Abstract
The rapid surge and wide spread of the coronavirus disease-2019 (COVID-19) overshadows the entire medical industries worldwide. The stringent medical resources hinder the diagnostic capacity globally, while 84 000 of new cases confirmed within a single day of April 14, 2020. Real-time reverse-transcription polymerase chain reaction (RT-PCR) with is the current first-line diagnosis, but the false-negative rate remains concerned. Radiographic technologies and tools, including computed tomography (CT) and chest X-ray, were applied for initial screening and follow-up, from which the tools provide detail diagnosis with specific pathologic features for staging and treatment arrangement. Although the radiographic imaging is found less sensitive, numerous CT-positive patients were not screened out by RT-PCR initially and later confirmed as COVID-19 positive. Besides, the shortage of sampling kits and the longer turn-over time of PCR examinations in some areas were noticed due to logistic issues and healthcare burden. In this review, we will discuss the challenges and the future perspectives of using radiographic modalities for COVID-19 diagnosis in view of securing human lives amid the crisis.
Keywords: Chest X-ray, Computed tomography, Coronavirus disease-2019, Radiographic technologies
1. INTRODUCTION
Starting from December of 2019, the symptomatic SARS-CoV-2 virus rapidly overshadows the entire world, causing global economic and epidemic crises. By far, the confirmed number of cases has reached 1.8 million, and the death toll has passed 111 thousand lives as of April 14, 2020.1 This pandemic has revealed various challenges across the globe particularly for the escalating spreading. Real-time reverse-transcription polymerase chain reaction (rRT-PCR) is the current first-line diagnostic measure, accompanied with computed tomography (CT) or chest radiography (CXR) for symptomatic staging and treatment arrangement.2 Despite the recent release from American College of Radiography does not recommend the use CT or CXR for coronavirus disease-2019 (COVID-19) confirmation,3 the debate continues as the diagnostic capacity in developing countries may not reach certain level comparing to well-developed countries, suffering from the shortage of examination kits and the long turn-over time in PCR tests.4 Thus, this review intends to illustrate an overview of the diagnostic value of CT, CXR, and additional modalities against COVID-19.
2. THE USE OF CT IMAGING IN THE DIAGNOSIS OF COVID-19
Within a month after the COVID-19 being declared infectious, the clinical and imaging features of COVID-19 in CT have been characterized correspondingly.5 Fever, cough, and shortness of breath in the later stage were widely observed pathologically. Diversified flu-like symptoms were documented, including sputum production, fatigue, and sore throat.5–8 Initially, CXR was deployed for quick screening in response to the overcrowded emergency room. The common pathologic patterns of CXR are pulmonary infiltration and consolidation at the lower regions bilaterally.9 In terms of CT imaging findings, ground-glass opacity (GGO) is an indicative feature that was initially used for diagnosis in the early stage of symptomatic patients.5 Consolidation, referring to the signs of pathological fluids or tissues in the pulmonary parenchyma, is documented with varied occurrence rates, considerably relating to the progress of the disease.10 Bilateral involvement and multifocal pathogenesis were found in over 50% of the patients with COVID-19.11–13 Other imaging features were also documented while the patterns are lack of correlation with the diagnosis, for example, reticular pattern, crazy paving, and air bronchogram, etc.14,15
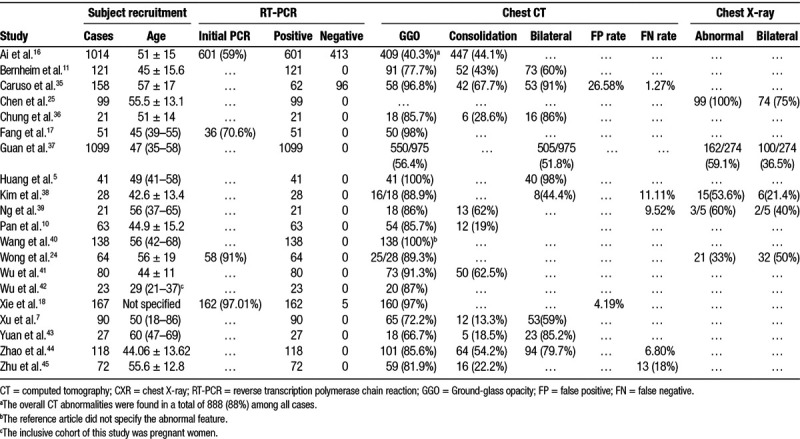
An article published by Ai et al. in late February claimed an 88% accuracy of CT diagnosis overpowered the 59% using RT-PCR in a cohort of 1014 patients.16 In early February, a series of reports suggest the use of CT image in addition to the swab-PCR test, due to the possible false-negative rate in PCR tests. Fang et al. reported that 50 out of 51 patients were diagnosed by CT whereas only 36 out of 51 were detected with SARS-CoV-2 from the PCR.17 Apart from this, Xie et al evaluated a total of 167 patients, of which 5 patients were tested negative by PCR but found positive in CT images.18 A 2- to 7-day delay of PCR detection was found by repeating swab sampling, suggesting a very limited virus titer during the disease early-onset or latent period. Xu et al. showed three cases with initial PCR negative with pathological features in CT screening.19 Feng et al. later reported a case with consecutive four negative PCR tests but found patchy and GGO in the initial CT imaging.20 In addition to the false-negative rate of swab testing, the severity of COVID-19 is inconclusive in the absence of imaging results. The discrepancies in the timing of using radiography were noticed among different countries. The University of Washington, who had the most confirmed cases in the USA by mid-March, implied a policy to only screen patients infected with COVID-19 with positive PCR results. The major concerns are the stringent of personal protective equipment and the risk of cross-contamination of staff and other non-COVID-19 patients sharing the imaging facilities.21 Meanwhile, a response from ASST Fatebenefratelli Sacco in Milan, Italy, decided to screen all symptomatic patients with imaging and discharged patients without pathological findings for quarantine to ease the burden of medical resources.22 This could be a major challenge against the healthcare system as well as resilience in response to such surge crisis.23 In spite of the uncertainty from PCR tests, the use of CT scan for screening is still debatable as the turnover time could be costly for repeated sanitizing, and the increased risk of aerosol spreading during the transportation, imaging, and possibly ventilation of patients. A recent retrospective study in Hong Kong evaluated the diagnostic value using CXR. In a total of 64 patients with COVID-19, Wong et al. revealed that the CXR screening only had 69% sensitivity comparing to 91% initial PCR testing; however, 6 (9%) abnormal CXR cases were initially tested negative by PCR.24 The conundrum at the current situation is that all diagnostic tools have their blind spots and the triage, organization, logistic, and the capacity of healthcare system making the establishment of guidelines varied from regions to regions. Table 1 collected numerous studies to allow an overview among diversified results in CT diagnosis, while most of the study did not specify the false-negative rate of initial RT-PCR tests. Four out of the 20 included studies showed a 100% or better diagnostic outcomes using chest CT than RT-PCR, and the GGO is dominant among other radiographic features. Although most of the CXR were unable to be conclusive for the disease onset, plenty of the studies implied the usefulness in follow-up cases rather than the excessive radiation dose of CT scans. Only one study by Chen et al. published in early February when the diagnostic guidelines had not been issued by authorities, claiming the 100% accuracy using CXR.25 The scenario could be the overload of the healthcare system in Hubei Province during the sudden escalating of confirmed cases. Patient admission was limited to a severe or advanced stage that certain symptoms had worsened. Other than that, the use of CXR can barely reach 50% in most presented studies. Given the fluctuating sensitivity and specificity of RT-PCR across studies, the general findings still support that RT-PCR is more consistent in COVID-19 diagnosis. CT imaging is not recommended for assessing patients with mild or no symptoms when admission in various statements, including Fleischner Society.26,27 The radiographic imaging may be beneficial in moderate to severe case-patients; moreover, the imaging can be move to front line when the medical resources are limited.
Table 1.
Summary of COVID-19 diagnosis using RT-PCR, CT, and CXR.
3. PERSPECTIVES OF THE USE OF CT IMAGING IN PATIENTS WITH COVID-19
For most patients confirmed with COVID-19, the battle continues to an average period of 3–4 weeks until discharged.28 Since the RT-PCR only answers the true-or-false question confirming the diagnosis of COVID-19, question, the progress of disease mainly relies on the imaging modalities. CT, of its advantages, provides full coverage of region-of-interests and detailed information;29 however, the overwhelming radiation dose as well as the sanitizing procedures discourage its application. CXR becomes more reasonable when portable X-ray tubes are equipped. The machine can be exclusively used in COVID-19 ward, and the fewer patient transportation further secures the disease control. The reliability of CXR was reported by Chen et al. where they recruited hospitalized patients using CXR.25 In addition to follow-up, the CT image may be concluded by quantitative CT score for prognostic use.30 To the extent of artificial intelligence, elevating studies have been initiated to conduct machine learning and fast screening on a radiomics basis.31–33 On top of it, a reputational computer science campaign, Hackathon, recently announce their highlighted projects regarding the COVID-19 research. MedCheX is honored by the competition with an automatic, high-throughput, and computational screening over CXR for COVID-19 diagnosis.34 Yet this pandemic circumstance continues, the development of machine learning and artificial intelligence-mediated quick screening may ameliorate the contribution of radiographic imaging in the combat against COVID-19.
ACKNOWLEDGMENTS
This study was funded by Taipei Veterans General Hospital (V108D46-004-MY2-1, V108E-006-4), Taiwan; the Shenzhen Basic Research Funding Scheme (JCYJ20170818103614207), Science and Technology Innovation Commission of Shenzhen Municipality, China.
Footnotes
Conflicts of interest: The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
REFERENCES
- 1.World Health Organization. Coronavirus disease (COVID-19) pandemic. Available at <https://www.who.int/emergencies/diseases/novel-coronavirus-2019> 2020.
- 2.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020200370 Doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Radiology. ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. Available at <https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection> 2020.
- 4.Shi H, Han X, Cao Y, Alwalid O, Zheng C. CT screening for early diagnosis of SARS-CoV-2 infection – authors’ reply. Lancet Infect Dis 2020. Doi: 10.1016/S1473-3099(20)30247-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao D, Yao F, Wang L, Zheng L, Gao Y, Ye J, et al. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis 2020. Doi:10.1093/cid/ciaa247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020;47:1275–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol 2020. Doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodrigues JCL, Hare SS, Edey A, Devaraj A, Jacob J, Johnstone A, et al. An update on COVID-19 for the radiologist – A British Society of Thoracic Imaging Statement. Clin Radiol 2020;75:323–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol 2020. Doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology 2020200463 Doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol 2020;21:494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu YH, Dong JH, An WM, Lv XY, Yin XP, Zhang JZ, et al. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect 2020;80:394–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol 2020. Doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020295:18 Doi: 10.1148/radiol.2020200236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020;200642 Doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 2020;200432 Doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 2020;200343 Doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu J, Wu R, Huang H, Zheng W, Ren X, Wu N, et al. Computed tomographic imaging of 3 patients with coronavirus disease 2019 pneumonia with negative virus real-time reverse-transcription polymerase chain reaction test. Clin Infect Dis 2020. Doi: 10.1093/cid/ciaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng H, Liu Y, Lv M, Zhong J. A case report of COVID-19 with false negative RT-PCR test: necessity of chest CT. Jpn J Radiol 2020. Doi: 10.1007/s11604-020-00967-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mossa-Basha M, Medverd J, Linnau K, Lynch JB, Wener MH, Kicska G, et al. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington. Radiology 2020;201326 Doi: 10.1148/radiol.2020201326. [DOI] [PubMed] [Google Scholar]
- 22.Orsi MA, Oliva AG, Cellina M. Radiology department preparedness for COVID-19: facing an unexpected outbreak of the disease. Radiology 2020;201214 Doi: 10.1148/radiol.2020201214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peiffer-Smadja N, Lucet JC, Bendjelloul G, Bouadma L, Gerard S, Choquet C, et al. Challenges and issues about organising a hospital to respond to the COVID-19 outbreak: experience from a French reference centre. Clin Microbiol Infec 2020. Doi: 10.1016/j.cmi.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology 2019;201160 Doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Chest 2020. Doi: 10.1016/j.chest.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology 2020;201365 Doi: 10.1148/radiol.2020201365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology 2020;200843 Doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duan YN, Qin J. Pre- and posttreatment chest CT findings: 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 202029521 Doi: 10.1148/radiol.2020200323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang G, Gong T, Wang G, Wang J, Guo X, Cai E, et al. Timely diagnosis and treatment shortens the time to resolution of coronavirus disease (COVID-19) pneumonia and lowers the highest and last CT scores from sequential chest CT. AJR Am J Roentgenol 2020; 1–7. Doi: 10.2214/AJR.20.23078. [DOI] [PubMed] [Google Scholar]
- 31.Alimadadi A, Aryal S, Manandhar I, Munroe PB, Joe B, Cheng X. Artificial intelligence and machine learning to fight COVID-19. Physiol Genomics 2020;52:200–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li L, Qin L, Xu Z, Yin Y, Wang X, Kong B, et al. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology 2020200905 Doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santosh KC. Ai-driven tools for coronavirus outbreak: need of active learning and cross-population train/test models on multitudinal/multimodal data. J Med Syst 2020;4493 Doi: 10.1007/s10916-020-01562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.An e-alert system for automatically detecting pneumonia from chest X-rays. Available at <https://covidglobalhackathon.com/projects/medchex> 2020.
- 35.Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT features of COVID-19 in Rome, Italy. Radiology 2020201237 Doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020;295:202–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guan CS, Lv ZB, Yan S, Du YN, Chen H, Wei LG, et al. Imaging features of coronavirus disease 2019 (COVID-19): evaluation on thin-section CT. Acad Radiol 2020. Doi: 10.1016/j.acra.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim ES, Chin BS, Kang CK, Kim NJ, Kang YM, Choi JP, et al. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean cohort study on COVID-19. J Korean Med Sci 202035:e142 Doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng MY, Lee EY, Yang J, Yang F, Li X, Wang H, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiology: Cardiothoracic Imaging 2020;2:e200034 Doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020. Doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu J, Wu X, Zeng W, Guo D, Fang Z, Chen L, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol 2020;55:257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu X, Sun R, Chen J, Xie Y, Zhang S, Wang X. Radiological findings and clinical characteristics of pregnant women with COVID-19 pneumonia. Int J Gynaecol Obstet 2020. Doi: 10.1002/ijgo.13165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yuan M, Yin W, Tao Z, Tan W, Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS ONE 2020;15e0230548 Doi: 10.1371/journal.pone.0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhao W, Zhong Z, Xie X, Yu Q, Liu J. CT scans of patients with 2019 novel coronavirus (COVID-19) pneumonia. Theranostics 2020;10:4606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhu T, Wang Y, Zhou S, Zhang N, Xia L. A comparative study of chest computed tomography features in young and older adults with corona virus disease (COVID-19). J Thorac Imaging 2020. Doi: 10.1097/RTI.0000000000000513. [DOI] [PMC free article] [PubMed] [Google Scholar]


