Abstract
Objective
The coronavirus disease 2019 (COVID-19) pandemic has specific implications for oral and maxillofacial surgeons because of an increased risk of exposure to the virus during surgical procedures involving the aerodigestive tract. The objective of this survey was to evaluate how the COVID-19 pandemic affected oral and maxillofacial surgery (OMFS) training programs during the early phase of the pandemic.
Study Design
During the period April 3 to May 6, 2020, a cross-sectional survey was sent to the program directors of 95 of the 101 accredited OMFS training programs in the United States. The 35-question survey, designed by using Qualtrics software, aimed to elicit information about the impact of the COVID-19 pandemic on OMFS residency programs and the resulting specific modifications made to clinical care, PPE, and resident training/wellness.
Results
The survey response rate from OMFS program directors was 35% (33 of 95), with most responses from the states with a high incidence of COVID-19. All OMFS programs (100%) implemented guidelines to suspend elective and nonurgent surgical procedures and limited ambulatory clinic visits by third week of March, with the average date being March 16, 2020 (date range March 8–23). The programs used telemedicine (40%) and modified in-person visit (51%) protocols for dental and maxillofacial emergency triage to minimize the risk of exposure of HCP to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Shortage of personal protective equipment (PPE) was experienced by 51% of the programs. Almost two-thirds (63%) of the respondents recommended the use of a filtered respirator (i.e., N95 respirator) with full-face shield and stated that it was their preferred PPE, whereas 21% recommended the use of powered air-purifying respirators (PAPRs) during OMFS procedures. Only (73%) of the programs had resources for resident wellness and stress reduction. Virtual didactic training sessions conducted on digital platforms, most commonly Zoom, formed a major part of education for all programs.
Conclusions
All programs promptly responded to the pandemic by making appropriate changes, including suspending elective surgery and limiting patient care to emergent and urgent services. OMFS training programs should give more consideration to providing residents with adequate stress reduction resources to maintain their well-being and training and to minimize exposure risk during an evolving global epidemic.
Statement of Clinical Relevance.
The early effects of COVID-19 pandemic on oral and maxillofacial surgery training programs is a topic of interest for all dental specialty training programs during the current pandemic. This study highlights the importance of adequate wellness resources for trainees and the need for structured training for proper use of personal protective equipment and infection control.
Alt-text: Unlabelled box
Coronavirus disease 2019 (COVID-19) has burdened health care systems; interrupted our lives in every aspect, including medical and surgical training programs; and disrupted the economy of societies across the world. The first cases of atypical pneumonia caused by the novel coronavirus were detected in Wuhan city, China, and reported to the World Health Organization (WHO) in December 2019.1 , 2 Subsequently, on January 8, 2020, the Chinese Center for Disease Control and Prevention announced the identification of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), an enveloped, positive-sense, single-stranded RNA virus, as the causative pathogen of COVID-19.3 Since then, the infection by this virus has spread rapidly within weeks to every part of the world. The rapid spread of this virus to every continent was facilitated by ever-increasing international air travel, by the integration of global supply chains, and, in part, by the greater transmissibility of SARS-CoV-2.4 , 5 On January 30, 2020, the WHO declared the COVID-19 outbreak a “Public Health Emergency of International Concern” and, shortly thereafter, on March 11, 2020, classified it as a “pandemic,” at which point, there were 130,000 confirmed cases in 118 countries.6
Health care personnel (HCP), particularly dentists, oral and maxillofacial surgeons, otolaryngologists, head and neck surgeons, craniofacial surgeons, and others who perform surgery of the aerodigestive tract, are at high risk for exposure to this virus. The primary mode of transmission of SARS-CoV-2 is via respiratory droplets (> 5 µm) and through airborne transmission of droplet nuclei (< 5 µm). Manipulation of the upper respiratory tract or the oral mucosa or surgical procedures in the aerodigestive tract can generate aerosol containing virus particles, increasing the risk to personnel operating on these anatomic areas.7 , 8 During the initial phase of the outbreak, data from Wuhan, China, showed that HCP accounted for 29% of the patients, emphasizing the importance of using appropriate PPE to reduce the risk of nosocomial transmission.2 , 7 Around the same time, in January 2020, communication from Stanford University (Stanford, CA) revealed anecdotal evidence of the nosocomial spread of COVID-19 among surgeons and other HCP involved in transsphenoidal pituitary surgery.9 , 10 Also, previous reports from Hong Kong during the first SARS outbreak in 2002–2003 had revealed a high risk to HCP, who accounted for 35% of the cases.11
In the United States, the evolution of this outbreak started with the first case reported on January 19, 2020, in Washington State.12 Less than 2 months after the detection of this index case, a national health emergency was declared in the United States on March 13, 2020. To date, there are greater than 25 million confirmed cases and 848,000 fatalities worldwide, with greater than 6.1 million of these cases and over 180,000 deaths in the United States.13 In the absence of a vaccine and with antiviral therapies with limited effectiveness, management of the COVID-19 pandemic has centered on providing supportive care to those with severe symptoms and the use of physical means, such as quarantine and “social distancing” to mitigate further spread of the disease.14
In the first 2 weeks of March 2020, through personal communication and the mass media, we became aware of the changes that were already being implemented in Washington State and other metropolitan areas, such as San Francisco in California. On March 13, 2020, the American College of Surgeons issued a statement based on preceding events in Italy and China, recommending rescheduling of elective surgeries and shifting inpatient procedures to outpatient settings, when feasible. Subsequently, on March 18. 2020, the Centers for Medicare and Medicaid Services (CMS) issued a directive to halt all elective surgeries, nonessential, nonemergent surgeries, and preventive services.15 This was done to reduce demands on hospitals and their resources, including personnel, PPE, ventilators, beds, and intensive care units (ICUs), and to lower the risk of exposure of health care personnel. The CMS also increased access to Medicare telehealth services for its beneficiaries under the Coronavirus Preparedness and Response Supplemental Appropriations Act. This rapid turn of events led to some urgent modifications to clinical care, including surgery, by U.S. health care providers in all specialties to accommodate the critical shortages of hospital resources as the pandemic was evolving.
At this early stage (March 6–18, 2020), there was sparse information as to what other OMFS training programs in teaching hospitals were experiencing; how they handled emergent procedures; and what measures they established to maintain the safety and wellness of their residents and faculty. This raised the need to survey OMFS training programs and to start a discussion regarding some of the changes in emergency triage, urgent surgical procedures, and the use of PPE to protect health care personnel. By the fourth week of March 2020, most of the professional societies, including the American Association of Oral and Maxillofacial Surgeons, the British Association of Oral and Maxillofacial Surgeons, the British Association of Oral Surgeons, had issued guidance statements regarding the need to minimize exposure risk to HCP. They suggested methods to avoid in-person encounters, such as telemedicine triage, keeping emergency visits brief, and having faculty or senior residents make definitive decisions for treatment to mitigate exposure risk. Further updates were provided for high-risk procedures in the aerodigestive tract, such as nasal endoscopy and tracheostomy.16
The aim of this survey was to assess the impact of COVID-19 on Oral and Maxillofacial Surgery (OMFS) training programs in the different regions of the United States during the early phase of this pandemic—between March 6 and May 6, 2020. As the pandemic was rapidly growing in the United States, we wanted to know what changes were implemented by other OMFS training programs in the country to maintain the safety of their providers and patients while accommodating for the surge of newly infected patients. We specifically asked questions about the management of dental and maxillofacial emergencies, recommendations for PPE during clinical care, staffing changes, and resources used for resident didactic surgical training and wellness.
Materials and Methods
A questionnaire titled “National Survey Assessing the Impact of COVID-19 pandemic on Oral and Maxillofacial Surgery Training Programs” was sent out via electronic mail (e-mail) on April 3, 2020, to the program directors of the 95 of 101 accredited OMFS training programs throughout the United States. We had access to public e-mail addresses of only 95 of 101 accredited OMFS programs at the time the survey was distributed. The questionnaire was developed by using Qualtrics software, which is a valuable online survey tool that allows one to build and distribute surveys and analyze responses. The survey questions were reviewed by the OMFS faculty and an officer of the Boston University's Institutional Review Board, and a waiver for informed consent was granted because none of the questions requested identifiable information about the respondents. This allowed us to expedite the survey distribution during the early phase of this pandemic. The survey was first sent to the 95 OMFS program directors on April 3, 2020, and subsequently a weekly follow-up reminder was sent to those who did not respond and to those who did not complete the survey over a 4-week period until the closing date of May 6, 2020 (Figure 1 ).
Fig. 1.
The situation of the COVID-19 pandemic in the United States on the date (April 3, 2020) the survey was distributed. Source: https://usafacts.org/.
The survey consisted of 35 questions designed to elicit information about the awareness of COVID-19 among personnel in OMFS residency programs and the modifications implemented to meet the response to the COVID-19 pandemic. The survey questions specifically addressed the following: (1) program type and COVID-19 statistics in their region; (2) clinical operations—date of suspension of elective surgery, changes to staffing, changes to outpatient and emergency services, and type of emergent and urgent surgical procedures performed; (3) personal protective equipment (PPE)—type of PPE used during clinical encounters and surgical procedures and any shortage; (4) resident didactic training and wellness—resources used to maintain resident well-being (Table I ). Descriptive statistics were automatically computed by using Boston University's Qualtrics software. We analyzed the data by region to compare the differences in West, Midwest, South, and Northeast United States, as well as U.S. Territories. We compared the differences among the programs that suspended routine clinical activities earlier than March 16, 2020, with those that did so on or after that date.
Table I.
Categories of survey questions on impact of COVID-19 on oral and maxillofacial surgery training programs
| 1. Program type and state COVID-19 statistics |
| 2. Clinical operations modifications |
| 3. Personal protective equipment availability and recommendations |
| 4. Resources for resident training and well-being |
COVID-19, coronavirus disease 2019.
Results
We received responses from 33 of the 95 OMFS residency program directors, for a response rate of 35%. Most of survey responses were completed in the first 2 weeks—that is, between April 3 and April 20, 2020. Only a fifth were completed in the first week of May 2020.
Program type and COVID-19 statistics
Among the OMFS residency programs that participated in this survey, 21% were only hospital based, and 79% were hospital based with university affiliation. The programs that responded to the survey were spread geographically across the United States, with good representation from each of the regions: 4 programs located in the West, 6 in the Midwest, 12 in the Northeast, 10 in the South, and 1 in the U.S. Territories as shown in Figure 2 . The majority of programs used their state registries (39%) and the Johns Hopkins University Coronavirus Resource Center (30%) to obtain COVID-19 statistics. A few of them used the Centers for Disease Control and Prevention (CDC) (9%) to track the COVID-19 cases in their region. The average number of COVID-19–positive cases varied in each region, depending on the survey response date, ranging from 200 to 324,000 in the Northeast; 805 to 60,000 in the Midwest, 414 to 29,000 in the West, 100 to 4800 in the South, and 378 in the U.S. Territories.
Fig. 2.
Geographic distribution of oral and maxillofacial surgery training programs that responded to the COVID-19 survey.
Clinical operations
To understand the impact of COVID-19 on clinical operations, participants were asked to report the date when they actually suspended all nonessential clinical activities in comparison with the date when they were asked to officially suspend clinical activities. Most programs suspended their clinical activities between March 8 and 23, the mean date being March 16, 2020 (Fig. 3, Fig. 4 ). More programs in the West and Northeast suspended regular clinical activities before March 16 (March 8–March 23) in comparison with the majority of programs in the South and Midwest, which limited their clinical activities a little on or after March 16 (March12–March 23). When we compared the differences in COVID-19 statistics by using a single-tailed t test, there was no statistical difference in the number of COVID-19 cases between the states that suspended clinical activities early and those that suspended them late (P = .14).
Fig. 3.
The cumulative number of residency programs (n = 33) who suspended their elective and nonurgent surgical procedures relative to the dates pertinent to COVID-19 guidelines and announcements. AAOMS, American Association of Oral and Maxillofacial Surgeons; CDC, Centers for Disease Control and Prevention; CMS, Centers for Medicare and Medicaid Services; WHO, World Health Organization.
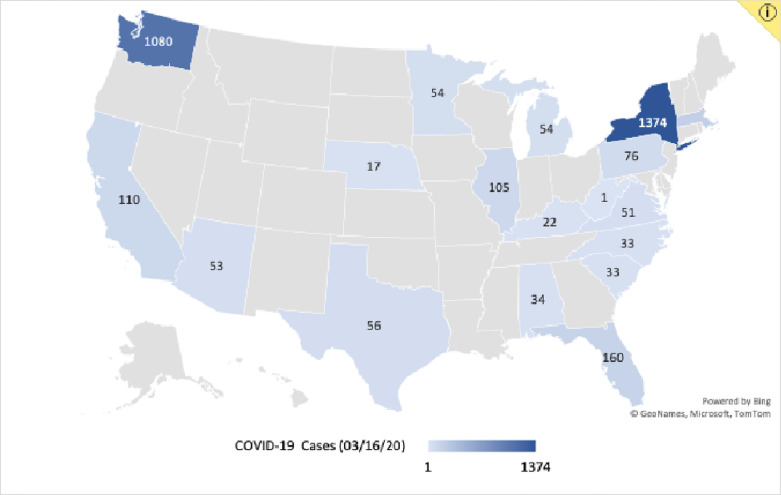
Fig. 4.
The number of COVID-19 cases in the various states of participating oral and maxillofacial surgery (OMFS) training as of March 16, 2020, the average date of suspension of elective surgery and routine clinical activities. Source: GeoNames, Microsoft, TomTom.
Range of clinical services
In the midst of the COVID-19 pandemic, all participating programs continued to provide limited patient services. These included emergency dental services (93.9%); emergent and urgent surgical procedures, such as repair of facial fractures or oncologic resection and reconstruction (93.9%); postoperative follow-up visits (75.8%); inpatient dental consultations (72.7%); and new outpatient consultations (36.4%) (Figure 5 ). None of the programs reported provision of elective or nonessential surgical procedures, such as dental implant, dentoalveolar, orthognathic, and temporomandibular joint surgeries.
Fig. 5.
The range of oral and maxillofacial surgery services provided by training programs during the COVID-19 pandemic.
The postoperative follow-up visits were completed through either a combination of telemedicine and in-person outpatient clinic visits (42.4%) or in-person outpatient clinic visits only (36.4%) or telemedicine only (21.2%). The in-person clinic visits were primarily reserved for postoperative infections; dressing change; drain, suture, or splint removal; or other postoperative care that cannot be accomplished through telemedicine alone. In these instances, prescreening through telemedicine was often completed before the in-person clinic visit.
Emergency services
All participating programs implemented a modified dental and maxillofacial emergency triage protocol. These emergency services were primarily rendered in the hospital setting in the emergency department (ED) (37.8%) or in the OMFS ambulatory clinic (28.4%). Emergency services were provided less often (16.2%) in the dental school setting. Remote consultation for emergency care was also provided through telemedicine (17.6%) by a limited number of programs. During the COVID-19 pandemic, the majority of programs (76%) reported an average reduction of 63% in ED encounters. A few programs (6%) reported a 15% average increase in the number of ED encounters, and the remaining reported no change during the pandemic. When asked about the frequency of the ED encounters 82% of the programs reported less than 10 encounters per day, with the majority reporting having less than 5 encounters. Only 15% reported greater than 10 ED encounters daily. The type of ED encounters are shown in Figure 6 .
Fig. 6.
Type of oral and maxillofacial surgery emergency department patient encounters reported during the COVID-19 pandemic.
Treatment
Emergent surgical procedures in the operating room were rendered by 93.9% of programs, whereas 6.1% provided no operating room services during this time. The emergent surgical procedures that were performed in the operating room during the pandemic are shown in Figure 7 . The emergency procedures conducted in the ambulatory (hospital or dental school) setting included clinical evaluation for dental emergencies, extractions, splinting dentoalveolar fractures, incision and drainage of dental abscesses, and closed reduction of mandibular fractures (Figure 8 ).
Fig. 7.
Type of oral and maxillofacial surgery procedures performed in the operating room during the COVID-19 pandemic.
Fig. 8.
Oral and maxillofacial surgery services provided in the ambulatory clinic setting during the COVID-19 pandemic.
Staffing changes
Respondents were asked to report any changes to faculty and resident schedules, including reallocation to other specialty services. The majority (93.9%) of the programs reported a reduction to a minimum number of essential faculty and residents present on site daily, whereas a few programs (6.1%) reported no changes in their daily schedules. Additionally, 25 of 33 programs (75.8%) reported that they had institutional protocols to reassign or delegate OMFS attendings, residents, and staff to other responsibilities during the COVID-19 pandemic. OMFS residents were reallocated to other services in 14 institutions (56%), with majority of the reassignments being made to medical and surgical ICUs, COVID-19 ICU, trauma and acute care surgery, internal medicine services, and COVID-19 testing centers. Five programs (20%) reported reallocation of OMFS attendings to other services, including trauma, emergency medicine, and medical and surgical ICUs. No reassignment protocols were implemented at 8 of 33 institutions (21.2%) and 1 program (3%) reported being unsure about the existence such protocols. Of note, 21% of the participating OMFS programs reported 1 or more trainees, staff, or faculty members testing positive for COVID-19.
Personal protective equipment
Sixteen of 33 programs (48.5%) reported no PPE shortages, whereas 51.5% of programs reported a shortage. Of those that experienced a shortage, the most common were of N95 respirators (94.1%); surgical masks with full-face shield (35.3%); or surgical masks (29.4%). Almost all programs (97%) reported following the guidelines established by their hospitals, with the exception of 3% that followed state health department guidelines. Of the 97% that followed hospital guidelines (28.1%) used these guidelines alone, whereas 65% reported using them in combination with other guidelines, including those from the CDC, dental school (21.9%), and state dental society (3.1%). There were no major differences with regard to the level of PPE recommended, regardless of the clinical setting—operating room versus ambulatory clinic or ED—for oral surgical procedures. There was a slight preference for using a powered air-purifying respirator (PAPR) in the operating room. Practitioners had a number of guidelines on appropriate PPE use while performing procedures.
The PPE recommended by OMFS training programs during dental procedures, such as nonsurgical extractions or incision and drainage, in the ED and ambulatory clinic settings for use by patients with unknown COVID-19 status, as well as COVID-19–negative and COVID-19–positive patients are shown in Figure 9 . In the operating room setting, the level of PPE recommended for aerosol-generating procedures involving the aerodigestive tract for use by patients of unknown COVID-19 status comprised primarily an N95 respirator with full-face shield, disposable gown, and gloves (61.5%). Other responses included PAPR with disposable gown and gloves (20.5%) (Figure 10 ).
Fig. 9.
PPE recommended for emergency department and ambulatory clinic procedures involving the aerodigestive tract, based on patient COVID-19 status. PPE, personal protective equipment; PUI, persons under investigation.
Fig. 10.
Personal protective equipment (PPE) recommendations for operating room procedures involving the aerodigestive tract, based on patients with unknown COVID-19 status.
Resident training and well-being
A number of guidelines influenced changes in resident didactic activities during the COVID-19 pandemic. These included internal departmental guidelines (33.3%); the Commission on Dental Accreditation guidelines (27.3%); university guidelines (25.8%); Accreditation Council on Graduate Medical Education guidelines (10.6%); and the American Dental Association guidelines (3%) (Figure 11 ). All OMFS programs reported continuation of their core didactic training protocols during the COVID-19 pandemic. These consisted of talks and lectures for attendings and residents (41.2%); journal club (29.7%); and interdisciplinary conferences, such as trauma, airway, or pathology conferences, tumor boards, and sleep or craniofacial clinics (28.4%). In addition, various self-study activities were used by residents during this period. The program directors reported that residents used collaborative interinstitutional webinars, textbooks, departmental didactics, and other lecture series delivered by multiple oral maxillofacial specialty organizations (Figure 12 ). The digital communication platforms that worked best for conducting OMFS didactic programs were Zoom (76%); GoToMeeting (6%); Microsoft Teams (6%); Webex (6%); BlueJeans (3%); and Blackboard Collaborate (3%) (Figure 13 ).
Fig. 11.
Guidelines used to help implement changes in resident didactic activities during the COVID-19 pandemic. ACGME, Accreditation Council on Graduate Medical Education; ADA, American Dental Association; CODA, Commission on Dental Accreditation.
Fig. 12.
Resources used for didactic resident education and training. ACOMS, American College of Oral and Maxillofacial Surgeons; IAMOS, International Association of Oral and Maxillofacial Surgeons; OMSKU, Oral and Maxillofacial Surgery Knowledge Update.
Fig. 13.
Video conferencing platforms used by residency programs to conduct didactic activities during the COVID-19 pandemic.
The COVID-19 pandemic challenged residents, faculty, and staff physically, mentally, and emotionally. During this time, wellness programs were of particular importance to maintain the health and safety of the trainees. Many institutions and OMFS programs offered initiatives, such as meditation and mindfulness seminars (32%); yoga and exercise routines (17%); free or reduced-fee transportation (17%); food delivery services (26%); counseling services (4%); and free hotel accommodation (4%) (Figure 14 ).
Fig. 14.
Wellness initiatives offered to oral and maxillofacial surgery (OMFS) residents, faculty, and staff during the COVID-19 pandemic.
Discussion
The purpose of this survey was to understand the impact of the COVID-19 pandemic during the early phase (March 6–May 6, 2020) on OMFS training programs in the United States. This national survey was sent to OMFS program directors to specifically ask about the changes implemented by their institutions and departments to maintain the safety of both health care providers and patients while accommodating for the surge of newly infected patients. For most of us, COVID-19 pandemic is an unparalleled event in our lives. In such a situation, a survey can be a valuable tool to investigate the actions or attitudes of individuals, and the results can reveal information that can help make decisions, come to a consensus, or evoke a discussion on an event or subject that is not well understood. Many past events, such as the H1 N1 pandemic in 2009; the SARS epidemic (2002–2003); natural disasters (floods, cyclones); or emergency crises (Boston Marathon bombing or 9/11 terrorist attack in New York City), required health care personnel to respond promptly, with caution and valor, risking their lives; however, the impact of this pandemic is unique for several reasons. Unlike the earlier disease outbreaks, which were largely regional epidemics/events with similar patterns, COVID-19 has spread rapidly across the globe, disrupting the social, economic, and emotional well-being of most societies. HCPs are required to make rapid changes within hours/days to adapt and work with such challenges as physical and social distancing, additional uncomfortable PPE, and shortage of hospital resources and to function under stressful conditions with limited assistance and with limited knowledge about the virus. As the pandemic has evolved, the governing authorities have had to rapidly modify plans from an “emergency preparedness” mode to the possibility of resorting to a “crisis standards of care” and make ethical decisions to accommodate the surge.17
Specific to OMFS and other specialties that work on the aerodigestive tract is the concern regarding increased exposure risk because of aerosol-generating procedures in the oral cavity, nose, and/or oropharynx.7 , 10 , 16 , 18, 19, 20 Many specialty organizations have documented recommendations to minimize exposure risk during performance of aerosol-generating procedures, including emergency airway procedures in the head and neck region.21 , 22 Additionally, SARS-CoV-2 is a novel virus, and there are still many gaps in the understanding of its behavior, particularly regarding the duration of viral shedding from the upper respiratory tract (12–31 days); the infectious period; the temporal changes in viral load in the aerodigestive tract of an infected individual; and the relationship between viral load and viral replication23, 24, 25 Also, HCPs working under stress caused by shortage of resources can experience anxiety regarding the well-being of their families and practical issues, such as childcare, housing, and food, during such a crisis.18 , 26 These were some of the factors that prompted us to perform our survey during the early phase of the pandemic.
We had a 35% survey response rate, representing 33 of 95 OMFS programs surveyed in all regions. The majority of our survey respondents were located in states with a high incidence of COVID-19, with 9 of the 33 early survey responses coming from New York state. This may be attributed to the rapidly changing situation in that region and to the awareness of OMFS program directors encountering many questions or dilemmas, just as we did, during the early phase of this pandemic. The vast majority (79%) of the survey responses came from hospital-based, university-affiliated programs. We speculated that hospital-based programs, particularly large academic centers, would have more prompt institutional support, direction, and assistance in terms of resources to support their HCPs and have access to sufficient supply of PPE from sponsoring industries.
Most OMFS training programs suspended their clinical activities by the middle of March 2020. As of March 16, 2020, the number of reported COVID-19 cases were as few as 1 case in West Virginia and 1374 in New York, with a mean of 186 cases and total of 4300 confirmed cases in the United States (see Figure 4). In comparison, merely after 2 months, on May 25, 2020, the CDC reported greater than 1.6 million confirmed cases and 100,000 deaths. This exponential increase in the number of cases reveals the speed of transmission of SARS-CoV-2 virus.27 As in the case of SARS-CoV, the angiotensin-converting enzyme-2 receptor is the primary entry point into the cell for SARS-CoV-2 via protease activation of the S (spike) protein on the viral surface. The affinity of the spike protein of SARS-CoV-2 for the angiotensin-converting enzyme-2 receptor is 10- to 20-fold that of SARS-CoV, which may, in part, explain its more rapid rate of spread.28 The other reason for this rapid transmission of disease is that without a vaccine or other prophylactic treatments, the best method to contain the virus and decrease the spread of COVID-19 is through strict enforcement of social and physical distancing. These measures were not instituted until the end of March or early April 2020 in a number of U.S. states. The results from our survey and a review of reports from state websites have revealed that by the third week of March 2020, only 9 states, including Washington, California, Illinois, Ohio, Louisiana, New York, and New Jersey, had implemented strict social distancing or “shelter-in-place” orders. In some metropolitan areas, such as San Francisco, where governing authorities took early action, the disease was contained, and they reported a lower number of cases and fatalities (2350 cases and 40 deaths). This lower number cannot be explained by the enforcement of social distancing measures alone. Other factors, such as demographic characteristics and socioeconomic factors, played a significant role.
On our survey, 7 of 33 programs (21%) reported trainees or faculty members being infected by SARS-CoV-2. This is inevitable, given the nature of the professional responsibilities and the types of procedures performed, especially in the context of shortage of PPE during the pandemic. Lancaster et al. reported on how the surgery department at an academic medical center optimized human resources. They identified key skills in each team member and ensured that there were multiple team members with similar skill sets to accommodate for absences in case any of the members were infected. They also ensured that faculty worked at single hospital sites and reduced the number of providers on site each day, with contingency plans for section or department leadership.29 Similarly, other surgical departments rapidly redesigned and shifted their workforce, depending on need.30
A number of OMFS trainees and faculty were redeployed to other services during the surge/height of the pandemic, as needed. More residents were redeployed in comparison with faculty. Fourteen of the 33 programs reported reallocation of residents to other services, including COVID-19 wards, and 5 of 33 programs reported redeployment of faculty. This may be a reflection of the number of trainees on their General Surgery, Medicine, or Anesthesia rotations. Ten of these 14 programs were dual-degree programs. Personal communication with program directors revealed 1 OMFS trainee fatality during the early phase of this pandemic. In its manual on how to protect health care personnel during global epidemics, the WHO has proposed recommendations to educate HCPs regarding ways to reduce exposure risk, reduce anxiety and fear, and promote health and well-being. The manual also emphasized the importance of direct, face-to-face communication with HCPs in a fair environment without blame.26
Clinical operations
All programs directors responded that only urgent and emergent procedures were performed during the pandemic. About 9% of the participants continued to provide new patient consultations. It was not clear whether these were urgent and whether they were performed by using telemedicine. About 63% of the programs reported using some form of telemedicine for patient care, mainly for postoperative follow-up. Active participation in clinical care through telemedicine can complement residents’ clinical training and facilitate emergency triage by decreasing exposure risk. On March 17, 2020, several temporary regulatory waivers and new rules were ordained to allow flexibility in the health care system to respond to the COVID-19 pandemic. This temporary relaxation in regulations helped many patients seek care in nontraditional ways, such as through telehealth, allowing hospitals to deal with patient surges.31 When in-person encounters were necessary, institutions and professional organizations have recommended that the most experienced or skilled team member assess the patient to make definitive treatment decisions to limit exposure of multiple individuals. As a result, surgical faculty in many institutions, including those in the Boston area, performed surgical procedures either independently or with another faculty member or senior resident when assistance was necessary. Operating during these conditions can be difficult, stressful, and more prone to errors. It is important to take the time to plan, delegate, and make difficult decisions.32 Many treatment decisions during the pandemic had to be modified even for emergent and urgent situations. Dilemmas, such as surgery versus a nonsurgical alternative, immediate treatment versus delayed treatment, and hospital care versus outpatient care, were faced by clinicians during the height of the pandemic while preparing for the surge. When making these ethical decisions, it is important to consider the risks and benefits from a societal standpoint as well as from the individual patient's perspective.
Reduction in the volume of operating room procedures was difficult to estimate because our questionnaire did not specifically ask programs to quantify this. On the basis of our institutional experience, we expected an 80% to 85% reduction in operating room volume after the CMS directive on March 18, 2020, to suspend elective and nonessential surgeries.15 Most OMFS programs reported about 62% reduction in ED patient encounters. Despite the significant reduction in patient encounters, cases of deep neck infections and maxillofacial injuries continued to present and comprised the majority of OMFS ED encounters. The number of maxillofacial injuries resulting from assaults was higher than those from motor vehicle accidents and falls. This can be expected because of the increase in violence, possibly resulting from food and shelter insecurity and frustration arising from social distancing. The number of cases of trauma from assault was higher compared with that from motor vehicle accidents during the pandemic, and this can be explained by the reduced road traffic during the pandemic. Increases in the rates of domestic violence and aggression among incarcerated and homeless individuals have been reported during the pandemic.33
Extraordinary situations, such as this pandemic, require strong leadership providing direction to all and cohesive teams that can work well and respond to take actions immediately. The leadership in OMFS has made tremendous efforts at local, state, and national levels to educate and to disseminate and share information about COVID-19 through national web conferences, and the American Association of Oral and Maxillofacial Surgeons website. Oral and Maxillofacial Surgeons in various hospitals and academic medical centers made schedule changes rapidly to manage dental emergencies, odontogenic infections, maxillofacial injuries, and oncologic cases, taking necessary precautions, with the use of airborne infection isolation rooms (AIIR), negative pressure rooms, telemedicine triage, and appropriate PPE for aerosol-generating procedures (e.g., eye protection, filtered face respirators [N-95], full-face shields, PAPRs).
Personal protective equipment
The access to and use of PPE has been a major concern during this pandemic. We felt that the choice of PPE may be influenced by their availability in institutions. Therefore, we questioned participants on what they would recommend rather than what PPE they used during the pandemic. A little over half of the participating programs (52%) reported PPE shortage. Those experiencing shortage reported the shortage of N95 respirators being the most common (94.1%) and that it led to the subsequent plan to recycle N-95 masks. There was overwhelming consistency in the PPE recommendations for all OMFS procedures, given the high risk for exposure to SARS-CoV-2. Most of the surgeons (62%) recommended N-95 respirators with full-face shield, in conjunction with fluid-resistant gown and gloves. PAPRs were recommended by a few (21%) for operating room procedures. All programs reported having hospital guidelines in place for the appropriate use of PPE. There is evidence that PAPRs provide greater protection because of their higher microbial filtration efficiency compared with N-95 masks; however, these devices can be cumbersome and preclude the use of head lights and the ability to communicate well with others during surgery. Surgeons in other related specialties consider PAPRs as essential for optimal safety while performing aerosol-generating procedures. Otolaryngologists have recommended the use of higher-level PPE during aerosol-generating procedures as a precautionary measure. They also feel that further clarification is necessary to determine the type of PPE to reduce the risk of exposure.7 Hirschmann et al. recommended that PPE for orthopedic surgeons working in a COVID-19 environment should consist of level 4 surgical gowns, full-face shields or goggles, double gloves, and FFP2-3 or N95-99 respirator masks.34 Awad et al. presented a detailed outline of perioperative guidelines for PPE, personal care, and hygiene to minimize exposure risk to HCPs when providing emergent care to suspected or COVID-positive patients.35
Resident training
All training programs responded that their residents had access to virtual didactic training sessions and self-study resources. It was important to have some structure to the didactic training and to continue their core activities by using virtual classroom technology. Residents were resourceful and attended several education webinars. Educational programs, such as the COVID Collaborative Lecture Series (3 hours per week) hosted by the University of Michigan and partner institutions, have become popular. Such initiatives may be the beginning of a national curriculum. Other surgical specialties, such as Otolaryngology and Urology, have reported using similar collaborative lecture series. They also used surgical simulations models for training residents.36 The most common digital platform used was Zoom. Some others used Microsoft Teams, which has better security features and collaborative options. The cost, the real-time collaborative features, and the number of participants allowed can vary in each of these video-conferencing applications.37 Our survey did not address the question about resident research activities, but personal communication with a number of programs revealed that many residents and faculty were productive in research and scholarly activities.
Steadiness, compassion, and resilience are important qualities to nurture during such demanding times. Among the surveyed OMFS programs, 73% (24 of 33) reported that their residents had access to wellness programs, such as mindfulness and meditation seminars, yoga, and other exercise activities. Some programs reported access to tele-psychiatry services, if necessary, to relieve anxiety and stress. Some other specialties reported the benefits of virtual departmental social hours. To facilitate connecting with colleagues and faculty, they made time for social hours within their weekly schedules. Practical issues affecting HCPs include childcare, housing, and meals. Our survey revealed that many residents used food delivery, transportation, and housing services.
Similar surveys have been conducted by most surgical specialties, including Otolaryngology, Urology, Orthopedic Surgery, and General Surgery.30 , 36, 37, 38 They reported more stringent schedules to manage the staffing shortages and structured didactic training, including virtual surgical simulation programs, seminars, and access to video libraries, as well as time for virtual social hours with colleagues and faculty. A qualitative study conducted by He et al. surveyed General Surgery residents in 2 major hospitals in the Boston area regarding their concerns about the COVID-19 outbreak.26 Most residents responded that their main concern was the health of their older family members and the possibility of transmitting the infection to them. They did not worry as much about increased work load or even getting the SARS-CoV-2 virus infection themselves.26 He et al. also emphasized the recommendations of the WHO that HCPs should be educated well about exposure risk through direct face-to-face communication in a blame-free environment during such global epidemics.
Limitations
One of the limitations of such a survey is the cross-sectional design, which only provides an overview of a single snapshot in time. Further follow-up surveys during the year will be necessary to understand the long-term impact of the changes made during the pandemic and which of these changes will be required to be maintained over time. Such surveys have the risk of recall bias and conformity bias. Additionally, there is a risk of cognitive dissonance—that is, the responder may answer questions based on what he or she believes rather than what was performed or actually happened. A brief weekly online survey tracking the knowledge and perceptions of all OMFS residents and faculty in training programs can be performed in real time, gather longitudinal data to overcome some of these risks, and inform or guide decisions during rapidly evolving infectious disease outbreaks. We surveyed the program directors of the training programs rather than the residents. Unfortunately, the results of this survey do not inform us how the residents were educated to minimize their risk of exposure. Future surveys can include questions regarding COVID-19 training to minimize exposure risk to HCPs, testing for COVID-19, and specific questions regarding aerosol-generating procedures. Information about the perioperative use of oral antiseptic preparations (2% povidone iodine solution or 3% hydrogen peroxide solution); suctioning methods used; type of drills used; use of advanced energy devices (cautery); intubation and extubation protocols; tracheostomy; and nasal endoscopy. Such pertinent surgical recommendations for procedures in the aerodigestive tract were implemented after we designed and distributed the survey. Despite these limitations, our survey did provide some valuable insight into the impact of the COVID-19 pandemic on OMFS training programs.
Conclusions
OMFS training programs responded in a timely fashion by limiting their clinical operations to emergent and urgent services during the early phase of the COVID-19 pandemic (March 6–May 6, 2020) and took measures to minimize the risk of exposure of their HCPs by using telemedicine triage, recommending appropriate PPE, and limiting staff on site. About half the programs reported experiencing PPE shortages (N-95 respirators). We should provide OMFS residents more resources for stress reduction to maintain their well-being and structured training to decrease exposure risk during such crises. A follow-up survey will be necessary to understand the long-term effects of the pandemic on residents and training programs. Future surveys should be centralized and designed to be performed in real time during an evolving global epidemic.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P., Yang X.-L., Wang X.-G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corman V.M., Landt O., Kaiser M. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phelan A.L., Katz R., Gostin L.O. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. 2020 Jan 30 doi: 10.1001/jama.2020.1097. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 7.Mick P., Murphy R. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: a literature review. J Otolaryngol Head Neck Surg. 2020;49:29. doi: 10.1186/s40463-020-00424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel Z.M., Fernandez-Miranda J., Hwang P.H. Letter: Precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020;87:E66–E67. doi: 10.1093/neuros/nyaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vukkadala N., Qian Z.J., Holsinger F.C., Patel Z.M., Rosenthal E. COVID-19 and the otolaryngologist—preliminary evidence-based review. Laryngoscope. 2020 Mar 26 doi: 10.1002/lary.28672. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Liu S., Chan T.C., Chu Y.T. Comparative epidemiology of human infections with Middle East respiratory syndrome and severe acute respiratory syndrome coronaviruses among healthcare personnel. PLoS One. 2016;11 doi: 10.1371/journal.pone.0149988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. WHO coronavirus disease (COVID-19) dashboard COVID 19 [Webpage] 2020 June 21, 2020 [cited 2020 May 28, 2020]. Available at: https://covid19.who.int/.
- 14.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa020. taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Medicare and Medicaid Services (CMS) CMS; Baltimore, MD: 2020. CMS Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. [Google Scholar]
- 16.Magennis P.A., Kumar N.Updated COVID-19 Advice from BAOMS and ENT UK for our surgical teams. COVID-19 2020 May 4, 2020 [cited April 15, 2020]. Available at: https://www.baoms.org.uk/about/news/124/updated_ppe_covid19_advice_ from_baoms__ent_uk.
- 17.Hanfling D., Hick J.L., Stroud C., editors. Crisis Standards of Care: A Toolkit for Indicators and Triggers. National Academies Press; Washington DC: 2013. [PubMed] [Google Scholar]
- 18.The Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kulcsar M.A., Montenegro F.L., Arap S.S., Tavares M.R., Kowalski L.P. High risk of COVID-19 infection for head and neck surgeons. Int Arch Otorhinolaryngol. 2020;24:e129–e130. doi: 10.1055/s-0040-1709725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg. 2020;48:521–526. doi: 10.1016/j.jcms.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tay J.K., Khoo M.L., Loh W.S. Surgical considerations for tracheostomy during the COVID-19 pandemic: lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg. 2020 Mar 31 doi: 10.1001/jamaoto.2020.0764. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Kowalski L.P., Sanabria A., Ridge J.A. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42:1259–1267. doi: 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yi Y., Lagniton P.N.P., Ye S., Li E., Xu R.H. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020;16:1753–1766. doi: 10.7150/ijbs.45134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y., Li L. SARS-CoV-2: Virus dynamics and host response. Lancet Infect Dis. 2020;20:515–516. doi: 10.1016/S1473-3099(20)30235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu F., Yan L., Wang N. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He K., Stolarski A., Whang E., Kristo G. Addressing general surgery residents' concerns in the early phase of the COVID-19 pandemic. J Surg Educ. 2020;77:735–738. doi: 10.1016/j.jsurg.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kucharski A.J., Russel T.W., Diamond C., Centre for Mathematical Modelling of Infectious Diseases COVID-19 working group Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect Dis. 2020;20:553–558. doi: 10.1016/S1473-3099(20)30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ou X., Liu X., Li P. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lancaster E.M., Sosa J.A., Sammann A. Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg. 2020;230:1064–1073. doi: 10.1016/j.jamcollsurg.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brethauer S.A., Poulose B.K., Needleman B.J. Redesigning a department of surgery during the COVID-19 pandemic. J Gastrointest Surg. 2020;24:1852–1859. doi: 10.1007/s11605-020-04608-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Medicare and Medicaid Services (CMS) CMS; Baltimore, MD: 2020. Medicare telemedicine health care provider fact sheet. [Google Scholar]
- 32.Ellis R., Hay-David A.G.C., Brennan P.A. Operating during the COVID-19 pandemic: how to reduce medical error. Br J Oral Maxillofac Surg. 2020;58:577–580. doi: 10.1016/j.bjoms.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;29:549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hirschmann M.T., Hart A., Henckel J., Sadoghi P., Seil R., Mouton C. COVID-19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc. 2020;28:1690–1698. doi: 10.1007/s00167-020-06093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Awad M.E., Rumley J.C.L., Vazquez J.A., Devine J.G. Perioperative considerations in urgent surgical care of suspected and confirmed COVID-19 orthopaedic patients: operating room protocols and recommendations in the current COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:451–463. doi: 10.5435/JAAOS-D-20-00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kwon Y.S., Tabakin A.L., Patel H.V. Adapting urology residency training in the COVID-19 era. Urology. 2020;141:15–19. doi: 10.1016/j.urology.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cai Y., Jiam N.T., Wai K.C. Otolaryngology resident practices and perceptions in the initial phase of the U.S. COVID-19 pandemic. Laryngoscope. 2020 May 5 doi: 10.1002/lary.28733. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]