1. Introduction
Primary care provides first-contact, accessible, coordinated, and comprehensive care.1 COVID-19 has dramatically changed how primary care can be safely provided. Face-to-face visits place patients and clinicians at risk of exposure to this deadly virus. On March 15th, 2020, in response to COVID-19 pandemic, the Veterans Health Administration (VHA) issued guidance to review and convert appropriate primary care visits to virtual (e.g. telephone, video, and patient-provider email “secure messages”) care options.2 As one of the largest integrated health systems serving more than 9 million Veterans, VHA was an early adopter of telemedicine technology. In 2016, more than 700,000 veterans received care through a non-face-to-face modality.3 Given this infrastructure, we describe weekly trends in face-to-face visits and virtual visits including telephone, video visits, and secure messages at 1169 primary care practices across national VHA system between January 5th and – June 13th, 2020.
2. Methods
The structure of VHA primary care is team-based and includes primary care providers, nurses, clinical associates, and administrative associates, supported by social workers, pharmacists, and behavioral health specialists.4 Data are derived from electronic medical records and stored at the national VHA Corporate Data Warehouse (CDW) and VHA Support Service Center (VSSC) Capital Assets Databases. We calculated national weekly total services counts by four types of primary care encounters: face-to-face, telephone, video visits, and secure messages. We used a previously developed algorithm to track clinical workload by location and type of health service.5 , 6
We examined weekly trends in primary care encounter types in the 11 weeks prior to mid-March VHA-directive and the 13 weeks after. We further stratified whether the encounter was done by a primary care provider or other team member (e.g. nurse, social worker, or administrative associate). All analyses were performed in R version 3.6.2. This study was completed as part of ongoing quality improvement effort at the VHA and was not considered research activity per VHA policy. Therefore, it was not subject to institutional review board review or waiver.
3. Results
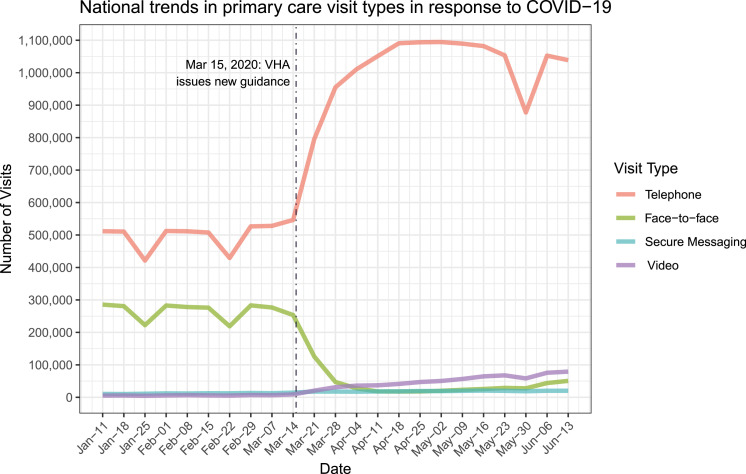
The average number of weekly primary care encounters increased from 784,586 visits prior March 15th to 1,128,587 after, representing an increase of 43.9%. From January to mid-March, there were an average weekly number of 265,798 face-to-face visits, 500,544 telephone visits, 6168 video visits, and 12,074 secure messages (Fig. 1 ). In the 13 weeks after VHA-directive, the number of weekly face-to-face visits decreased to 36,491 visits per week. The use of virtual visits increased dramatically, including telephone visits (1,021,937 per week), video visits (51,144 per week), and secure messages (19,015 per week). Specifically, virtual visits represented 66.1% prior to mid-March but increased to 96.8% of all visit types after. Of all virtual visit encounters, telephone visits had the largest percentage increase from 63.8% prior to mid-March to 90.6% after. During this time, the share of video visits increased by 8-fold going from 0.8% to 4.5%.
Fig. 1.
National trends in primary care viists in response to COVID-19.
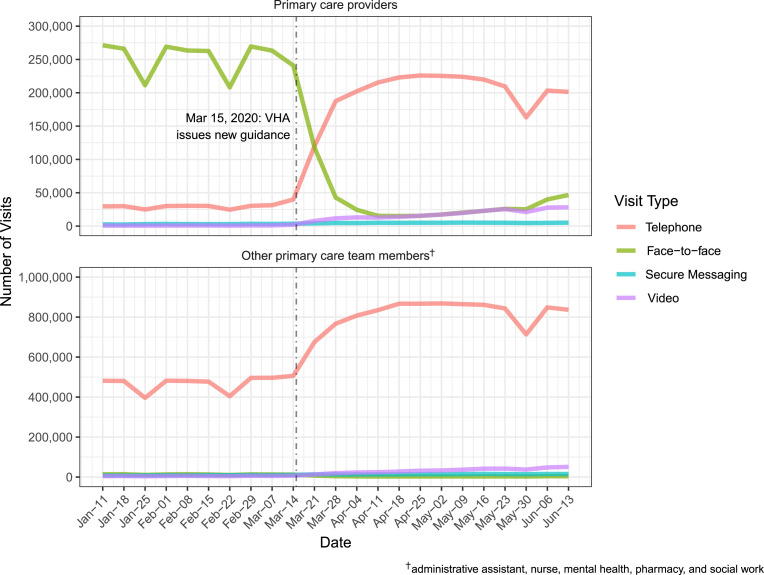
We also examined trends in encounters completed by primary care providers or other members of the primary care team (Fig. 2 ). Overall, the average number of weekly encounters by primary care providers decreased by 10.1%, from 286,602 visits prior to mid-March to 257,680 visits after. From January to mid-March 2020, primary care providers had an average weekly number of 252,591 face-to-face visits, 30,112 telephone visits, 903 video visits, and 2995 secure messages. After mid-March, primary care providers provided an average weekly number of 33,048 face-to-face visits, 201,588 telephone visits, 18,202 video visits, and 4842 secure messages. For primary care providers, the percentage of virtual visits were 11.9% prior to mid-March increased to 87.2% or all visit types after. Of virtual visit types, telephone visits had the largest percentage increase from 10.5% prior to mid-March to 78.2% after. During this time, video visits increased over 26-fold going from 0.3% to 7.1%.
Fig. 2.
National trends in primary care visits in response to COVID-19 (by provider type).
Encounters done by all other primary care team members both prior to and after VHA-directive were mostly conducted via telephone visits throughout this year (94.6% of all encounters). However, the overall number of these encounters increased after mid-March by nearly 75.0%, from 497,165 visits prior to mid-March to 870,008 visits after.
4. Discussion
VHA has rapidly expanded virtual visits in response to COVID-19 primarily by accelerating use of telephone visits. Although we find a modest decrease in the overall number of primary care provider encounters, this was largely offset by a substantial increase in the number of encounters completed by other members of the primary care team.
Our report highlights three important findings. First, outside of the VHA the number of ambulatory visits declined quite dramatically in response to COVID-19, by some estimates a nearly 60 percent drop in visits.7 In contrast, the VHA primary care demonstrated significant resilience by expanding access to virtual visits. Known payment barriers for virtual visits outside the VHA may have limited providers ability to make this shift.8 Second, despite a significant increase in video visits most virtual visits were telephone encounters. This finding highlights key implementation barriers in the VA including training workforce, patient education, and the need to expand technology infrastructure.2 Moreover, many older Veterans have chosen telephone visits due to limited access to home internet and/or smartphones.9 Finally, the substantial increase in encounters done by the primary care team highlight an important role of team-based care. While encounters with the primary care team may not substitute for a visit with a primary care provider, these visits may provide necessary communication to respond to patient questions around the pandemic.10 , 11
Our study has limitations. Misclassification of encounter type is a possibility; however, it is unlikely that providers would systematically misrepresent the type of encounter completed. The descriptive design using aggregated encounter data cannot assess the extent to which virtual care services can substitute for face-to-face care or the consequences of delayed face-to-face care. Given these limitations, we believe future work is urgently needed to evaluate these issues, including the quality and implementation of virtual services. Nonetheless, primary care must continue to rapidly adopt virtual care services as a priority during this pandemic for the safety and health of Veterans everywhere.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by the VHA Office of Primary Care.
References
- 1.Starfield Barbara. Oxford University Press; 1992. Primary Care: Concept, Evaluation, and Policy. [Google Scholar]
- 2.Heyworth L., Kirsh S., Zulman D., Ferguson J.M., Kizer K.W. Expanding access through virtual care: the VA's early experience with Covid-19. NEJM Catalyst Innovations in Care Delivery. 2020;1(4) [Google Scholar]
- 3.Zulman D.M., Wong E.P., Slightam C. Making connections: nationwide implementation of video telehealth tablets to address access barriers in veterans. JAMIA Open. 2019 Oct;2(3):323–329. doi: 10.1093/jamiaopen/ooz024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Helfrich C.D., Dolan E.D., Simonetti J. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. J Gen Intern Med. 2014;29(2):659–666. doi: 10.1007/s11606-013-2702-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adams S.V., Mader M.J., Bollinger M.J., Wong E.S., Hudson T.J., Littman A.J. Utilization of interactive clinical video telemedicine by rural and urban veterans in the Veterans Health Administration health care system. J Rural Health. 2019 Jun;35(3):308–318. doi: 10.1111/jrh.12343. [DOI] [PubMed] [Google Scholar]
- 6.Katz D.A., McCoy K.D., Vaughan‐Sarrazin M.S. Does greater continuity of veterans administration primary care reduce emergency department visits and hospitalization in older veterans? J Am Geriatr Soc. 2015;63(12):2510–2518. doi: 10.1111/jgs.13841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehrotra A., Chernew M., Linetsky D., Hatch H., Cutler D. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges. The Commonw Fund. 2020 [Google Scholar]
- 8.Mehrotra A., Ray K., Brockmeyer D.M., Barnett M.L., Bender J.A. Rapidly converting to “virtual practices”: outpatient care in the era of Covid-19. NEJM catalyst innovations in care delivery. 2020;1(2) [Google Scholar]
- 9.Luger T.M., Hogan T.P., Richardson L.M., Cioffari-Bailiff L., Harvey K., Houston T.K. Older veteran digital disparities: examining the potential for solutions within social networks. J Med Internet Res. 2016;18(11):e296. doi: 10.2196/jmir.6385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reddy A., Wong E., Canamucio A. Vol. 53. Health Services Research; 2018. Association between Continuity and Team‐Based Care and Health Care Utilization: An Observational Study of Medicare‐Eligible Veterans in VA Patient Aligned Care Team; pp. 5201–5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helfrich C.D., Dolan E.D., Fihn S.D. Association of medical home team-based care functions and perceived improvements in patient-centered care at VHA primary care clinics. Healthcare. 2014;2(4):238–244. doi: 10.1016/j.hjdsi.2014.09.008. Elsevier. [DOI] [PubMed] [Google Scholar]