Abstract
This study examines: (1) the association between the neighborhood social environment and obesity among adolescents, (2) whether physical activity, screen time, and short sleep mediates this association, and (3) examine sex differences. Participants (n=12,692; age 11-19 years old) came from Waves I and II of the National Longitudinal Study of Adolescent to Adult Health. Neighborhood social disorganization and socioeconomic status (NSES) measures were associated with obesity adjusting for sex, race, age, parental education, and urbanicity. Screen time mediated NSES and obesity. Very short sleep duration (<6 hours) mediated social disorganization and obesity among females only. Findings suggest improving neighborhood social conditions may reduce the risk for obesity.
Keywords: pediatric obesity, sleep, exercise, screen time, social environment
Introduction
Obesity has been linked to poorer health outcomes and remains prevalent among adolescents with approximately 1 in 5 children between the ages of 6 to 19 years old having obesity (Ogden et al., 2015). Several studies have explored the built environment as a contributor to adolescent obesity, but few studies have examined the neighborhood social context as a determinant of obesity (Suglia et al., 2016). Based on prior conceptualization by Diez-Roux et al., the neighborhood social environment encompasses the sociodemographic characteristics and “the degree and nature of social connections between neighbors, the presence of social norms, levels of safety and violence, and various features of the social organization” of a neighborhood (Diez Roux and Mair, 2010). Studies focusing on the social environment among adolescents have mainly examined measures of neighborhood socioeconomic status (SES) and found that living in worse neighborhood social economic conditions is associated with greater obesity (Alvarado, 2016; Carter and Dubois, 2010; Franzini et al., 2009; Greves Grow et al., 2010; Singh et al., 2010). For instance, a study of adolescents using data from the 1979 National Longitudinal Survey of Youth found that living in more socioeconomically disadvantaged neighborhoods measured by education, income, and occupation could increase the odds of obesity by 40% (Alvarado, 2016). In addition, neighborhood SES is correlated with other features of the social environment including social disorganization that may be linked to obesity (Suglia et al., 2016). For instance, studies on measures of neighborhood social disorganization, such as crime, perceived safety, and lack of social cohesion, have found associations between these neighborhood factors and obesity among adolescents (Borrell et al., 2016; Carrillo-Álvarez et al., 2019; Cecil-Karb and Grogan-Kaylor, 2009; Chaparro et al., 2018).
Health behaviors, including physical activity, sedentary behaviors and sleep, may be driving the associations between the neighborhood social environment and obesity. Neighborhoods of lower socioeconomic status have less access to parks, recreational facilities, and sidewalks, which can influence health behaviors (e.g. physical activity and sedentary behavior) related to increase risk for obesity (Suglia et al., 2016). In addition, living in socially disorganized neighborhoods characterized by lack of safety, low social cohesion, and weak social networks may act as a stressor that lead to poor coping behaviors that include both physical inactivity and sedentary behavior increasing the risk for obesity among adolescents (Borrell et al., 2016; Lumeng et al., 2006; Theall et al., 2019; Veitch et al., 2012a). Prior studies support these hypotheses as they have found that physical inactivity and sedentary behavior mediated the association between the measures of neighborhood social disorganization (e.g. neighborhood safety, collective efficacy, and disorder) and obesity among adolescents (Franzini et al., 2009; Tu et al., 2016). A less studied health behavior that may link the neighborhood social environment and obesity is sleep duration as it is plausible that living in a stressful neighborhood social environment could alter sleep duration patterns that in turn contribute to a higher risk for obesity.
Sleep duration is particularly important to study among adolescents as the Centers for Disease Control and Prevention reported approximately 72.7% of U.S high school students had short sleep duration (<8 hours of sleep) (Wheaton et al., 2018). Prior studies have demonstrated that the neighborhood disorganization such as social fragmentation (Bagley et al., 2016; Pabayo et al., 2014) and socioeconomic deprivation (Bagley et al., 2016; Street et al., 2018; Watson et al., 2016) are associated with shorter sleep duration among adolescents. Mechanisms driving these associations could be due to greater exposure to neighborhood stressors such as environmental noise and violence related to neighborhood disadvantage that can lead to hypervigilance and distress resulting in the release of stress hormones that impair sleep (Singh and Kenney, 2013; Troxel et al., 2017). In addition, neighborhoods of lower SES have limited access to health promoting features (e.g. sidewalks, recreational facilities, and healthy foods) that support healthy behaviors (e.g. physical activity and less sedentary behavior) shown to promote sleep (Hale and Guan, 2015; Singh and Kenney, 2013; Sophie and Manuel, 2018). Mechanisms linking physical activity to sleep duration is that increased physical activity reduces anxiety and depressive symptoms and improves thermoregulation of the body that are all beneficial for sleep (Lubans et al., 2016; Youngstedt, 2005). Also, greater screen time is related to delayed bedtime, psychological arousal, and increased exposure to blue light that are all detrimental to sleep (Hale et al., 2018). Furthermore, previous prospective studies have consistently shown that shorter sleep duration increases the risk of obesity by 30% among adolescents (Miller et al., 2018). The underlying biological mechanisms include short sleep duration leading to increases in appetite (e.g. increase in ghrelin and decrease in leptin) and decreases in metabolism (e.g. insulin resistance, increases in cortisol, and decrease in thyroid stimulating hormones) that all contribute to energy imbalance increasing the risk for obesity (Duraccio et al., 2019; Miller et al., 2018). However, studies have not formally investigated whether sleep duration is a mediator in the relationship between the neighborhood social environment and obesity in adolescents. Moreover, studies have not examined whether physical activity and screen time mediate the association between the neighborhood environment and obesity through sleep duration.
Prior evidence suggests that the impact of exposure to an accumulation of neighborhood stressors on health among adolescents may be more important than single neighborhood exposures (Evans et al., 2013; Singh and Kenney, 2013; Singh et al., 2010; Theall et al., 2012). Data from the 2007 National Survey of Children’s Health indicated that living in higher cumulative risk neighborhoods characterized by greater disorganization such as lack of perceived safety, poor housing, presence of litter, and vandalism were associated with adolescent obesity (Theall et al., 2012). Yet, most studies among adolescents have examined these neighborhood social characteristics separately as risk factors for obesity, but few have focused on the cumulative impact of these various aspects of the neighborhood social environment. A study conducted in Baltimore found that living in neighborhoods with greater psychosocial hazards was associated with obesity among older adults. This cumulative measure of the neighborhood social environment was measured with the Neighborhood Psychosocial Hazards (NPH) scale that captures neighborhood economic deprivation, physical disorder, and social disorganization (Glass et al., 2006). These findings suggests the importance of examining cumulative neighborhood risk on obesity among adults, but whether this association exists among adolescents remains understudied.
Adolescence is a critical developmental period in which the health status and behaviors formed could profoundly shape the health status and behaviors during adulthood. Obesity among adolescents has been linked to poorer mental health (Rankin et al., 2016), bullying (Pont et al., 2017), lower engagement in physical activity (Sundar et al., 2018), and other health conditions such as asthma (Forno and Celedon, 2017). In addition, prior studies have demonstrated that sleep behaviors and obesity during adolescence is predictive of sleep behaviors (Maslowsky and Ozer, 2014) and obesity during adulthood (Ward et al., 2017). Furthermore, one study has found that the neighborhood social environment during adolescence was linked to obesity during adulthood (Lippert, 2016). Therefore, it is important to investigate risk factors in the pathway linking the neighborhood social environment and obesity during adolescence. Identifying these risk factors can inform the development of interventions to prevent obesity during adolescence and eventually obesity during adulthood.
The purpose of this study was to investigate the cumulative impact of various aspects of the neighborhood social environment on obesity among adolescents. Moreover, this study examined simultaneously whether physical activity, screen time, and short sleep duration mediated this association. Specifically, the study tested four mediation pathways in the associations between neighborhood SES and social disorganization with obesity that included mediation by: (1) physical activity, (2) screen time, (3) short sleep duration, and (4) physical activity and screen time via short sleep duration. Furthermore, we examined whether these associations varied by sex as prior studies suggest that both the association between the neighborhood social environment and obesity (Alvarado, 2016; Singh et al., 2010) and the relationship between sleep and obesity (Knutson, 2005; Lytle et al., 2011; Suglia et al., 2014) may differ between males and females. We hypothesized that living in a poorer neighborhood social environment was associated with obesity and that physical activity, screen time, and short sleep duration will account for some, but not all, of the association given that other health behaviors such as diet may be another mediator in the pathway not included in this study.
Methods
Study Population
Participants are from Wave I (1994-95) and Wave II (1996) of the National Longitudinal Study of Adolescent Health (Add Health). Add Health is an ongoing nationally representative school based longitudinal study of adolescent health and their outcomes during young adulthood. Details about the study design have been previously published (Harris et al., 2009). In brief, a sample of 80 high schools and 52 middle schools from the US were selected with unequal probability of selection. Incorporating systematic sampling methods and implicit stratification into the Add Health study design ensured the sample was representative of US schools with respect to region of country, urbanicity, school size, school type, and ethnicity. At baseline, 90,118 students between grades 7-12 during 1994-1995 were administered an in-school questionnaire on topics such as school extracurricular activities, friendships, and health status. A sample (n=20,745) including both those who completed the in-school questionnaire and those who did not complete the questionnaire but on the school roster, were interviewed in their homes (Wave I). A one-year follow-up occurred (Wave II) that included 13,568 (65.4%) adolescents who were a part of Wave I.
Participants were included if they were in both Wave I and Wave II (n=13,568). Those with missing geocoded data, missing U.S. census data for their geographic area, and unstable estimates for their geographic area due to small sample sizes were excluded (n=306). Those with missing data on neighborhood variables (n=306), height and weight (n=357), sleep duration (n=36), and/or covariates of interest (n=217) were also excluded. The final analytic sample included 12,692 participants. The Add Health study was approved by the institutional review board of the University of North Carolina, Chapel Hill and written informed consent were provided by participants’ parents. These analyses were approved by the institutional review board at Emory University.
Measures of the Neighborhood Social Environment
Since both objective and perceived measures of the neighborhood social environment have been previously associated with sleep duration and/or obesity, both census-based and self-reported measures were included. Participant home addresses during Wave I were geocoded using the following sources in order of priority: 1) street-segment matches from commercial geographic information system (GIS) databases; 2) global positioning system (GPS) units, when street segments were not available; 3) a ZIP+4/ZIP+2 or a 5 digit zip centroid match when neither GIS or GPS data were available; and 4) respondent's geocoded school location (Boone-Heinonen et al., 2010). The home addresses were linked to block, group, tract and county information from the 1990 US Census and the National Archive of Criminal Justice Data for crime information.
Census-based measures were selected based on the neighborhood psychosocial hazards (NPH) scale (Glass et al., 2006) in which nine of the original 12 corresponding measures were identified in the Add Health dataset in Wave I. Those nine indicators included eight census block level measures (e.g., proportion households that are male or female household, no spouse present households with children under 18 years, proportion aged 18 years and over with no high school diploma or equivalency, proportion of males separated or divorced, proportion of females separated or divorced, proportion of housing units vacant, per capita income in 1989, unemployment rate, and proportion families with income in 1989 below poverty level ) and one county level measure (e.g., violent crimes per 100,000 population in reporting area). A comparison of the measures from the NPH scale and those found in Add Health are shown in Table S1.
Self-reported neighborhood measures from Wave I included adolescent reported neighborhood safety, parent reported neighborhood disorder, and parent reported informal control. Neighborhood safety was assessed with a yes/no response to the question of whether adolescents felt safe in their neighborhood. Neighborhood disorder was based on a summary score of responses to three questions using a three point Likert scale related to neighborhood problems with litter or trash on the streets, issues with drug dealers and drug use, and their desire to move away. The first two questions used a scale of 1=no problem at all, to 3=a big problem while the last question used a scale of 1=not at all to, 3=very much. Informal control was based on a summary score from responses using a five point Likert scale (from 1=definitely would, to 5= definitely would not) of two questions regarding whether they would tell their neighbor if their neighbor’s child was in trouble and if their neighbor would tell them if their own child was in trouble.
Exploratory factor analysis (EFA) with a Geomin rotation was conducted with all logtransformed versions of the neighborhood measures to determine the number of latent constructs underlying the 12 different items. Based on recommended research practices (Howard, 2016), factors with eigenvalues >1 and a visual inspection of a scree plot indicated a two factor solution. In addition, a cutoff of 0.4 for the factor loadings were used to determine whether a neighborhood variable sufficiently loaded onto a factor. Indicator variables < 0.4 were removed and the EFA analysis was reconducted until all factor loadings were ≥ 0.4. All self-reported measures (neighborhood safety, disorder, and informal control) and neighborhood crime had factor loadings <0.4, thus were not included in the constructs for analysis. The first factor contained five measures that reflected neighborhood socioeconomic status (SES) and included the neighborhood census tract measures on education, poverty level, unemployment rates, per capita income, and vacant housing. The second factor consisted of three items that were measures of neighborhood social disorganization which included the neighborhood census measures of single parent households and the proportion of those divorce or separated for both males and females. The Cronbach’s alpha for both factor 1 (α=0.70) and factor 2 (α=0.79) suggests acceptable internal consistency (Taber, 2018). A description of the final set of items for the two constructs are shown in Table S2. These two factors were included in our analysis as two separate latent variables.
Physical Activity
In Wave I, adolescent participants were asked how many times per week they engaged in physical activities in which the activities that had 5– 8 metabolic equivalents were considered to be moderate to vigorous physical activity (MVPA) (e.g. skating, rollerblading, dancing, cycling, martial arts, and active sports). Physical activity was modeled as five or more times of MVPA per week based on prior studies with Add Health (Gordon-Larsen et al., 2000; Suglia et al., 2014).
Screen Time (Television Watching)
Screen time was assessed in Wave I by asking participants “How many hours a week do you watch television?” TV watched per week was dichotomized as more or less than two hours of television watching per day based on guidelines by the American Academy of Pediatrics (2001).
Sleep Duration
Sleep duration was ascertained at Wave I by asking adolescents “How many hours of sleep do you usually get?” and responses were given in whole hours. Sleep duration was dichotomized based on the recommended amount of sleep for age by the National Sleep Foundation (NSF) into short sleep duration (<9 hours for 6-12 years old and <8 hours for 14-17 years old) compared to adequate sleepers (≥9 hours for 6-12 years old and ≥8 hours for 14-17 years old) (Hirshkowitz et al., 2015).
Obesity
Height and weight were measured by trained study staff at the participants’ homes in Wave II and used to calculate the body mass index (BMI). Age and sex specific BMI percentiles were then determined using the Centers for Disease Control and Prevention growth references chart (Kuczmarski et al., 2002). Obesity was defined as BMI ≥ 95th percentile.
Other Measures
Age, race/ethnicity, sex, parental education, hours spent per week watching television and self-reported physical activity were ascertained through questionnaires at Wave 1. Age was modeled continuously. Race/ethnicity was categorized as non-Hispanic White, African American, Asian, Hispanic, or Other. The highest education level attained by either the mother or the father was selected to determine the highest parental education achieved and was categorized as less than high school, high school graduate or vocational school, some college, college graduate or graduate education. Urban residence was based on 1990 Census data and was dichotomized as urban or rural. Age, race/ethnicity, sex, parental education, and urban residence were included as covariates.
Statistical Analysis
The distribution of the sociodemographic and health characteristics of the study sample by sex were examined using PROC SURVEY procedures in SAS 9.4 (SAS Institute, Cary, NC) to account for complex survey weights. Correlations between the neighborhood constructs, physical activity, TV watching, sleep duration, and obesity were examined using Pearson’s and tetrachoric correlations. Structural equation modeling (SEM) was used to examine pathways between the two-neighborhood social environment constructs as latent variables, physical activity, TV watching, sleep duration and obesity while adjusting for age, sex, race/ethnicity, highest parental education, urban residence and accounting for complex sample weights. In addition, multi-group analysis examined sex differences among these pathways. Measurement invariance (e.g. configural, metric, and scalar) was assessed. Each model was compared using chi-squared difference tests (all p-value’s > 0.05) and all models had adequate to good model fit suggesting invariance (Brown, 2015). The correlations and SEM was conducted using MPLUS 8.0 (Muthen et al., 2017) with a weighted least squares means and variance estimator and theta parameterization providing standardized probit coefficients, standard errors (SE), and two-sided p-values for the pathways. Sensitivity analyses were conducted to examine very short sleep duration (< 6 hours) which a prior study using Add Health Wave II noted to be associated with obesity among adolescents (Suglia et al., 2014).
Results
Characteristics of the overall sample and by sex are shown in Table 1. Females were slightly younger, watched less television per week, less likely to perform MVPA five times per week, more likely to have short sleep duration, very short sleep duration and a lower proportion have obesity compared to males (p<.05). There were no significant differences in race/ethnicity and highest parental education between males and females.
Table 1.
Demographic Characteristics and Health Behaviors of Adolescents, stratified by sex, National Longitudinal Study of Adolescent to Adult Health (n=12,692)
| Characteristics | Overall | Female | Male | ||||
|---|---|---|---|---|---|---|---|
| % | SE | % | SE | % | SE | p-value | |
| Age, years (mean) | 15 | 0.1 | 14.9 | 0.1 | 15.1 | 0.1 | <.001 |
| Sex, Female | 49.6 | 0.6 | -- | -- | -- | -- | |
| Race/Ethnicity | .29 | ||||||
| White | 66.0 | 2.9 | 66.3 | 2.9 | 65.8 | 2.9 | |
| African American | 14.8 | 2.0 | 15.4 | 2.0 | 14.3 | 2.0 | |
| Asian | 12.2 | 1.7 | 11.9 | 1.7 | 12.4 | 1.7 | |
| Hispanic | 3.9 | 0.8 | 3.7 | 0.8 | 4.1 | 0.8 | |
| Other | 3.1 | 0.3 | 2.8 | 0.3 | 3.4 | 0.5 | |
| Parental Highest Education | .13 | ||||||
| Less than High School | 11.5 | 1.2 | 11.5 | 1.2 | 11.6 | 1.4 | |
| High School Graduate | 27.6 | 1.1 | 28.8 | 1.2 | 26.4 | 1.3 | |
| More Than High School | 30.1 | 0.9 | 29.3 | 1.0 | 30.9 | 1.1 | |
| College Education or Higher | 30.8 | 1.7 | 30.4 | 1.8 | 31.1 | 1.8 | |
| Urban Residence | 51.8 | 4.4 | 52.2 | 4.3 | 51.3 | 4.4 | .44 |
| TV Watching, ≥2 hrs/week | 45.8 | 1.1 | 42.0 | 1.4 | 49.2 | 1.2 | <.001 |
| Physical Activity, 5+ times/week | 46.2 | 0.8 | 36.8 | 1.1 | 55.5 | 1.1 | <.001 |
| Short Sleep Durationa | 41.0 | 0.8 | 43.7 | 1.1 | 38.3 | 0.9 | <.001 |
| Very Short Sleep Durationb | 3.5 | 0.3 | 4.1 | 0.4 | 3.0 | 0.3 | .016 |
| Obesity (≥ 30 kg/m2)c | 12.6 | 0.6 | 11.2 | 0.8 | 13.9 | 0.7 | .003 |
Note: p-values come from t-tests and chi-square tests for gender differences.
Defined as below the range of recommended sleep for age set by the National Sleep Foundation
Defined as < 6 hours of sleep duration
Defined by body mass index ≥ 95th percentile which is determined by the age and sex specific BMI growth charts from the Centers for Disease Control and Prevention
Note: All variables are from Wave I of the study except obesity
Correlations between the neighborhood SES latent construct, neighborhood social disorganization latent construct, physical activity, TV watching, short sleep duration, very short sleep duration, and obesity are shown in Table 2. Neighborhood SES was significantly correlated with physical activity, TV watching, very short sleep duration, and obesity. Neighborhood social disorganization was correlated with TV watching, very short sleep duration, and obesity. Physical activity and TV watching were correlated with short sleep duration, very short sleep duration, and obesity. Very short sleep duration, not short sleep duration, was significantly correlated with obesity. The standardized estimates and standard errors from the SEM are shown in Table 3 and a simplified version of the direct effects are shown in Figure 1.
Table 2.
Correlations between the neighborhood social environment, physical activity, screen time, sleep duration, and obesity
| Neighborhood Socioeconomic Status |
Neighborhood Social Disorganization |
Physical Activity, 5+ times/week |
TV Watching, ≥2 hrs/week |
Short Sleep Durationa |
Very Short Sleep Durationb |
Obesityc | |
|---|---|---|---|---|---|---|---|
| Neighborhood Socioeconomic Status | 1.000 | ||||||
| Neighborhood Social Disorganization | 599*** | 1.000 | |||||
| Physical Activity, 5+ times/week | −.063** | −.002 | 1.000 | ||||
| TV Watching, ≥2 hrs/week | 116*** | .073** | −.023 | 1.00 | |||
| Short Sleep Durationa | .014 | .015 | −.060** | −.062** | 1.000 | ||
| Very Short Sleep Durationb | .128*** | .196*** | −.094** | −.115** | .865 | 1.000 | |
| Obesityc | .209*** | .152*** | −.110*** | .133*** | .004 | .110* | 1.000 |
Notes:
p<.05
p<.01
p<.001
Defined as below the range of recommended sleep for age set by the National Sleep Foundation
Defined as < 6 hours of sleep duration
Defined by body mass index ≥ 95th percentile which is determined by the age and sex specific
Table 3.
Results from Structural Equation Model Examining Short Sleep Duration in the Pathway between the Neighborhood Social Environment and Obesity, stratified by sex
| Pathways | Overall | Female | Male | |||
|---|---|---|---|---|---|---|
| β (SE) | p-value | β (SE) | p-value | β (SE) | p-value | |
| Direct Effects: | ||||||
| Neighborhood Socioeconomic Status → Obesity | .169 (.027) | <.001 | .149 (.042) | <.001 | .191 (.033) | <.001 |
| Neighborhood Social Disorganization → Obesity | .117 (.028) | <.001 | .123 (.039) | .002 | .108 (.033) | .001 |
| Neighborhood Socioeconomic Status → Physical Activity | −.032 (.019) | .100 | −0.007 (.030) | .804 | −.055 (.028) | .05 |
| Neighborhood Social Disorganization → Physical Activity | .022 (.019) | .241 | .007 (.025) | .783 | .040 (.033) | .22 |
| Neighborhood Socioeconomic Status → Screen Time | .075 (.021) | <.001 | .065 (.028) | .021 | .084 (.027) | .002 |
| Neighborhood Social Disorganization → Screen Time | .014 (.021) | .486 | .029 (.029) | .325 | .007 (.027) | .796 |
| Neighborhood Socioeconomic Status → Short Sleep Duration | −.019 (.020) | .332 | −.006 (.026) | .803 | −.035 (.028) | .218 |
| Neighborhood Social Disorganization → Short Sleep Duration | −.009 (.021) | .670 | −.019 (.026) | .465 | .001 (.039) | .975 |
| Physical Activity → Short Sleep Duration | −.059 (.019) | .002 | −.054 (.026) | .037 | −.061 (.026) | .019 |
| Screen Time → Short Sleep Duration | −.072 (.019) | <.001 | −.108 (.026) | <.001 | −.033 (.029) | .258 |
| Short Sleep Duration → Obesity | .006 (.023) | .805 | →.052 (.032) | .100 | .067 (.035) | .055 |
| Physical Activity → Obesity | −.129 (.027) | <.001 | −.122 (.038) | .001 | −.123 (.038) | .001 |
| Screen Time → Obesity | .096 (.024) | <.001 | .122 (.037) | .001 | .066 (.035) | .059 |
| Indirect Effects: | ||||||
| Neighborhood Socioeconomic Status → Physical Activity → Short Sleep Duration→ Obesity | <.001 (<.001) | .800 | <.001 (<.001) | .801 | <.001 (<.001) | .203 |
| Neighborhood Social Disorganization → Physical Activity → Short Sleep Duration → Obesity | <.001 (<.001) | .804 | <.001 (<.001) | .795 | <.001 (<.001) | .353 |
| Neighborhood Socioeconomic Status → Screen Time → Short Sleep Duration → Obesity | <.001 (<.001) | .805 | <.001 (<.001) | .176 | <.001 (<.001) | .344 |
| Neighborhood Social Disorganization → Screen Time → Short Sleep Duration → Obesity | <.001 (<.001) | .819 | <.001 (<.001) | .375 | <.001 (<.001) | .801 |
| Neighborhood Socioeconomic Status → Short Sleep | <.001 (<.001) | .807 | <.001 (.001) | .806 | −.002 (.002) | .326 |
| Duration → Obesity Neighborhood Social Disorganization → Short Sleep Duration → Obesity | <.001 (<.001) | .834 | .001 (.001) | .490 | <.001 (.003) | .975 |
| Neighborhood Socioeconomic Status → Physical Activity → Obesity | .004 (.003) | .116 | .001 (.004) | .802 | .007 (.004) | .089 |
| Neighborhood Social Disorganization → Physical Activity → Obesity | −.003 (.003) | .268 | −.001 (.003) | .782 | −.005 (.005) | .269 |
| Neighborhood Socioeconomic Status → Screen Time → Obesity | .007 (.003) | .007 | .008 (.004) | .074 | .006 (.003) | .070 |
| Neighborhood Social Disorganization → Screen Time → Obesity | .001 (.002) | .488 | .004 (.004) | .355 | <.001 (.002) | .793 |
| Total Effects: | ||||||
| Neighborhood Socioeconomic Status → Obesity | .180 (.028) | <.001 | .159 (.043) | <.001 | .201 (.033) | <.001 |
| Neighborhood Social Disorganization → Obesity | .115 (.028) | <.001 | .127 (.040) | .001 | .104 (.033) | .001 |
Abbreviations: β= Standardized probit coefficients, SE = Standard Error
Note: Results adjusted for race, sex, age, highest parental education, and urban residence.
Figure 1.
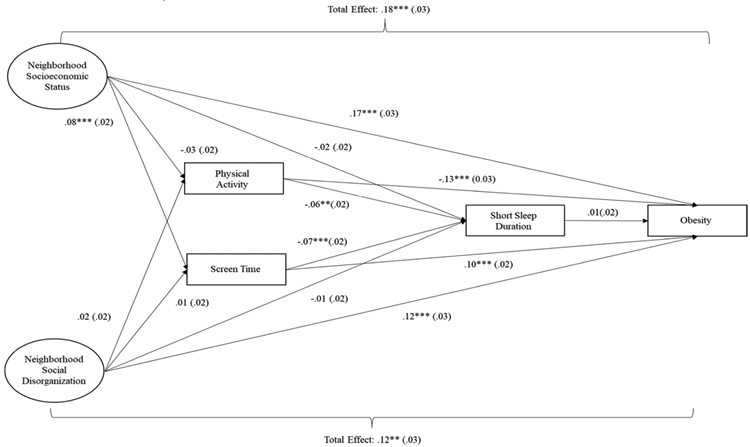
Diagram for the primary structural equation model examining short sleep duration in the pathway between the neighborhood social environment and obesity.
Standardized probit coefficients (standard errors) are presented. Results adjusted for race, sex, age, highest parental education, and urban residence Ellipses represent latent variables and boxes represent measured variables. **p<.01, ***p<0.001
Neighborhood Social Environment, Sleep Duration, and Obesity
Mediation analyses revealed that there were statistically significant direct effects of neighborhood SES (β = .169, SE = .027, p < .001) and social disorganization (β = .117, SE = .028, p = <.001) on obesity after adjusting for race, age, sex, highest parental education, and urban residence. However, the results show that there were no statistically significant indirect effects of neighborhood SES or social disorganization on obesity through sleep duration. There were also no statistically significant associations between both latent constructs of the neighborhood social environment and short sleep duration. Furthermore, there was no statistically significant relationship between short sleep duration and obesity (β = .006, SE = .023, p =.81).
Mediation Models Further Accounting for Physical Activity
There were no significant direct effects between either neighborhood social environment construct and physical activity. Increased physical activity was related to decreased probability for short sleep duration (β = −.059, SE = .019, p = .002) and obesity (β = −.129, SE = .027, p < .001). However, there were no significant indirect effects of physical activity on the relationship between either neighborhood social environment constructs, sleep duration, and obesity.
Mediation Models Further Accounting for Television Watching
Neighborhood SES was significantly associated with greater TV watching (β = .075, SE = .021, p < .001), TV watching was associated with lower probability of short sleep duration (β = −.072, SE = .019, p < .001), and greater obesity (β = .096, SE = .024, p < .001). TV watching partially mediated the association between neighborhood SES and obesity (β = .007, SE = .003, p = .007) but not through short sleep duration (p=.81). Neighborhood social disorganization was not significantly related to TV watching (p=.49) and TV watching did not mediate the association between neighborhood social disorganization and obesity (p=.49).
Sex Differences in the Pathways Between the Neighborhood Social Environment and Obesity
Both latent constructs of the neighborhood social environment were significantly associated with obesity between sexes (Table 3). There was no significant mediation by short sleep duration in any of the pathways among both females and males (p’s>0.05). Also, the measures of neighborhood SES and social disorganization were not significantly related to short sleep duration and short sleep duration was marginally associated with obesity for males only (β = .075, SE = .035, p = .030). Neighborhood SES was only marginally associated with physical activity among males (β = −.055, SE = .028, p = .050) while neighborhood social disorganization was not significantly associated with physical activity for both sexes. Physical activity was significantly associated with both short sleep duration and obesity, but there were no significant indirect effects between the neighborhood latent constructs and obesity for both sexes. In addition, neighborhood SES was significantly related screen time between sexes, but neighborhood social disorganization was not significantly associated for either sexes. Screen time was significantly associated with short sleep duration among females only (β = −.108, SE = .026, p = <.001) and was significantly associated with obesity between both sexes. There was marginally significant indirect effects by screen time in the pathway between neighborhood SES and obesity for both sexes, but no indirect effects in the association between neighborhood social disorganization and obesity. There were no significant indirect effects between either neighborhood social environment construct, physical activity, sleep duration, and obesity. Similarly, there were no significant indirect effects in the pathways between each of the neighborhood constructs, TV watching, sleep duration, and obesity.
Sensitivity Analyses
Neighborhood Social Environment, Very Short Sleep Duration, and Obesity
In analyses of very short sleep duration as < 6 hours of sleep, both the neighborhood SES (β = .160, SE = .027, p <.001) and social disorganization (β = .104, SE = .028, p < .001) constructs were significantly associated with obesity in the overall sample. There was no significant mediation by very short sleep duration in any of the pathways for the relationship between neighborhood SES and obesity (p’s>.05), but very short sleep duration partially mediated the association between neighborhood social disorganization and obesity (β = .013, SE = .006, p = .044) not involving physical activity or TV watching. Both neighborhood SES (β =.081, SE = .035, p=.020) and social disorganization (β =.116, SE = .038, p=.002) were significantly associated with very short sleep duration. Very short sleep duration was significantly related to greater probability of obesity (β = .111, SE = .048, p = .021) and only mediated the association between neighborhood social disorganization and obesity (β =.013, SE = .006, p=.044) in pathways not including TV watching and physical activity.
Sex Differences in Neighborhood Social Environment, Very Sleep Duration, and Obesity
Neighborhood SES and social disorganization was significantly associated with obesity for both females and males (Table 4). There was marginally significant indirect effects suggesting partial mediation by very short sleep duration in the pathway between neighborhood social disorganization and obesity among females only (β = .018, SE = .010, p = .059), but no other significant mediation by very short sleep in any of the other pathways for both sexes (p’s>0.05). Neighborhood SES (β = .108, SE = .035, p = .002) and social disorganization (β =.142, SE = .043, p=.001) was significantly associated with very short sleep duration among females only. Furthermore, very short sleep duration was only significantly related to obesity among females (β = .127, SE = .050, p= .019).
Table 4.
Sensitivity Analysis Results from Structural Equation Models Examining Very Short Sleep Duration (<6 Hours of Sleep) as a Mediator in the Relationship between the Neighborhood Social Environment and Obesity, stratified by sex
| Pathways | Overall | Female | Male | |||
|---|---|---|---|---|---|---|
| β (SE) | p-value | β (SE) | p-value | β (SE) | p-value | |
| Direct Effects: | ||||||
| Neighborhood Socioeconomic Status → Obesity | .160 (.027) | <.001 | .136 (.043) | .002 | .185 (.033) | <.001 |
| Neighborhood Social Disorganization → Obesity | .104 (.028) | <.001 | .107 (.040) | .008 | .101 (.034) | .003 |
| Neighborhood Socioeconomic Status → Physical Activity | −.032 (.019) | .100 | −.007 (.030) | .806 | −.054 (.028) | .051 |
| Neighborhood Social Disorganization → Physical Activity | .022 (.019) | .247 | .007 (.025) | .786 | .040 (.033) | .222 |
| Neighborhood Socioeconomic Status → Screen Time | .075 (.035) | .020 | .065 (.028) | .020 | .084 (.027) | .002 |
| Neighborhood Social Disorganization → Screen Time | .014 (.021) | .491 | .029 (.029) | .327 | .007 (.027) | .796 |
| Neighborhood Socioeconomic Status → Very Short Sleep Duration | .081 (.035) | .020 | .108 (.035) | .002 | .037 (.055) | .503 |
| Neighborhood Social Disorganization → Very Short Sleep Duration | .116 (.038) | .002 | .142 (.043) | .001 | .079 (.067) | .237 |
| Physical Activity → Very Short Sleep Duration | −.034 (.032) | .284 | .026 (.038) | .497 | −.102 (.055) | .064 |
| Screen Time → Very Short Sleep Duration | −.108 (.033) | .001 | −.143 (.040) | <.001 | −.071 (.049) | .147 |
| Very Short Sleep Duration → Obesity | .111 (.048) | .021 | .127 (.054) | .019 | .098 (.079) | .216 |
| Physical Activity → Obesity | −.125 (.026) | <.001 | −.123 (.038) | .001 | −.117 (.038) | .002 |
| Screen Time → Obesity | .108 (.025) | <.001 | .146 (.037) | <.001 | .070 (.035) | .046 |
| Indirect Effects: | ||||||
| Neighborhood Socioeconomic Status → Physical Activity → Very Short Sleep Duration → Obesity | <.001 (<.001) | .341 | <.001 (<.001) | .818 | .001 (.001) | .378 |
| Neighborhood Social Disorganization → Physical Activity → Very Short Sleep Duration → Obesity | <.001 (<.001) | .461 | <.001 (<.001) | .797 | <.001 (.001) | .454 |
| Neighborhood Socioeconomic Status → Screen Time → Very Short Sleep Duration → Obesity | −.001 (.001) | .080 | −.001 (.001) | .141 | −.001 (.001) | .307 |
| Neighborhood Social Disorganization → Screen Time Very Short Sleep Duration → Obesity | <.001 (<.001) | .509 | −.001 (.001) | .380 | <.001 (<.001) | .800 |
| Neighborhood Socioeconomic Status → Very Short Sleep Duration → Obesity | .009 (.005) | .096 | .014 (.008) | .072 | .004 (.006) | .526 |
| Neighborhood Social Disorganization → Very Short Sleep | .013 (.006) | .044 | .018 (.010) | .059 | .008 (.008) | .338 |
| Duration Obesity → Neighborhood Socioeconomic Status → Physical Activity → Obesity | .004 (.003) | .118 | .001 (.004) | .804 | .006 (.004) | .093 |
| Neighborhood Social Disorganization → Physical Activity → Obesity | −.003 (.002) | .272 | −.001 (.003) | .784 | −.005 (.004) | .276 |
| Neighborhood Socioeconomic Status → Screen Time → Obesity | .008 (.003) | .005 | .009 (.005) | .058 | .006 (.003) | .058 |
| Neighborhood Social Disorganization → Screen Time → Obesity | .002 (.002) | .490 | .004 (.004) | .348 | <.001 (.002) | .793 |
| Total Effects: | ||||||
| Neighborhood Socioeconomic Status → Obesity | .180 (.028) | <.001 | .159 (.043) | <.001 | .201 (.033) | <.001 |
| Neighborhood Social Disorganization → Obesity | .115 (.028) | <.001 | .128 (.040) | .001 | .104 (.033) | .001 |
Abbreviations: β= Standardized probit coefficients, SE = Standard Error
Note: Results adjusted for race, sex, age, highest parental education, and urban residence
Discussion
The primary purpose of our study was to examine physical activity, screen time, and sleep duration as mediators in the pathway between the neighborhood social environment and obesity. Prior evidence suggest that living in a poorer neighborhood social environment is correlated with greater stress and a worse built environment that promote physical inactivity and sedentary behavior that are both associated with short sleep duration and obesity. Moreover, previous studies have demonstrated that living in a more stressful neighborhood social environment could reduce sleep duration and that decreased amounts of sleep could increase the risk for obesity. Thus, we hypothesized that physical activity, screen time, and sleep duration would each independently mediate the neighborhood social environment and obesity association with physical activity and screen time also mediating this association through sleep duration. Results from this study indicate that living in neighborhoods with greater psychosocial hazards measured by aspects of the neighborhood SES and social disorganization are related to obesity among adolescents. In addition, the results indicate that screen time may be one mechanism linking neighborhood SES and obesity. Furthermore, the findings suggest that very short sleep duration (< 6 hours) may be a mechanism that links the neighborhood social disorganization and obesity for adolescent females.
Consistent with prior research, our cumulative measures of the neighborhood social environment was associated with obesity. Neighborhood SES and social disorganization are distinct constructs that can influence obesity through different pathways (Suglia et al., 2016). Neighborhood social disorganization is more related to living in poorer neighborhood social environments (e.g. crime, low cohesion, and collective efficacy) that can result in adverse psychosocial processes and stress which in turn will influence obesogenic behaviors (e.g. diet, physical activity, and sedentary behavior) (Theall et al., 2019; van der Valk et al., 2018). Similarly, one potential mechanism connecting neighborhood SES and obesity is that neighborhood SES can impact features of the social environment as previous studies have shown neighborhood poverty to be correlates of higher crime rates, low social cohesion and greater residential segregation, but it can also influence obesity through the built environment (Suglia et al., 2016). Prior studies found that neighborhoods of lower SES have less access to recreational facilities, supermarkets and parks which are related to greater obesogenic behaviors (Suglia et al., 2016).
Results from prior studies examining physical activity and screen time as potential mechanisms linking the neighborhood social environment and obesity among adolescents have been mixed (Franzini et al., 2009; Tu et al., 2016; Veitch et al., 2012b). Our results partly support this hypothesis as television watching was a significant mediator in the pathway between measures of neighborhood SES and obesity, but physical activity was not a mediator in any of the pathways. In addition, dietary behavior may be another pathway as those living in a lower SES neighborhood and in single parent households are less likely to have access to healthy foods and unhealthy dietary behaviors that can increase the risk for obesity (Huffman et al., 2010; Powell et al., 2007; Ranjit et al., 2015), however we do not have available diet information to assess this pathway.
The null results on the relationship between both neighborhood latent constructs and short sleep duration defined by NSF guidelines in this study are inconsistent with previous research. One study of adolescents using data from the Auburn University Sleep Study (Bagley et al., 2016) found that neighborhood poverty was associated with shorter sleep duration measured with actigraphy while another study of an adolescent cohort from the Boston Youth Survey (Street et al., 2018) demonstrated that concentrated neighborhood poverty was related to greater self-reported sleep duration. Similar to our results, a study on a multiethnic adolescent cohort from Southern California (Troxel et al., 2017) found that neighborhood poverty was not associated with self-reported sleep duration, but was related to earlier rather than later bed start times. The discrepancy between our results and prior research could be due to our study using a latent construct to measure various aspects of neighborhood SES while these studies included either one measure or a standardized mean composite score based on neighborhood census information to capture neighborhood SES. The inconsistencies in results with prior studies could also be due to the difference in the definition of short sleep duration in which our study defined short sleep duration using the NSF guidelines whereas other studies use the American Academy of Sleep Medicine guidelines. In addition our self-reported sleep measure ascertained sleep in whole hours only.
Our results also documented no significant prospective relationship between sleep duration and obesity when short sleep duration was defined using the NSF guidelines but very short sleep duration was associated with greater obesity defined as < 6 hours of sleep. A meta-analysis that included only longitudinal studies using either subjectively or objectively measured sleep duration, found that short sleep duration (defined by sleep for age) was associated with a 2.2 and 1.2 times the risk of being obese for children 9 to 11 years old and adolescents 12-18 years old, respectively (Miller et al., 2018). An explanation for the incongruent results could be due to the variation in the measurement tools used to ascertain sleep duration with some studies using self-reported sleep from parents or adolescents, which may be subjected to reporting bias, while other studies used more objective measures such, as actigraphy and polysomnography.
In sensitivity analyses examining very short sleep duration, we note that similar to the main analyses, both neighborhood constructs were significantly associated with obesity for both females and males. However, in contrast to our main analyses, there was partial mediation by very short sleep duration in the relationship between neighborhood social disorganization and obesity among females. One plausible explanation for observing mediation among adolescent females only could be that living in a socially disorganized neighborhood characterized by high family instability (e.g. high proportion of single parent-households and those divorced or separated) that expose them to greater stress compared to adolescent males. Prior studies have found that adolescent females living in single parent households and/or with divorced parents were more likely to be have conflicts with their parents and to develop depressive symptoms than adolescent males (Daryanani et al., 2016; Frost and Pakiz, 1990; Hetherington et al., 1998; Laursen, 2005). This greater exposure to stress may result in shorter sleep duration and an increase risk for the development of obesity. In addition, this suggests that there may be a threshold for the amount of sleep deprivation needed to influence the relationship between neighborhood social disorganization and obesity for adolescent females. Furthermore, this indicates that sleep interventions for adolescent females who sleep less than six hours a night in neighborhoods characterized by high social disorganization could help reduce the risk for obesity.
There are several strengths to this study. To our knowledge, this is one of the first studies to formally test physical activity, screen time, and sleep duration simultaneously as potential mediators in the association between the neighborhood social environment and obesity among adolescents. This is important as it allowed for the decomposition of the mediating effects of each health behavior while accounting for the effects of the other health behaviors (Sánchez et al., 2005). In addition, modeling the neighborhood social environment as latent variables allows for the combining of the various indicators of the social environment, which may not have been possible in a regression model that include these individual variables simultaneously due to their high correlation (Duncan and Kawachi, 2018; Kline, 2016; Palumbo et al., 2016). Another advantage of modeling the indicators of the neighborhood social environment as latent variables compared to using a continuous index is that latent variables account for the potential of each indicator of the neighborhood social environment to have different effects on the health behaviors and obesity (Sánchez et al., 2005). Furthermore, the study was conducted using a large nationally representative longitudinal sample of U.S. adolescents, which may address the limitation of prior studies that have examined physical activity and/or screen time as mediators between the neighborhood social environment and obesity. These studies had smaller sample sizes (Dulin-Keita et al., 2013; Franzini et al., 2009; Siceloff et al., 2014; Veitch et al., 2012a), were cross-sectional in nature and limited in geographic representation of the U.S. with studies being either outside of the U.S. or representative of a single U.S. city (Dulin-Keita et al., 2013; Franzini et al., 2009; Tu et al., 2016; Veitch et al., 2012a). The study also included a racially diverse nationally representative sample allowing the results to be more generalizable to U.S. adolescents. Finally, our study included objective measures of height and weight, which helps to reduce measurement errors associated with self-report measures that are often used in adolescent studies.
Despite these strengths, there are limitations to this study. Although the neighborhood social environment construct included comprehensive Census based measures, there are still other aspects of the social environment such as residential racial segregation (Ryabov, 2015) and community violence and hopelessness (Umlauf et al., 2015) that were not captured that could potentially influence sleep duration and obesity. Also, prior studies comparing self-reported sleep to actigraphy among U.S. adolescents have found moderate correlations and the resulting random misclassification of sleep may have biased our results towards the null (Matthews et al., 2014; Wolfson et al., 2003). Although there was no significant mediation by short sleep duration (defined by the NSF) in the association between the neighborhood constructs and obesity, there was significant mediation of very short sleep duration (< 6 hours of sleep) in the association between the neighborhood social disorganization construct and obesity. In addition, physical activity was associated with short sleep duration and screen time mediated the association between neighborhood SES and obesity. These significant findings suggest that the measurement error of self-reported sleep may not have been the primary contributor to the null results. Furthermore, the data only captured TV watching as a measure of screen time since the data was from 1994-1995 which may not represent other mediums of screen time relevant today such as smart phones, tablets, and computers (Stiglic and Viner, 2019).
Our study provides significant contributions to the growing literature on the relationship between neighborhood social environments and obesity among adolescents. Consistent with prior research, our findings suggest that developing interventions to improve neighborhood social conditions may reduce the risk for obesity. For instance, policy initiatives that improve socioeconomic opportunities in neighborhoods for parents such as increases in minimum wage, job training programs, and mixed income housing can translate into better health for their children (Daniel et al., 2018; Levy et al., 2013). Future studies should investigate whether other neighborhood social factors influence sleep and obesity. In addition, studies should explore objectively measured sleep and other health behaviors such as, diet, as potential mediators in this pathway. Doing so can help identify points of intervention for reducing obesity early in the life course and prevent obesity during adulthood.
Supplementary Material
Highlights.
Worse neighborhood socioeconomic status and social disorganization were associated with obesity.
Screen time (>2 hours/day of television) mediated neighborhood socioeconomic status and obesity.
Very short sleep duration (< 6 hours) mediated social disorganization and obesity for females.
Acknowledgements:
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01- HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Funding: Supported by the National Institutes of Health (T32HL130025 and HL125761).
Abbreviations:
- SES:
Socioeconomic Status
- Add Health:
The Longitudinal Study of Adolescent to Adult Health
- BMI:
Body Mass Index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: The authors declared no conflict of interest.
References
- 2001. American Academy of Pediatrics: Children, adolescents, and television. Pediatrics 107, 423–426. [DOI] [PubMed] [Google Scholar]
- Alvarado SE, 2016. Neighborhood disadvantage and obesity across childhood and adolescence: Evidence from the NLSY children and young adults cohort (1986–2010). Social Science Research 57, 80–98. [DOI] [PubMed] [Google Scholar]
- Bagley EJ, Fuller-Rowell TE, Saini EK, Philbrook LE, El-Sheikh M, 2016. Neighborhood economic deprivation and social fragmentation: associations with children’s sleep. Behavioral Sleep Medicine, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Evenson KR, Song Y, Gordon-Larsen P, 2010. Built and socioeconomic environments: patterning and associations with physical activity in U.S. adolescents. International Journal of Behavioral Nutrition and Physical Activity 7, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell LN, Graham L, Joseph SP, 2016. Associations of neighborhood safety and neighborhood support with overweight and obesity in US children and adolescents. Ethnicity & Disease 26, 469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, 2015. Confirmatory factor analysis for applied research, 2nd ed. The Guilford Press, New York, NY, US. [Google Scholar]
- Carrillo-Álvarez E, Kawachi I, Riera-Romaní J, 2019. Neighbourhood social capital and obesity: a systematic review of the literature. Obesity Reviews 20, 119–141. [DOI] [PubMed] [Google Scholar]
- Carter MA, Dubois L, 2010. Neighbourhoods and child adiposity: A critical appraisal of the literature. Health & Place 16, 616–628. [DOI] [PubMed] [Google Scholar]
- Cecil-Karb R, Grogan-Kaylor A, 2009. Childhood body mass index in community context: neighborhood safety, television viewing, and growth trajectories of BMI. Health Soc Work 34, 169–177. [DOI] [PubMed] [Google Scholar]
- Chaparro MP, Bilfield A, Theall KP, 2018. Exposure to Neighborhood Crime Is Associated with Lower Levels of Physical Activity and Higher Obesity Risk among Adolescent Girls, but Not Boys. Childhood Obesity 15, 87–92. [DOI] [PubMed] [Google Scholar]
- Daniel H, Bornstein SS, Kane GC, 2018. Addressing social determinants to improve patient care and promote health equity: An american college of physicians position paper. Annals of Internal Medicine 168, 577–578. [DOI] [PubMed] [Google Scholar]
- Daryanani I, Hamilton JL, Abramson LY, Alloy LB, 2016. Single Mother Parenting and Adolescent Psychopathology. Journal of abnormal child psychology 44, 1411–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C, 2010. Neighborhoods and health. Ann N Y Acad Sci 1186, 125–145. [DOI] [PubMed] [Google Scholar]
- Dulin-Keita A, Kaur Thind H, Affuso O, Baskin ML, 2013. The associations of perceived neighborhood disorder and physical activity with obesity among African American adolescents. BMC Public Health 13, 440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Kawachi I, 2018. Neighborhoods and health. [Google Scholar]
- Duraccio KM, Krietsch KN, Chardon ML, Van Dyk TR, Beebe DW, 2019. Poor sleep and adolescent obesity risk: a narrative review of potential mechanisms. Adolescent health, medicine and therapeutics 10, 117–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Li D, Whipple SS, 2013. Cumulative risk and child development. Psychol Bull 139, 1342–1396. [DOI] [PubMed] [Google Scholar]
- Forno E, Celedón JC, 2017. The effect of obesity, weight gain, and weight loss on asthma inception and control. Current Opinion in Allergy and Clinical Immunology 17, 123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzini L, Elliott MN, Cuccaro P, Schuster M, Gilliland MJ, Grunbaum JA, Franklin F, Tortolero SR, 2009. Influences of physical and social neighborhood environments on children's physical activity and obesity. American Journal of Public Health 99, 271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost AK, Pakiz B, 1990. The effects of marital disruption on adolescents: time as a dynamic. Am J Orthopsychiatry 60, 544–555. [DOI] [PubMed] [Google Scholar]
- Glass TA, Rasmussen MD, Schwartz BS, 2006. Neighborhoods and obesity in older adults: The Baltimore memory study. Am J Prev Med 31, 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, McMurray RG, Popkin BM, 2000. Determinants of adolescent physical activity and inactivity patterns. Pediatrics 105, E83. [DOI] [PubMed] [Google Scholar]
- Greves Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P, 2010. Child obesity associated with social disadvantage of children's neighborhoods. Social Science & Medicine 71, 584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Guan S, 2015. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Medicine Reviews 21, 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Kirschen GW, LeBourgeois MK, Gradisar M, Garrison MM, Montgomery-Downs H, Kirschen H, McHale SM, Chang A-M, Buxton OM, 2018. Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child and adolescent psychiatric clinics of North America 27, 229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, Udry JR, 2009. The National Longitudinal Study of Adolescent to Adult Health: Research design Hetherington EM, Bridges M, Insabella GM, 1998. What matters? What does not? Five perspectives on the association between marital transitions and children's adjustment. American Psychologist 53, 167–184. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, Adams Hillard PJ, 2015. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health: Journal of the National Sleep Foundation 1, 40–43. [DOI] [PubMed] [Google Scholar]
- Howard MC, 2016. A review of exploratory factor analysis decisions and overview of current practices: What we are doing and how can we improve? International Journal of Human- Computer Interaction 32, 51–62. [Google Scholar]
- Huffman FG, Kanikireddy S, Patel M, 2010. Parenthood—a contributing factor to childhood obesity. International Journal of Environmental Research and Public Health 7, 2800–2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB, 2016. Principles and practice of structural equation modeling, 4th ed. Guilford Press, New York, NY, US. [Google Scholar]
- Knutson KL, 2005. Sex differences in the association between sleep and body mass index in adolescents. The Journal of pediatrics 147, 830–834. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL, 2002. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat 11, 1–190. [PubMed] [Google Scholar]
- Laursen B, 2005. Conflict Between Mothers and Adolescents in Single-Mother, Blended, and Two-Biological-Parent Families. Parenting, science and practice 5, 347–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DK, McDade Z, Bertumen K, 2013. Mixed-income living: Anticipated and realized benefits for low-income households. Cityscape 15, 15–28. [Google Scholar]
- Lippert AM, 2016. Stuck in Unhealthy Places: How Entering, Exiting, and Remaining in Poor and Nonpoor Neighborhoods Is Associated with Obesity during the Transition to Adulthood. J Health Soc Behav 57, 1–21. [DOI] [PubMed] [Google Scholar]
- Lubans D, Richards J, Hillman C, Faulkner G, Beauchamp M, Nilsson M, Kelly P, Smith J, Raine L, Biddle S, 2016. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics 138, e20161642. [DOI] [PubMed] [Google Scholar]
- Lumeng JC, Appugliese D, Cabral HJ, Bradley RH, Zuckerman B, 2006. Neighborhood safety and overweight status in children. Archives of Pediatrics & Adolescent Medicine 160, 25–31. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Pasch KE, Farbakhsh K, 2011. The relationship between sleep and weight in a sample of adolescents. Obesity 19, 324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Ozer E, 2014. Developmental trends in sleep duration in adolescence and young adulthood: Evidence from a national US sample. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 54, 691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Hall M, Dahl RE, 2014. Sleep in healthy black and white adolescents. Pediatrics 133, e1189–e1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MA, Kruisbrink M, Wallace J, Ji C, Cappuccio FP, 2018. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep 41. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthén BO, Muthén M, 2017. Mplus Version 8 User's Guide. Muthen & Muthen. [Google Scholar]
- Ogden CL, Carroll MD, Fryar CD, Flegal KM, 2015. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief, 1–8. [PubMed] [Google Scholar]
- Pabayo R, Molnar BE, Street N, Kawachi I, 2014. The relationship between social fragmentation and sleep among adolescents living in Boston, Massachusetts. J Public Health (Oxf) 36, 587–598. [DOI] [PubMed] [Google Scholar]
- Palumbo A, Michael Y, Hyslop T, 2016. Latent class model characterization of neighborhood socioeconomic status. Cancer causes & control : CCC 27, 445–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pont SJ, Puhl R, Cook SR, Slusser W, 2017. Stigma Experienced by Children and Adolescents With Obesity. Pediatrics 140, e20173034. [DOI] [PubMed] [Google Scholar]
- Powell LM, Chaloupka FJ, Bao Y, 2007. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med 33, S240–245. [DOI] [PubMed] [Google Scholar]
- Ranjit N, Wilkinson AV, Lytle LM, Evans AE, Saxton D, Hoelscher DM, 2015. Socioeconomic inequalities in children’s diet: the role of the home food environment. Int J Behav Nutr Phys Act 12, S4–S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin J, Matthews L, Cobley S, Han A, Sanders R, Wiltshire HD, Baker JS, 2016. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolescent health, medicine and therapeutics 7, 125–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryabov I, 2015. The role of residential segregation in explaining racial gaps in childhood and adolescent obesity. Youth & Society 50, 485–505. [Google Scholar]
- Sánchez BN, Budtz-Jørgensen E, Ryan LM, Hu H, 2005. Structural Equation Models: A Review with Applications to Environmental Epidemiology. Journal of the American Statistical Association 100, 1443–1455. [Google Scholar]
- Siceloff ER, Coulon SM, Wilson DK, 2014. Physical activity as a mediator linking neighborhood environmental supports and obesity in African Americans in the path trial. Health Psychol 33, 481–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Kenney MK, 2013. Rising Prevalence and Neighborhood, Social, and Behavioral Determinants of Sleep Problems in US Children and Adolescents, 2003-2012. Sleep Disorders 2013, 394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, Kogan MD, 2010. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Affairs 29, 503–512. [DOI] [PubMed] [Google Scholar]
- Sophie D, Manuel T-L, 2018. The Effects of Physical Activity on Sleep among Adolescents and Adults: A Narrative Review. Journal of Sleep and Sleep Disorder Research 1, 42–59. [Google Scholar]
- Stiglic N, Viner RM, 2019. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ open 9, e023191–e023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street NW, McCormick MC, Austin SB, Slopen N, Habre R, Molnar BE, 2018. Examining family and neighborhood level predictors of sleep duration in urban youth. Families, Systems, & Health, No Pagination Specified-No Pagination Specified. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Kara S, Robinson WR, 2014. Sleep duration and obesity among adolescents transitioning to adulthood: do results differ by sex? The Journal of pediatrics 165, 750–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Shelton RC, Hsiao A, Wang YC, Rundle A, Link BG, 2016. Why the neighborhood social environment is critical in obesity prevention. J Urban Health 93, 206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundar TKB, Løndal K, Lagerløv P, Glavin K, Helseth S, 2018. Overweight adolescents' views on physical activity - experiences of participants in an internet-based intervention: a qualitative study. BMC Public Health 18, 448–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taber KS, 2018. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education 48, 1273–1296. [Google Scholar]
- Theall KP, Chaparro MP, Denstel K, Bilfield A, Drury SS, 2019. Childhood obesity and the associated roles of neighborhood and biologic stress. Preventive Medicine Reports 14, 100849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theall KP, Drury SS, Shirtcliff EA, 2012. Cumulative Neighborhood Risk of Psychosocial Stress and Allostatic Load in Adolescents. American Journal of Epidemiology 176, S164–S174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Shih RA, Ewing B, Tucker JS, Nugroho A, D’Amico EJ, 2017. Examining of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health & Place 45, 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu AW, Mâsse LC, Lear SA, Gotay CC, Richardson CG, 2016. Exploring the mediating roles of physical activity and television time on the relationship between the neighbourhood environment and childhood obesity. Canadian Journal of Public Health / Revue Canadienne de Santé Publique 107, e168–e175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umlauf MG, Bolland AC, Bolland KA, Tomek S, Bolland JM, 2015. The effects of age, gender, hopelessness, and exposure to violence on sleep disorder symptoms and daytime sleepiness among adolescents in impoverished neighborhoods. J Youth Adolesc 44, 518–542. [DOI] [PubMed] [Google Scholar]
- van der Valk ES, Savas M, van Rossum EFC, 2018. Stress and obesity: Are there more susceptible individuals? Current Obesity Reports 7, 193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veitch J, van Stralen MM, Chinapaw MJM, te Velde SJ, Crawford D, Salmon J, Timperio A, 2012a. The neighborhood social environment and body mass index among youth: a mediation analysis. Int J Behav Nutr Phys Act 9, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veitch J, van Stralen MM, Chinapaw, te Velde SJ, Crawford D, Salmon J, Timperio A, 2012b. The neighborhood social environment and body mass index among youth: a mediation analysis. Int J Behav Nutr Phys Act 9, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL, 2017. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N Engl J Med 377, 2145–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson NF, Horn E, Duncan GE, Buchwald D, Vitiello MV, Turkheimer E, 2016. Sleep duration and area-level deprivation in twins. Sleep 39, 67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton AG, Jones SE, Cooper AC, Croft JB, 2018. Short Sleep Duration Among Middle School and High School Students - United States, 2015. MMWR Morb Mortal Wkly Rep 67, 85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL, 2003. Evidence for the validity of a sleep habits survey for adolescents. Sleep 26, 213–216. [DOI] [PubMed] [Google Scholar]
- Youngstedt SD, 2005. Effects of exercise on sleep. Clin Sports Med 24, 355–365, xi. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


