed] [Google Scholar]
- 14.Shimizu K, Ikeda N, Tsuboi M, Hirano T, Kato H. Percutaneous CT-guided fine needle aspiration for lung cancer smaller than 2 cm and revealed by ground-glass opacity at CT. Lung Cancer. 2006;51:173–9. [DOI] [PubMed] [Google Scholar]
- 15.Huang CS, Hsu PK, Chen CK, Yeh YC, Chen HS, Wu MH, et al. Preoperative biopsy and tumor recurrence of stage I adenocarcinoma of the lung. Surg Today. 2019. Doi: 10.1007/s00595-019-01941-3. [DOI] [PubMed] [Google Scholar]
- 16.Flores RM, Nicastri D, Bauer T, Aye R, Andaz S, Kohman L, et al. Computed tomography screening for lung cancer: mediastinal lymph node resection in stage IA nonsmall cell lung cancer manifesting as subsolid and solid nodules. Ann Surg. 2017;265:1025–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin YH, Chen CK, Hsieh CC, Hsu WH, Wu YC, Hung JJ, et al. Lymphadenectomy is unnecessary for pure ground-glass opacity pulmonary nodules. J Clin Med. 2020;9 Doi: 10.3390/jcm9030672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fan J, Wang L, Jiang GN, Gao W. Sublobectomy versus lobectomy for stage I non-small-cell lung cancer, a meta-analysis of published studies. Ann Surg Oncol. 2012;19:661–8. [DOI] [PubMed] [Google Scholar]
- 19.Lardinois D, De Leyn P, Van Schil P, Porta RR, Waller D, Passlick B, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg. 2006;30:787–92. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki K, Nagai K, Yoshida J, Ohmatsu H, Takahashi K, Nishimura M, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest. 1999;115:563–8. [DOI] [PubMed] [Google Scholar]
- 21.Lin MW, Chen JS. Image-guided techniques for localizing pulmonary nodules in thoracoscopic surgery. J Thorac Dis. 2016;8(Suppl 9):749–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hung CT, Chen CK, Chang YY, Hsu PK, Hung JJ, Huang CS, et al. Electromagnetic navigation-guided versus computed tomography-guided percutaneous localization of small lung nodules before uniportal video-assisted thoracoscopic surgery: a propensity score-matched analysis. Eur J Cardiothorac Surg. 2020. Doi: 10.1093/ejcts/ezz338. [DOI] [PubMed] [Google Scholar]
- 23.Santambrogio R, Montorsi M, Bianchi P, Mantovani A, Ghelma F, Mezzetti M. Intraoperative ultrasound during thoracoscopic procedures for solitary pulmonary nodules. Ann Thorac Surg. 1999;68:218–22. [DOI] [PubMed] [Google Scholar]
- 24.Naruke T, Goya T, Tsuchiya R, Suemasu K. The importance of surgery to non-small cell carcinoma of lung with mediastinal lymph node metastasis. Ann Thorac Surg. 1988;46:603–10. [DOI] [PubMed] [Google Scholar]
- 25.Cerfolio RJ, Ojha B, Bryant AS, Raghuveer V, Mountz JM, Bartolucci AA. The accuracy of integrated PET-CT compared with dedicated PET alone for the staging of patients with nonsmall cell lung cancer. Ann Thorac Surg. 2004;781017–23. [DOI] [PubMed] [Google Scholar]


