Abstract
There are several indications of erector spinae plane block (ESPB) for managing postoperative surgical pain. We investigated the efficacy of ultrasound-guided ESPB at T2–T3 level in five patients undergoing surgery for proximal humerus fracture and found that it provided excellent analgesia in the postoperative period. To investigate the spread of local anaesthetic at this level, we performed contrast-enhanced computed tomography studies, to understand the possible mechanism of action. We believe that ESPB at this level is a good and safe alternative to routinely used brachial plexus blocks, as it not only provides good analgesia but also spares the phrenic nerve.
Keywords: Erector spinae, shoulder, surgery, ultrasound
Introduction
The erector spinae plane block (ESPB) is emerging as a valuable regional anaesthesia technique (1). Forero et al. (2) have reported successful use of cervical ESPB for chronic shoulder pain management. Tsui et al. (3) have reported using a cervical ESPB in a high-risk patient who underwent a forequarter shoulder amputation.
Case Presentation
In a series of five patients with American Society of Anesthesiologists Physical Status I–III who underwent open fixation for the fracture of the proximal humerus, a cervical ESPB was performed after general anaesthesia induction for postoperative pain relief. Institutional Ethics Committee approval was obtained for reporting this case series. After securing intravenous (IV) access and attaching the standard monitoring, anaesthesia was induced using standard general anaesthetic protocol (fentanyl, propofol and cisatracurium). Airway was secured using an appropriately sized endotracheal tube, and anaesthesia was maintained with oxygen, air and sevoflurane over a closed circle system. IV diclofenac 75 mg was administered before the skin incision, as there was no contraindication on the basis of serum creatinine levels. Postoperatively, all patients received IV paracetamol 1 g every 8 h.
We used a linear array, high-frequency ultrasound (US) probe 2–5 Mhz Sonosite Inc.). The needle was inserted at the T2–3 level on the side of surgery, with the bevel of the needle directed cephalad. Initially 20 mL of 0.25% bupivacaine was injected, followed by the insertion of a 20-G epidural catheter to a depth of 5–7 cm from the skin. Following this, 0.1% ropivacaine was infused at 5 mL h−1 in the postoperative period for next 48 h. This provided excellent pain relief (visual analogue score, 1–2/10). Diminished pinprick and cold sensation from C3–5 to T2–3 dermatomes over the anterior, lateral and posterior parts of the neck and the cape of the shoulder was documented after ESPB in all patients.
On day 2, contrast-enhanced computed tomography (CT) studies were performed in all five patients; 5 mL of omnipaque™ (iohexol: GE Healthcare), which is a radiopaque contrast having 300 mg iodine mL−1, was diluted in 20 mL of 0.9% normal saline. This solution was injected through the pre-existing catheter. Informed consent was obtained from all patients prior to performing CT.
On analysis, we found that the contrast had spread deep to the erector spinae muscle, which is consistent with ESPB’s interfascial nature. In addition, the images demonstrated a medial retrolaminar spread, a cervical paravertebral spread reaching the cervical root at C3–4 level (Figures 1-axial section, 2-sagittal section and 3-coronal section) and a retrograde spread of the contrast in ESP along the path of dorsal rami.
Figure 1.
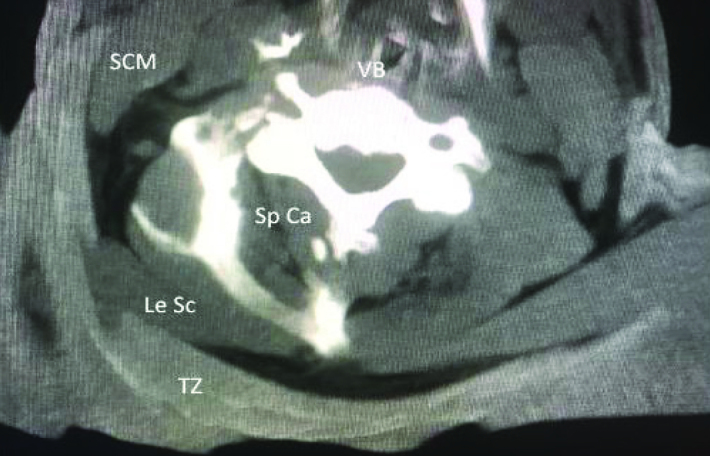
Axial section at C 5–6 level
SCM: sternocleidomastoid muscle; Le Sc: levator scapulae muscle; Sp Ca: splenius capitis muscle; VB: vertebral body; TZ: trapezius muscle
Discussion
Interscalene block is the gold standard for shoulder surgery (4). Distal phrenic sparing nerve blocks are replacing the standard analgesic interscalene technique (5). On the basis of our experience with this limited case series, we suggest that ESPB, which is probably another diaphragm sparing block, could be a viable alternative to be used in shoulder surgeries.
Conclusion
With this case series, we propose another indication of ESPB, i.e., postoperative analgesia after shoulder surgery. ESPB is a relatively easy block to perform under US guidance, with CT images depicting a consistent spread of the injectate.
Figure 2.

Sagittal section: Contrast extending from C2–T8 above ESM and at one point at T4 below ESM
ESM: erector spinae muscle; TZ: trapezius muscle
Figure 3.
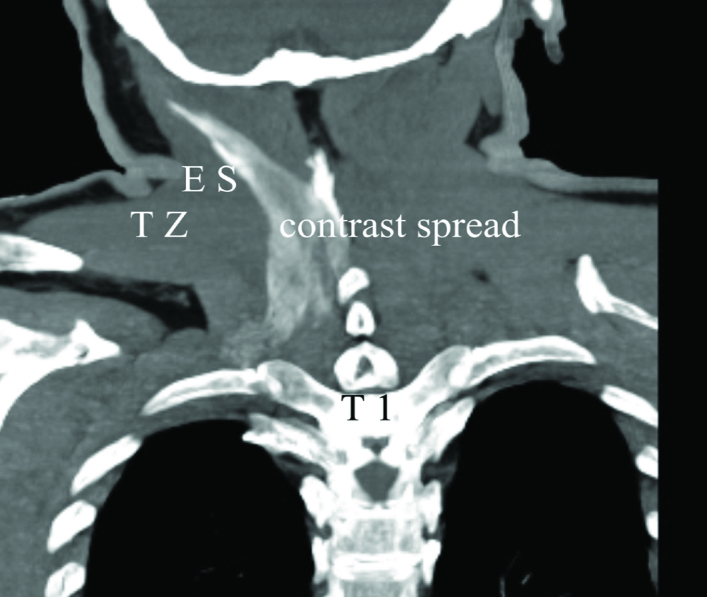
Coronal section: The contrast spread across the erector spinae plane; cephalad and caudad spreads laterally
ES: erector spinae muscle; TZ: trapezius muscle
Footnotes
Informed Consent: Written informed consent was obtained from patients who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – S.D.; Design – S.D.; Supervision – S.D.; Data Collection and/or Processing – A.N.; Analysis and/or Interpretation – S.D.; Literature Search – A.N.; Writing Manuscript – S.D.; Critical Review – S.D., A.N.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erectorspinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 2.Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: a case report. Can J Anesth. 2018;65:288–93. doi: 10.1007/s12630-017-1010-1. [DOI] [PubMed] [Google Scholar]
- 3.Tsui BCH, Mohler D, Caruso TJ, Horn JL. Cervical erector spinae plane block catheter using a thoracic approach: an alternative to brachial plexus blockade for forequarter amputation. Can J Anaesth. 2019;66:119–20. doi: 10.1007/s12630-018-1170-7. [DOI] [PubMed] [Google Scholar]
- 4.Fredrikson MJ, Krishnan S, Chen CY. Postoperative analgesiafor Shoulder surgery: a critical appraisal and review of current techniques. Anesthesia. 2010;65:608–24. doi: 10.1111/j.1365-2044.2009.06231.x. [DOI] [PubMed] [Google Scholar]
- 5.Neuts A, Stessel B, Wouters PF, Dierickx C, Cools W, Ory JP, et al. Selective suprascapular and axillary nerve block versus interscalene plexus block for pain control after arthroscopic shoulder surgery: a noninferiority randomized parallel-controlled clinical trial. Reg Anesth Pain Med. 2018;43:738–44. doi: 10.1097/AAP.0000000000000777. [DOI] [PubMed] [Google Scholar]


