Arrhythmias and other cardiovascular symptoms in patients with coronavirus disease 2019 (COVID-19) are frequently reported and are likely associated with infection-related myocarditis, ischaemia, and/or systemic proinflammatory stimulation (so-called cytokine storm). In a case series including 138 hospitalized patients, 17% (and 44% of the patients admitted to the intensive care unit) had an (unspecified) arrhythmia [1]. Moreover, medications used in COVID-19 patients may increase arrhythmic risk. We have observed fever plus relative bradycardia, i.e. an inappropriately low heart rate response to increased body temperature [2], in several hospitalized COVID-19 patients. Our primary objective was to assess the prevalence of relative bradycardia in patients with COVID-19.
We retrospectively reviewed the electronic medical records of the first 174 patients with confirmed COVID-19 (detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by real-time reverse transcriptase PCR from nasopharyngeal swabs) admitted to the University Hospital Basel, Switzerland, from 27 February 2020 to 15 April 2020. During this period, symptomatic inpatients without contraindications were routinely treated with lopinavir/ritonavir for 5 to 7 days and hydroxychloroquine for 2 days. In addition, patients with severe disease received tocilizumab. An electrocardiogram (ECG) was routinely performed at admission in all patients and again on the third day of hospitalization in all patients receiving treatment. We included in our analysis only patients primarily admitted to the ward (162 patients) and excluded a further 52 patients for the following reasons: treatment with heart rate–lowering agents (e.g. β-blockers, nondihydropyridine calcium channel blockers, amiodarone, digoxin) and conditions associated with bradycardia (e.g. hypokalemia <3.0 mmol/L) (n = 33), nonsinus rhythm on ECG (n = 7), missing ECG (n = 1) and refusal of consent (n = 11).
Relative bradycardia was defined as heart rate <90 bpm and concomitant fever (tympanic temperature ≥38.3°C), measured at least twice within 24 hours. If more measurements met these criteria, we included the measurements with the highest body temperature.
The local ethical board approved the study (EKNZ 2020-00769).
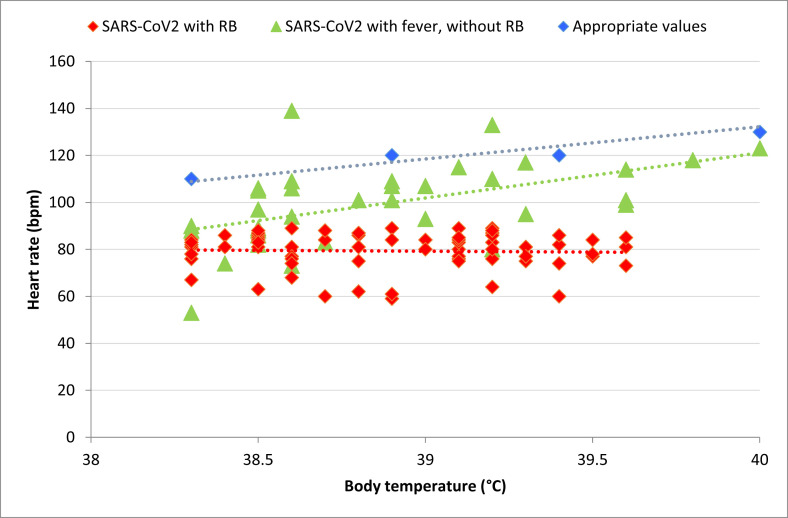
One hundred ten patients with COVID-19 (median age, 59 years; 60% male subjects) were evaluated for bradycardia. Seventy-one (64%) of the 110 patients had fever during hospitalization. Forty patients had relative bradycardia (36% of all COVID-19 patients and 56% of COVID-19 patients with fever). Relative bradycardia occurred a median (interquartile range) of 9 (6–11) days after onset of symptoms. Moreover, 38 (34%) of 110 patients had a heart rate of <60 bpm at least once during the hospital stay, regardless of body temperature (18 of the relative bradycardia group, 20 without relative bradycardia). None of the 110 patients had a QT prolongation. The temperature–heart rate relationship in patients with relative bradycardia is reported in Fig. 1 .
Fig. 1.
(A) Temperature–heart rate relationship in patients with COVID-19 and relative bradycardia; for each patient, two values with highest temperature ≥38.3°C and heart rate < 90 bpm measured in consecutive 24 hours are reported (red). (B) Physiologically appropriate temperature–heart rate relationship (blue); adapted from Cunha [2]. Temperature–heart rate relationship in patients with COVID-19 without relative bradycardia; for each patient two values with highest temperature are reported (green). Dotted lines represent linear regression between temperature and heart rate. COVID-19, coronavirus disease 2019; RB, relative bradycardia; SARS-CoV, severe acute respiratory syndrome coronavirus.
Patients with relative bradycardia were significantly older (median age, 62 years) and presented with significantly higher maximum temperatures (median, 39.3°C) compared to patients with fever and an appropriate heart rate response (49 years; 38.7°C). Otherwise, the two groups did not differ significantly regarding off-label drug treatment, oxygen therapy or laboratory findings. The clinical outcome (intensive care unit admission, intubation, death) was similar in patients with fever and relative bradycardia (20%, 18% and 3% of patients respectively) and in patients with fever and appropriate heart rate response (19%, 13% and 6%).
We found that by applying a conservative definition, 56% of hospitalized COVID-19 patients with fever had relative bradycardia. A recently released study of 54 Japanese patients with mild to moderate COVID-19 used a broader definition (not requiring the presence of fever or a minimal temperature) and also showed that relative bradycardia was a common characteristic [3].
Typically the heart rate increases by about 10 bpm for each Fahrenheit degree increase in body temperature above 101°F (38.3°C). The appropriate heart rate with a body temperature of 38.3°C is about 110 bpm [2]. The term ‘relative bradycardia’ describes the failure of the heart rate to rise when body temperature is elevated.
Many infectious and noninfectious causes of relative bradycardia in febrile patients have been described (e.g. typhoid fever), but the pathogenesis of this phenomenon is still unknown. Direct pathogen effects on the sinoatrial node and effects of inflammatory cytokines are among the proposed mechanisms [4]. Interestingly, interleukin 6 (IL-6) is the cytokine reported to exhibit the strongest correlation with depressed heart rate variability, which in turn may predict relative bradycardia [4]. On the other hand, IL-6 appears to play also an important role in the cytokine storm caused by SARS-CoV-2.
A recent report described the development of sinus bradycardia in 8 of 26 patients with severe COVID-19 pneumonia (without mentioning the presence of fever). The authors postulated an inhibitory effect of SARS-CoV-2 on sinus node activity [5].
In conclusion, relative bradycardia is a frequent clinical feature of COVID-19, occurring in 56% of febrile patients hospitalized on our hospital's wards. This fact should be taken into account while evaluating febrile patients in the context of a possible SARS-CoV-2 infection. Relative bradycardia in non–critically ill patients does not appear to be associated with a worse clinical outcome.
Transparency declaration
All authors report no conflicts of interest relevant to this letter.
Editor: L. Leibovici
References
- 1.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cunha B.A. The diagnostic significance of relative bradycardia in infectious disease. Clin Microbiol Infect. 2000;6:633–634. doi: 10.1046/j.1469-0691.2000.0194f.x. [DOI] [PubMed] [Google Scholar]
- 3.Ikeuchi K., Saito M., Yamamoto S., Nagai H., Adachi E. Relative bradycardia in patients with mild-to-moderate coronavirus disease, Japan. Emerg Infect Dis. 2020 doi: 10.3201/eid2610.202648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ye F., Winchester D., Stalvey C., Jansen M., Lee A., Khuddus M. Proposed mechanisms of relative bradycardia. Med Hypotheses. 2018;119:63–67. doi: 10.1016/j.mehy.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Hu L., Gong L., Jiang Z., Wang Q., Zou Y., Zhu L. Clinical analysis of sinus bradycardia in patients with severe COVID-19 pneumonia. Crit Care. 2020;24:257. doi: 10.1186/s13054-020-02933-3. [DOI] [PMC free article] [PubMed] [Google Scholar]