Abstract
Background
The daily lives of children with physical disabilities and their families have been significantly affected by the COVID-19 pandemic. The children face health risks, especially mental, behavioral, social and physical risks.
Objective
This study aimed to identify potential healthcare issues relating to the wellbeing of disabled children, continuity of rehabilitation and medical care, and parental concerns during the COVID-19 lockdown.
Methods
The Enfant Confinement Handicap besOins (ECHO [child lockdown disability needs]) national survey was developed by a multidisciplinary group and disseminated in France from April 6, 2020 via email and social networks. This online survey was addressed to the parents of children with physical disabilities aged 0 to 18 years. It explored the experiences of children and their families during the lockdown. Information regarding children's wellbeing, rehabilitation and family organization was collected. The first 1000 eligible surveys were analyzed.
Results
The children (mean [SD] age 9.5 [4.8] years) mostly had cerebral palsy (42%) or neuromuscular diseases (11%). The lockdown had negative effects on morale (44% of children), behaviour (55% of children) and social interactions (55% no contact with other children). Overall, 44% of children stopped physical activities; 76% were educated at home; 22% maintained medical follow-up, and 48% and 27% continued physiotherapy and occupational therapy respectively. For more than 60% of children, parents performed the therapy. The main parental concern was rehabilitation (72%) and their main difficulty was the mental load (50%); parents complained of lack of help and support (60%).
Conclusions
This study highlighted substantial effects on the health of children with physical disabilities and loss of opportunity, with a massive interruption of medical follow-up and rehabilitation, during the lockdown. Regular assessment of the health benefit/risk is essential to support families and ensure continuity of care during a pandemic.
Keywords: COVID-19, Children with physical disabilities, Lockdown, Rehabilitation, Health risks
1. Introduction
In March 2020, the World Health Organisation reported more than 118,000 cases of coronavirus disease 2019 (COVID-19) worldwide and declared the situation a pandemic [1]. After health campaigns recommending preventative measures and social distancing, lockdowns were established in numerous countries to limit the spread of the infection (> 3.4 billion people confined worldwide on March 31). In this unprecedented situation, schools were closed, the possibility to go out was limited, direct contact with friends and other family members was stopped, and rehabilitation and medical follow-up were interrupted.
This exceptional situation abruptly changed daily life for children with disabilities and their families. In France, since the 2005 disability law, many children with physical disabilities attend school; 85% in regular schools and 12% in specialized establishments [2]. They also have regular medical appointments and rehabilitation sessions (physiotherapy, occupational therapy, psychological counselling, etc.), which are based on goals that are pre-determined with the children and their families [3]. According to one study, children with cerebral palsy consult a physician about 5 times a year and attend almost 4 therapy sessions per week [4]. Moreover, family management was totally disrupted during the pandemic.
The sudden and unexpected changes induced by the lockdown are likely to create new difficulties and needs for children with disabilities and their parents. The pandemic is likely to have a large impact on the health of these children, including their physical, mental and social wellbeing as defined by the WHO in the International Classification of Functioning (ICF) [5]. During the first weeks of the lockdown, some families of children with disabilities around the world alerted health systems to the effects of the lockdown on both the health and loss of opportunity for their children. However, a collective vision was required to highlight the specific needs of children and their families during the pandemic and to provide efficient services after the lockdown. We hypothesized that children with disabilities faced health risks, especially relating to mental health, behavioral disorders, social isolation, sedentarism in a context of rehabilitation and interrupted medical follow-up. Consequences on the family were also expected.
A large national survey of parents of children with physical disabilities was developed to 1) gain knowledge of the effects of lockdown on these families and 2) provide data on which to base decisions for the appropriate adaptation of rehabilitation services to improve care both individually and collectively. The survey's specific aim was to report the experiences, difficulties and needs of children with physical disabilities and their parents during the lockdown. The study we describe here focused on healthcare issues via the exploration of the child's wellbeing (morale, behavior, social interaction, physical activity), continuity of rehabilitation and medical care, and parental concerns.
2. Methods
2.1. Ethical and regulatory considerations
This study was a cross-sectional study conducted in France with an online survey and following the STROBE guidelines [6]. It began on April 6, 2020, 3 weeks after the start of the lockdown in France (March 17 to May 11, 2020), and was conducted according to current French legislation (loi Jardé, no. 2012-300) [7]). Responders could not be identified from the survey (no email or IP address), so anonymity was guaranteed [8]. The survey was registered at ClinicalTrials.gov (NCT04395833).
2.2. Development of the survey
Given the unprecedented situation, the ECHO survey (Enfant Confinement Handicap BesOins [child lockdown disability needs]) was specifically created to report the experiences, difficulties and needs of children with physical disabilities and their parents during the COVID-19 lockdown. It was addressed to parents or legal guardians of children with physical disabilities (cerebral palsy, neuromuscular disease, orthopedic disease, etc.), with or without other associated impairments, who were 0 to 18 years old.
To ensure face and content validity [9], the survey was developed by a national multidisciplinary group that included 7 parents of children with physical disabilities, representatives of 3 family organizations and 3 learned societies, researchers, medical and rehabilitation professionals who were all experienced in disability care (see acknowledgements). In a biopsychosocial perspective [10], the conceptual framework of the ICF describing the individual in terms of activity, participation and environment was used [5]. The content and formulation were in French and were approved by all stakeholders before launching. The survey was conceived to be short and to take less than 20 min to complete. The survey was tested by the 7 families before its diffusion to check comprehensibility of the instructions, items, response options and completion time.
The survey was developed by using the online tool SurveyMonkey (San Mateo, CA, USA). The completion could only be proposed online because of the lockdown measures. The survey consisted of 115 questions. The first part related to general information about the child. This part collected data on age, sex, region of residence, type of residence during the lockdown, motor function (autonomy level rated A to D for the following items: walking, dominant upper-limb use, non-dominant upper-limb use and fine motor skill, where A indicates “activity possible without difficulty or help” and D “not possible” [11]), diagnosis and rehabilitation setting (outpatient clinic, rehabilitation center or specialized services [provided at home, at school or in an establishment]). The second part of the survey related to the child's condition and the third to the parents’ experience. The questions on the child's condition corresponded to medical follow-up, rehabilitation and daily life (schooling, physical activity, morale, behavior and social interaction) during the lockdown. The section on parent experience asked about family management, concerns, difficulties and needs during daily life in the lockdown. Most questions had closed answers, either binary (yes/no) or multiple choice. All questions did not have to be answered (e.g., children without physiotherapy follow-up did not have to answer questions related to physiotherapy). For more details, all questions and responses to the ECHO survey are available at https://fr.surveymonkey.com/r/TESTECHO.
2.3. Dissemination strategy
The survey was promoted nationally through parent groups, advocacy groups, learning societies and professional bodies. It was widely disseminated via email and social media (Facebook, Linked-in and Twitter) to collect real-time information on the impact of the lockdown on daily life and to obtain data on children with a wide range of ages and situations. It was also diffused countrywide, in all regions of France, to limit local bias. Weekly reminders were sent to families, patients, learned societies, organizations etc. to encourage completion and diffusion until the end of the lockdown. Care was taken to ensure that the survey reached family networks.
Because of the unprecedented situation, the number of required responses could not be estimated. However, a sample of at least 1000 responses was considered appropriate to provide consistent information on the experience of children with physical disabilities and their parents during the lockdown.
2.4. Statistical analysis
The variables and questions relating to general information about the children, child's wellbeing, continuity of rehabilitation and medical care, and parental concerns were selected for the present study from the larger ECHO survey. Thus, data on demographics, morale, behavior, social interaction, physical activity, medical follow-up, rehabilitation, main parental concerns, difficulties and needs were analyzed. We excluded from the analysis only surveys that were not completed by parents or legal guardians, that were not finished, or if the child was not living at home during the lockdown. Descriptive analysis was performed on the first 1000 responses that fulfilled the inclusion criteria. Results are provided for all possible responses to each question. Quantitative results are expressed as mean (standard deviation) and categorical results as number (%).
3. Results
3.1. Population description
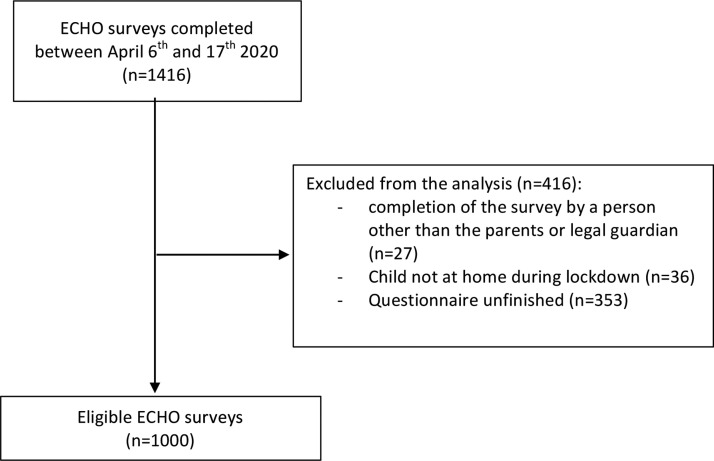
Between April 6 and April 17, 2020, 1416 questionnaires were completed (Table 1 ). We excluded questionnaires completed by a person other than the child's parents or legal guardian (n = 27), were not finished (n = 353), or children were not living at home during the lockdown (n = 36). In total, 1000 questionnaires were analyzed (Fig. 1 ).
Table 1.
Characteristics of respondents to the ECHO survey.
| Children with physical disabilities | |
|---|---|
| Age (years) (n = 1000) | |
| Mean (SD) | 9.5 (4.8) |
| Range [min-max] | [1–18] |
| Sex (n = 1000) | |
| Female | 459 (46%) |
| Male | 541 (54%) |
| Region of residence in France (n = 1000) | |
| Auvergne-Rhône-Alpes | 301 (30%) |
| Brittany | 121 (12%) |
| Ile-de-France (Paris region) | 118 (12%) |
| Pays de la Loire | 88 (9%) |
| Aquitaine-Limousin-Poitou-Charentes | 76 (8%) |
| Languedoc-Roussillon-Midi-Pyrénées | 74 (7%) |
| Alsace-Champagne-Ardenne-Lorraine | 64 (6%) |
| Centre-Val de Loire | 31 (3%) |
| Normandy | 31 (3%) |
| Bourgogne-Franche-Comté | 30 (3%) |
| Nord-Pas-de-Calais-Picardie | 29 (3%) |
| Provence-Alpes-Côte d’Azur | 27 (3%) |
| Overseas | 10 (1%) |
| Corsica | 0 (0%) |
| Pathologies (n = 1000) | |
| Cerebral palsy | 418 (42%) |
| Genetic diseases or congenital malformations | 245 (25%) |
| Neuromuscular diseases (Duchenne muscular dystrophy, spinal amyotrophy, etc.) | 111 (11%) |
| Other neurological lesions (dysraphism, traumatic brain injury) | 55 (6%) |
| Orthopedic diseases (bone malformations, amputation, bone tumor etc.) | 15 (2%) |
| Other | 156 (16%) |
| Functional abilities (n = 1000) | |
| Walking | |
| Possible without difficulty or help | 208 (21%) |
| Possible with difficulty but no help | 185 (19%) |
| Possible with human help or stimulation | 222 (22%) |
| Not possible | 385 (39%) |
| Fine motor skills | |
| Possible without difficulty or help | 97 (10%) |
| Possible with difficulty but no help | 273 (27%) |
| Possible with human help or stimulation | 382 (38%) |
| Not possible | 248 (25%) |
| Associated impairments (n = 906) | |
| Cognitive | 367 (41%) |
| Behavioural | 227 (25%) |
| Sensory | 139 (15%) |
| Other | 161 (18%) |
| None | 303 (33%) |
| Rehabilitation main setting (n = 1000) | |
| Specialized servicesa | 619 (62%) |
| Outpatient clinic | 208 (21%) |
| Rehabilitation centre | 55 (6%) |
| Other | 118 (12%) |
| Person answering the questionnaire | |
| Respondents (n = 1000) | |
| Mother | 875 (88%) |
| Father | 117 (12%) |
| Legal guardian | 8 (1%) |
Specialized services, at home, at school or in establishment, included CAMSP (Centre d’action médico-sociale précoce [early medical-social center for action]), SESSAD (service d’éducation spéciale et de soins à domicile [special education and home health service]), IME (Institut Médico-Educatif [medical-educational institution]), IEM (Institut d’Education Motrice [educational institution for children with physical disabilities]).
Fig. 1.
Flow of participants in the study. ECHO, Enfant Confinement Handicap besOins.
The mean age of children was 9.5 (4.8) years; 46% were female. Responses were received from 12 of 13 regions of France, with 3 regions more represented (Table 1). Most of the children had cerebral palsy (42%) or neuromuscular diseases (11%). They had various levels of motor function: 38.5% could not walk and 38.2% needed help or stimulation for fine motor skills. Associated impairments were reported for 67% (cognitive [41%], behavioral [25%] and sensory [15%]). Rehabilitation during the lockdown was mostly performed by specialized services (62%). Mothers completed 88% of the questionnaires.
3.2. Wellbeing of children with physical disabilities
A negative effect of lockdown on morale was reported for 43% of children; 55% no longer had contact with other children during this period (Table 2 ). In total, 55% of children showed behavior changes, mostly behavioral problems (32%) and sleeping difficulties (22%). Among the 732 children who usually practiced physical activities, 44% had stopped them during the lockdown.
Table 2.
Main results for child wellbeing, rehabilitation, and parent concerns in the ECHO survey (based on 1000 answers).
| Questions | Number of responses (n) | (%) |
|---|---|---|
| Child wellbeing | ||
| Morale | 1000 | |
| Positively impacted | 128 (13) | |
| Negatively impacted | 433 (43) | |
| Not impacted | 439 (44) | |
| Interaction with other children | 1000 | |
| Yes | 454 (45) | |
| No | 546 (55) | |
| Changes in children | 1000 | |
| Behavioural disorders (agitation, anger, isolation, etc.) | 318 (32) | |
| Sleeping difficulties | 218 (22) | |
| Somatic complaints (pain, etc.) | 136 (14) | |
| Eating disorders | 89 (9) | |
| Regression | 80 (8) | |
| Other | 97 (10) | |
| None | 466 (47) | |
| Physical activity (among children who practiced an activity before the lockdown) | 732 | |
| Yes | 408 (56) | |
| No | 324 (44) | |
| Rehabilitation | ||
| Planed medical follow-up consultation | 588 | |
| Cancelled | 262 (45) | |
| Delayed | 189 (32) | |
| Telehealth | 103 (18) | |
| Held | 26 (4) | |
| Maintained but cancelled by parents due to COVID-19 fear | 8 (1) | |
| Rehabilitation maintained by the therapist, parents or the childa | ||
| Physiotherapy | 872 | 418 (48) |
| Occupational therapy | 644 | 176 (27) |
| Speaking therapy | 548 | 176 (32) |
| Psychomotricity | 604 | 186 (31) |
| Orthoptist | 208 | 27 (13) |
| Rehabilitation performed by parents during the lockdowna | ||
| Physiotherapy | 418 | 345 (83) |
| Occupational Therapy | 179 | 138 (77) |
| Speaking therapy | 178 | 142 (80) |
| Psychomotricity | 188 | 149 (79) |
| Orthoptist | 26 | 16 (62) |
| Parent concerns | ||
| Schooling | 786 | |
| At home | 596 (76) | |
| At school or usual establishment | 29 (4) | |
| Not maintained | 161 (21) | |
| Parental help with home-schooling | 594 | |
| Extensive help | 483 (81) | |
| Little help | 86 (15) | |
| Child independent | 25 (4) | |
| Main concern for the parents | 1000 | |
| Rehabilitation | 720 (72) | |
| Social interaction | 462 (46) | |
| Risk of COVID-19 infection | 453 (45) | |
| School learning | 376 (38) | |
| Medical follow-up | 345 (35) | |
| Morale | 324 (32) | |
| Physical activities | 296 (30) | |
| Leisure activities | 232 (23) | |
| Behaviour | 236 (24) | |
| Other | 31 (3) | |
| None | 31 (3) | |
| Difficulties in everyday life for the parents | 1000 | |
| Mental load | 503 (50) | |
| Feelings of helplessness | 398 (40) | |
| Daily life coordination | 321 (32) | |
| Prioritization of the child's needs | 313 (31) | |
| Lack of human support | 289 (29) | |
| Lack of time | 272 (27) | |
| Lack of material support | 207 (21) | |
| Financial concerns | 131 (13) | |
| None | 159 (16) | |
| Other | 56 (6) | |
| Claim for need of support (human or material) | 359 | |
| Yes | 215 (60) | |
| No | 144 (40) | |
Questions relating to maintained therapy sessions or sessions performed by parents were only answered if the child usually had rehabilitation.
3.3. Rehabilitation and medical follow-up
For 77% of children, medical consultations were cancelled or postponed during the lockdown (Table 2). Consultations that were maintained were performed face to face (4%) or by telehealth (18%). Physiotherapy, occupational therapy, speech therapy, psychomotor therapy and orthoptic sessions were continued for 48%, 27%, 32%, 31% and 13% of children, respectively. Therapy was performed by parents (physiotherapy, occupational therapy, speech therapy, psychomotor therapy and orthoptist) for 83%, 77%, 80%, 79% and 62% of children, respectively.
3.4. Parental concerns during the lockdown
Overall, 76% of children were educated at home; 81% of these required significant parental help (Table 2). For 72% of parents, the primary concern was rehabilitation. Other major concerns were social interactions (46%) and risk of COVID-19 infection (45%). For 50% of parents, mental load was the main daily difficulty; 60% reported a need for support in terms of human resources, psychological support or schooling recommendations.
4. Discussion
The ECHO survey was an original, national, multidisciplinary, family-centered initiative to describe the experiences of children with disabilities and their families during the COVID-19 pandemic. The responses revealed that families faced major difficulties, and many of their needs were unmet owing to the cessation of medical follow-up and rehabilitation. From the beginning of the lockdown, all children's care, rehabilitation, schooling etc. had to be performed at home, placing all the onus on parents.
4.1. Health-related risks for children and their families
This survey highlighted the negative effects of the lockdown on the children's wellbeing and their mental and social health (morale, behavior, social interaction and physical activity), similar to a recent report on children without disability [12]. The psychological effects of the lockdown, including post-traumatic stress symptoms, confusion and anger have been reported in the general population and are related to the duration of the lockdown [13], [14], [15]. Children with physical disabilities have an increased risk of mental health symptoms [16], [17], [18], which could be exacerbated during the pandemic. The lack of social interaction may not only affect their morale but may also lead to a regression in their communication ability. Moreover, the development or worsening of behavioral disorders could further affect their wellbeing and increase the parental sensation of helplessness. Children with physical disabilities have higher risk of sedentarism and its consequences than other children [19], [20]. As was found for children without disability [21], the results of the present survey showed that during the lockdown, the level of physical activity of children with disabilities was reduced considerably. Furthermore, these children are likely to experience a loss of motor skills because motor capacity is related to physical activity and sedentary time negatively affects motor skills [22], [23].
The most frequent parental concern was the lack of rehabilitation during the lockdown. The purpose of regular rehabilitation is to maintain or progress motor skills and to prevent complications that could further alter mobility and increase difficulties in daily life, such as orthopedic deformities or physical deconditioning. Therefore, the interruption or modification of medical care and rehabilitation could inevitably deteriorate the child's physical status and functional ability.
The greatest difficulty reported by the parents was the mental load faced daily. Usual family life was disrupted by the need for intensive parent intervention in activities that are usually performed by a multidisciplinary team (rehabilitation professionals, teachers, etc.). The parents of children with disabilities already have to cope with the physical and mental health challenges associated with having a child with disabilities in normal times and are therefore particularly vulnerable during the pandemic [24], [25]. The closure of schools and some specialized services and establishments in France during the lockdown increased the pressure on these parents, generating a high risk of parental exhaustion [25], [26].
The results of this survey highlight the secondary impact of the COVID-19 pandemic on the care and wellbeing of children with physical disabilities, as was shown in other chronic conditions [27]. The Cerebral Palsy Rehabilitation Charter [28], which promotes the rights of children with disabilities in terms of shared, participation-related goals, whatever the situation, was not applied during the lockdown for a large proportion of children. Similarly, the concept of the “F words” (Function, Family, Fitness, Fun, Friends, and Future [29]) that support the implementation of the ICF, promoted by the WHO [5], was not applied.
4.2. Evaluating the benefits and healthcare-related risks during the lockdown and progressive easing of the lockdown
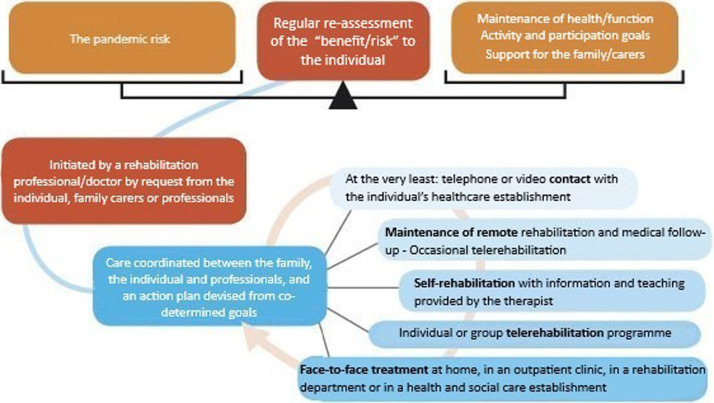
One of the main results of the ECHO survey was that the effects and experiences of the lockdown differed among families. This finding demonstrates the importance of assessing each situation individually to maintain and promote quality of life in children and their families, including during and after the lockdown. The lockdown resulted in an extended period with no access to usual care, which is set to continue during the progressive easing of the lockdown. Surveys such as ECHO will increase our understanding of the challenges that children with disabilities and their families face during the COVID-19 pandemic and should lead to new propositions for prompt action and the promotion of collaboration. Care must be centered around the children and their families at all times and in all settings, and rehabilitation professionals should aim to prevent the secondary effects of the health crisis on children and their families [30], [31]. During the health crisis, the individual “benefit/risk” ratio should be regularly re-evaluated to ensure a balance between the pandemic risk and the maintenance of overall health, activity and participation goals for the child as well as provide support for the family and caregivers (Fig. 2 ). The risk of COVID-19 infection is considered low for children [32], [33], [34]; however, the pandemic has large, potentially long-lasting, indirect consequences for children with disabilities.
Fig. 2.
Coordination of rehabilitation for children with disabilities during the COVID-19 lockdown and during easing of the lockdown. A proposition for regular evaluation of the “benefit/risk” to the individual during the pandemic situation to obtain a balance between the risk of the spread of the infection, and overall health, activity and participation goals for the child as well as providing support for the family and carers. The assessment may be initiated by the rehabilitation professional/doctor, the individual or the family. The aim is for care to be coordinated between all those concerned and based on co-determined goals in the interest of the individual. The action plan may be graduated according to the individual's needs, from telephone or video contact with the family to face-to-face treatment at home.
Rehabilitation must remain organized according to activity and participation goals that are co-determined with the child and the family to help them adapt to the situation and self-manage as far as possible [35]. A key worker or coordinator should be appointed for each child, as is already recommended with the health crisis, but is even more necessary in the present context [36]. Depending on the individual's needs, the provision of rehabilitation can be graded from a simple telephone contact with the family to a home visit when absolutely necessary. The level of provision must be regularly re-evaluated because the child's and family's needs may change. Existing new approaches for the long-term continuity of care should be implemented during the lockdown and its easing as well as in usual-care situations [3]. For example, telerehabilitation provides a means for therapy sessions that is fully compliant with barrier measures. Large-scale studies of the indirect effects of the pandemic on children with disabilities are required, along with the development of innovative healthcare management approaches that are patient- and family-centered to provide continuous care and support for these children and their families.
The findings of this survey, performed during the lockdown, regarding medical care and rehabilitation, child well-being and parental concerns, must be considered in the context of the actual health situation and social distancing measures and also for the usual management of some children (e.g., those living in isolated regions). We now need innovative care systems that follow the principles of the child's rehabilitation, prevent the secondary effects of the lockdown on children and their families, and can be used both in a pandemic situation as well as usual care.
4.3. Limitations
The representativeness of the responders could not be ensured in this study. However, the receipt of a large number of responses in just a few days from parents of children with disabilities of varying severity, associated disorders and family situations from all over France demonstrates the importance of the issue and their great concern for their children's condition and therefore must be closely considered. This article presented the descriptive results of the first 1000 responses to the ECHO survey, but a larger sample size is expected at the end of the collection period. This larger sample will allow specific questions to be addressed using multivariate analyses (e.g., the impact on daily life or on medical follow-up and rehabilitation) in further studies. Addressing the survey to parents and not children may have led to some response bias. The survey was specially created for the COVID-19 pandemic, designed to be rapidly diffused during the lockdown and was only available online. Therefore, it was not available to people who do not have access to the Internet, who may have faced even greater difficulties during the lockdown. The unfinished surveys were not analyzed so as to obtain the same number of responses in all domains explored, but this could have affected the generalizability of results. Although healthcare systems and the measures taken to cope with the pandemic differ among countries, some of the data from this French survey could be used for studies in other countries.
5. Conclusions
The lockdown in France in response to the COVID-19 pandemic has disrupted daily life for children with physical disabilities and their families. This study revealed major consequences for the wellbeing of the children. Rehabilitation services were massively interrupted, and this was the main parental concern. Parents were faced with the burden of managing the child's daily life as well as providing rehabilitation. The situation of the child and family must be regularly re-evaluated and goals must be family-centered, adapted and prioritized as a function of the “benefit/risk” balance.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
We thank the parents and their children for completing the ECHO survey and thank BEaCHILD (Centre Breton de recherche et d’innovation pour la réadaptation et le développement de l’enfant), FRISBEE (Fédération des SSR pédiatriques de Bretagne occidentale), R4P (Réseau régional de rééducation et de réadaptation pédiatrique en Auvergne-Rhône Alpes), SFERHE (Société francophone d’études et de recherche sur les handicaps de l’enfance), SOFMER (Société française de médecine physique et de réadaptation), Fondation paralysie cérébrale, l’IFRH (Institut fédératif de recherche sur le handicap), AFM-Téléthon (Association française contre les myopathies), FFAIMC (Fédération française des associations d’infirmes moteurs cérébraux), Institut motricité cérébrale-formation-et-documentation, FIRAH (Fondation internationale pour la recherche appliquée sur le handicap) and SNP (Société française de neuropédiatrie). We also thank Johanna Robertson for language assistance and FFAIMC for the figure design.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.rehab.2020.08.001.
Appendix A. Supplementary data
References
- 1.Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebersold S., Plaisance E., Zander C. 2016. École inclusive pour les élèves en situation de handicap. Accessibilité, réussite scolaire et parcours individuels. Conseil national d’évaluation du système scolaire-CNESCO, Conférence de comparaisons internationales. [Google Scholar]
- 3.Wade D. Rehabilitation–a new approach. Overview and part one: the problems. Clin Rehabil. 2015;29:1041–1050. doi: 10.1177/0269215515601174. [DOI] [PubMed] [Google Scholar]
- 4.Sacaze E., Garlantezec R., Rémy-néris O., Peudenier S., Rauscent H., le Tallec H., et al. A survey of medical and paramedical involvement in children with cerebral palsy in Britanny: preliminary results. Ann Phys Rehab Med. 2013;56:253–267. doi: 10.1016/j.rehab.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Constitution of the World Health, Organization . 45th ed. World Health Organization; Geneva: 2006. World Health Organization: basic documents. [https://www.who.int/governance/eb/who_constitution_en.pdf] [Google Scholar]
- 6.Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13:S31–S34. doi: 10.4103/sja.SJA_543_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rat C., Tudrej B., Kinouani S., Guineberteau C., Bertrand P., Renard V., et al. 2017. Réglementation I méthodologie; p. 8. [Google Scholar]
- 8.Toulouse E., Masseguin C., Lafont B., McGurk G., Harbonn A., Roberts A.J., et al. French legal approach to clinical research. Anaesth Crit Care Pain Med. 2018;37:607–614. doi: 10.1016/j.accpm.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Mokkink L.B., Terwee C.B., Patrick D.L., Alonso J., Stratford P.W., Knol D.L., et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19:539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wade D.T., Halligan P.W. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil. 2017;31:995–1004. doi: 10.1177/0269215517709890. [DOI] [PubMed] [Google Scholar]
- 11.Formulaire 15695*01 : Certificat médical à joindre à une demande à la maison départementale des personnes handicapées (MDPH) | service-public.fr n.d.
- 12.Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;0 doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020 doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sigurdardottir S., Indredavik M.S., Eiriksdottir A., Einarsdottir K., Gudmundsson H.S., Vik T. Behavioural and emotional symptoms of preschool children with cerebral palsy: a population-based study. Dev Med Child Neurol. 2010;52:1056–1061. doi: 10.1111/j.1469-8749.2010.03698.x. [DOI] [PubMed] [Google Scholar]
- 17.Steele M., Taylor E., Young C., McGrath P., Lyttle B.D.B., Davidson B. Mental health of children and adolescents with Duchenne muscular dystrophy. Dev Med Child Neurol. 2008;50:638–639. doi: 10.1111/j.1469-8749.2008.03024.x. [DOI] [PubMed] [Google Scholar]
- 18.Klein B. Mental health problems in children with neuromotor disabilities. Paediatr Child Health. 2016;21:93–96. doi: 10.1093/pch/21.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bell K.L., Boyd R.N., Tweedy S.M., Weir K.A., Stevenson R.D., Davies P.S. A prospective, longitudinal study of growth, nutrition and sedentary behaviour in young children with cerebral palsy. BMC Public Health. 2010;10:179. doi: 10.1186/1471-2458-10-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maltais D.B., Wiart L., Fowler E., Verschuren O., Damiano D.L. Health-related physical fitness for children with cerebral palsy. J Child Neurol. 2014;29:1091–1100. doi: 10.1177/0883073814533152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiang M., Zhang Z., Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keawutan P., Bell K.L., Oftedal S., Davies P.S.W., Ware R.S., Boyd R.N. Relationship between habitual physical activity, motor capacity, and capability in children with cerebral palsy aged 4–5 years across all functional abilities. Disab Health J. 2018;11:632–636. doi: 10.1016/j.dhjo.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 23.Keawutan P., Bell K., Davies P.S.W., Boyd R.N. Systematic review of the relationship between habitual physical activity and motor capacity in children with cerebral palsy. Res Dev Disabil. 2014;35:1301–1309. doi: 10.1016/j.ridd.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 24.Magliano L., Patalano M., Sagliocchi A., Scutifero M., Zaccaro A., D’angelo M.G., et al. Burden, professional support, and social network in families of children and young adults with muscular dystrophies. Muscle Nerve. 2015;52:13–21. doi: 10.1002/mus.24503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park E.-Y., Nam S.-J. Time burden of caring and depression among parents of individuals with cerebral palsy. Disabil Rehabil. 2019;41:1508–1513. doi: 10.1080/09638288.2018.1432705. [DOI] [PubMed] [Google Scholar]
- 26.Bray L., Carter B., Sanders C., Blake L., Keegan K. Parent-to-parent peer support for parents of children with a disability: a mixed method study. Patient Educ Couns. 2017;100:1537–1543. doi: 10.1016/j.pec.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Ashton J.J., Batra A., Coelho T.A.F., Afzal N.A., Beattie R.M. Challenges in chronic paediatric disease during the COVID-19 pandemic: diagnosis and management of inflammatory bowel disease in children. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-319482. [DOI] [PubMed] [Google Scholar]
- 28.Charte de la rééducation/réadaptation des personnes avec paralysie, cérébrale. Motric Cerebr. 2019;40:116–118. doi: 10.1016/j.motcer.2019.10.001. [DOI] [Google Scholar]
- 29.Rosenbaum P., Gorter J.W. The ‘F-words’ in childhood disability: I swear this is how we should think! Child Care Health Develop. 2012;38:457–463. doi: 10.1111/j.1365-2214.2011.01338.x. [DOI] [PubMed] [Google Scholar]
- 30.Kruijsen-Terpstra A.J.A., Verschuren O., Ketelaar M., Riedijk L., Gorter J.W., Jongmans M.J., et al. Parents’ experiences and needs regarding physical and occupational therapy for their young children with cerebral palsy. Res Dev Disabil. 2016:53–54. doi: 10.1016/j.ridd.2016.02.012. [314–22] [DOI] [PubMed] [Google Scholar]
- 31.Chabrier S., Pouyfaucon M., Chatelin A., Bleyenheuft Y., Fluss J., Gautheron V., et al. From congenial paralysis to post-early brain injury developmental condition: where does cerebral palsy actually stand? Ann Phys Rehabil Med. 2019 doi: 10.1016/j.rehab.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 32.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J., et al. SARS-CoV-2 Infection in Children. New Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.She J., Liu L., Liu W. COVID-19 epidemic: disease characteristics in children. J Med Virol. 2020;92:747–754. doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brodin P. Why is COVID-19 so mild in children? Acta Paediatrica. 2020;109:1082–1083. doi: 10.1111/apa.15271. [DOI] [PubMed] [Google Scholar]
- 35.Huber M., Knottnerus J.A., Green L., van der Horst H., Jadad A.R., Kromhout D., et al. How should we define health? BMJ. 2011;343:d4163. doi: 10.1136/bmj.d4163. [DOI] [PubMed] [Google Scholar]
- 36.Cornec G., Drewnowski G., Desguerre I., Toullet P., Boivin J., Bodoria M., et al. Determinants of satisfaction with motor rehabilitation in people with cerebral palsy: a national survey in France (ESPaCe) Ann Phys Rehab Med. 2019 doi: 10.1016/j.rehab.2019.09.002. [S1877065719301435]. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.