Abstract
Background and aims
The coronavirus disease 2019 (COVID-19) pandemic has caused a significant impact on all aspects of life. One of the comorbidities associated with severe outcome and mortality of COVID-19 is diabetes. Metformin is one of the drugs which is most commonly used for the treatment of diabetes patients. This study aims to analyze the potential benefit of metformin use in reducing the mortality rate from COVID-19 infection.
Methods
We systematically searched the Google Scholar database using specific keywords related to our aims until August 3rd, 2020. All articles published on COVID-19 and metformin were retrieved. Statistical analysis was done using Review Manager 5.4 software.
Results
A total of 5 studies with a total of 6937 patients were included in our analysis. Our meta-analysis showed that metformin use is associated with reduction in mortality rate from COVID-19 infections [RR 0.54 (95% CI 0.32–0.90), p = 0.02, I2 = 54%, random-effect modelling].
Conclusion
Metformin has shown benefits in reducing the mortality rate from COVID-19 infections. Patients with diabetes should be advised to continue taking metformin drugs despite COVID-19 infection status.
Keywords: Coronavirus disease 2019, COVID-19, Metformin, Diabetes, Treatment
Highlights
-
•
Currently, the association between metformin use and COVID-19 has not yet been established.
-
•
Our meta-analysis showed that metformin use is associated with reduction in mortality rate from COVID-19 infections.
-
•
Patients with diabetes should be advised to continue taking metformin drugs despite COVID-19 infection status.
1. Introduction
The global pandemic disease declared by the World Health Organization (WHO), coronavirus disease 2019 (COVID-19), has been caused a significant burden in health and economic aspects around the world. Until now, the number of positive and death cases is still increasing. Therefore, identification of the factors that involve in the development of the severe disease is very important to enable stratification of risk, optimize the reallocation of hospital resources, and guide public health recommendations and interventions. Several comorbid conditions such as hypertension, diabetes, cardiovascular disease, dyslipidemia, and thyroid disease have been identified to be associated with the development of severe outcomes from COVID-19 (Huang et al., 2020; Hariyanto and Kurniawan, 2020a, 2020b). One of the drugs most commonly taken by diabetes patients is metformin. Metformin has demonstrated beneficial effects in lowering blood glucose in patients with diabetes (Bramante et al., 2020). However, the association between metformin use and COVID-19 has not yet been established. This study aims to analyze the potential association between metformin use and the mortality rate from COVID-19 infection.
2. Materials and methods
We conducted a systematic search of the literature on Google scholar using the keywords “metformin” OR “biguanides” AND “coronavirus disease 2019″ OR “COVID-19″, until the present time (August 3rd, 2020) with language restricted to English only. The title, abstract, and full text of all articles identified that matched the search criteria were assessed, and those reporting the rate of metformin use in COVID-19 patients with a clinically validated definition of “mortality” were included in this meta-analysis. The references of all identified studies were also analyzed (forward and backward citation tracking) to identify other potentially eligible articles.
A meta-analysis was performed using Review Manager 5.4 (Cochrane Collaboration) software. Dichotomous variables were calculated using the Mantel-Haenszel formula with random-effects models. We used the I2 statistic to assess the heterogeneity, value of <25%, 26–50%, and >50% considered as low, moderate, and high degrees of heterogeneity, respectively. The effect estimate was reported as risk ratio (RR) along with its 95% confidence intervals (CIs) for dichotomous variables, respectively. P-value was two-tailed, and the statistical significance set at ≤0.05.
3. Results
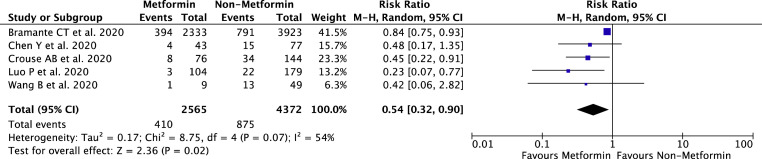
A total of 8110 records were obtained through systematic electronic searches and other ways. After screening titles, abstracts, and full texts, 5 studies (Bramante et al., 2020; Chen et al., 2020; Crouse et al., 2020; Luo et al., 2020; Wang et al., 2020) with a total of 6937 COVID-19 patients were included in the meta-analysis. The essential characteristics of the included studies are summarized in Table 1 , whilst the individual and pooled RRs for the association between metformin use and mortality rate from COVID-19 is shown in Fig. 1 . Our pooled analysis showed a significant association of metformin use with reduction of mortality rate from COVID-19 infection, with high heterogeneity [RR 0.54 (95% CI 0.32–0.90), p = 0.02, I 2 = 54%, random-effect modelling].
Table 1.
Characteristics of included studies.
| Study | Sample size | Design | Taking metformin | Not taking metformin | ||
| n (%) | Age (years) | n (%) | Age (years) | |||
| Bramante et al., 2020 | 6256 | Retrospective cohort | 2333 (37.3%) | 73 ± 10.3 | 3923 (62.7%) | 75.6 ± 12.5 |
| Chen et al., 2020 | 120 | Retrospective cohort | 43 (35.8%) | 62.3 ± 9.6 | 77 (64.2%) | 65.8 ± 11.4 |
| Crouse et al., 2020 | 220 | Retrospective cohort | 76 (34.5%) | N/A | 144 (65.5%) | N/A |
| Luo et al., 2020 | 283 | Retrospective cohort | 104 (36.7%) | 62.3 ± 9.2 | 179 (63.3%) | 64.5 ± 10 |
| Wang et al., 2020 | 58 | Retrospective cohort | 9 (15.5%) | N/A | 49 (84.5%) | N/A |
Fig. 1.
Forest plot that demonstrates the association of metformin with the mortality rate from COVID-19 infection.
4. Discussion
Based on our meta-analysis of available data, metformin use seems to be associated with a reduced risk of mortality from COVID-19 infection. Several reasons can be proposed to explain this result. First, metformin works by inhibiting the ATP synthesis to increase the AMP or ADP levels that in turn indirectly induce the activation of the AMP-activated protein kinase (AMPK) in hepatocytes. AMPK itself has been shown to increase ACE2 stability by phosphorylating ACE2 Ser680 in human umbilical vein endothelial cells and human embryonic kidney 293 cells. Therefore, the usage of metformin will indirectly activate AMPK which leads to ACE2 phosphorylation and finally resulted in conformational and functional changes in the ACE2 receptor through the addition of a phosphate group (PO4 3−). These changes can lead to decreased binding between ACE2 receptor and SARS-CoV-2 Receptor Binding Domain (RBD) due to steric hindrance by the addition of a large sized PO4 3− molecule, thus reducing SARS-CoV-2 infectivity (Ursini et al., 2020; Singh et al., 2020). Second, metformin inhibits the mammalian target of rapamycin (mTOR) signaling via liver kinase B1 (LKB1). It also indirectly attenuates AKT activation through phosphorylation of insulin receptor substrate 1 (IRS-1) that resulted in inhibition of the mTOR signaling cascade. The PI3K/AKT/mTOR pathway plays a major role in MERS-CoV infection, which may also be implicated in the pathogenesis of SARS-CoV-2 infection, given many similarities between these two viruses. Therefore, inhibition of mTOR signaling by metformin may result in a reduction of SARS-CoV-2 infectivity and mortality from COVID-19 infection (Sharma et al., 2020). Finally, through activation of AMPK, metformin can inhibit the inflammatory response that could potentially contribute to mortality through mechanism such as cytokine storm and vascular damage (Singh et al., 2020; Al-Benna, 2020). Therefore, metformin use will decrease the inflammatory response, reducing the incidence of cytokine storm or vascular damage and finally lead to reduction in mortality rate. Patients with diabetes should hence be advised to continue taking metformin during the COVID-19 pandemic given its potential benefit in reducing the mortality rate of COVID-19. Physicians should also consider adding metformin into the regime of their diabetes patients' treatment if the patients have not been given it yet. Finally, the metformin drugs shall be regarded as an important factor in the management plan for COVID-19 patients.
This study has several limitations. First, the presence of confounding factors such as age, other comorbid conditions of patients, and other medications which are taken by patients that can affect the relationship between metformin and the mortality of COVID-19 shall still be considered. Second, no study states the information regarding dosage and duration of metformin treatment in their studied samples, however, we believed that metformin will still give positive impact and benefit from its pharmacodynamics nature regardless of the dosage and duration of treatment. We hope that this study can still give early insight into the further treatment protocol for COVID-19 infections, especially in those with diabetes.
Funding
None.
CRediT authorship contribution statement
Timotius Ivan Hariyanto: Conceptualization, Data curation, Methodology, Investigation, Validation, Visualization, Writing - original draft, Writing - review & editing. Andree Kurniawan: Conceptualization, Validation, Resources, Writing - original draft, Writing - review & editing, Supervision.
Declaration of competing interest
None.
Acknowledgment
None.
References
- Al-Benna S. Association of high level gene expression of ACE2 in adipose tissue with mortality of COVID-19 infection in obese patients. Obes Med. 2020;19:100283. doi: 10.1016/j.obmed.2020.100283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramante C., Ingraham N., Murray T., Marmor S., Hoversten S., Gronski J. 2020. Observational Study of Metformin and Risk of Mortality in Patients Hospitalized with Covid-19. medRxiv. 2020.06.19.20135095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Yang D., Cheng B., Chen J., Peng A., Yang C. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care. 2020;43(7):1399–1407. doi: 10.2337/dc20-0660. [DOI] [PubMed] [Google Scholar]
- Crouse A.B., Grimes T., Li P., Might M., Ovalle F., Shalev A. Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. medRxiv. 2020 doi: 10.1101/2020.07.29.20164020. 2020.07.29.20164020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariyanto T.I., Kurniawan A. Thyroid disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Diabetes Metab Syndr. 2020;14(5):1429–1430. doi: 10.1016/j.dsx.2020.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariyanto T.I., Kurniawan A. Dyslipidemia is associated with severe coronavirus disease 2019 (COVID-19) infection. Diabetes Metab Syndr. 2020;14(5):1463–1465. doi: 10.1016/j.dsx.2020.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang I., Lim M.A., Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14(4):395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo P., Qiu L., Liu Y., Liu X.L., Zheng J.L., Xue H.Y. Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am. J. Trop. Med. Hyg. 2020;103(1):69–72. doi: 10.4269/ajtmh.20-0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S., Ray A., Sadasivam B. Metformin in COVID-19: a possible role beyond diabetes. Diabetes Res. Clin. Pract. 2020;164:108183. doi: 10.1016/j.diabres.2020.108183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A.K., Gupta R., Ghosh A., Misra A. Diabetes in COVID-19: prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. 2020;14(4):303–310. doi: 10.1016/j.dsx.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursini F., Ciaffi J., Landini M.P., Meliconi R. COVID-19 and diabetes: is metformin a friend or foe? Diabetes Res. Clin. Pract. 2020;164:108167. doi: 10.1016/j.diabres.2020.108167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Van Oekelen O., Mouhieddine T.H., Del Valle D.M., Richter J., Cho H.J. A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward. J. Hematol. Oncol. 2020;13(1):94. doi: 10.1186/s13045-020-00934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]