Abstract
Aim
This study audits the delivery and standards of New Zealand (NZ) inflammatory bowel disease (IBD) care against international standards, with emphasis on the IBD nursing role.
Methods
Utilising international standards in IBD care, a 3 phase national multicentre survey study was performed between 2015 and 2019. We 1) evaluated the current role and practices of IBD nurses, 2) evaluated IBD service provision and identified areas for improvement, and 3) audited key aspects of IBD patient care, directly comparing nurse-led and doctor-led outpatient clinics.
Results
The median duration spent in an IBD nursing role was 21 months (range 2 to 120 months) with the majority (12/15) performing two or more nursing roles. The median IBD nurse full-time equivalent (FTE) was 0.8 (range 0.2 to 1.25). The average number of hours spent undertaking IBD nursing tasks was 22.2 – a 6.8-hour shortfall compared to rostered hours. No service had a per capita IBD multidisciplinary team (MDT) FTE which met international standards. Just under two-thirds (62.5%) of departments held a regular MDT meeting. All responding services could be contacted directly by IBD patients and respond within 48 hours of contact. During 492 doctor-led and 196 nurse-led scheduled outpatient clinic visits, nurses were significantly more likely to document weight, smoking status and organise appropriate colonoscopic surveillance than doctors.
Conclusion
Multiple nursing job roles resulted in rostered hours being insufficient to complete IBD specific tasks. IBD FTE did not meet international standards. The IBD care was patient-centred, encouraging direct contact from patients with prompt response. IBD nurses in NZ provide high-quality outpatient care when measured against auditable standards. As the IBD nursing role continues to develop, following the implementation of an educational framework and education programme, an increase in numbers is required in order to achieve the recommended minimum FTE per 250 000 population.
Keywords: inflammatory bowel disease, standards, specialist nursing, New Zealand
Introduction
Inflammatory bowel disease (IBD) is a chronic medical condition, commonly affecting adolescents and young adults, which impacts significantly on patients’ personal, social and work life. Lifetime medical costs associated with IBD care are comparable to those of other chronic diseases such as diabetes mellitus or cancer.1
Whilst no national studies quantifying the prevalence of IBD have been undertaken, extrapolated data from local studies estimate a prevalence of 20,792 affected individuals with 1 in 227 New Zealanders affected.1 This places New Zealand’s IBD prevalence amongst the highest in the world and, with a 5.6% increase year on year from 2004 to 2016, the IBD patient population is projected to double by 2026.1
“Standards of Care” are those “which a minimally competent physician in the same field would do under similar circumstances”2 These standards provide guidance as to the structure (ie, system-level factors) which influence how care is delivered, and process (ie, the actions required to move through the structure) in order to provide care for a defined illness.3
High-quality IBD patient care is based upon a collaborative multidisciplinary team (MDT) approach. Standards for care delivery, including the ideal team complement of an IBD service, have already been published in Australia,4 United Kingdom (UK)5 and Canada.6
Whilst an established role overseas, facilitated by formal postgraduate qualifications, the IBD nursing role in New Zealand (NZ) remains in its infancy. IBD nurses provide essential links between the IBD service, the patient and primary care providers. This facilitates rapid access to locally delivered care, maintains a patient-centred service and provides patient education and support.3,7-9
The aim of this study was to audit IBD care across New Zealand against international standards, with particular emphasis on the IBD nursing role.
Methods
A Medline search identified international audits and standards of care. We reviewed all audits of IBD care and identified audit fields directly pertaining to nursing care. These standards provided an audit framework.
A national multicentre study, carried out over a four year period 2015 to 2019, was divided into three discrete phases:
Phase 1 (2015): Evaluation of the Current Role and Practices of Those Nurses Who Self-Identify as an IBD Nurse
Twenty IBD nurses, distributed across New Zealand, were identified from an existing email network and invited to participate in a 10 question survey (Appendix Table 1). The survey was performed using the Survey Monkey platform with data collated using Excel spreadsheets. The aim of this survey was to evaluate the time spent in role as an IBD nurse, the responsibilities in that role, resources available for professional development and educational resources available to patients. The survey also asked for comments regarding IBD nursing in New Zealand.
Repeat invitations, including telephone contact and email, were used to improve response rates.
Phase 2 (February 2016–February 2017): Evaluation of the Provision of IBD Services in New Zealand and Identification of Areas for Improvement
A fifty point survey was formulated by a panel of IBD nurses and gastroenterologists (Appendix Table 2). The survey questions followed selected principles, relevant to our study, set out in the Australian IBD Standards 2016,4 themselves having been adapted from the UK Standards.5 These standards of care support six overriding principles, the delivery of high-quality clinical care, local delivery of care, maintaining a patient-centred service, patient education and support, data, information technology and audit and evidence-based practice and research.
Our survey focused only on the outpatient management of IBD patients and was divided into four sections: service organisation, accessibility for patients and health-care professionals, local practice for disease and therapy monitoring, and management of infusion medicines. All 21 District Health Boards (DHBs), comprising 22 services, were invited to participate in an online survey. The survey invitation was addressed to the services’ IBD nurse, but, where there was no IBD nurse employed or if they were unable to complete the survey other clinicians were invited to reply on their behalf.
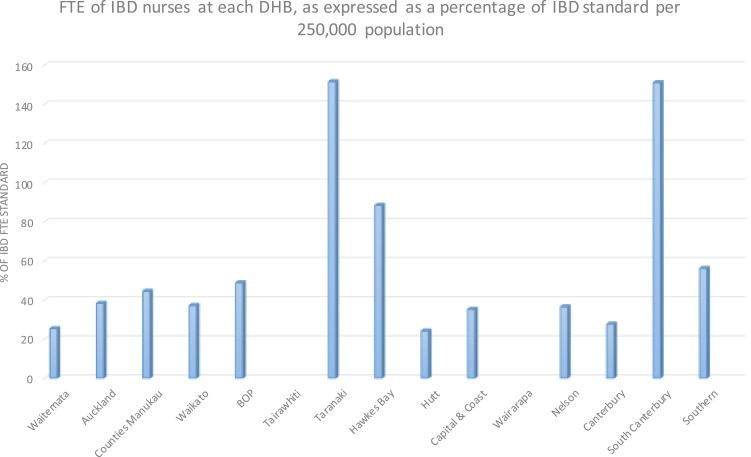
The data were collated and compared to the 2016 Australian IBD standards of care. These standards advise a minimum 1.5 FTE clinical nurse specialist with competency in IBD per 250,000 population. Utilising figures from the 2013 New Zealand census10 the IBD nurse FTE per population was calculated as a percentage of the 2016 Australian standard.
Phase 3 (2017-2019): Audit of Key Aspects of IBD Patient Care, Recorded During Nurse-Led and Doctor-Led Scheduled Outpatient Clinics
Quality and Key performance indicators are used to assess the structure, process and outcomes of clinical care.3,11 A retrospective study, conducted March 2017 to January 2019, captured key auditable quality and performance indicators pertaining to IBD care from 50 consecutive scheduled gastroenterology outpatient visits at each of 14 participating DHB sites (Appendix Table 3).
Using published performance measures12–15 we selected the indicators of recording of weight,12,14 smoking status14,15 and cessation advice12,15 and ensuring delivery of appropriately timed surveillance colonoscopy.12,15
Patient data were anonymised at site and reported only in an aggregated way so that no individual patient could be identified from the data.
Pearson’s Chi-Squared test was used to compare the proportions of doctors and nurses documenting each outcome in order to assess whether there were significant differences in the standards of care between the two groups.
As this audit did not involve the collection of any patient information, but rather the measurement of systematic factors in IBD care and auditable outcomes achieved by health-care teams, it was deemed exempt from ethics review as per the Health and Disability Ethics Committee Standard Operating Procedure. https://ethics.health.govt.nz/operating-procedures. Health professionals participating in the study, including in the collection and return of survey data, provided informed consent by return email following the initial request to participate.
Results
Phase 1 (2015): Evaluation of the Current Role and Practices of Self-Identifying IBD Nurses
A total of twenty participation invitations were sent out, of which fifteen were returned (75%). The median duration spent in an IBD nursing role was 21 months (range 2–120) months with the majority of nurses (12/15) performing two or more nursing roles. Other roles included endoscopy nursing (8/15), clinical nurse manager (2/15), rheumatology specialist nursing (2/15), outpatient gastroenterology nursing (1/15) and research (1/15).
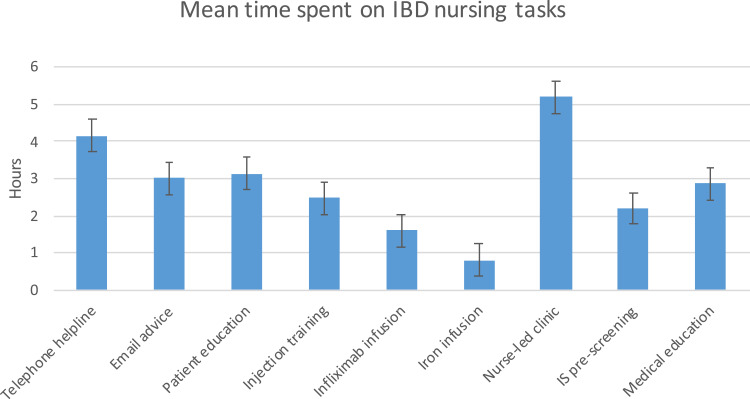
The mean number of hours per week rostered to IBD specific nursing tasks was 15.4 hours, median (IQR) 16 (8–20) hours. The greatest number of hours were spent on telephone and email advice (combined mean 7.1 hours), followed by patient education and injection training (combined mean 5.5 hours) and nurse led clinic (mean 5.2 hours) (Figure 1). Whilst we did not request nurses to document exactly what they discuss during telephone and email patient correspondence the majority of these interactions involve the evaluation and management of patients with deterioration of their IBD symptoms. When time spent administering infusions, immune suppression pre-screening and continued medical education were factored in, the average number of hours spent undertaking IBD nursing tasks was 22.2 hours – a 6.8-hour shortfall compared to rostered hours.
Figure 1.
Mean time spent on IBD nursing tasks (hours spent: error bars show 95% CI).
All IBD nurses participated in continuing professional development, most commonly delivered through pharmaceutical company arranged activities (15/15), New Zealand Society of Gastroenterology (NZSG) Annual Scientific Meeting (14/15), or local Multidisciplinary team meetings (10/15).
The most commonly utilised patient information sources were Crohn's and Colitis NZ (15/15) and pharmaceutical company literature (12/15). Only 9/15 utilised locally developed patient resources.
Immune suppression (IS) pre-screening was most often a collaborative effort between the Gastroenterology consultant and the IBD nurse (13/15) with only one respondent having sole responsibility for IS pre-screening.
The majority of iron and infliximab infusions were given in medical day stay units (11/15), three in endoscopy units and one in the oncology unit.
The development of a formal training and education program and a job framework were the comments most frequently expressed in relation to the development of IBD nursing in NZ.
Phase 2: Evaluation of the Provision of IBD Nursing Services in NZ and Identifying Areas for Improvement
All of the 21 DHBs in NZ, comprising 22 IBD services, were invited to participate in the online survey. Sixteen of the 22 services (73%) responded during the 12-month period of data collection. The respondents comprised ten IBD Nurses, two Gastrointestinal clinical nurse specialists (CNS), one inflammatory autoimmune disease CNS, one outpatients registered nurse, one registrar and one consultant physician.
High-Quality Clinical Care
Only three of the responding services, Waitemata DHB, South Canterbury DHB and Taranaki DHB had access to a full complement IBD team (gastroenterologist, consultant colorectal surgeon, clinical nurse specialist with competency in IBD, stoma therapist and dietitian allocated to gastroenterology). Furthermore, only one of the responding services were able to provide specific information regarding the FTE dedicated to the IBD service for all core members of the IBD team.
The FTE of the IBD specialist nurse at each DHB, calculated as a percentage of that advised in the 2016 Australian standard per 250,000 head population, is shown below (Figure 2).
Figure 2.
FTE of the IBD specialist nurse at each DHB, expressed as a percentage of that proposed in the 2016 Australian standard per 250,000 head population.
Thirteen services gave details of the IBD Nurse FTE, with a mean IBD Nurse FTE across all services of 0.74, median FTE 0.8 (range 0.2 to 1.25). Two-thirds of IBD nurses reported the role was uncovered when they were on leave. Based on population size, and as percentage of the FTE advised in the 2016 Australian standard, only two services met the IBD nurse FTE standard. These were the two smallest DHBs by population size – South Canterbury DHB (151% of standard) and Taranaki DHB (151%). The major centres faired worst, with the two largest DHBs by population size Waitemata DHB and Canterbury DHB having only 25.3% and 27.6% of the advised standard for IBD nurse FTE, respectively.
Just under two-thirds (62.5%) of departments held a regular MDT meeting; a gastroenterologist and nurse attended in all, followed by a surgeon (60%), gastroenterology registrar (60%), radiologist (30%); ward charge nurse, pathologist and dietician (all 20%). Of services responding to the question of frequency of MDT meetings, six departments held their meetings weekly, three monthly and one did not state the interval.
Local Delivery of Care
In the event of a deterioration in their IBD symptoms, all but three services (81%) advised the patients to make direct contact with the IBD nurse. The remaining three services (19%) advised patients to contact their General Practitioner (GP) or the Emergency Department (ED) first. Only 19% of IBD nurses had access to a local standardised care plan regarding how to manage unwell IBD patients.
Eleven IBD nurses were involved in health monitoring for patients in areas such as dysplasia surveillance, renal surveillance for 5-aminosalicylic acid, immunosuppression monitoring, or bone health. One did not answer.
Maintaining a Patient-Centred Service
All sixteen responding services could be contacted directly by IBD patients and believed their service could respond to patient’s concerns or questions within 48 hours of contact. All but three of the respondents had a method for new patients to make direct contact with the service. A dedicated IBD phone line or email was utilised by 81% of services. Written information could be provided regarding the IBD services with 75% using business cards and 25% using a locally created patient information sheet.
Patient Education and Support
Written information regarding IBD, accessible to patients, was available at 94% of responding services.
Patient information sheets for immune suppression medications were produced locally by 38% of services, with 6% of services-producing information sheets regarding dysplasia. Written information in languages other than English was available at only 6% of services with 25% of services having no locally produced written patient information. Thirty-one percent of respondents did not answer questions regarding availability of written patient information.
In regards to patient support services, 88% of services supplied patients with contact details for Crohn's and Colitis NZ. Patients wishing to discuss concerns about their IBD could be offered access to an IBD nurse at 88% of services with the same proportion of services providing patients with repeat clinic visits. Patients could access self-management strategies at three of the sixteen services.
Smoking status was routinely recorded at fifteen of the sixteen services with the remaining service not returning an answer. Formal training for the provision of smoking cessation and access to cessation tools was available at eleven services. Two services had access to cessation tools only and two had no access to training or tools.
Phase 3: Audit of Key Aspects of IBD Patient Care, Recorded During Nurse-Led and Doctor-Led Scheduled Outpatient Clinics, to Determine Whether There Was a Difference in the Quality of Care Provided
Fourteen DHB sites participated with 710 audit forms completed in total (Hutt Valley (50), Wellington (50), Canterbury (50), Southern (50), Hawkes Bay (49), Auckland (50), Taranaki (51), Midcentral (50), Wairarapa (50), Waitemata (50), Waikato (52), South Canterbury (50), Southland (50), Counties Manukau (58)). Twenty-two were discarded because the patient saw doctor and nurse together (n=21) or patient did not attend (n=1).
Six hundred and eighty-eight scheduled outpatient clinic visits included: 492 were doctor-led (Consultant (393), Registrar (88), Fellow (9), House Surgeon (2)) and 196 nurse-led. 58.7%, of patients, were diagnosed with Crohn’s disease, 2.8% Indeterminate colitis and 38.5% Ulcerative Colitis.
Both Doctors and nurses performed well against the care standards. However, nurses were significantly more likely to document weight, document smoking status and organise appropriate colonoscopic surveillance (as per current guidelines) than doctors (Table 1).
Table 1.
Documentation of Key Auditable Outcomes of IBD Patient Care, Recorded During Nurse-Led and Doctor-Led Scheduled Outpatient Clinics
| Key Auditable Outcome | N | % of Visits | P-value | |
|---|---|---|---|---|
| Doctor Led | Nurse Led | |||
| Weight documented | 686 | 77 | 95 | <0.0001* |
| Smoking status documented | 687 | 64 | 73.8 | 0.014* |
| Smoking cessation advice offered | 87 | 69 | 86 | 0.081 |
| Surveillance colonoscopy arranged | 379 | 66.2 | 79.6 | 0.009* |
Note: *Statistically significant <0.05.
Discussion
Phase 1
All nurses in NZ belong to the NZ Nurses Organisation, itself consisting of separate colleges, one of which is dedicated to Gastroenterology. From this College nurses specialising in IBD were identified. As the NZ gastroenterology nursing community is small, we believe we identified all nurses who specialise in IBD care.
This study highlights the relative youth and evolution of the IBD nursing role in NZ with the longest duration in role 10 years but a median (IQR) duration in role of only 21 (11–36) months. We found that the IBD nurse role was often not a dedicated position but undertaken alongside other nursing roles, most commonly endoscopy nursing. A median (IQR) roster of 16 (8–20) hours per week appeared insufficient in order to complete IBD specific tasks with on average further 6.8 hours required to complete these tasks. As a proportion of hours in role, the greatest number were spent in direct patient contact – in clinic, providing advice by telephone or email and in patient education and injection training. The deficit in hours required to complete IBD specific tasks may reflect an under provision of IBD nurses in relation to IBD specific workload, the complexity of management of IBD patients or that the IBD nursing staff are under supported in their roles.
All IBD nurses participated in continuing professional development (CPD) with on average 2.8 hours per week spent in medical education. However, there was a reliance on Pharmaceutical company arranged activities to provide a significant proportion of CPD. Crohn's and Colitis NZ were the most commonly utilised patient information resource, followed by pharmaceutical company literature with only 60% of respondents having access to locally developed resources.
Whilst this study was not designed to assess the influence of pharmaceutical company arranged educational activities on the care dispensed by IBD nurses, it does highlight the utilisation of pharmaceutical company produced literature and educational resources by both IBD nurses and patients.
Those already in role seemed motivated to develop IBD specialist nursing in NZ and were awaiting the development of formal training, educational programmes and job frameworks.
Following the first phase of the study, the NZ IBD nurse working group have developed a knowledge and skills framework.16 This outlines the core competencies required for IBD nursing and develops a roadmap for the development of a modular training system for IBD nurses in NZ.
Commencing 2021 NZ IBD nurses plan to utilise the Gastroenterological Nurses college of Australia (GENCA) online education modules17 and assessments in order to gain these competencies.
Phase 2
A complete picture of the standards of care being delivered across NZ was compromised by a 75% response rate to the survey along with frequent gaps in data collection, particularly in regards to FTE of IBD team members. This 75% response rate was identical to that of the first UK IBD survey in 2006.18 The majority of respondents to our survey were nursing staff (88%).
Although appearing to demonstrate an alarming absence of members of the IBD team at the majority of DHBs, this likely reflects the specificity of our survey questions – namely what FTE was dedicated solely to the IBD service. However, notwithstanding this statement, none of the participating IBD services meet the international standards for the FTE of members of IBD MDT based on population size.
The difficulties in obtaining FTE figures may reflect that few services operate IBD specific clinics, with most IBD patients being reviewed during general gastroenterology outpatient clinics. Specialist IBD clinics, utilising an MDT approach, are evolving as the preferred model for delivery of IBD care in Europe19–21 having demonstrated cost and clinical efficacy19,22 in long-term patient follow up. Inpatient admissions account for the greatest proportion of IBD related health-care costs.23 Ensuring provision of efficient, effective and accessible outpatient services can help to prevent admissions by aiding maintenance of remission and recognising and intervening early in disease flares.
Only 62% of services held MDT meetings with 60% of these meetings taking place weekly and the majority comprising a Gastroenterologist and IBD nurse only. Fourteen of the sixteen services had access to an IBD nurse, with a mean FTE of 0.74. As demonstrated in the first phase, and supported in this second phase of our study, IBD nurses provide important roles in regards to access, education and support for IBD patients. The majority of IBD nurses are also actively involved in disease and therapeutic drug monitoring. IBD nurses have been demonstrated to enhance patients’ understanding of their disease and its management, and reduce admissions and emergency department visits.7–9 They are therefore an integral part of the IBD service.
The paucity of clinical pathways for GPs – only three services had a clinical pathway for GPs to follow with concerns regarding IBD patients – and local care plans for unwell IBD patients indicates areas for standard improvement. All IBD services could be contacted by patients with the majority (81%) actively encouraging patients with a flare of their IBD to do so, thereby circumventing delays associated any requirement to attend their GP or ED first.
IBD services in NZ are accessible to patients and all reported that they could respond to queries or concerns within 48 hours. Most services had dedicated IBD telephone or email methods for contact and written information for patients documenting these methods.
Clear areas for improvement were identified in the creation and provision of written format patient information relating to IBD and related investigations, complications and therapeutics. As per the first phase of our study, the majority of patient information sources rely on Crohn's and Colitis NZ, and Pharmaceutical company literature. It was also demonstrated that only 6% of departments had access to information in a language other than English.
Investigation of data, information technology and audit and evidence-based practice and research were not collected in this audit.
Phase 3
Standards of Care and Guidelines provide a framework to create the structures and processes to manage IBD patients. Quality indicators are used to assess the structure and process while Key Performance Indicators (KPIs) assess the outcomes of the structures and processes created, ie, what happens to the patients as a result of the care received.
A 2015 retrospective study compared monitoring of IBD patients on thiopurine therapy in physician- and nurse-led outpatient clinics. This study concluded nurse-led clinics reduced the requirement for physician-led follow-up, and missed thiopurine surveillance blood tests, without differences in leukopenic episodes or complications.24
Our study supports this finding, with IBD nurses in NZ providing high-quality outpatient care when measured against the auditable standards of documentation of weight, smoking status and arrangement of surveillance colonoscopy. Whilst our study does not allow us to determine why nurses might be more likely to document important outcomes, it would seem to be a function of training and perhaps the way the work environment is designed.
Final Conclusions
This first national audit highlights both positive and negative aspects in the standards of IBD care across NZ. We identified that IBD nurses, key members of the IBD MDT, are already working in Gastroenterology departments and providing good quality patient care. Their number and FTE dedicated to IBD, along with other members of the IBD MDT, were however insufficient to meet international recommendations regarding appropriate FTE based upon population size.
Whilst a skills and development framework has been developed since this study was commenced, with a more structured and independent education programme17 due to commence in 2021, the evolution of the IBD Nursing role will require ongoing support at both a DHB and national level. With the high prevalence of IBD in NZ relative to other countries expected to continue to increase, demand on IBD services is expected to grow. Increased recognition of this subspecialty role is vital in order to attract nurses of sufficient number and quality, whilst an increase in funding and capacity for training will be required in order to continue producing high-quality IBD nurses.
Assessing outcomes of IBD care in NZ will require identifying and adopting quality indicators appropriate to New Zealand’s resources as well as the development of NZ specific KPIs. A more robust, compulsory, audit of IBD standards of care across all DHBs against established international standards is currently in development.
Acknowledgments
We thank the Gastroenterology Departments of Waitemata, Auckland, Counties Manukau, Waikato, Bay of Plenty, Tairawhiti, Taranaki, Hawkes Bay, Hutt, Capital and Coast, Wairarapa, Nelson, Canterbury, South Canterbury and Southern District Health Boards for their participation in the surveys.
Funding Statement
This project was supported by an unconditional research grant from AbbVie Limited.
Disclosure
Dr Robert Hackett reports grants from AbbVie Limited, during the conduct of the study. Professor Richard Gearry reports grants, personal fees from Abbvie, grants, personal fees from Zespri, outside the submitted work. The authors have no other conflicts of interest to declare.
References
- 1.Kahui S, Snively S, Ternent M. Reducing the growing burden of Inflammatory Bowel Disease in New Zealand. Crohns and Colitis NZ; 2017. Available from: https://issuu.com/crohnsandcolitisnz/docs/271017_master_formatted_bod_report_. Accessed August3, 2020.
- 2.Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;(1):4. [PMC free article] [PubMed] [Google Scholar]
- 3.Fiorino G, Allocca M, Chaparro M, et al. ‘Quality of care’ standards in inflammatory bowel disease: a systematic review. J Crohns Colitis. 2019;13(1):127–137. doi: 10.1093/ecco-jcc/jjy140 [DOI] [PubMed] [Google Scholar]
- 4.Pavli P, Andrews J et al. Australian IBD Standards 2016: standards of healthcare for people with inflammatory bowel disease in Australia. Crohns and Colitis Australia. Available from: https://www.crohnsandcolitis.com.au/site/wp-content/uploads/IBD-Standards-Final.pdf. Accessed August3, 2020.
- 5.IBD Standards Group. Standards for the Healthcare of People who have Inflammatory Bowel Disease. 2013. Available from: http://s3-eu-west-1.amazonaws.com/files.crohnsandcolitis.org.uk/Publications/PPR/ibd-standards.pdf. Accessed August3, 2020.
- 6.Nguyen GC, Devlin SM, Afif W, et al. Defining quality indicators for best-practice management of inflammatory bowel disease in Canada. Can J Gastroenterol Hepatol. 2014;28(5):275–285. doi: 10.1155/2014/941245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sack C, Phan VA, Grafton R, et al. A chronic care model significantly decreases costs and healthcare utilisation in patients with inflammatory bowel disease. J Crohns Colitis. 2012;6(3):302–310. doi: 10.1016/j.crohns.2011.08.019 [DOI] [PubMed] [Google Scholar]
- 8.Nightingale. Evaluation of the effectiveness of a specialist nurse in the management of inflammatory bowel disease (IBD). Eur J Gastroenterol Hepatol. 2000;12(9):967–973. doi: 10.1097/00042737-200012090-00001 [DOI] [PubMed] [Google Scholar]
- 9.Leach P, De Silva M, Mountifield R, et al. The effect of an inflammatory bowel disease nurse position on service delivery. J Crohns Colitis. 2014;8(5):370–374. doi: 10.1016/j.crohns.2013.09.018 [DOI] [PubMed] [Google Scholar]
- 10.Available from: http://archive.stats.govt.nz/Census/2013-census/data-tables/dhb-tables.aspx#gsc.tab=0. Accessed August3, 2020.
- 11.Berry SK, Melmed GY. Quality indicators in inflammatory bowel disease. Intest Res. 2018;16(1):43. doi: 10.5217/ir.2018.16.1.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melmed GY, Siegel CA. Quality Improvement in Inflammatory Bowel Disease. Gastroenterol Hepatol. 2013;9(5):286–292. [PMC free article] [PubMed] [Google Scholar]
- 13.Inflammatory bowel disease. International Consortium for Health Outcome Measurement (ICHOM). Available from: https://www.ichom.org/portfolio/inflammatory-bowel-disease/. Accessed August3, 2020.
- 14.Kim AH, Roberts C, Feagan BG, et al. Developing a standard set of patient-centred outcomes for inflammatory bowel disease—an international, cross-disciplinary consensus. J Crohns Colitis. 2018;12(4):408–418. doi: 10.1093/ecco-jcc/jjx161 [DOI] [PubMed] [Google Scholar]
- 15.AGA Bridges to excellence. Available from: http://www.bridgestoexcellence.org/sites/default/files/BTE%20IBD%20Care%20Program%20Guide%20020618.pdf. Accessed August3, 2020.
- 16.Available from: www.nzno.org.nz/Portals/0Files/Documents/Groups/Gastroenterology/2019-New%20Zealand%20KSF%20June%202018%20final-_.pdf. Accessed August3, 2020.
- 17.https://www.genca.org.
- 18.UK IBD Audit Steering Group. UK IBD Audit 2006: national results for the organisation and process of IBD Care in the UK. 2007. Available from: www.rcplondon.ac.uk/projects/ibdauditround1. Accessed August3, 2020.
- 19.Lönnfors S, Vermeire S, Greco M, Hommes D, Bell C, Avedano L. IBD and health-related quality of life — discovering the true impact. J Crohns Colitis. 2014;8(10):1281–1286. doi: 10.1016/j.crohns.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 20.Mikocka-Walus A, Clin P, Holtmann G, Andrews J. An integrated model of care for inflammatory bowel disease sufferers in australia: development and the effects of its implementation. Inflamm Bowel Dis. 2012;18(8):1573–1581. [DOI] [PubMed] [Google Scholar]
- 21.Panés J, O’Connor M, Peyrin-Biroulet L, Irving P, Petersson J, Colombel J-F. Improving quality of care in inflammatory bowel disease: what changes can be made today? J Crohns Colitis. 2014;8(9):919–926. doi: 10.1016/j.crohns.2014.02.022 [DOI] [PubMed] [Google Scholar]
- 22.Mawdsley JED, Irving PM, Makins RJ, Rampton DS. Optimizing quality of outpatient care for patients with inflammatory bowel disease: the importance of specialist clinics. Eur J Gastroenterol Hepatol. 2006;18(3):249–253. doi: 10.1097/00042737-200603000-00004 [DOI] [PubMed] [Google Scholar]
- 23.Odes S, Vardi H, Friger M, et al. Cost analysis and cost determinants in a european inflammatory bowel disease inception cohort with 10 years of follow-up evaluation. Gastroenterology. 2006;131(3):719–728. doi: 10.1053/j.gastro.2006.05.052 [DOI] [PubMed] [Google Scholar]
- 24.López M, Dosal A, Villoria A, Moreno L, Calvet X. A nurse-driven outpatient clinic for thiopurine-treated inflammatory bowel disease patients reduces physician visits and increases follow-up efficiency. Gastroenterol Nurs. 2015;38(2):116–120. doi: 10.1097/SGA.0000000000000103 [DOI] [PubMed] [Google Scholar]