Abstract
The global pandemic has an inherently urban character. The UN-Habitat's publication of a Response Plan for mollification of the SARS-CoV-2 based externalities in the cities of the world testifies to that. This article takes the UN-Habitat report as the premise to carry out an empirical investigation in the four major metro cities of India. The report's concern with the urban character of the pandemic has underlined the role of cities in disease transmission. In that wake, the study demarcates factors at the sub-city level that tend to jeopardize the two mandatory precautionary measures during COVID-19 – Social Distancing and Lockdown. It investigates those factors through a Covid Vulnerability Index. The Index devised with the help of Analytic Hierarchy Process demarcates the low, moderate, high, and very high vulnerable city sub-units. Secondly, UN-Habitat's one of the major action areas is evidence-based knowledge creation through mapping and its analysis. In our study, we do it at a granular scale for arriving at a more nuanced understanding. Thus, in harmony with the UN-habitat's we take the urban seriously and identify the gaps that need to be plugged for the pandemic cities of now and of the future.
Keywords: UN-Habitat, COVID-19, Social distancing, Lockdown, Metro cities, Covid Vulnerability Index
Highlights
-
•
COVID-19 has an inherently urban character as UN habitat's Response plan says.
-
•
Social Distancing and Lockdown are jeopardized when basic needs not met inside house premises.
-
•
Covid Vulnerability Index devised using Analytic Hierarchy Process.
-
•
Demarcation of vulnerable areas to prevent recent pandemic and that of the future.
-
•
The investigation can be reproduced in studying cities of the developing world.
1. Introduction
The Coronavirus Disease (COVID-19) pandemic has wreaked havoc in the life of global citizens. It has led to standing still of the economy (Fong et al., 2020) and social being, and has aggravated life, health, and livelihood vulnerabilities. The SARS-CoV-2 virus has its origin in one of the prominent urban centers of China – Wuhan (Ogen, 2020) from where it has spread across the globe, penetrating indiscriminately through the cities of global north and south. In a recently published response plan for COVID-19, UN-Habitat has underlined the urban-centric character of the infectious disease (UN Habitat, 2020). It says, more than 1430 cities are affected by the pandemic in 210 countries and well above 95% of the total cases are located in urban areas. In its response to the exclusively urban character of the pandemic, UN-Habitat has embarked upon charting city-level action plan for the diminution of the disease. It comes in the pertinent moment when WHO has emphasized that the pandemic's first transmission happened in the megacities that are connected internationally (WHO, 2020).
The cities across both the north-south divide have felt the disease-induced brunt uniformly. For instance, a global city (Sasssen, 1991) like New York has crossed 3.5 Million positive cases and has recorded more than 30,000 deaths as of 10th June 2020 (The New York Times, 2020). On the other hand, the large metropolis of South Asia, Mumbai, has 51,100 positive cases with 1760 deaths as of 10th June 2020 and has exceeded that of pandemic's epicenter – Wuhan (Gupta & Chitnis, 2020). In cities, those sectors having more dilapidated living and deprived conditions, are most susceptible to transmission. On the other hand, hill cities in the Himalayas are experiencing vulnerability due to the dearth of level land on which social distancing can be fruitfully maintained (Gupta, 2020). The sloping land where homes are clumsily and proximately lined restricts such an exercise. Asia's largest slum Dharavi, in Mumbai, is reeling with a large number of positive cases but recently has shown some sign of control (Gupta & Chitnis, 2020). The overall condition in India is such that out of 5000-odd cities, only 30 cities have registered 79% of the total cases (PTI, 2020). Besides, in a much recent report by Indian Council of Medical Research, the apex medical body in India, the risk is 1.09 times higher in urban areas and 1.89 times higher in urban slum-like conditions vis-a-vis the rural areas (Swarajya, 2020).
Even though there is urban universality of the disease, the cities of the global south are more susceptible to it as for their population densities, low income and meager savings, risky occupations, and lack of affordable health services (Mitlin, 2020). In the global south, as UN-Habitat says, the Asia-Pacific region could be the most susceptible region owing to its fast urbanization rate and a large concentration of urban poverty with one-third of urban dwellers in slums or slum-like conditions (UN Habitat, 2020). In such circumstances, UN-Habitat's one of the major action areas in response to the pandemic is the provision of ‘urban data evidence-based, mapping and knowledge for informed decision making’ (UN Habitat, 2020). This article coheres around UN-Habitat's concern with Asia-Pacific and its major plan to generate evidence-based knowledge. Besides, the piece also expands the perspective window by generating COVID-19 related evidence for a more granular scale – at the sub-city level.
The global pandemic's most certain prevention is ‘Social Distancing’ that restricts the transmission from one person to the other (Fong et al., 2020; Wasdani & Prasad, 2020). To make social distancing more effective, the governments all over the world have resorted to a lockdown (Paital, Das, & Parida, 2020), wherein the physical mobility is curtailed and routine businesses are regularized. India had experienced a countrywide complete lockdown for 68 days from 25 March 2020 to 31 May 2020. The city neighbourhoods that are deprived of civic, hygienic, and sanitation services are seemingly more susceptible to the transmission and consequently the more vulnerable. Besides, the fast pace of urbanization in India has led to housing shortfalls and severe stress due to the paucity of water, electricity, and open space (Mayank, Nanavaty, Chakraborty, Mitra, & Limaye, 2012).
In this article, we empirically show how the mandatory pandemic precautions – social distancing and lockdown-are thwarted when the most deprived households in the four metro cities have to cram in the residence with neither prescribed inter-mutual distance nor any chance of isolation, and the urgency to move out of the premises for meeting the water need and attend to nature's call. These vulnerable factors aggravate more if the conditions of untreated water (Naddeo & Liu, 2020; UN Habitat, 2020) and population density (PTI, 2020; Rocklöv & Sjödin, 2020) are favorable for the transmission.
Thus, the article contributes in two ways – firstly, by extending the vulnerability question of cities induced by UN-habitat into domains that directly jeopardize our efforts (i.e., social distancing and lockdown) to restrain the global pandemic. And, secondly, it does the exercise at a more granular level to generate a more reliable ‘evidence-based knowledge’ that the UN-Habitat seeks in its endeavor to curb COVID-19.
2. COVID-19 and urban geographies
The researchers and scholars reiterate UN-Habitat's observation of the urban character of the global pandemic. For instance, an article published in The Economist that talks of COVID-19 in the cities of the global north such as London, New York, and Milan is optimistic about the pandemic's post-situation (The Economist, 2020). It posits, with references, that cities experienced with handling historical events of plague, cholera, and tuberculosis have their urban architecture patterned in sync with them. Therefore, a pandemic can do little harm in such situations.
In one of the other pieces that talks across both the global north and the global south, the author invests in channelizing our thought to the post-pandemic scenario and implications it holds in designing our cities (Constable, 2020). She insists that the ‘pandemic-resilient cities of tomorrow’ must refrain from overcrowding, as the population density is one of the main reasons for disease transmission in cities stretching from New York to Wuhan. These post-pandemic cities need to be self-sufficient as they grow with the pandemic.
Now, moving exclusively to the cities of the global south, as the moment of ‘surplus humanity’ found in its all-pervasive slum (Davis, 2006), the pandemic has more lethal consequences. COVID-19 ‘poses particular risks for the one billion people living in informal urban settlements in the global South’ as it escalates due to the presence of high-density residences and the absence of minimal civic services (Mitlin, 2020). The packed and crammed residences are supplemented by decreasing piped water to the premises, especially in Sub-Saharan Africa. Besides, with the poor income levels and zero saving the urban poor is keen on doing outdoor work keeping isolation and social distancing at bay. In their study of Bangalore slums in India, Wasdani and Prasad (2020) underline the impossibility of slums to maintain social distancing at any cost. They observe that slums are more at risk because of the population density and regular wage-earning nature of the dwellers. The population density and the need to move out for the sake of livelihood and sustenance compromise the sole important precaution – Social Distancing - in pandemic times.
When, the average population density of India is 384 persons per square kilometer, Asia's largest slum Dharavi reels under the pressure of 3,35,907 persons per square kilometer (Nutkiewicz, Jain, & Bardhan, 2018). Such is the potentiality of the slum to transmit disease that it soon became a piece of news when the first case was reported (Yashoda, 2020). Slums that are all-pervasive in South-Asia may meet the same fate sooner or later. In foresight, Corburn et al. (2020) have suggested policies and a prescription for not only tackling the ensuing pandemic but also for the post-endemic circumstances.
However, a slum, especially in the south Asian context, need not only be determined by the statute but must be demarcated based on deprivation indicators (Patel, Koizumi, & Crooks, 2014), which includes large scale devastating situation that uncontrolled population growth in urban areas could bring (WHO & UN-Habitat, 2016). Thus, in this article, we move beyond the limitation formal slums put on grasping and generating evidence-based knowledge by adopting a deprivation based empirical investigation. The deprivation indicators are directly linked to the pandemic's principal precautionary measures of social distancing and lockdown.
3. Research objectives
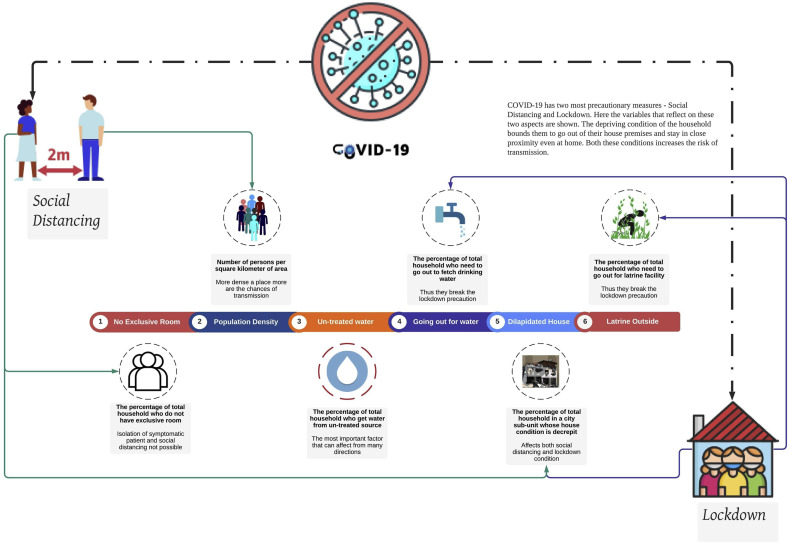
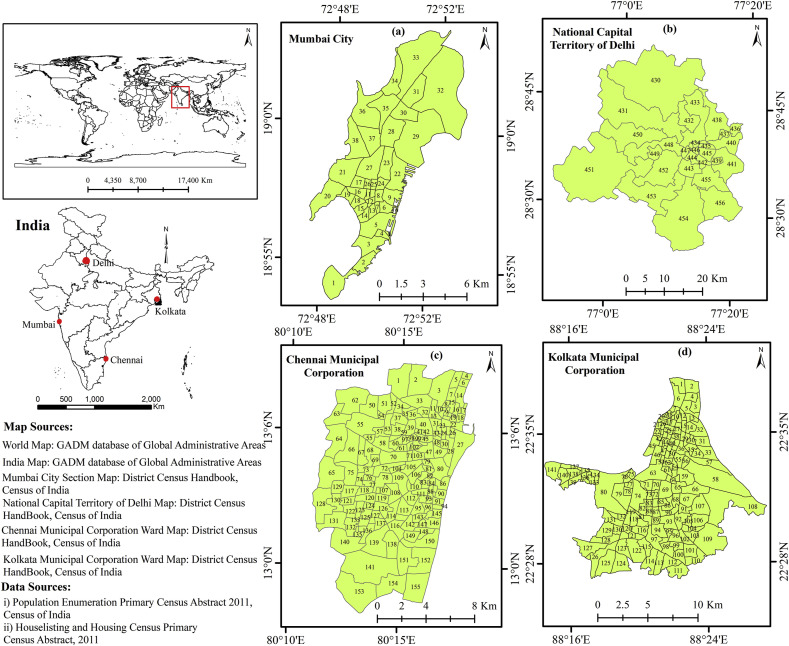
The article realizes two objectives (Fig. 1 ). Firstly, in harmony with the UN-Habitat's concern with the urban nature of the pandemic and implication it holds for the already deprived people, we have devised a set of deprivation variables that tends to make the population vulnerable to COVID-19 transmission. The indispensable measures like social distancing and lockdown are defeated with crammed indoor living in a densely populated area along with the urgency of moving outside the house premises for basic human needs like drinking water and latrine facility. Thus, we emphatically investigate the variables that not only mark the limit of deprivation but also couple as the most susceptible to COVID-19 transmission. We have devised a Covid Vulnerability Index for four major metro cities of India –Mumbai, Delhi, Kolkata, and Chennai (Fig. A1). At the time of writing the piece, these four cities account for nearly 50% of the country's covid cases (PTI, 2020). In one recent study (Patel, 2020), the author has assessed ‘the effectiveness and implications of social distancing, frequent handwashing, and lockdown in the context of slums in Indian cities’. The study merges with our first objective and we supplement it with inclusion of variables at the city sub-unit level.
Fig. 1.
COVID-19 mandatory precautions and its link to the variables under study.
Secondly, in tandem with the UN-Habitat's call for an evidence-based knowledge, we have embarked on generating an empirical investigation of COVID-19 related indicators for the four metro cities of India. In that vein, we have supplemented it by investigating at a more granular scale for the city. By granularity, we identify with those spatial units that are found at sub-city scale. Thus, using the latest Census data, we have identified variables and procured data at the municipal ward, section, and tehsil 1 level for all the four cities. Therefore, the results give a more detailed and robust picture of the vulnerability situation wherein the UN-habitat's mission for city-based knowledge becomes finer and more decision-enabled.
4. Database and methodology
4.1. Data preparation
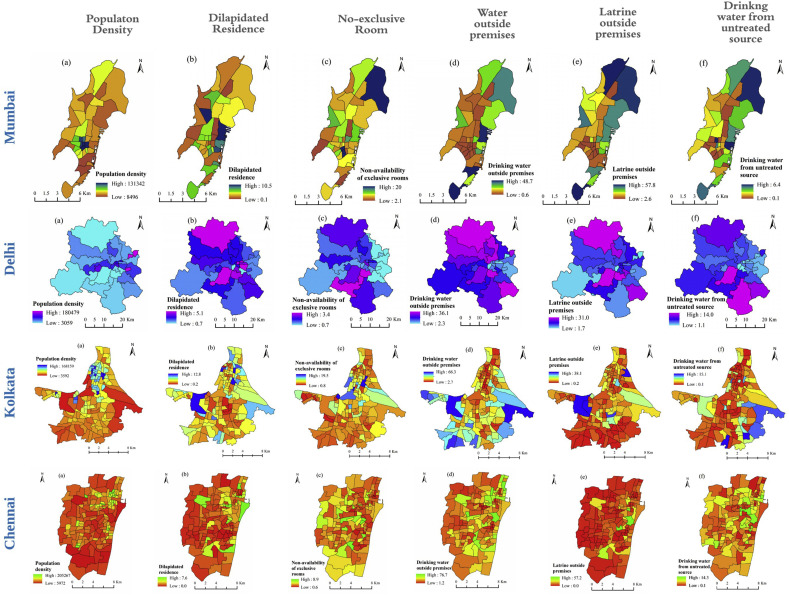
Different variables related to COVID-19 precaution is considered for this study under the broad categories of social distancing, lockdown, and direct health (Table 1 ). Ward wise data for Kolkata Municipal Corporation (KMC), Chennai Municipal Corporation (CMC), section-wise data for Mumbai City (MMC), and tehsil level data for National Capital Territory of Delhi (NCT) is collected from the Population Enumeration's Primary Census Abstract 2011, Census of India (CoI), and House listing and Housing Census's Primary Census Abstract, 2011 Census of India (CoI) (Fig. 2 ). Under the social distancing category, three variables are selected. The first one is population density, which is an important consideration in infectious diseases (Ai, Zhang, & Zhang, 2016; Alaniz, Bacigalupo, & Cattan, 2017; Jia et al., 2020). In COVID-19 a preliminary investigation has found that population density can have a large impact on transmission through contact rates (Rocklöv & Sjödin, 2020). We have not taken the more sophisticated measures of population density for keeping the device simple, applicable in multiple contexts, and the dearth of such data for all the cities. The second variable, dilapidated residence, has material, physical and mental health (Chan & Ma, 2020) dimensions. In dilapidated conditions, there are more chances that inter-mutual distance is compromised as the house condition inhibits spreading to secluded corners. Secondly, dilapidated conditions are also known to aggravate the respiratory ailments like asthma (Ernie, 2005) and given its direct link to COVID-19 susceptibility (AAAAI, 2020; Johnston, 2020), this variable seem to be of direct concern. We have kept it as a social distancing variable as for the absence of secluded corners and compulsion of people with respiration problem to move out for the cleaner air. Non-availability of exclusive rooms even in a non-dilapidated house inhibits not only social distancing but also hinders the prescribed isolation of symptomatic patients. Lockdown category includes the location of drinking water facility outside the premises thus jeopardizing the lockdown with high chances of transmission as people need to move out. Similarly, for latrine outside the premises not only there is an undermining of lockdown but in places where community toilets are attended the social distancing goes awry. On the other hand, untreated source of drinking water is measured as the most important variable after population density as water being a potential carrier of the virus can transmit more if it is untreated (Naddeo & Liu, 2020). As a matter of fact, WHO in one of its interim guidance has clarified that water disinfection is needed for the reduction of the coronavirus (WHO Global, 2020). It is treated as the direct health variable with significant health implications (Table 1).
Table 1.
Variables considered for the Covid Vulnerability Index.
| COVID-19 Precaution | Variable | Description |
|---|---|---|
| Social Distancing | Population Density | persons per square kilometer |
| Dilapidated residential house condition | percentage of total households in a city sub-unit whose house condition is decrepit | |
| No exclusive room | percentage of total households in a city sub-unit who do not have an exclusive room for living in their house | |
| Lockdown | Main source of drinking water – away from the premises | percentage of total households in a city sub-unit who need to go at least 100 m from their house to fetch drinking water |
| Number of households not having latrine facility within the premises | percentage of total households in a city sub-unit who need to go outside their house for availing latrine facility | |
| Direct Health Variable | Drinking water from un-treated source | percentage of total households in a city sub-unit who get water from an untreated source |
Fig. 2.
The city sub-unit wise distribution of variable values.
4.2. The Covid Vulnerability Index
The study proposes a Covid Vulnerability Index by aggregating the weighted scores of each of the above-said variables for each of the sub-units of the four metro cities. To derive the weights of each of the variables we have employed Analytic Hierarchy Process (AHP). It is an extensively used Multi Criteria Decision Making (MCDM) technique in different disciplines owing to its feasibility in calculation that helps in decision making by a host of government and non-government agencies (Dos Santos, Neves, Sant’Anna, Oliveira, & Carvalho, 2019; Omar, Bushby, & Williams, 2019). It is because of this computational convenience and pervasive understanding that we chose the method over modified AHP (Lyu, Sun, Shen, & Arulrajah, 2018, 2020) and other MCDM techniques like PCA (Earnest et al., 2015) or the more robust and spatial variant of it – Geographically Weighted Principal Component Analysis (GWPCA) (Basu, Das, & Pal, 2020; Das et al., 2020; Mishra, 2018). Other techniques like Slum Severity Index (Patel et al., 2014, 2019, 2020) that is being recently developed and applied in multiple contexts along with deviating from only slum based indices, is also a simpler option for computation and drawing inferences.
However, AHP has certain advantages like it helps integrate the ‘domain-related knowledge’ into the model (Gharizadeh Beiragh et al., 2020) and as a corollary to that, it helps take cognizance of the contextuality of the space under investigation (Dos Santos et al., 2019). It is because of its ‘simplicity, ease of use, and great flexibility [that] the AHP has been studied extensively’ (Gharizadeh Beiragh et al., 2020) and motivated us to induct it in our study. Besides, it is widely used in social science and health research. For instance, AHP is used for effective policy intervention in Ghana (Baffoe, 2019) and for gauging ZIKA risk assessment in China (Li et al., 2017) or dengue risk assessment in tropical Malaysia (Dom, Ahmad, Latif, & Ismail, 2016).
Analytic Hierarchy Process was developed in the 1970s by Thomas L. Saaty (1980), which has developed as a powerful multi-criteria decision method over the years. It is modified and made more robust with improvements in recent times (Lyu, Zhou, Shen, & Zhou, 2020, 2020; Saha, Gayen, Pourghasemi, & Tiefenbacher, 2019). In this method, the decision analysis is decomposed into different levels like a hierarchy. At the first level is the Goal or the Object Layer which ascertains locating the vulnerable city sub-units that are susceptible to COVID-19 transmission now and also in the pandemic cities of the future. The second level, Criteria, is divided into Index Layer and Sub-Index Layer. The Index Layer is the variables under consideration and Sub-Index Layer is the factor class i.e., classification of variable values. The third level is the Alternative Layer that gives different options available for making decisions.
The AHP is conducted in four steps. First, the hierarchical structure is ascertained with definite goals and criteria. The second step is to create a Pairwise Comparison Matrix (Equation (1)) for the assessment of vulnerability factors and their relative importance which is then normalised. Generally, it is used for ranking the attributes to select the optimal one based on the hierarchical structure with numbers ranging from 1 to 9 and their reciprocal. If variable population density (pd) is more important than variable dilapidated residence (dil) for covid vulnerability, the degree of importance of variable “population density” to “dilapidated residence” is assigned 9. Also, the degree of importance of factor “dilapidated residence” to “population density” is assigned reciprocal value 1/9. It is in this step that we derive weights of each of the variables (Wahp) and their factor classes (Wfc) (Table 2 ).
| (1) |
Where, pd stands for population density, dil for dilapidated housing, ldp for latrine outside premises, dwn for drinking water from an untreated source, ner for non-availability of exclusive rooms, and dr for drinking water outside premises.
Table 2.
Weights of assessment factors calibrated from AHP.
| Index layer |
Sub-index layer |
Consistency Ratio (CR) | ||
|---|---|---|---|---|
| Index | Weights (Wahp) | Factor class | Weights (Wfc) | |
| Population density (pd) | 0.329 | <10,000 | 0.071 | 0.039 |
| 10,000–30,000 | 0.152 | |||
| 30,000–70,000 | 0.313 | |||
| >70,000 | 0.463 | |||
| Drinking water outside premises (dr) | 0.229 | <10 | 0.068 | 0.011 |
| 10–20 | 0.167 | |||
| 20–30 | 0.280 | |||
| >30 | 0.485 | |||
| Latrine outside premises (lpd) | 0.229 | <10 | 0.060 | 0.054 |
| 10–20 | 0.128 | |||
| 20–40 | 0.274 | |||
| >40 | 0.538 | |||
| Drinking water from untreated source (dwn) | 0.102 | >3 | 0.078 | 0.018 |
| 3–7 | 0.125 | |||
| 7–12 | 0.306 | |||
| >12 | 0.492 | |||
| Non-availability of exclusive rooms (ner) | 0.071 | >3.0 | 0.062 | 0.030 |
| 3.0–9.5 | 0.114 | |||
| 9.5–15.5 | 0.271 | |||
| >15.5 | 0.553 | |||
| Dilapidated housing (dil) | 0.041 | >4.5 | 0.067 | 0.038 |
| 4.5–8.5 | 0.149 | |||
| 8.5–10.5 | 0.325 | |||
| >10.5 | 0.460 | |||
The third step is to check the consistency of the calculation by calculating the Consistency Ratio (CR). Its value varies between 0 and 1. A CR value below 0.1 reveals the consistency of the matrix or elimination of type II error (Saaty, 1980; Saha et al., 2019). In our study, the CR value of the matrix is 0.032 (less than 0.1), representing that the priority matrix is consistent. The relative importance of variables, CR, and pairwise comparison matrix calculation methods are elaborated in the literature (Lyu et al., 2020; Saaty & Vargas, 2001).
The weights that we derived in the second step helps generate the Covid Vulnerability Index. It is the product of weights i.e., the variable weight and the factor class weight (Table 2) computed for each of the city sub-units (Equation (2)).
| (2) |
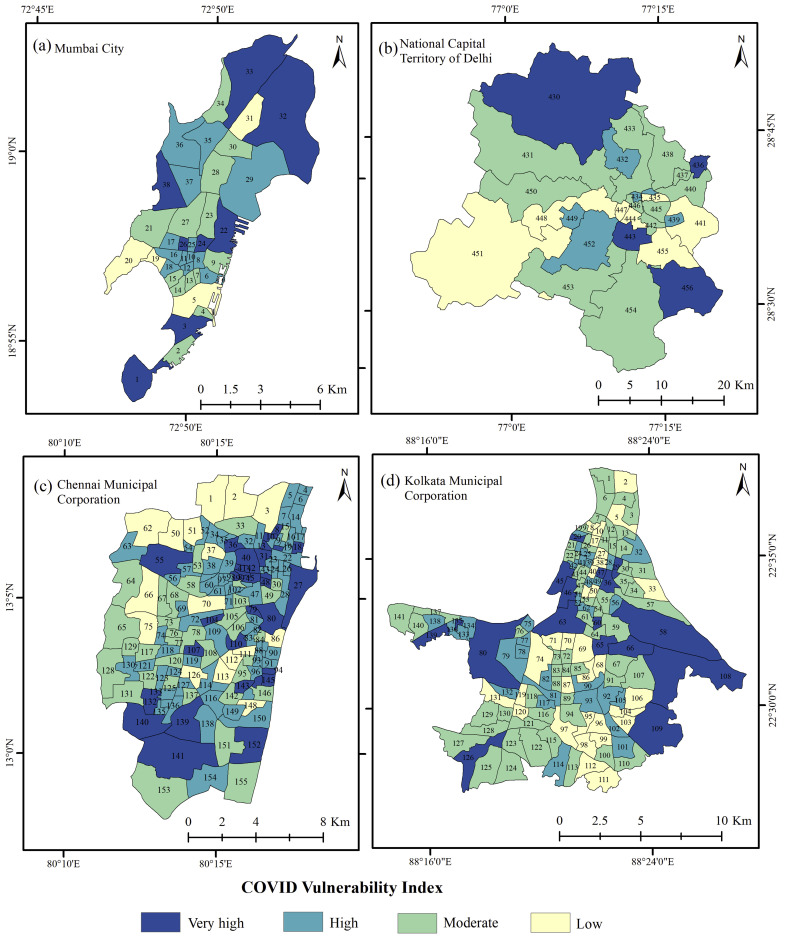
where CV index is the Covid Vulnerability Index, Wahp is the weight of each COVID-19 induced vulnerability conditioning factor and Wfc is the weight of each of the factor class for each of the variables. Finally, based on the Index computation a COVID-19 induced vulnerability index map is generated for the four metro cities in India. The vulnerability index values are categorised into 4 classes by applying Jenks natural breaks classification (Shahabi, Khezri, Ahmad, & Hashim, 2014). These are very high, high, moderate, and low vulnerability zones (Fig. 3 ).
Fig. 3.
The Covid Vulnerability Index.
4.3. Validation
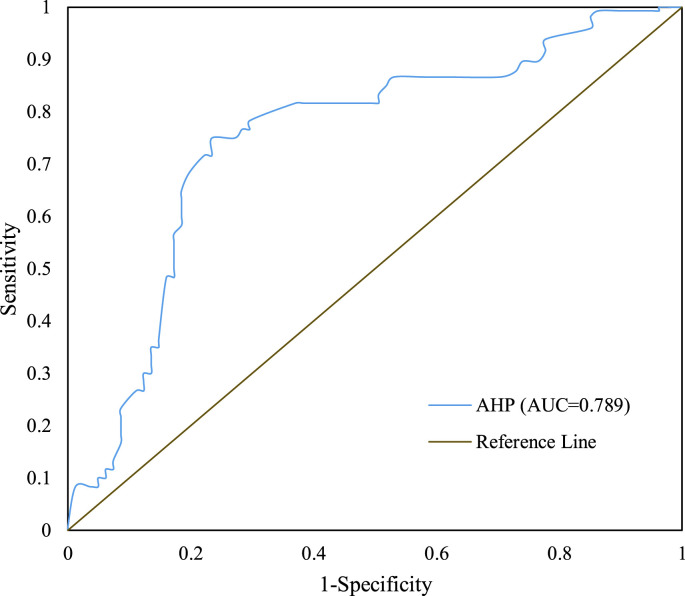
Receiver Operating Characteristics (ROC) curve is used for the verification and validation of the model (Pourghasemi, Gayen, Edalat, Zarafshar, & Tiefenbacher, 2020; Pourghasemi, Pouyan, et al., 2020). It juxtaposes the validation dataset with the model output (Gayen, Pourghasemi, Saha, Keesstra, & Bai, 2019). In our study, the number of containment zones in each of the city sub-units is considered as the validation dataset. The ROC curve and the area under the curve (AUC) are categorised into five classes. The classes are poor (0.5–0.6), moderate (0.6–0.7), good (0.7–0.8), very good (0.8–0.9), and excellent (0.9–1.00) (Pourghasemi, Pouyan, et al., 2020).
In our study, we have used the validation dataset for Kolkata because for the validation purpose it is mandatory to have both the datasets at a uniform scale. In all the other cities the number of containment zones is not provided at the scale of our study. The condition arises because of the existing gap in the conception of the administrative city between the Urban Local Bodies and the Census of India. Besides, since the model seeks to arrive at a vulnerable quotient for each of the city sub-units, a sample validation will serve the purpose.
5. Result and discussion
The discussion section is done individually for each of the metro cities, wherein we proceed with discussing the model output followed by a brief discussion on the facets from literature and observations. The last sub-section talks of model validation for which, as said earlier, we have chosen Kolkata as the sample.
5.1. Mumbai
The city with its intermittent spikes in COVID positive cases has earned the title of ‘India's Covid-19 hotspot’ (Shaikh, 2020) and has experienced the transmission faster than the national average. As the map shows (Fig. 3a) the very high vulnerable zones are located in the northern and the central part of the city. sections 32 (Sion) and 33 (Dadar) are the oldest parts of the city where more than 50% of the households have to go outside for latrine facility and a bit less than 20% in case of Dadar and a little less than 30% in case of Sion have to go out for getting drinking water. Section 33 is also home to Asia's largest slum Dharavi. It has recorded 1984 positive cases with 75 deaths as of 11 June 2020 (Choudhary, 2020) in an area of only 2 sq. km with more than 7 lakh people crammed (Singh, 2020). Similarly, the central section of the city with a relatively smaller area has moderate to very high vulnerability. Sections 10 to 18 (with exception of 13) have high population densities ranging between 60,000 and 1,31,342 persons per sq. km. Besides, in section 12 the percentage of households who have no exclusive room is 19%. In section 1 those who need to go outside their premises for water or latrine are abysmally high at 48.7% and 56.6%, respectively. Whereas, those who need to drink untreated water is the highest in section 26 (6.4%). Among these dismal pictures, sections like 5 (Esplanade), 19 (Chaupaty), 20 (Walkeshwar), and 31 (Matunga), are enclaves of low vulnerability. In all these sections the population density figures are remarkably low vis-à-vis other sections – 8496, 25731, 25399 and 21733 persons per sq. km, respectively. In addition, these sections have strikingly low marks in other variables. For instance, only 2.1% of the households in section 9 and 2.2% of the households in section 31 need to go out for fetching water. And, the highest among these wards for latrine outside premises is section 20 (16.5%), which is much less than the city average (33%).
With around 50% of persons living in slum conditions in Mumbai (Bardhan, Sarkar, Jana, & Velaga, 2015) with very low freshness quotient (Bardhan, Debnath, Jana, & Norford, 2018) the city is certain of defying the mandatory precautions until and unless rarely stringent actions are taken through governance. Areas like Dharavi slum and Khara Talao which are historically subaltern and consequently downtrodden (Kidambi, 2007, pp. 1890–1920) are more vulnerable because of the global pandemic that requires physical distance and zero cohesiveness. As understood from prior studies, Mumbai's main concern is with regard to the water supply that is astutely dealt with through rainwater harvesting by the middle class but cannot be emulated by the poor for the dearth of space (Button, 2017). The municipality has embarked on supplying water through self-organised groups; nevertheless, the piped water supply to the house premises is a distant dream for the people. Therefore, Mumbai has one of the highest waiting times and carrying distance of water to the household premises in India (Graham, Desai, & McFarlane, 2013). Secondly, the city with very dense informal settlements ought to have inevitable toilet shortages. Community-based approaches like Slum Sanitation Program (McFarlane, 2008) and community-led initiatives by Indian Alliance (Tomlinson, 2015) have borne fruit but the endeavour is short of achieving universal access. As a consequence, many of the residents openly defecate in Mumbai (Desai, McFarlane, & Graham, 2015). The COVID-19 induced mandatory precaution gets defeated as and when a person goes out for latrine facility or getting water; and, community toilets are transmission hotspots as the inter-mutual distancing is reduced to zero.
5.2. Delhi
At the time of writing this article, the National Capital Territory of Delhi is the only city with complete containment with all the districts of the city-state declared a red zone2 (PTI, 2020). The Covid vulnerability pattern shows clustering of similar zones – high vulnerability in contiguity with high or very high vulnerability (Fig. 3b). And, low vulnerable zones follow a linear pattern from the west to the east. Tehsils 430 (Narela), 436 (Seelam Pur), 443 (Chanakya Puri), and 456 (Kalkaji) are high vulnerable zones. Even though the population density is quite low in tehsils 430 (3059 persons per sq. km), 443 (12138 persons per sq. km) and 456 (12980 persons per sq. km), the other covid variables have shot up the vulnerability quotient of these city sub-units. For instance, in tehsil 430 more than 25% of the households need to go outside the premises for latrine facilities and more than 36% of them need to go outside for fetching drinking water. Similarly, in tehsil 443 the percentage is 31% and 30%, respectively. In tehsil 456, the percentage of those who need to move out for drinking water is 30.7%, around 12% of the total households drink untreated water and more than 23% of them go outside the premises for latrine facilities. However, in tehsil 436 the population density (180479 persons per sq. km) is the highest in the city, which couples with more than 28% of households moving outside for fetching drinking water to make the picture more appalling. On the other hand, low vulnerable zones are restricted to tehsils 435 (Kotwali), 441 (Preet Vihar), 444 (Parliament Street), 447 (Karol Bagh), 448 (Patel Nagar), 451 (Najafgarh), and 455 (Defence Colony). Tehsil 435 have very low figures in lockdown variables – 6.4% and 7.1% of households move outside their premises for fetching drinking water and latrine facility, respectively. In tehsil 441 all the variables have considerably low values reflecting a least depriving condition (covid variables) and consequently low vulnerability.
From earlier studies, we can find general picture of the city where the civic administration must work. For example, in one study of East Delhi, it was found that the area's per capita open space is remarkably less than the prescribed level by the UN and WHO (Shahfahad et al., 2019), in which tehsils 439 (high covid vulnerable) and 440 (moderate covid vulnerable) falls. Open defecation is a major concern in the capital. Despite being declared Open Defecation Free in 2017, most of the areas of the city have usual sight of such deeds (Ravi, 2018). As a matter of fact, in a study of 476 cities concerning open defecation and solid waste management, Delhi's rank is devastatingly 398. Even though the city has ubiquity in public toilets, most of them are either too unclean to attend or the lack of water makes their utilisation impossible (Upadhyay, 2020). On the front of drinking water, Delhi does not fare well. Delhi has a huge disparity in planned provisioning of water (Das Gupta et al., 2019) and nearly 20% of the total population has no access to drinking water (Saroj, Goli, Rana, & Choudhary, 2020).
Delhi was very prompt in dealing with the pandemic. The administration closed the schools, colleges, universities, and places of entertainment on 12 March 2020 until 31 March 2020 (Jain, 2020). Nevertheless, at the time of writing this piece, the national capital was totally under the control of the disease and the federal government had declared the whole city a Red Zone – the zone of full containment (PTI, 2020).
5.3. Kolkata
The Covid Vulnerability Index gives a picture wherein the Central Business District (Wards 45, 46 and 63), the port area (wards 75 and 80), and the eastern fringe (wards 58, 108 and 109) show very high vulnerability (Fig. 3d). The most dismal picture is presented by ward 80 where 66% of the total households need to go out of their premises for fetching water and more than 38% of them go out for latrine facilities. 7% of the households live in dilapidated housing. Whereas, in ward 75 more than 13% of them have no exclusive rooms and population density is 48573 persons per sq. km. The population density is remarkably low in wards 45, 46 and 63 as they accommodate day population (for being the CBD), nevertheless, 11.4% of the households do not have exclusive room in ward 45 (this data for ward 63 is 11.3%) and more than 30% of the households need to go out for getting water in ward 46. The central and northern wards are relatively smaller than the eastern, western, or southern wards where population density is naturally higher. Nevertheless, they also show a variegated picture. For instance, in ward number 3 which houses Belgachhia slum - the ‘ground zero of the COVID battle’ (Ray, Khanna, Yengkhom, & Ghosh, 2020) – is just moderately vulnerable. The reason is the ward has only a section of it as the slum, the major section is full of greenery and middle and upper middle-class residences in a relatively open space. The moderately vulnerable wards are seen as clustering in the south, central, and eastern section. On the other hand, low vulnerable wards are less in the northern part than in the southern parts of the city. Wards from 95 to 99 (Tollygunj, Baghajatin, Golf Green, and Jadavpur area) and 69 to 71 (Ballygunge, Beckbagan, and Bhawanipur area) are the posh neighbourhoods of the city where most of the variables show a very low mark. Out of these wards, 71 has the highest percentage of those who need to move out for latrine (3.6%) and 95 has the highest population density – 31417 persons per sq. km. Both these highest are much below the city's highest – 38.1% (ward 80) and 168159 persons per sq. km (ward 135), respectively.
From earlier studies we can find that in Port area and Hastings (wards 75, 80 and 134), College Street (ward 39), Rajabazar (wards 37 and 36) and Maniktala (ward 27) the condition is deplorable due to slum concentration, congested tenements, presence of warehouses (Haque, 2013; Haque & Bandyopadhyay, 2012). On the other hand, such a condition persists in Chowringhee (wards 46 and 63) and BBD Bag-Dalhousie (ward 45) area due to the presence of slums, institutional households, and administrative buildings, mostly from the British era (Haque & Bandyopadhyay, 2012). The city with its definite geographies of deprivation has kept its fringes the most deprived in household, economic, and environmental dimensions (Mishra, 2018). In fact, despite having less crowded residences vis-à-vis Mumbai, the deprived conditions in non-slum areas are bleaker in Kolkata (Patel et al., 2014). The water-related anomaly (Ray & Shaw, 2016) and housing inequalities (Haque, Rana, & Patel, 2020) are also prominent in the city of joy. Such is the condition of water accessibility that Kolkata has the least water supply coverage among the four metro cities (Ray & Shaw, 2016). Things are not good inside the city as well. While the central and the northern parts of the city have pure water provision, the belt areas in the east, west, and south have groundwater as the primary source (Ray & Shaw, 2016).
5.4. Chennai
Chennai is one of the most densely populated cities in the southern part of the country. The marked vulnerable areas like Royapuram (ward 18), Thiru-vi-ka Nagar (ward 38), and Tondiarpet (ward 14) in the northern part of the city has already contributed to more than 50% of the total cases in the city (TNN, 2020) at the time of writing this section. These three wards have high to very high vulnerability. In general, three main clusters of high vulnerability are observed – one in the north (wards 8, 10, 13, 31, 36, 40, 41, 42, 45, 48, 55, 56, and 99) (Fig. 3c). The other two are in the east along the coast (wards 18, 27, 80, 94, 143, 145 and 152) and in the south (132, 133, 139, 140 and 141). Out of these wards, the highest population density (148476 persons per sq. km) is found in ward 10 (Kumarasamy Nagar (South)) and the highest percentage of households who need to go outside their premises for water and latrine is observed in ward 80 (Chindadripet) - 70.7% and 57.2%, respectively. On the other hand, the highest percentage of people who have dilapidated housing (7.6%) is found in ward number 45 (Thattankulam), while the highest percentage of those who drink untreated water (9.5%) is highest in ward 18 (Royapuram). As a matter of fact, the most depriving condition in all these wards is with regard to those who need to move out of their premises for getting drinking water, which ranges starkly between 26.8% and 70.7% as against the city average of 23.7%. The low vulnerable wards are found in the northern fringe wards and in the central part of the city (wards 1, 2, 3, 37, 50, 51, 62, 66, 70, 75, 86, 111, 112, 113, 126). The population density does not reach even 30,000 persons per sq. km in all these wards. On the other hand, among them, the dilapidated residence is highest (0.9%) in ward 11 (Dr.Radhakrishnan Nagar (South)) and the non-availability of the exclusive room is highest in wards 50 (Agaram (North)) and 126 (Rajaji Nagar). However, the requirement to go outside for fetching water is very high in the city as a whole, which also reflects in these wards. For instance, in ward 86 (Zambazaar) where all the variables are considerably low, the percentage of those who go outside their premises for getting water is as high as 18.9%.
One of the studies has observed that the city has more concentration of population along the coast (Arun Kumar & Kunte, 2012) and with time the population would become denser there (Srinivasan, Seto, Emerson, & Gorelick, 2013). As a corollary, we can expect to see an intensification of population density and other factors in this region in times to come. Chennai has a very low percentage of piped water supply but the possession of private wells by the middle class has not raised the demands (Srinivasan et al., 2013). However, the poor residents in the town do not have private wells and they rely on piped water for daily needs (Srinivasan et al., 2013). In such circumstances, deprived areas like Ambedkar Paalam (ward 146) have a defunct supply system (Coelho, 2016) leading to an obvious flouting of COVID precautions. Secondly, even if the city has good marks on open defecation statistic (Das Gupta et al., 2019), many localities have different stories. For instance, in Udhaya Suriyan Nagar (ward 32) people have built toilets between two houses (Coelho, 2016) and, in some cases, the dearth of ample water has instigated open defecation (Coelho, 2016).
5.5. Validation
At the time of writing this section, Kolkata which had open during the first unlock phase was again put into lockdown mode. The containment zones have increased in the last few days and stricter protocols are being imposed rigorously. Thus, with cases increasing and transmitting at a rapid pace, it is inferred that things would deteriorate in times to come. The ROC and AUC value for our model is 0.789 (78.9%) (Fig. 4 ), which is considered as a good fit as it falls within the range of 0.7 and 0.8 (Pourghasemi, Pouyan, et al., 2020). Given the current condition of confirmed cases and its amplification, the model would fit more accurately with time.
Fig. 4.
The ROC curve for the validation of Covid Vulnerability Index results.
6. Concluding remarks
The proposed Covid Vulnerability Index looks at city sub-units of four major Indian metro cities that now accounts for half of the total national cases. It highlights the vulnerability based on the degree to which the precautionary measures of social distancing and lockdown are defeated in these zones. It also takes into consideration vulnerability that accrues from untreated water much in resonance with WHO's Interim Guidance. The concerning picture is presented by all the four cities where the accreting COVID-19, while writing this piece, could change vulnerability into actuality. It is through stringent adoption of lockdown and social distancing protocols that the community spread of the disease can be mitigated. However, the depriving condition of the households in the demarcated sub-units may prohibit realizing the mandatory precautions at full scale. It is in this regard that the policy framers and planners must engage themselves in chalking alternative plans during the pandemic and materialising future-ready plans for inhibiting any such circumstances in the pandemic cities of the future (Constable, 2020). It must concern itself with spatial inequality in multiple deprivations and other depreciating characteristics. Thus enabling equity-based urban planning that vows to restrict the transmission of SARS-CoV-2 now or any similar pandemic in the future.
The UN-Habitat's effort to arrive at ‘innovative and appropriate solutions to ensure that cities are better prepared for the future’ is the premise of our conclusion. The study not only empirically investigates the COVID-19 vulnerable condition of the major metro cities of India in resonance with their specific context, but it also generates an evidence-based knowledge at a much granular scale so that the community, government, and NGOs could be mobilized in specific locales of a city. In that consideration, the study is both prospective and prescriptive. In times of the urban character of the global pandemic, our cities must remain sustainable for the human futurity to prosper.
CRediT authorship contribution statement
Swasti Vardhan Mishra: Conceptualization, Data curation, Visualization, Writing - original draft. Amiya Gayen: Methodology, Software, Visualization. Sk Mafizul Haque: Writing - original draft, Visualization, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We owe this paper to the comments and suggestions made by the four reviewers that helped us shape the paper. We also acknowledge the support and advice provided by Prof. Hualou Long and Prof. Eddie Chi Man Hui during the course of this article.
Footnotes
Tehsil is the sub-division of a district in India. Delhi's nine districts are further divided into several tehsils.
The COVID-19 episode has seen demarcation of cities and states into three kinds of zones – Red, Orange and Green. A Red zone has the most number of confirmed cases where nothing expect essential services is allowed.
Fig. A.1.
Contributor Information
Swasti Vardhan Mishra, Email: swastivardhanmishra@gmail.com.
Amiya Gayen, Email: mr.amiyagayen@gmail.com.
Sk Mafizul Haque, Email: mafi_haque@yahoo.co.in.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- AAAAI COVID-19 and asthma: What patients Need to know. The American academy of allergy, asthma & immunology. 2020. https://www.aaaai.org/conditions-and-treatments/library/asthma-library/covid-asthma
- Ai J.W., Zhang Y., Zhang W. Zika virus outbreak: ‘a perfect storm. Emerging Microbes & Infections. 2016;5(1):1–3. doi: 10.1038/emi.2016.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaniz A.J., Bacigalupo A., Cattan P.E. Spatial quantification of the world population potentially exposed to Zika virus. International Journal of Epidemiology. 2017;46(3):966–975. doi: 10.1093/ije/dyw366. [DOI] [PubMed] [Google Scholar]
- Arun Kumar A., Kunte P.D. Coastal vulnerability assessment for Chennai, east coast of India using geospatial techniques. Natural Hazards. 2012;64(1):853–872. doi: 10.1007/s11069-012-0276-4. [DOI] [Google Scholar]
- Baffoe G. Exploring the utility of Analytic Hierarchy Process (AHP) in ranking livelihood activities for effective and sustainable rural development interventions in developing countries. Evaluation and Program Planning. 2019;72:197–204. doi: 10.1016/j.evalprogplan.2018.10.017. [DOI] [PubMed] [Google Scholar]
- Bardhan R., Debnath R., Jana A., Norford L.K. Investigating the association of healthcare-seeking behavior with the freshness of indoor spaces in low-income tenement housing in Mumbai. Habitat International. 2018;71:156–168. doi: 10.1016/j.habitatint.2017.12.007. [DOI] [Google Scholar]
- Bardhan R., Sarkar S., Jana A., Velaga N.R. Mumbai slums since independence: Evaluating the policy outcomes. Habitat International. 2015;50:1–11. doi: 10.1016/j.habitatint.2015.07.009. [DOI] [Google Scholar]
- Basu T., Das A., Pal S. Application of geographically weighted principal component analysis and fuzzy approach for unsupervised landslide susceptibility mapping on Gish River Basin, India. Geocarto International. 2020:1–24. doi: 10.1080/10106049.2020.1778105. [DOI] [Google Scholar]
- Button C. Domesticating water supplies through rainwater harvesting in Mumbai. Gender and Development. 2017;25(2):269–282. doi: 10.1080/13552074.2017.1339949. [DOI] [Google Scholar]
- Chan J.H.L., Ma C.C. Public health in the context of environment and housing. In: Fong B.Y.F., Law V.T.S., Lee A., editors. Primary care Revisited : Interdisciplinary perspectives for a new era. Springer Singapore; 2020. pp. 295–310. [DOI] [Google Scholar]
- Choudhary S. Mumbai: Dharavi reports 20 new COVID-19 cases on Thursday, two deaths. Mumbai Mirror. 2020, June 11. https://mumbaimirror.indiatimes.com/coronavirus/news/mumbai-dharavi-reports-20-new-covid-19-cases-on-thursday-two-deaths/articleshow/76324546.cms
- Coelho K. Tenements, ghettos, or neighbourhoods? Outcomes of slum-clearance interventions in Chennai. Review of Development and Change. 2016;21(1):111–136. doi: 10.1177/0972266120160106. [DOI] [Google Scholar]
- Constable H. 2020. April 27). How do you build a city for a pandemic? BBC.https://www.bbc.com/future/article/20200424-how-do-you-build-a-city-for-a-pandemic [Google Scholar]
- Corburn J., Vlahov D., Mberu B., Riley L., Caiaffa W.T., Rashid S.F. Slum health: Arresting COVID-19 and improving well-being in urban informal settlements. Journal of Urban Health. 2020 doi: 10.1007/s11524-020-00438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das Gupta M., Dasgupta R., Kugananthan P., Rao V., Somanathan T.V., Tewari K.N. Flies without borders: Lessons from Chennai on improving India's municipal public health services. Journal of Development Studies. 2019;56(5):907–928. doi: 10.1080/00220388.2019.1605053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das A., Ghosh S., Das K., Basu T., Das M., Dutta I. Public Health; India: 2020. Modelling the effect of area-deprivation on COVID-19 incidences: A study of Chennai megacity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis M. Verso; 2006. Planet of slums. [Google Scholar]
- Desai R., McFarlane C., Graham S. The politics of open defecation: Informality, body, and infrastructure in Mumbai. Antipode. 2015;47(1):98–120. doi: 10.1111/anti.12117. [DOI] [Google Scholar]
- Dom N.C., Ahmad A.H., Latif Z.A., Ismail R. Application of geographical information system-based analytical hierarchy process as a tool for dengue risk assessment. Asian Pacific Journal of Tropical Disease. 2016;6(12):928–935. doi: 10.1016/S2222-1808(16)61158-1. [DOI] [Google Scholar]
- Dos Santos P.H., Neves S.M., Sant'Anna D.O., Oliveira C. H. de, Carvalho H.D. The analytic hierarchy process supporting decision making for sustainable development: An overview of applications. Journal of Cleaner Production. 2019;212:119–138. doi: 10.1016/j.jclepro.2018.11.270. [DOI] [Google Scholar]
- Earnest A., Ong M.E.H., Shahidah N., Chan A., Wah W., Thumboo J. Derivation of indices of socioeconomic status for health services research in Asia. Preventive Medicine Reports. 2015;2:326–332. doi: 10.1016/j.pmedr.2015.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernie H. Dwelling disparities: How poor housing leads to poor health. Environmental Health Perspectives. 2005;113(5):A310–A317. doi: 10.1289/ehp.113-a310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong M.W., Gao H., Wong J.Y., Xiao J., Shiu E.Y.C., Ryu S. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerging Infectious Diseases. 2020;26(5):976–984. doi: 10.3201/eid2605.190995. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayen A., Pourghasemi H.R., Saha S., Keesstra S., Bai S. Gully erosion susceptibility assessment and management of hazard-prone areas in India using different machine learning algorithms. The Science of the Total Environment. 2019;668:124–138. doi: 10.1016/j.scitotenv.2019.02.436. [DOI] [PubMed] [Google Scholar]
- Gharizadeh Beiragh R., Alizadeh R., Shafiei Kaleibari S., Cavallaro F., Zolfani S.H., Bausys R. An integrated multi-criteria decision making model for sustainability performance assessment for insurance companies. Sustainability. 2020;12(3):789. doi: 10.3390/su12030789. [DOI] [Google Scholar]
- Graham S., Desai R., McFarlane C. Water wars in Mumbai. Public Culture. 2013;25(69):115–141. doi: 10.1215/08992363-1890486. 1. [DOI] [Google Scholar]
- Gupta J. 2020, April 7. Coronavirus: Social distancing a cruel joke for slum dwellers in Himalayan cities. Chinadialogue.https://www.chinadialogue.net/article/show/single/en/11942-Coronavirus-Social-distancing-a-cruel-joke-for-slum-dwellers-in-Himalayan-cities [Google Scholar]
- Gupta S., Chitnis P. Mumbai, with 51,100 coronavirus cases, crosses wuhan. NDTV. 2020, June 10. https://www.ndtv.com/india-news/maharashtra-crosses-90-000-mark-mumbai-has-51-100-coronavirus-cases-2243491
- Haque S.M. University of Calcutta; 2013. Urban expansion around Kolkata Metropolitan core and its impact on land use changes-a geo-spatial analysis [PhD thesis] [Google Scholar]
- Haque S.M., Bandyopadhyay S. Identification of metropolitan core using geo-spatial data for Kolkata, India. "Scientific Annals of ""Alexandru Ioan Cuza"" University of Iasi - Geography Series". 2012;58(2):185–206. doi: 10.15551/scigeo.v58i2.190. [DOI] [Google Scholar]
- Haque S.M., Bandyopadhyay S. Demographic challenges and regional disparities in India. Global Books Organisation; 2012. Spatial disparities in vertical space-use due to proliferation of slums in Kolkata Municipal Corporation; pp. 251–267. [Google Scholar]
- Haque I., Rana M.J., Patel P.P. Location matters: Unravelling the spatial dimensions of neighbourhood level housing quality in Kolkata, India. Habitat International. 2020;99:102157. doi: 10.1016/j.habitatint.2020.102157. [DOI] [Google Scholar]
- Jain P. Delhi govt declares coronavirus an epidemic, cinema halls, schools and colleges shut till March 31 - India News. India Today. 2020, March 12. https://www.indiatoday.in/india/story/coronavirus-delhi-cinema-halls-schools-colleges-shut-kejriwal-1654856-2020-03-12
- Jia P., Dong W., Yang S., Zhan Z., Tu L., Lai S. Spatial lifecourse epidemiology and infectious disease research. Trends in Parasitology. 2020;36(3):235–238. doi: 10.1016/j.pt.2019.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston S.L. Asthma and COVID-19: Is asthma a risk factor for severe outcomes? Allergy. 2020 doi: 10.1111/all.14348. n/a(n/a) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidambi P. Routledge; 2007. The making of an Indian metropolis: Colonial governance and public culture in Bombay. [Google Scholar]
- Li X., Liu T., Lin L., Song T., Du X., Lin H. Application of the analytic hierarchy approach to the risk assessment of Zika virus disease transmission in Guangdong Province, China. BMC Infectious Diseases. 2017;17(1):65. doi: 10.1186/s12879-016-2170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu H.M., Sun W.J., Shen S.L., Arulrajah A. Flood risk assessment in metro systems of mega-cities using a GIS-based modeling approach. The Science of the Total Environment. 2018;626:1012–1025. doi: 10.1016/j.scitotenv.2018.01.138. [DOI] [PubMed] [Google Scholar]
- Lyu H.M., Zhou W.H., Shen S.L., Zhou A.N. Inundation risk assessment of metro system using AHP and TFN-AHP in Shenzhen. Sustainable Cities and Society. 2020;56:102103. doi: 10.1016/j.scs.2020.102103. [DOI] [Google Scholar]
- Mayank H., Nanavaty M., Chakraborty S.D., Mitra S., Limaye A. Jones Lang LaSalle; 2012. Global report on urban health: Equitable, healthier cities for sustainable development, WHO and UN habitat. [Google Scholar]
- McFarlane C. Sanitation in Mumbai's informal settlements: State, ‘slum’, and infrastructure. Environment & Planning A: Economy and Space. 2008;40(1):88–107. doi: 10.1068/a39221. [DOI] [Google Scholar]
- Mishra S.V. Urban deprivation in a global south city-a neighborhood scale study of Kolkata, India. Habitat International. 2018;80:1–10. doi: 10.1016/j.habitatint.2018.08.006. [DOI] [Google Scholar]
- Mitlin D. International Institute for Environment and Development; 2020, March 27. Dealing with COVID-19 in the towns and cities of the global South.https://www.iied.org/dealing-covid-19-towns-cities-global-south [Google Scholar]
- Naddeo V., Liu H. Environmental science: Water Research & technology. 2020. Editorial perspectives: 2019 novel coronavirus (SARS-CoV-2): What is its fate in urban water cycle and how can the water research community respond? [DOI] [Google Scholar]
- Nutkiewicz A., Jain R.K., Bardhan R. Energy modeling of urban informal settlement redevelopment: Exploring design parameters for optimal thermal comfort in Dharavi, Mumbai, India. Applied Energy. 2018;231:433–445. doi: 10.1016/j.apenergy.2018.09.002. [DOI] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. The Science of the Total Environment. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omar F., Bushby S.T., Williams R.D. Assessing the performance of residential energy management control Algorithms: Multi-criteria decision making using the analytical hierarchy process. Energy and Buildings. 2019;199:537–546. doi: 10.1016/j.enbuild.2019.07.033. [DOI] [Google Scholar]
- Paital B., Das K., Parida S.K. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. The Science of the Total Environment. 2020;728:138914. doi: 10.1016/j.scitotenv.2020.138914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A. World Medical & Health Policy; 2020. Preventing COVID-19 amid public health and urban planning failures in slums of Indian cities. n/a(n/a) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A., Joseph G., Shrestha A., Foint Y. Measuring deprivations in the slums of Bangladesh: Implications for achieving sustainable development goals. Housing and Society. 2019;46(2):81–109. doi: 10.1080/08882746.2019.1622346. [DOI] [Google Scholar]
- Patel A., Koizumi N., Crooks A. Measuring slum severity in Mumbai and Kolkata: A household-based approach. Habitat International. 2014;41:300–306. doi: 10.1016/j.habitatint.2013.09.002. [DOI] [Google Scholar]
- Patel A., Shah P., Beauregard B.E. Measuring multiple housing deprivations in urban India using Slum Severity Index. Habitat International. 2020;101:102190. doi: 10.1016/j.habitatint.2020.102190. [DOI] [Google Scholar]
- Pourghasemi H.R., Gayen A., Edalat M., Zarafshar M., Tiefenbacher J.P. Is multi-hazard mapping effective in assessing natural hazards and integrated watershed management? Geoscience Frontiers. 2020;11(4):1203–1217. doi: 10.1016/j.gsf.2019.10.008. [DOI] [Google Scholar]
- Pourghasemi H.R., Pouyan S., Heidari B., Farajzadeh Z., Shamsi S.R.F., Babaei S. Spatial modelling, risk mapping, change detection, and outbreak trend analysis of coronavirus (COVID-19) in Iran (days between 19 February to 14 June 2020) International Journal of Infectious Diseases. 2020 doi: 10.1016/j.ijid.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PTI . The Times of India; 2020. India Lockdown update: Centre lists red, green zone districts for week after May 3 | India News - times of India.https://timesofindia.indiatimes.com/india/covid-19-centre-lists-red-green-zone-districts-for-week-after-may-3/articleshow/75489944.cms [Google Scholar]
- PTI . India Today; 2020. 13 more test positive for coronavirus in Dharavi, tally reaches 288.https://www.indiatoday.in/india/story/maharashtra-mumbai-dharavi-coronavirus-total-cases-death-toll-april-27-1671798-2020-04-27 April 27) [Google Scholar]
- PTI . The Times of India; 2020, May 15. ). 30 municipal areas account for 79% of India's Covid caseload.https://timesofindia.indiatimes.com/india/30-municipal-areas-account-for-79-of-indias-covid-caseload/articleshow/75763216.cms [Google Scholar]
- PTI Delhi, Mumbai, Kolkata and Chennai account for nearly 50% of nationwide Covid-19 cases. 2020, June 7. https://theprint.in/india/delhi-mumbai-kolkata-and-chennai-account-for-nearly-50-of-nationwide-covid-19-cases/437222/ The Print.
- Ravi S. The Hindu; 2018, August 9. Open defecation still happens in east Delhi.https://www.thehindu.com/news/cities/Delhi/open-defecation-stillhappens-in-east-delhi/article24637389.ece [Google Scholar]
- Ray S., Khanna R., Yengkhom S., Ghosh D. Congested Belgachhia slum emerges as ground zero of Covid battle in city. The Times of India; 2020. April 14) [Google Scholar]
- Ray B., Shaw R. Water stress in the megacity of Kolkata, India, and its implications for urban resilience. In: Shaw R., Atta-ur-Rahman, Surjan A., Parvin G.A., editors. Urban disasters and resilience in Asia. Butterworth-Heinemann; 2016. pp. 317–336. [DOI] [Google Scholar]
- Rocklöv J., Sjödin H. High population densities catalyze the spread of COVID-19. Journal of Travel Medicine. 2020 doi: 10.1093/jtm/taaa038. taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saaty T.L. McGraw-Hill; 1980. The analytic Hierarchy process: Planning, priority setting, resource allocation. [Google Scholar]
- Saaty T.L., Vargas L.G. Kluwer; 2001. Models, methods, concepts & applications of the analytic Hierarchy process. [Google Scholar]
- Saha S., Gayen A., Pourghasemi H.R., Tiefenbacher J.P. Identification of soil erosion-susceptible areas using fuzzy logic and analytical hierarchy process modeling in an agricultural watershed of Burdwan district, India. Environmental Earth Sciences. 2019;78(23):649. doi: 10.1007/s12665-019-8658-5. [DOI] [Google Scholar]
- Saroj S.K., Goli S., Rana M.J., Choudhary B.K. Availability, accessibility, and inequalities of water, sanitation, and hygiene (WASH) services in Indian metro cities. Sustainable Cities and Society. 2020;54:101878. doi: 10.1016/j.scs.2019.101878. [DOI] [Google Scholar]
- Sasssen S. Princeton University Press; New York, London, Tokyo: 1991. The global city. [Google Scholar]
- Shahabi H., Khezri S., Ahmad B.B., Hashim M. Landslide susceptibility mapping at central zab basin, Iran: A comparison between analytical hierarchy process, frequency ratio and logistic regression models. Catena. 2014;115:55–70. doi: 10.1016/j.catena.2013.11.014. [DOI] [Google Scholar]
- Shahfahad, Kumari B., Tayyab M., Hang H.T., Khan M.F., Rahman A. Assessment of public open spaces (POS) and landscape quality based on per capita POS index in Delhi, India. SN Applied Sciences. 2019;1(4):368. doi: 10.1007/s42452-019-0372-0. [DOI] [Google Scholar]
- Shaikh M. India Today; 2020, April 10. With over 1,000 cases, Mumbai becomes India's Covid-19 hotspot.https://www.indiatoday.in/india/story/with-over-1-000-cases-mumbai-becomes-india-s-covid-19-hotspot-1665623-2020-04-10 [Google Scholar]
- Singh V.V. The Times of India; 2020. Dharavi Corona Cases: Dharavi sees highest one-day jump with 34 new cases; tally rises to 275.https://timesofindia.indiatimes.com/city/mumbai/dharavi-sees-highest-one-day-jump-with-34-new-cases-tally-rises-to-275/articleshow/75397957.cms [Google Scholar]
- Srinivasan V., Seto K.C., Emerson R., Gorelick S.M. The impact of urbanization on water vulnerability: A coupled human–environment system approach for Chennai, India. Global Environmental Change. 2013;23(1):229–239. doi: 10.1016/j.gloenvcha.2012.10.002. [DOI] [Google Scholar]
- Swarajya . 2020, June 11. ICMR serosurvey: Just 0.73 per cent of population had evidence of past exposure to coronavirus. Swarajya.https://swarajyamag.com/insta/icmr-serosurvey-just-073-per-cent-of-population-had-evidence-of-past-exposure-to-coronavirus [Google Scholar]
- The Economist Covid-19 might not change cities as much as previous pandemics. Economist. 2020, April 25 https://www.economist.com/books-and-arts/2020/04/25/covid-19-might-not-change-cities-as-much-as-previous-pandemics [Google Scholar]
- The New York Times . The New York Times; 2020. New York coronavirus map and case count.https://www.nytimes.com/interactive/2020/us/new-york-coronavirus-cases.html [Google Scholar]
- TNN . The Times of India; 2020. Chennai corona hotspots: Why Chennai remains a covid-19 hotspot.https://timesofindia.indiatimes.com/city/chennai/why-chennai-remains-a-hotspot/articleshow/75281921.cms [Google Scholar]
- Tomlinson R. Scalable community-led slum upgrading: The Indian Alliance and community toilet blocks in Pune and Mumbai. Habitat International. 2015;50:160–168. doi: 10.1016/j.habitatint.2015.08.020. [DOI] [Google Scholar]
- UN Habitat UN-habitat COVID-19 response plan [response plan]. UN habitat. 2020. https://unhabitat.org/sites/default/files/2020/04/final_un-habitat_covid-19_response_plan.pdf
- Upadhyay A. “Building toilets is not enough to eradicate open defecation,” experts stress on the need to maintain the toilets in Delhi | access to toilets. NDTV-dettol banega swasth swachh India. 2020, February 10. https://swachhindia.ndtv.com/building-toilets-is-not-enough-to-eradicate-open-defecation-experts-stress-on-the-need-to-maintain-the-toilets-in-delhi-41581/
- Wasdani K.P., Prasad A. Local Environment; 2020. The impossibility of social distancing among the urban poor: The case of an Indian slum in the times of COVID-19. [DOI] [Google Scholar]
- WHO . World Health Organization; 2020. Coronavirus disease 2019 (COVID-19) situation report – 40 [situation report]https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200229-sitrep-40-covid-19.pdf?sfvrsn=849d0665_2 [Google Scholar]
- WHO Global . World Health Organization; 2020. Water, sanitation, hygiene, and waste management for the COVID-19 virus: Interim guidance (interim guidance WHO/2019-nCoV/IPC_WASH/2020.3; p. 9.https://www.who.int/publications-detail-redirect/water-sanitation-hygiene-and-waste-management-for-the-covid-19-virus-interim-guidance [Google Scholar]
- WHO, UN-Habitat . World Health Organization; 2016. Global report on urban health: Equitable healthier cities for sustainable development. [Google Scholar]
- Yashoda V. COVID-19 comes to Asia's most densely populated slum. 2020. https://thediplomat.com/2020/04/covid-19-comes-to-asias-most-densely-populated-slum/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.