Abstract
Introduction
Coronavirus disease 2019 (Covid-19) has led to unprecedented healthcare demand. This study seeks to characterize Emergency Department (ED) discharges suspected of Covid-19 that are admitted within 72 h.
Methods
We abstracted all adult discharges with suspected Covid-19 from five New York City EDs between March 2nd and April 15th. Those admitted within 72 h were then compared against those who were not using descriptive and regression analysis of background and clinical characteristics.
Results
Discharged ED patients returning within 72 h were more often admitted if suspected of Covid-19 (32.9% vs 12.1%, p < .0001). Of 7433 suspected Covid-19 discharges, the 139 (1.9%) admitted within 72 h were older (55.4 vs. 45.6 years, OR 1.03) and more often male (1.32) or with a history of obstructive lung disease (2.77) or diabetes (1.58) than those who were not admitted (p < .05). Additional associations included non-English preference, cancer, heart failure, hypertension, renal disease, ambulance arrival, higher triage acuity, longer ED stay or time from symptom onset, fever, tachycardia, dyspnea, gastrointestinal symptoms, x-ray abnormalities, and decreased platelets and lymphocytes (p < .05 for all). On 72-h return, 91 (65.5%) subjects required oxygen, and 7 (5.0%) required mechanical ventilation in the ED. Twenty-two (15.8%) of the study group have since died.
Conclusion
Several factors emerge as associated with 72-h ED return admission in subjects suspected of Covid-19. These should be considered when assessing discharge risk in clinical practice.
Keywords: Coronavirus, Patient discharge, Emergency medicine, Clinical decision-making, Pandemics, Disaster medicine
1. Introduction
Novel coronavirus disease 2019 (Covid-19) has emerged as an extraordinary challenge to the healthcare system. Early case fatality estimates for patients with Covid-19 are between 0.6% and 3.5% [1], with 3.2% reported as having required endotracheal intubation in China [2]. As Covid-19 cases continue to rise globally [[3], [4], [5], [6]], hospitals have needed to adapt their usual practices, with increased emphasis on the Emergency Department (ED) role in directing resources to where they are most needed [[7], [8], [9], [10]].
During the study period, the availability of rapid testing for Covid-19 remained limited in many parts of the United States, with many hospitals, including the study sites, utilizing these scarce tests only for patients upon admission. Instead, clinical suspicion of Covid-19 guided medical decision-making. A number of factors have been proposed as having an association with morbidity and mortality among those hospitalized: increased age, male sex, malignancy, diabetes, hypertension, chronic obstructive pulmonary disease, bilateral pneumonia, and inflammatory changes such as low platelets and increased transaminases, lactate dehydrogenase, C-reactive protein, and D-dimer [[11], [12], [13]]. For ED patients deemed stable for discharge rather than admission, however, minimal guidance exists to clarify a clinical approach to patients who remain under investigation.
In this paper, we focus on ED disposition decision-making in New York City during the Covid-19 pandemic, by identifying patients suspected of Covid-19 who are discharged yet ultimately require hospital return and admission within 72 h. This study seeks to describe the historical, clinical, and demographic characteristics that are associated with an unscheduled return to the ED for admission.
2. Methods
2.1. Study design
We performed a retrospective case-control study of ED discharges between March 2, 2020, the earliest date with public Department of Health surveillance data [14], and April 15, 2020. These discharges spanned five EDs of a single hospital system in New York City, the epicenter of the United States Covid-19 outbreak during this period [15]. We compared the characteristics of suspected Covid-19 patients discharged from the ED who then returned within 72 h for admission with those suspected Covid-19 patients discharged from the ED who did not. A nested case-control analysis was also performed for clinical characteristics of the initial ED encounter, and logistic regression was employed to determine significant predictors of 72-h return admission. Our hospital's Institutional Review Board reviewed and approved this research.
2.2. Study setting and population
We analyzed all ED visits from patients aged 18 years and above who raised clinical suspicion for Covid-19 between March 2nd and April 15th. An encounter raising clinical concern for Covid-19 was defined as (1) laboratory SARS-CoV-2 real-time reverse transcription polymerase chain reaction (rRT-PCR) or nucleic acid amplification (NAA) testing from nasopharyngeal swab specimens regardless of result, (2) clinician-entered discharge instructions pertaining to confirmed or suspected Covid-19, and/or (3) a self-isolation discharge order.
Case subjects were identified as those patients suspected of Covid-19 and discharged from the ED but who returned to an ED within the system in 72 h and required admission. Control subjects were identified as those patients suspected of Covid-19 and discharged from the ED who did not require admission within the system in 72 h. We then created a nested case-control with one control per case using single-iteration random number generation. This random sampling of controls was then compared to the larger cohort to confirm representativeness.
2.3. Study protocol
The primary outcome of this study was hospital admission within 72 h of ED discharge. Data were abstracted from the hospital's electronic medical record system (Hyperspace, February 2019, Epic Systems Corporation, Verona, WI). Zip codes were used to determine median household income through existing United States Census data [16]. In order to group listed health problems, past medical history was evaluated for key comorbidities and their associated medical terms as determined by the clinician authors.
For a nested case-control comparison of clinical features from the initial ED visit, three emergency physicians each abstracted an equal and random selection of patients from case and control groups. A brief training session was provided prior to data collection, and supervision was maintained throughout the abstraction process. Data was collected with assistance from the REDCap electronic data capture tool [17], and a sample from each reviewer's panel was subsequently reviewed by a separate abstractor to ensure uniform data abstraction. Vital signs out of reportable norm were treated as missing. Symptoms and laboratory values were noted based on previously reported manifestations of pandemic coronavirus [18]. Chest x-ray reports were manually categorized by the presence of acute pulmonary pathology as well as by multifocal distributions based on the diffuse pattern often seen in Covid-19 [19,20].
2.4. Data analysis
Prism (Version 8.4.2, GraphPad Software, San Diego, CA) was used for all descriptive statistics. Continuous variables were assessed with the unpaired Welch's t-test if normally distributed and the Mann Whitney U test if not. The χ2 test was employed for all categorical variables unless the smallest expected value within a given contingency table was less than five observations. A two-sided α of less than 0.05 determined statistical significance. Significant exposures with respect to the cohort group were then included in multivariate logistic regression using RStudio (Version 1.2.5042, RStudio, Boston, MA). Variables involving the provision of care were excluded from the model. Confidence intervals (CI) of the odds ratio (OR) were bounded at the 0.025 and 0.975-quantiles.
3. Results
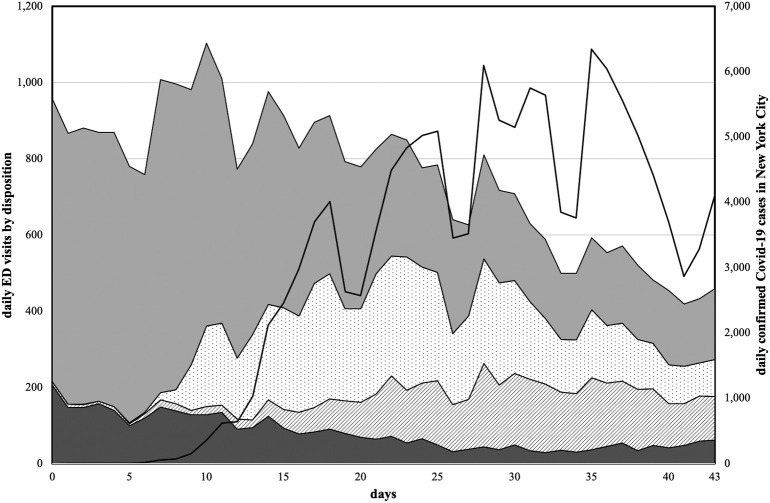
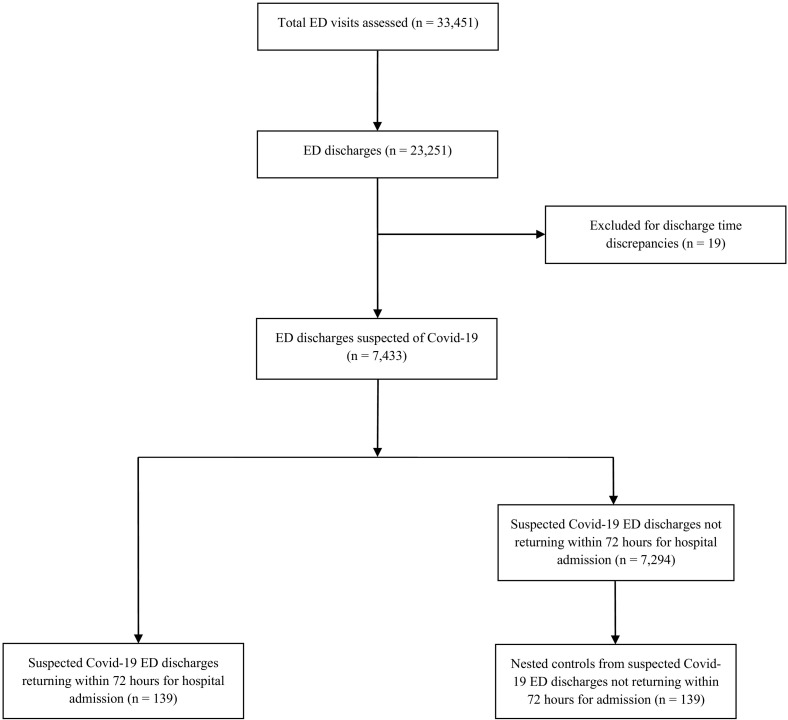
Among the 33,451 total visits to the five New York City EDs during this period (Fig. 1 ), there were 23,251 discharges: 7433 with suspicion for Covid-19 (32.0%) and 15,818 without (68.0%) (Fig. 2 ). Among those ED discharges suspected of Covid-19, 423 returned in less than 72 h. Of these, 139 (32.9%) required admission, which was significantly more than for patients who returned in 72 h without suspicion of Covid-19 (135/1115, 12.1%) (p<0.0001).
Fig. 1.
ED volume by disposition during the Covid-19 pandemic, with the stacked area plot (leftward axis) demonstrating trends in discharges and admissions over time with suspicion (dotted and striped, respectively) and without suspicion (grey and dark grey, respectively) for Covid-19. Overlying is a line graph (rightward axis) depicting those publicly available confirmed daily cases in New York City, as of May 14th.
Fig. 2.
Consort flow diagram demonstrating derivation of the study group of those suspected Covid-19 ED discharges returning within 72 h for hospital admission, the control group of those suspected Covid-19 discharges not returning within 72 h for admission, and the nested control group for direct comparison of various clinical features of the first hospital encounter. Excluded were 19 ED discharges with discrepant visit timelines that were either erroneously duplicated or should have been treated as continuous encounters.
Of the 139 case subjects discharged with suspicion for Covid-19 who returned for admission within 72 h, 90 (64.7%) were male, 31 (22.3%) were identified as African American, 105 (75.5%) listed English as their preferred language, and 58 (41.7%) relied on Medicare or Medicaid coverage (Table 1, Table 2 ). Average age was 55.4 ± 15.6 years, body mass index was 29.0 ± 6.9 for whom it was listed, and median income, as determined by zip code, was $63,005 ± $25,028. The following comorbid conditions were reported as past medical history for ten or more subjects: asthma (14.4%), cancer (9.4%), chronic obstructive pulmonary disease (7.2%), diabetes (25.2%), hypertension (38.8%), and renal disease (7.2%). For their initial ED encounter, 41 (29.5%) subjects came by ambulance, and 25 (18.0%) were triaged at an Emergency Severity Index (ESI) ≤2. ED length of stay was 5.6 ± 4.2 h.
Table 1.
Characteristics of 139 patients returning after discharge to one of five New York City EDs within 72 h for admission.
| Characteristic | 72 h return admission |
Cohort as control |
p Value |
|---|---|---|---|
| N = 139 | N = 7294 | ||
| Age, mean ± SD (n) | 55.4 ± 15.6 (139) | 45.6 ± 15.4 (7293) | <.0001 |
| Male, n (%) | 90 (64.7) | 3657 (50.1) | .0006 |
| Median household income, mean ± SD (n) | 63,005 ± 25,028 (138) | 63,334 ± 28,416 (7260) | .592 |
| Racea | |||
| White, n (%) | 27 (19.4) | 1489 (20.4) | .7742 |
| African American | 31 (22.3) | 1807 (24.8) | .5034 |
| Other/unidentified race | 81 (58.3) | 3998 (54.8) | |
| Language | |||
| English, n (%) | 105 (75.5) | 6073 (83.3) | .0161 |
| Spanish | 26 (18.1) | 947 (13.0) | .0476 |
| Other language | 5 (3.6) | 184 (2.5) | |
| Coverage | |||
| Medicare, n (%) | 27 (19.4) | 552 (7.6) | <.0001 |
| Medicaid | 31 (22.3) | 1437 (19.7) | .4454 |
| Self-pay | 36 (25.9) | 1888 (25.9) | .9968 |
| Other coverage | 45 (32.4) | 3417 (46.8) | |
| Comorbidities | |||
| Asthma, n (%) | 20 (14.4) | 798 (10.9) | .1982 |
| Cancer | 13 (9.4) | 269 (3.7) | .0005 |
| Chronic obstructive pulmonary disease⁎ | 10 (7.2) | 90 (1.2) | <.0001 |
| Congestive heart failure⁎ | 8 (5.8) | 76 (1.0) | .0002 |
| Diabetes mellitus | 35 (25.2) | 804 (11.0) | <.0001 |
| Human immunodeficiency virus (HIV)⁎ | 3 (2.2) | 124 (1.7) | .5146 |
| Hypertension | 54 (38.8) | 1444 (19.8) | <.0001 |
| Renal disease⁎ | 10 (7.2) | 253 (3.5) | .0317 |
| Thromboembolism⁎ | 2 (1.4) | 115 (1.6) | >.9999 |
| Transplant patient⁎ | 0 (0) | 14 (0.2) | >.9999 |
| BMI, mean ± SD (n) | 29.0 ± 6.9 (33) | 28.6 ± 6.3 (1562) | .7548 |
| Care provision | |||
| Ambulance arrival, n (%) | 41 (29.5) | 1316 (18.0) | .0005 |
| Emergency Severity Index (ESI) ≤2 | 25 (18.0) | 681 (9.3) | .0006 |
| Length of stay, mean ± SD (n) | 5.6 ± 4.2 (139) | 3.9 ± 4.5 (7294) | <.0001 |
Bold indicates a two-sided α of less than 0.05 determined statistical significance.
Fisher's exact test was used for determination of p-value.
Racial breakdown limited by institutional data collection.
Table 2.
Additional clinical characteristics of patients returning for hospital admission within 72-h of discharge.
| Characteristic | 72 h return admission |
Nested Control |
p Value |
|---|---|---|---|
| N = 139 | N = 139 | ||
| Home medications | |||
| ACE Inhibitor | 14 (10.1) | 12 (8.6) | .6804 |
| Angiotensin receptor blocker (ARB) | 14 (10.1) | 7 (5.0) | .1121 |
| Presenting Symptoms | |||
| Symptom duration, days | 4.8 ± 3.2 (133) | 4.7 ± 4.4 (135) | .0426 |
| Abdominal pain | 14 (10.1) | 5 (3.6) | .0324 |
| Chest pain | 28 (20.1) | 27 (19.4) | .9039 |
| Cough | 100 (71.9) | 101 (72.7) | .9705 |
| Dyspnea | 66 (47.5) | 49 (35.2) | .0384 |
| Diarrhea | 31 (22.3) | 15 (10.8) | .0098 |
| Syncope⁎ | 7 (5.0) | 1 (0.7) | .0664 |
| Vomiting | 19 (13.7) | 6 (4.3) | .0064 |
| Vital signs | |||
| Temperature ≥ 38 °C | 49 (35.3) | 26 (18.7) | .0019 |
| Mean arterial blood pressure, mmHg | 95.1 ± 11.8 (138) | 95.8 ± 12.4 (139) | .8536 |
| Heart rate ≥ 100 beats per minute | 57 (41.0) | 41 (29.5) | .0446 |
| Respiratory rate ≥ 20 breaths per minute | 48 (34.5) | 36 (25.9) | .1170 |
| Oxygen saturation < 95% | 20 (14.4) | 10 (7.2) | .0532 |
| Interventions | |||
| Steroids administered | 5 (3.6) | 5 (3.6) | >.999 |
| Antibiotics administered | 23 (16.5) | 11 (7.9) | .0280 |
| Intravenous fluids administered | 38 (27.3) | 20 (14.4) | .1186 |
| Discharged with antibiotics | 32 (23.0) | 23 (16.5) | .1754 |
| Imaging | |||
| Chest x-ray obtained | 95 (68.3) | 75 (54.0) | .0139 |
| Abnormal chest x-ray | 58 (41.7) | 37 (26.6) | .0080 |
| Multifocal positive findings on x-ray | 41 (29.5) | 20 (14.4) | .0023 |
| Laboratory studies | |||
| Brain natriuretic peptide (BNP), pg/dL | 209.4 ± 715.5 (15) | 115.0 ± 223.9 (10) | .3445 |
| C-reactive protein (CRP), mg/L | 83.9 ± 89.4 (9) | 91.3 ± 93.8 (5) | >.9999 |
| Creatinine (Cr), mg/dL | 1.0 ± 0.6 (64) | 0.9 ± 0.8 (39) | .1016 |
| D-dimer, μg/mL | 0.9 ± 0.7 (7) | 1.0 ± 0.9 (8) | .7206 |
| Glucose, mg/dL | 134.3 ± 55.7 (66) | 124.6 ± 59.5 (41) | .0364 |
| Lactate dehydrogenase (LDH), U/L | 416.0 ± 228.0 (7) | 332.6 ± 189.8 (5) | .6389 |
| Lactic Acid, mmol/L | 1.6 ± 1.3 (31) | 1.3 ± 0.3 (14) | .7939 |
| Platelets, K/μL | 207.6 ± 86.0 (64) | 266.0 ± 110.5 (40) | .0084 |
| Procalcitonin, ng/dL | 0.3 ± 0.3 (8) | 0.4 ± 0.8 (5) | .5532 |
| Troponin, ng/mL | 0.0 ± 0.0 (48) | 0.0 ± 0.0 (26) | .5807 |
| White blood cells (WBC), K/μL | 7.1 ± 3.4 (65) | 7.0 ± 3.1 (40) | .7513 |
| Neutrophils (ANC), K/μL | 5.4 ± 3.1 (65) | 4.9 ± 3.0 (39) | .4787 |
| Lymphocytes (ALC), K/μL | 1.1 ± 0.5 (65) | 1.3 ± 0.5 (39) | .0202 |
| Return visita | |||
| Return to ED within study period | 139 (100.0) | 20 (14.4) | |
| Chest x-ray obtained | 115 (82.7) | 9 (6.5) | |
| Abnormal chest x-ray | 102 (73.4) | 8 (5.8) | |
| Multifocal positive findings on x-ray | 73 (52.5) | 6 (4.3) | |
| Nasal cannula or greater | 91 (65.5) | 2 (1.4) | |
| Non-rebreather or greater | 25 (18.0) | 0 (0) | |
| Non-invasive ventilation or greater | 8 (5.8) | 0 (0) | |
| Endotracheal intubation | 7 (5.0) | 0 (0) | |
| Critical care engagement | 16 (11.5) | 0 (0) | |
| Deaths (as of May 8th) | 22 (15.8) | 1 (0.7) | |
Bold indicates a two-sided α of less than 0.05 determined statistical significance.
Fisher's exact test was used for determination of p-value.
By definition, all members of the study group returned to the ED within 72 h of discharge, and all of these patients were admitted on that subsequent encounter. The control cohort, however, includes some patients who returned to the ED within 72 h, although none were admitted.
Chest x-rays were obtained for 95 (68.3%) and 115 (82.7%) subjects on the initial and return encounters, respectively. Fifty-eight (61.1%) chest x-rays were abnormal on the initial visit, compared with 102 (88.7%) on return. Seventy-eight (56.1%) subjects had chest x-rays obtained on both the initial and return visit, enabling temporal comparison: twenty-one (26.9%) became abnormal, and 21 (26.9%) became multifocal within 72 h.
Upon 72-h ED return, 91 (65.5%) of the study group required oxygen supplementation. Sixteen (11.5%) of those deemed safe enough for discharge less than 72 h prior required engaging a critical care team or intensive care unit on reevaluation, and 7 (5.0%) required endotracheal intubation in the ED or prehospital setting. As of May 8th, 22 subjects (15.8%) had died.
When suspected Covid-19 discharges with 72-h return admission were compared to the cohort of those without, men were more likely to be admitted within 72 h (64.7 vs. 50.1%, p = .0006), as were older individuals (55.4 ± 15.6 vs. 45.6 ± 15.4 years, p < .0001) and those on Medicare (19.4 vs. 7.6%, p < .0001) or listing a language other than English as their preferred language (24.5 vs. 16.7%, p = .0161). Additionally, those returning for admission more often had the following comorbidities listed in their medical histories: cancer (9.4 vs. 3.7%, p = .0005), chronic obstructive pulmonary disease (7.2 vs. 1.2%, p < .0001), congestive heart failure (5.8 vs. 1.0%, p = .0002), diabetes (25.2 vs. 11.0%, p < .0001), hypertension (38.8 vs. 19.8%, p < .0001), and renal disease (7.2 vs. 3.5%, p = .0317). Ambulance arrival (29.5 vs. 18.0%, p = .0005), Emergency Severity Index (ESI) ≤2 (18.0 vs. 9.3%, p = .0006), and a longer ED length of stay (5.6 ± 4.2 vs. 3.9 ± 4.5 h, p < .0001) also demonstrated a greater association with admission.
A subgroup of the 7294 control cohort equal in size to the 139 case subjects was prepared in order to compare manually abstracted clinical data pertaining to the initial ED encounter. In preparing this nested control subgroup, we first evaluated the 139 randomly selected controls against the rest of the control cohort and found no statistical difference in baseline characteristics (supplement A).
Compared to the 139 nested controls, the study group more frequently reported vomiting (13.7 vs. 4.3%, p = .0064), diarrhea (22.3 vs. 10.8%, p = .0098), abdominal pain (10.1 vs. 3.6%, p = .0324), and dyspnea (47.5 vs. 35.2%, p = .0384) among their initial visit's presenting symptoms. Of treatments provided, only the administration of antibiotics was found to be associated with return admission within 72 h (16.5 vs. 7.9%, p = .0280). Fever, defined as a temperature ≥ 38 °C (35.3 vs. 18.7%, p = .0019), and tachycardia, defined as a heart rate ≥ 100 beats per minute (41.0 vs. 29.5%, p = .0446), were the two vital sign abnormalities that demonstrated a significant difference. Home angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) use was not significant.
The 139 suspected Covid-19 patients returning for admission within 72 h were more likely to have had a plain film of the chest on their initial encounter compared with the 139 nested controls (68.3 vs. 54.0%, p = .0139). For those with chest x-rays obtained, the study group had more abnormal results (41.7 vs. 26.6%, p = .0080) and more multifocal positive findings (29.5 vs. 14.4%, p = .0023) within the radiologist's documented impression. When compared with the nested controls, those requiring 72-h return admission had higher glucose (134.3 ± 55.7 vs. 124.6 ± 59.5 mg/dL, p = .0364), lower lymphocyte counts (1.1 ± 0.5 vs. 1.3 ± 0.5 K/μL, p = .0202), and lower platelet counts (207.6 ± 86.0 vs. 266.0 ± 110.5 K/μL, p = .0084) on the first ED encounter. We did not find a significant difference in brain natriuretic peptide, C-reactive protein, creatinine, D-dimer, lactate dehydrogenase, lactic acid, procalcitonin, or troponin.
In conducting multivariate logistic regression of the case subjects against the full control cohort (Table 3 ), one control was omitted due to missing data. Age was found to increase the odds of return admission within 72 h (OR 1.03 [95% CI 1.01–1.04], p < .001), as was being of the male sex (OR 1.89 [95% CI 1.32–2.70], p < .001). Chronic obstructive pulmonary disease (OR 2.77 [95% CI 1.35–5.69], p = .006) and diabetes mellitus (OR 1.58 [95%CI 1.01–2.47], p = .044) were also found to be predictive.
Table 3.
Multivariable logistic regression analysis of 72-h return admission for suspected Covid-19 discharges, demonstrating regression coefficients, odds ratios, and 95% confidence intervals of odds ratios.
| Characteristics | Coefficient | Odds ratio | 2.5% | 97.5% | p value |
|---|---|---|---|---|---|
| (n = 7433)⁎ | |||||
| Age, years | 0.03 | 1.03 | 1.01 | 1.04 | <.001 |
| Male | 0.64 | 1.89 | 1.32 | 2.70 | <.001 |
| Medicare | 0.24 | 1.27 | 0.77 | 2.10 | .347 |
| Cancer | 0.39 | 1.48 | 0.79 | 2.75 | .218 |
| Congestive heart failure | 0.79 | 2.20 | 0.98 | 4.97 | .056 |
| Chronic obstructive pulmonary disease | 1.02 | 2.77 | 1.35 | 5.69 | .006 |
| Diabetes mellitus | 0.46 | 1.58 | 1.01 | 2.47 | .044 |
| Hypertension | 0.15 | 1.16 | 0.75 | 1.80 | .493 |
| Renal disease | 0.06 | 1.06 | 0.53 | 2.14 | .868 |
Bold indicates a two-sided α of less than 0.05 determined statistical significance.
Included were those variables with p < .05 in univariate analysis. 1 result was removed due to missing data.
4. Discussion
With a documented 30,903 hospitalizations and 7563 deaths within the study period between March 2nd and April 15th [21], the burden of Covid-19 on the New York City healthcare system has been significant. While efforts to understand disease progression among hospitalized patients with confirmed Covid-19 are invaluable, the ability to safely discharge a patient is of critical importance to both ED resource stewardship and clinical practice. This analysis of suspected Covid-19 patients aimed to describe key features of the initial ED visit that may ultimately influence the likelihood of ED return for admission within 72 h of discharge.
Prior to the emergence of Covid-19, several studies assessing return admission indicated associations with increasing age, disease severity, ambulance transport, gastrointestinal or infectious disease symptoms, and prolonged time in the ED. [[22], [23], [24], [25], [26]] Many of these previous conclusions also appear to remain significant to 72-h return admission in the setting of Covid-19. Gastrointestinal symptoms predominate, for example, while increasing age, triage acuity, and ED length of stay all remain significant.
Covid-19 often presents with respiratory features, such that the association with dyspnea and the predictive value of chronic obstructive pulmonary disease were both to be expected [27]. Yet, unlike a temperature over 38 °C and a heart rate over 100 beats per minute, the initial triage vital signs of blood pressure, respirations over 20 breaths per minute, and oxygen saturation less than 95% on room air did not achieve significance for return admission. This is perhaps because of their established role in the initial disposition decision, with hemodynamically unstable or hypoxic patients unlikely to be sent home [28]. The finding may lend credence to alternative ED clinical assessments of respiratory status, such as single breath counting [29,30] and desaturation with ambulation [31,32].
Despite the clinical priority of respiratory symptoms, it is noteworthy that gastrointestinal symptoms were significantly associated with admission within 72 h of discharge. Vomiting and diarrhea are not only more readily managed through outpatient supportive care than are respiratory complaints, but, when seen in Covid-19, they may also present earlier and suggest a longer disease course in which the patient is more likely to decompensate [33,34].
Medical history also appears to be associated with 72-h return for admission. Glucose level and diabetes history, for example, were both found to be significant, consistent with a previously shown association between glycemic dysregulation and mortality [11,13]. Differences seen with histories of cancer, diabetes, and hypertension all point to a possible predisposition with metabolic derangement. Notably, we did not find an association with body mass index, despite previously reported significance [35]. However, with body mass index available for only 23.7% of cases and 21.4% of controls, and with many of those values not updated during the ED visit, our results may not have accurately captured a possible association. We also did not find an association with renal disease. We theorize that patients with chronic kidney disease may have warranted admission on initial visit and that our timeframe of 72 h may have been too short to accurately capture patients who develop acute kidney injury [36].
We did not include laboratory testing in our initial meta-analysis due to infrequent testing, however, for those that did have them drawn on the initial ED encounter, lower lymphocytes and lower platelets appeared associated with return admission. This corroborates meta-analysis and case series data suggesting an association with disease severity in both [18,37,38].
Chest x-ray remains central to early detection of disease [20]. In our study, abnormal x-rays, particularly those reported with multifocal distributions, were significantly associated with return admission in the next 72 h. Curiously, even the decision to obtain a chest x-ray in the first place proved significant, possibly indicating the overall clinical picture, or perhaps a degree of diagnostic uncertainty, not otherwise conveyed. While 26.9% of normal chest x-rays within the study group progressed to abnormality when repeated within 72 h, 1 of 3 (33.3%) controls progressed similarly, impeding meaningful conclusions on the utility of this kind of radiographic screen.
Return after ED discharge has been attributed to disease course [39], but this study has also shown that patients on federal health insurance and preferring a language other than English were more likely to return for admission within 72 h. Medicare is highly correlated with age, which likely explains why this categorical variable was ineffective in the regression analysis. Even so, these characteristics suggest a possible link to socioeconomic status that has previously been associated with return admission after ED discharge [40].
4.1. Limitations
This study has several limitations. While not considered a favorable outcome, ED return admission does not necessarily indicate an error in disposition decision [41]. All ED discharge considerations include the potential for disease progression. In times of resource scarcity, discharging patients with higher than normal potential for return admission may be necessary in order to prioritize interim bed availability. Additionally, timeframes longer than 72 h may also serve as appropriate cutoffs for reviewing ED return admissions [42]. However, the decision to rely on 72-h return was made based on its established use as a healthcare quality metric for patient recidivism [[43], [44], [45], [46]].
Additional limitations pertain to the extent to which the cohort prepared here adequately captures suspected Covid-19 cases. During the study period, health system policy changed, ultimately advising against routine viral testing in favor of discharge guidance only for those ‘persons under investigation’ (PUI), patients who could be safely discharged despite risk factors or symptoms consistent with Covid-19 [47]. We therefore relied on a combination of Covid-19 testing, discharge instructions, and a Covid-19-specific ‘self-isolation at home’ discharge order as surrogates for Covid-19 suspicion. Mirroring the ambiguity ED clinicians currently face, this study likely included some patients without disease and neglected a portion of infected individuals without typical symptoms, of which there are many [48]. Even among cases included in this study, still some may have subsequently died in the community or re-presented to outside hospitals [49], preventing analysis of their disease progression.
Finally, the very immediacy of the pandemic necessitating study of this kind also limits its generalizability. Limiting analysis to the study period prevented comparison to pre-pandemic 72-h returns. In manually abstracting data pertaining to individual ED visits, we opted for representative sampling of a nested control group aggregated from five hospitals, where case and control groups are more often selected from the same set of data and not from pooled data. Although not significantly different from the larger cohort, these nested controls may nonetheless lack true representativeness. This concern for introducing additional bias obligated their exclusion from the regression model. Similarly, in an effort to maintain clinical relevance and overcome dilutional effects, some continuous variables were converted to categorical alternatives (e.g., oxygen saturation less than 95%, based on convention), recognizing that doing so could sacrifice information [50]. Although the decision was made not to pair cases and controls temporally, the acceleration and deceleration of the pandemic wave in New York City still likely influenced the acuity of patients presenting over time.
5. Conclusion
In summary, these data suggest an opportunity for risk stratification prior to discharge of suspected Covid-19 patients. The period of time examined is unparalleled and, in New York City, unlikely to reflect the acuity, volume, and management strategies to follow. Successful implementation of more rapid and reliable testing may one day allow for definitive diagnosis in the ED, such that further clarification of these risks will be made possible. But, in this unprecedented moment, the findings detailed here may offer some guidance to those clinicians still facing these unknowns from the frontline.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
We thank Wei Zhao, M.D., M.Sc. for methodological guidance, which greatly improved the manuscript.
Author contributions
CM, SS, and NP collected data and, along with TS, wrote the manuscript, while BS, KN, and HH provided additional expertise and vision. All authors reviewed the final manuscript.
Funding information
None.
Prior presentations
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2020.08.034.
Appendix A. Supplementary data
Supplementary material: Characteristics of a nested, randomly-selected representative sample of 139 patients discharged with suspicion for Covid-19 who did not return for admission within 72 hours, compared to the larger 7,294 control group. *Fisher's exact test was used for determination of p-value. **Racial breakdown limited by institutional data collection.
References
- 1.Wilson N., Kvalsvig A., Telfar Barnard L., Baker M.G. Case-fatality estimates for COVID-19 calculated by using a lag time for fatality. Emerg Infect Dis. 13 Mar 2020 doi: 10.3201/eid2606.200320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meng L., Qiu H., Wan L., et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology. 2020 Jun;132(6):1317–1332. doi: 10.1097/ALN.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020 Feb 29;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anastassopoulou C., Russo L., Tsakris A., Siettos C. Data-based analysis, modelling and forecasting of the COVID-19 outbreak. PLoS One. 2020 Mar 31;15(3) doi: 10.1371/journal.pone.0230405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020 Apr 11;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verity R., Okell L.C., Dorigatti I., et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020 Jun;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hick J.L., Hanfling D., Cantrill S.V. Allocating scarce resources in disasters: emergency department principles. Ann Emerg Med. 2012 Mar;59(3):177–187. doi: 10.1016/j.annemergmed.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell R. Banks C; authoring working party. Emergency departments and the COVID-19 pandemic: making the most of limited resources. Emerg Med J. 2020 May;37(5):258–259. doi: 10.1136/emermed-2020-209660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenbaum L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the Epidemic’s front line. N Engl J Med. 2020 May 14;382(20):1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 10.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020 May 21;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 11.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mo P., Xing Y., Xiao Y., et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020 Mar 16 doi: 10.1093/cid/ciaa270. ciaa270. [Epub ahead of print] [DOI] [Google Scholar]
- 13.Guan W.J., Liang W.H., Zhao Y., et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020 May 14;55(5):2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVID-19: Data archive. Department of Health; City of New York: May 23, 2007. https://www1.nyc.gov/site/doh/covid/covid-19-data.page Published. Updated May 2, 2020. Accessed May 14, 2020. [Google Scholar]
- 15.United States COVID-19 cases: Reported to the CDC since January 21, 2020. Centers for Disease Control and Prevention (CDC), U.S. Department of Health & Human Services; May 6, 2020. https://www.cdc.gov/covid-data-tracker/ Updated. Accessed May 7, 2020. [Google Scholar]
- 16.U.S. Census Bureau . 2018. B19013 median household income in the past 12 months (in 2018 inflation-adjusted dollars), 2018 American Community Survey 5-Year Estimates. [Google Scholar]
- 17.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D.W., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong H.Y.F., Lam H.Y.S., Fong A.H., et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019 Mar;27:201160. doi: 10.1148/radiol.2020201160. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jacobi A., Chung M., Bernheim A., Eber C. Portable chest X-ray in coronavirus disease-19 (COVID-19): a pictorial review. Clin Imaging. 2020 Aug;64:35–42. doi: 10.1016/j.clinimag.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.COVID-19: Data archive. Department of Health; City of New York: 2020. https://www1.nyc.gov/site/doh/covid/covid-19-data-archive.page Published. Accessed May 1, 2020. [Google Scholar]
- 22.Martin-Gill C., Reiser R.C. Risk factors for 72-hour admission to the ED. Am J Emerg Med. 2004 Oct;22(6):448–453. doi: 10.1016/j.ajem.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 23.Fan J.S., Kao W.F., Yen D.H., Wang L.M., Huang C.I., Lee C.H. Risk factors and prognostic predictors of unexpected intensive care unit admission within 3 days after ED discharge. Am J Emerg Med. 2007 Nov;25(9):1009–1014. doi: 10.1016/j.ajem.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 24.van der Linden M.C., Lindeboom R., de Haan R., et al. Unscheduled return visits to a Dutch inner-city emergency department. Int J Emerg Med. 2014 Jul 5;7:23. doi: 10.1186/s12245-014-0023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hayward J., Hagtvedt R., Ma W., Gauri A., Vester M., Holroyd B.R. Predictors of admission in adult unscheduled return visits to the emergency department. West J Emerg Med. 2018 Nov;19(6):912–918. doi: 10.5811/westjem.2018.8.38225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hiti E.A., Tamim H., Makki M., Geha M., Kaddoura R., Obermeyer Z. Characteristics and determinants of high-risk unscheduled return visits to the emergency department. Emerg Med J. 2020 Feb;37(2):79–84. doi: 10.1136/emermed-2018-208343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao Q., Meng M., Kumar R., et al. The impact of COPD and smoking history on the severity of Covid-19: a systemic review and meta-analysis. J Med Virol. 2020 Apr 15 doi: 10.1002/jmv.25889. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xie J., Covassin N., Fan Z., et al. Association between hypoxemia and mortality in patients with COVID-19. Mayo Clin Proc. 2020 Jun;95(6):1138–1147. doi: 10.1016/j.mayocp.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bartfield J.M., Ushkow B.S., Rosen J.M., Dylong K. Single breath counting in the assessment of pulmonary function. Ann Emerg Med. 1994 Aug;24(2):256–259. doi: 10.1016/s0196-0644(94)70138-5. [DOI] [PubMed] [Google Scholar]
- 30.Chorin E., Padegimas A., Havakuk O., Birati E.Y., Shacham Y., Milman A., et al. Assessment of respiratory distress by the Roth score. Clin Cardiol. 2016 Nov;39(11):636–639. doi: 10.1002/clc.22586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Casanova C., Cote C., Marin J.M., et al. Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008 Oct;134(4):746–752. doi: 10.1378/chest.08-0520. [DOI] [PubMed] [Google Scholar]
- 32.Agarwala P., Salzman S.H. Six-minute walk test: clinical role, technique, coding, and reimbursement. Chest. 2020 Mar;157(3):603–611. doi: 10.1016/j.chest.2019.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan L., Mu M., Yang P., et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020 May;115(5):766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jin X., Lian J.S., Hu J.H., et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020 Jun;69(6):1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dietz W., Santos-Burgoa C. Obesity and its Implications for COVID-19 mortality. Obesity (Silver Spring) 2020 Jun;28(6) doi: 10.1002/oby.22818. 1005. [DOI] [PubMed] [Google Scholar]
- 36.Cheng Y., Luo R., Wang K., et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020 May;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lippi G., Plebani M., Henry B.M. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020 Jul;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu Y., Du X., Chen J., et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020 Jul;81(1):e6–e12. doi: 10.1016/j.jinf.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hocagil A.C., Bildik F., Kılıçaslan İ., et al. Evaluating unscheduled readmission to Emergency Department in the early period. Balkan Med J. 2016 Jan;33(1):72–79. doi: 10.5152/balkanmedj.2015.15917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gabayan G.Z., Asch S.M., Hsia R.Y., et al. Factors associated with short-term bounce-back admissions after emergency department discharge. Ann Emerg Med. 2013 Aug;62(2) doi: 10.1016/j.annemergmed.2013.01.017. 136–144.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pham J.C., Kirsch T.D., Hill P.M., DeRuggerio K., Hoffmann B. Seventy-two-hour returns may not be a good indicator of safety in the emergency department: a national study. Acad Emerg Med. 2011;18:390–397. doi: 10.1111/j.1553-2712.2011.01042.x. [DOI] [PubMed] [Google Scholar]
- 42.Rising K.L., Victor T.W., Hollander J.E., Carr B.G. Patient returns to the emergency department: the time-to-return curve. Acad Emerg Med. 2014 Aug;21(8):864–871. doi: 10.1111/acem.12442. [DOI] [PubMed] [Google Scholar]
- 43.Lerman B., Kobernick M.S. Return visits to the emergency department. J Emerg Med. 1987;5:359–362. doi: 10.1016/0736-4679(87)90138-7. [DOI] [PubMed] [Google Scholar]
- 44.Keith K.D., Bocka J.J., Kobernick M.S., Krome R.L., Ross M.A. Emergency department revisits. Ann Emerg Med. 1989;18:964–968. doi: 10.1016/s0196-0644(89)80461-5. [DOI] [PubMed] [Google Scholar]
- 45.Pierce J.M., Kellerman A.L., Oster C. “Bounces”: an analysis of short-term return visits to a public hospital emergency department. Ann Emerg Med. 1990;19:752–757. doi: 10.1016/s0196-0644(05)81698-1. [DOI] [PubMed] [Google Scholar]
- 46.Ngai K.M., Grudzen C.R., Lee R., Tong V.Y., Richardson L.D., Fernandez A. The association between limited English proficiency and unplanned emergency department revisit within 72 hours. Ann Emerg Med. 2016 Aug;68(2):213–221. doi: 10.1016/j.annemergmed.2016.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bajema K.L., Oster A.M., McGovern O.L. Et al; 2019-nCoV persons under investigation team; 2019-CoV persons under investigation team. Persons evaluated for 2019 novel coronavirus - United States, January 2020. MMWR Morb Mortal Wkly Rep. 2020 Feb 14;69(6):166–170. doi: 10.15585/mmwr.mm6906e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shy B.D., Loo G.T., Lowry T., et al. Bouncing Back Elsewhere: Multilevel Analysis of Return Visits to the Same or a Different Hospital After Initial Emergency Department Presentation. Ann Emerg Med. 2018 May;71(5) doi: 10.1016/j.annemergmed.2017.08.023. 555–563.e1. [DOI] [PubMed] [Google Scholar]
- 50.Ranganathan P., Pramesh C.S., Rakesh A. Common pitfalls in statistical analysis: logistic regression. Perspect Clin Res. 2017 Jul-Sep;8(3):148–151. doi: 10.4103/picr.PICR_87_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: Characteristics of a nested, randomly-selected representative sample of 139 patients discharged with suspicion for Covid-19 who did not return for admission within 72 hours, compared to the larger 7,294 control group. *Fisher's exact test was used for determination of p-value. **Racial breakdown limited by institutional data collection.