Abstract
Objectives
The coronavirus disease 2019 (COVID-19) outbreak, along with implementation of lockdown and strict public movement restrictions, in Greece has affected hospital visits and admissions. We aimed to investigate trends of cardiac disease admissions during the outbreak of the pandemic and possible associations with the applied restrictive measures.
Study design
This is a retrospective observational study.
Methods
Data for 4970 patients admitted via the cardiology emergency department (ED) across 3 large-volume urban hospitals in Athens and 2 regional/rural hospitals from February 3, 2020, up to April 12 were recorded. Data from the equivalent (for the COVID-19 outbreak) time period of 2019 and from the postlockdown time period were also collected.
Results
A falling trend of cardiology ED visits and hospital admissions was observed starting from the week when the restrictive measures due to COVID-19 were implemented. Compared with the pre–COVID-19 outbreak time period, acute coronary syndrome (ACS) [145 (29/week) vs. 60 (12/week), −59%, P < 0.001], ST elevation myocardial infarction [46 (9.2/week) vs. 21 (4.2/week), −54%, P = 0.002], and non-ST elevation ACS [99 cases (19.8/week) vs. 39 (7.8/week), −60% P < 0.001] were reduced at the COVID-19 outbreak time period. Reductions were also noted for heart failure worsening and arrhythmias. The ED visits in the postlockdown period were significantly higher than in the COVID-19 outbreak time period (1511 vs 660; P < 0.05).
Conclusion
Our data show significant drops in cardiology visits and admissions during the COVID-19 outbreak time period. Whether this results from restrictive measures or depicts a true reduction of cardiac disease cases warrants further investigation.
Keywords: COVID-19, SARS-CoV-2, Emergency department, Acute coronary syndromes
Highlights
-
•
The coronavirus disease 2019 (COVID-19) outbreak has led to an unprecedented health system overload.
-
•
The restrictive measures in Greece resulted in a low number of COVID-19 cases.
-
•
Hospital visits and cardiovascular events have diminished after implementation of restrictive measures.
-
•
Acute coronary syndromes reduced by approximately 55%, despite limited incidence of COVID-19.
-
•
The multifactorial etiology of this finding should be thoroughly investigated.
Introduction
During the first quarter of 2020, the worldwide spread of a disease outbreak that originated in Wuhan, China, namely, coronavirus disease 2019 (COVID-19), has put several national healthcare systems in a situation of serious overload. Longer delays in the treatment of patients with ST elevation myocardial infarction (STEMI), as well as a significant lag between symptom onset and first medical contact, have been recorded, suggesting that patients are reluctant to seek medical care.1 Although anecdotal reports are many, true registries of cardiac visits to hospitals and admissions are scarce. In Spain, there was a 40% decrease in patients treated by percutaneous coronary intervention for STEMI,2 which is corroborated by similar decreases from data in catheterization laboratories in the United States of America (USA).3
This observed reduction could be attributed to misdiagnosis in the setting of healthcare overload, to reluctance to seek medical help in an environment that is perceived to precipitate infection, to hindered access due to strict movement restrictions during lockdown, or to a true paradoxical reduction of acute cardiovascular events, possibly owing to beneficial changes in lifestyle.
The course of the pandemic in Greece merits particular attendance. Lockdown and strict movement restrictions were implemented early, resulting in a remarkably low number of COVID-19 cases and deaths (121 deaths as of April 21). We aimed to record trends in hospital visits and admissions for cardiac diseases, with an emphasis on acute coronary syndrome (ACS), during the outbreak of the pandemic and investigate possible associations with restrictive measures. For this purpose, we collected data from 5 high-volume hospitals during the periods of interest.
Methods
Study design and population
This is a retrospective analysis of the data collected from cardiology emergency departments (EDs) in Greece in 5 large-volume hospitals of the national health system. Three hospitals belong to the larger metropolitan area of Athens (Hippokration General Hospital, Athens; Laiko General Hospital, Athens; Red Cross General Hospital, Athens), and 2 are regional hospitals of the national health system outside the metropolitan area of Athens (Kalamata General Hospital and Trikala General Hospital). We opted for representativeness including both university and non-university, as well as metropolitan and regional, hospitals. Data were collected for the period from February 3, 2020, up to April 13 (before and during the pandemic outbreak) and from the equivalent (COVID-19 outbreak) time period of 2019. After the lifting of restrictive measures, we also collected data from an equivalent (4/5/2020 to 7/6/2020) time period (postlockdown period).
Based on an ad hoc design form, we collected demographic data (such as age and gender), as well as patients' medical history, the reason of the visit, and diagnosis of admission.
The study was carried out in accordance with the Declaration of Helsinki (1989) and with the General Data Protection Regulation.
Statistical analysis
Statistical analysis was carried out by E.O., P.T., and T.Z. Continuous variables (presented as mean ± standard deviation) were tested for normality of distribution using the Kolmogorov-Smirnov test and by visual inspection of P-P plots. Student's t-test was used to test for differences between 2 categories of normally distributed continuous data. Differences between categorical variables were tested by forming contingency tables and performing chi-squared tests. Adjustment for multiple comparisons was performed as appropriate. All reported P values were based on two-sided hypotheses. All statistical calculations were performed using SPSS software (version 25.0; SPSS Inc., Chicago, Illinois, USA).
Results
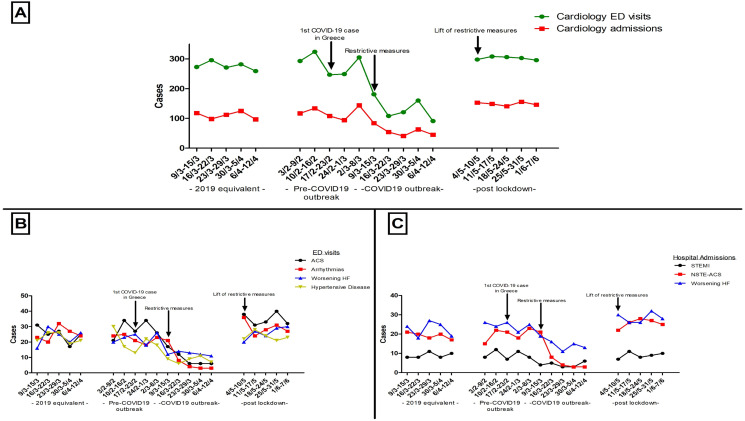
Data from a total of 4970 cardiology ED visits were collected. The cumulative cardiology ED visits and cardiology department admissions per week in the 3 public large-volume urban hospitals from February 2020 are shown in Supplementary Table 1 and in Fig. 1 A. As shown in Supplementary Table 1 and in Fig. 1A, a reduction in cardiology ED visits and admissions was observed in the beginning of the week on March 9, which corresponds with the implementation of the first restrictive measures (i.e., closure of schools). Given that the lockdown (closure of educational institutions, restaurants, cafeterias, and so on) was initiated on March 11, 2020, and that the first COVID-19–associated death in Greece, which may have influenced public awareness, occurred on March 12, 2020, we divided this retrospective analysis into 2 equivalent time periods: COVID-19 outbreak time period (5-week length: from March 9, 2020, up to April 12, 2020) and pre–COVID-19 outbreak time period (5-week length: from February 3, 2020, up to March 8, 2020).
Fig. 1.
Emergency department and cardiology department data before and during the time of the COVID-19 outbreak in Greece. (A) Cardiology emergency department visits and admissions as per dates before and during the COVID-19 outbreak in Greece. (B) Etiology of cardiology emergency departments visits as per dates before and during the COVID-19 outbreak in Greece. (C) Causes of cardiology department admissions as per dates before and during the COVID-19 outbreak in Greece ED: emergency department; COVID-19: coronavirus disease 2019; ACS: acute coronary syndrome; STEMI: ST elevation myocardial infarction; NSTE-ACS: non-ST elevation acute coronary syndrome; HF: heart failure.
We observed a falling trend of cardiology ED visits and admissions starting from the week when the restrictive measures due to COVID-19 were implemented. As shown in Table 1 and Fig. 1A, the cumulative visits in the pre–COVID-19 outbreak time period were 1418, whereas the respective cardiology ED visits in the COVID-19 outbreak time period were 660 (P < 0.001). Τhe average number of visits dropped from 283.6 per week in the pre–COVID-19 outbreak time period to 132.2 per week in the COVID-19 outbreak time period.
Table 1.
Comparison of cardiology emergency department visits and hospital admissions between the pre–COVID-19 outbreak time period, the COVID-19 outbreak time period of 2020, the equivalent time period of 2019, and the postlockdown time period.
| Characteristics | Equivalent 2019 time period, 9/3/2019–2/4/2019 | Pre–COVID-19 outbreak time period, 3/2/2020–8/3/2020 | COVID-19 outbreak time period, 9/3/2020–12/4/2020 | Postlockdown time period, 4/5/2020–7/6/2020 | % change | Pa | Pb | Pc |
|---|---|---|---|---|---|---|---|---|
| Cardiology ED visits | 1381 | 1418 | 660 | 1511f | −53% | .48 | <.001 | <.001 |
| Age | 62.9 ± 19.2 | 62.9 ± 17.8 | 62.8 ± 17.3 | 64.9 ± 16.3d,e,f | .79 | 1.00 | 1.00 | |
| Gender (male) | 55.1 | 58.9 | 62.3 | 61.5 | .09 | .006 | .16 | |
| Cardiac arrest | 11 | 20 | 15 | 27d | −25% | .11 | .43 | .40 |
| Hospital admissions | 550 | 597 | 257 | 745d,e,f | −57% | .17 | <.001 | <.001 |
| ACS | 141 | 145 | 60 | 174f | −59% | .81 | <.001 | <.001 |
| STEMI | 45 | 46 | 21 | 45f | −54% | .92 | .003 | .002 |
| NSTE-ACS | 96 | 99 | 39 | 129f | −60% | .83 | <.001 | <.001 |
| Worsening HF | 111 | 122 | 74 | 142f | −39% | .47 | .01 | .001 |
| Atrial fibrillation | 46 | 70 | 24 | 22d,e | −66% | .03 | .01 | <.001 |
| Pulmonary embolism | 5 | 6 | 1 | 18d,f | −83% | .76 | .10 | .06 |
| Hypertensive crisis | 6 | 8 | 6 | 8 | −25% | .59 | 1.00 | .59 |
| Pericarditis | 10 | 9 | 9 | 12 | 0% | .82 | .82 | 1.00 |
| Aortic disease | 1 | 3 | 1 | 3 | −67% | .32 | 1.00 | .32 |
ED: emergency department, ACS: acute coronary syndrome, STEMI: ST elevation myocardial infarction, NSTE-ACS: non-ST elevation acute coronary syndrome, HF: heart failure; COVID-19: coronavirus disease 2019.
Denotes comparison between the equivalent 2019 time period and pre–COVID-19 outbreak time period.
Denotes comparison between the equivalent 2019 time period and COVID-19 outbreak time period.
Denotes comparison between the pre–COVID-19 outbreak time period and COVID-19 outbreak time period.
Denotes statistically significant difference when comparing the postlockdown time period with the 2019 equivalent-to-COVID-19 outbreak time period.
Denotes statistically significant difference when comparing the postlockdown time period with the pre–COVID-19 outbreak time period.
Denotes statistically significant difference when comparing the postlockdown time period with the COVID-19 outbreak time period; correction for multiple comparisons was applied; % change denotes change from the pre-outbreak to the outbreak period.
The prevalence of more common etiologies of cardiology ED visits is presented in Fig. 1B. We recorded 597 hospital admissions during the pre–COVID-19 outbreak time period, opposed to 257 in the COVID-19 outbreak time period, translating to a fall from an average of 119.4 per week to 57.4 per week (57% reduction) during the aforementioned time stamps (Table 1 and Fig. 1C). Concerning the most common reasons for cardiology department admissions, ACS cases were reduced from 145 (29/week) in the pre–COVID-19 outbreak time period to 60 (12/week) in the COVID-19 outbreak time period, corresponding to a 59% reduction. Specifically, we recorded 46 (9.2/week) cases of STEMI during the pre–COVID-19 outbreak time period, with only 21 (4.2/week) in the COVID-19 outbreak time period (54% reduction). A more notable difference was noted in non-ST elevation (NSTE) ACS, with 99 cases (19.8/week) during the pre–COVID-19 outbreak time period and just 39 (7.8/week) during the COVID-19 outbreak time period (60% reduction). It is worth mentioning that no significant difference with regard to age was noted in patients with STEMI (pre–COVID-19 outbreak time period: 62.9 ± 13.6 years vs. COVID-19 outbreak time period: 62.5 ± 11.7 years, P = 0.92) or NSTE-ACS (pre–COVID-19 outbreak time period: 63.5 ± 14.4 years vs. COVID-19 outbreak time period: 65.2 ± 13.3 years, P = 0.57). Hospitalizations for worsening heart failure were also decreased, with 122 cases (24.4/week) in the pre–COVID-19 outbreak time period and 74 cases (14.8/week) in the COVID-19 outbreak time period.
To explore the impact of restrictive measures on ED visits and cardiology department admissions as per sex (Supplementary Table 2) and age (Supplementary Table 3), we proceeded to subgroup analysis. The falling trend of cardiology ED visits and admissions after the lockdown was observed in both genders (Supplementary Table 2) and in all age ranges (in those aged >65 years and in younger subjects) (Supplementary Table 3).
To further validate our findings, we analyzed cardiology ED visits and cardiology department admissions in an equivalent 2019 time period of the pandemic (from March 9, 2019, until April 12, 2019). Visits and admissions in the 2019 period were practically similar to those in the pre–COVID-19 outbreak time period of 2020 (Table 1 and Fig. 1). Importantly, comparisons of the 2019 period and the outbreak period showed similar results with the comparison of the pre-outbreak and during outbreak periods (Table 1 and Fig. 1).
Compared to the COVID-19 lockdown period, in the post-lockdown period a significant increase was observed in cardiology ED visits and cardiology department admissions, especially for ACS cases. As shown in Table 1 and Fig. 1A, the cumulative visits in the post-lockdown period was higher than the COVID-19 outbreak time period (1511 vs 660; P < 0.05) and pre–COVID-19 outbreak time period (1418; P = 0.48).
We performed a separate (exploratory) analysis for regional hospitals outside the metropolitan area of Athens. In these hospitals, 19 STEMI and 18 NSTE-ACS cases were reported during the COVID-19 outbreak time period, which were similar to those reported during the pre–COVID-19 outbreak time period (19 STEMI and 19 NSTE-ACS cases, P = NS for both). Compared with the equivalent 2019 time period, STEMI cases after the 2020 restrictive measures were almost identical (equivalent 2019 time period: 20 STEMI cases vs. COVID-19 outbreak time period: 19 cases, P = NS). On the other hand, NSTE-ACS cases in the COVID-19 outbreak time period of 2020 decreased, albeit non-significantly, compared with the equivalent 2019 time period (2019: 35 cases vs. 2020: 18 cases, P = 0.072).
Discussion
Our multicenter data show a significant reduction in cardiology ED visits and hospital admissions during the outbreak of the COVID-19 pandemic. Importantly, this reduction concerns particularly ACS cases, with the reduction of NSTE-ACS cases being higher than the respective decrease of STEMI cases. Interestingly, the trends of ACS reduction were not evident in rural hospitals. These data are particularly important in the context of early implementation of lockdown and strict public movement restrictions that resulted in a remarkably low number of COVID-19 cases in Greece.
The worldwide declining trends of patients treated for acute cardiovascular disease may represent either reduced seeking of medical treatment in a background of unchanged, or even increased, incidence of cardiovascular disease, or a true reduction of such events.1, 2, 3, 4 Our study has particular methodological strengths that ensure its validity and aid in interpretation of findings, namely, (i) comparisons were made not only within 2020 periods but also with the respective 2019 period, (ii) data were collected from metropolitan and non-metropolitan hospitals, (iii) lockdown and restrictive measures were implemented early, and compliance of the population was very high, and (iv) the number of COVID-19 cases was very small, and there was no excessive load in the healthcare system.
In the case that reduced hospital visits and admissions do not represent true cardiovascular disease incidence, reduced hospital accessibility due to healthcare overload may play an important role. However, Greece has been fortunate to have a relatively low number of confirmed COVID-19 cases, with critically ill patients well within current healthcare system capacity.4 Patients' fear of COVID-19 may be another factor affecting the number of ED visits.5 Indeed, our data show that visits and admissions seem to have a temporal association with the first COVID-19–related death in Greece (albeit not with the first COVID-19 case). Another finding that may offer corroboration to this explanation is the fact that NSTE-ACS cases have decreased during the COVID-19 outbreak to a higher proportion relative to STEMI, implying that patients with lenient symptoms may be more reluctant to visit the hospital during the COVID-19 pandemic. Reduced mobility due to strict public circulation measures may have accounted for the trends observed. This is supported by the temporal association with the imposed measures and possibly by the fact that ACS cases did not decrease in regional hospitals outside Athens, where accessibility is easier.
In terms of proper treatment of ACS, this spurious decrease of visits and admissions has important implications. A reduction in patients receiving treatment for STEMI or the introduction of delays in timely reperfusion may have detrimental effects both in the acute and long term; thus, policies that secure in-hospital and out-of-hospital pathways for patients with ACS need to be implemented.6
The selection of facilities dedicated exclusively to the management of COVID-19 cases is a reasonable approach for limiting hospital visits for other health issues. This would help minimize nosocomial transmission of COVID-19. The issue of delayed healthcare seeking by patients with significant cardiovascular pathology is a concern as this could lead to preventable morbidity and mortality. Patient awareness, education, and reassurance measures are required so that affected patients seek appropriate health care in a timely fashion. Similarly, clinical care pathways need to be adapted so that timely healthcare assistance is provided for patients with symptoms suggestive of cardiovascular disease (i.e., chest pain or discomfort, acute dyspnea, and so on).
Conclusion
The data of the present multicenter study data show significant drops in cardiology visits and admissions during the COVID-19 outbreak. Importantly, this reduction concerns particularly ACS cases, with the reduction of NSTE-ACS cases being greater than the respective decrease in STEMI cases. Whether this represents a spurious or true reduction of cardiac disease cases needs to be further investigated. However, the association with the early implementation of lockdown and strict public restrictions that resulted in a remarkably low number of COVID-19 cases in Greece aids interpretations and shaping of timely health policies especially concerning prompt accessibility to healthcare services for cardiovascular emergency cases.
Author statements
Ethical approval
The study was approved by the ethics committee of each institution.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
None declared.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2020.08.007.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Tam C.F., Cheung K.S., Lam S., Wong A., Yung A., Sze M. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Negreira Caamano M., Piqueras Flores J., Mateo Gomez C. [Impact of COVID-19 pandemic in cardiology admissions] Med Clin (Barc) 2020;155:179–180. doi: 10.1016/j.medcli.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cosentino N., Assanelli E., Merlino L., Mazza M., Bartorelli A.L., Marenzi G. An in-hospital pathway for acute coronary syndrome patients during the COVID-19 outbreak: initial experience under real-world suboptimal conditions. Can J Cardiol. 2020;36:961–964. doi: 10.1016/j.cjca.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.