Related article, p. 532
More than 37 million (15%) adults in the United States have chronic kidney disease (CKD).1 CKD often is silent and frequently goes undetected until its advanced stages, even in high-risk subgroups such as adults 60 years and older, those with diabetes, and those with hypertension.1 Racial and ethnic disparities in the prevalence of CKD and progression to end-stage kidney disease (ESKD) persist, with Blacks having more than a 2-fold increase in risk for developing ESKD compared with Whites.1 Although many persons with CKD eventually receive care from nephrologists, many more (especially at early stages of the disease) do not, underscoring the critical role for primary care physicians (PCPs) and other specialties in educating patients about CKD. Critically, ∼90% of people who have CKD are unaware of their condition. Even among those with advanced disease who are not undergoing dialysis, only ∼50% are aware of their CKD.1
In a study in this issue of Kidney Medicine, Barrett et al2 examined how patients with CKD (stages 2-5) prioritize information that they receive from health care providers. Of 453 adults with CKD, they found that approximately half relied on nephrologists primarily for information about kidney disease, whereas almost a quarter relied on PCPs and a fifth relied on both equally. Patients with a longer history of nephrology care and those who perceived their last interactions as patient centered were more likely to rely on nephrologists for health information.
These findings raise 3 important questions: First, for patients with CKD, what information should be communicated earlier in the disease course to prevent progression and by whom? Second, how should care be coordinated to ensure consistency in messaging and patient-centered care? Third, how should we measure patient-centered care? Barrett et al describe extremely high scores on the Patient Perception of Patient Centeredness Scale: median, 3.8 (interquartile range, 3.4-4.0) of a highest possible score of 4. Although it is reassuring to see that patients perceive their nephrology care to be patient centered, the very high responses against a backdrop of limited variation suggests that more sensitive tools for assessing patient-centered care are needed. These issues, along with opportunities for improvement, are addressed next.
What Information Should Be Communicated Earlier in the Disease Course and by Whom?
Lack of consistent patient education for persons with kidney disease is an important and persistent challenge facing the kidney community. Public knowledge of kidney disease is low compared with other conditions, and awareness of CKD among persons with the condition is also extremely low. Using a diverse racial and socioeconomic population in Baltimore City, Tuot et al3 found that only 20% of participants were aware of having CKD (range, 11% for CKD stages 1 and 2 and 29% for CKD stages 3 and 4). Similarly, Chu et al4 found that between 2011 and 2016, CKD awareness ranged from 10% to just 49% among low- and high-risk groups, respectively. Tummalapalli et al5 found that of 6,529 participants with CKD, just 4.4% were aware of their CKD. CKD awareness was associated with 1.44 increased odds of ESKD. These studies and others suggest that CKD awareness, although universally low, is higher among people with more advanced disease, highlighting the need for education at early stages of CKD.5
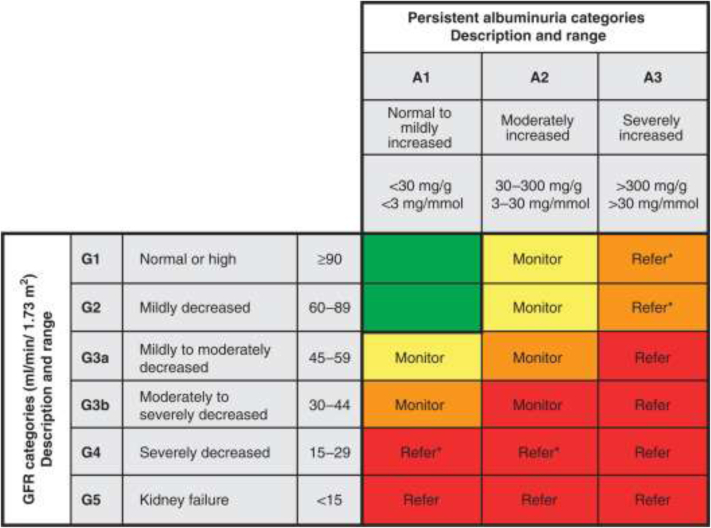
Patient education and CKD awareness are associated with better outcomes, including higher rates of pre-ESKD nephrology care, higher likelihood of permanent access use for dialysis initiation, higher rates of satisfaction with care, preemptive transplant wait listing, and transplantation.6,7 KDIGO (Kidney Disease: Improving Global Outcomes) guidelines provide stage-specific action plans for the continuum of CKD care, emphasizing screening for CKD and its risk factors in the early stages to slow down progression (Fig 1).8 Importantly, their heat map incorporates both estimated glomerular filtration rate (eGFR) and albuminuria to risk stratify patients. Thus a 70-year-old man with a stable eGFR of 40 mL/min with no albuminuria could be monitored by his PCP. However, a 70-year-old man with an eGFR of 65 mL/min and albuminuria with albumin excretion > 300 mg/g should be referred to nephrology given the high risk for rapid progression.
Figure 1.
Nephrology referral decision making by glomerular filtration rate (GFR) and albuminuria. Reproduced from KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease8 with permission of Elsevier.
Despite evidence showing the benefits of early patient education, most kidney education is focused on dialysis initiation and occurs in the late stages of CKD, leaving many patients with poor understanding of their diagnosis, prognosis, and options.9 Educating and engaging patients in the earlier stages of CKD will require a primary care workforce able to identify patients at risk for CKD, stay up to date with CKD guidelines, and detect those at risk to progress quickly to facilitate timely nephrology referral. Through early education, primary care providers can empower patients to slow CKD progression by improving early preventive care, including nutrition and exercise, while reducing injurious behaviors such as use of nephrotoxic medication and tobacco use. Access to mental health services and cognitive screening should be key components of any early CKD education program. Incorporating risk calculators that provide personalized estimates of patients’ risk for CKD progression may also enhance opportunities for early education, shared decision making, timely referral, and follow-up. Web-based decision aids that educate patients about CKD, prognosis, and treatment options also hold promise, especially for patients with limited health literacy and those in rural areas for whom engaging during medical encounters is difficult.10 To support shared decision making, education programs should clarify decision points, provide facts and probabilities, help patients and families clarify values and preferences, guide the deliberation, and engage patients and their caregivers throughout the care continuum.
How Should Care Be Coordinated to Ensure Consistency in Messaging and Patient Centeredness?
Improving patient-centered CKD care requires greater care coordination between PCPs and kidney clinicians. Educating patients with earlier CKD stages often falls to PCPs, who are confronted with numerous competing priorities during brief visits. In addition to limited time, PCPs may face multiple barriers, including difficulty staying current with CKD guidelines, inadequate resources and decision support, and insufficient coordination with social work, nutritionists, and nursing.11 Conversely, nephrologists struggle with delayed referrals, which have been associated with worse health outcomes including death in the first year of dialysis.12 Barrett et al’s findings reinforce the notion that building on trust developed over long-standing physician-patient relationships is critical to successful outreach to patients early in their CKD progression. Smoother transitions, greater emotional support, clarification of roles, increased collaboration, and consistency in messaging are all crucial to improving care for patients.13
Rooted in the Chronic Care Model, improving upstream kidney care is a promising patient-centered approach to more cohesive streamlined care while ensuring consistent messaging for patients. These include integrated care models with multidisciplinary teams that bring together PCPs, nephrologists, nutritionists, social workers, nurses, and pharmacists to improve education and care continuity for patients with complex needs.14 Such models, often combined with disease management strategies such as telephone-based outreach, self-management, and coaching, have been shown to delay the progression of CKD and improve patient engagement and satisfaction.15, 16, 17 Shared medical records, risk calculators, and decision aids all provide opportunities for multidisciplinary collaboration even remotely, an increasingly vital feature during the current coronavirus disease 2019 (COVID-19) pandemic, in which kidney care is often delivered remotely.
How Should We Measure Patient-Centered Care?
With growing commendable efforts to improve patient-centered kidney care, new measures are being developed to assess patient centeredness. One persistent challenge with such measures is the often limited variation in responses and ceiling effects, as demonstrated in the patient-perceived patient-centeredness scale used by Barrett et al. In measuring trust in nephrologists, Oskoui et al18 observed high levels of trust in nephrologists across participants (mean score of 9.1 on a scale from 0-10) in a sample of older patients with advanced CKD, even when pertinent decision-making factors had not been discussed. Response bias, including social desirability bias and recall bias, in addition to sampling bias (participation in research by patients who are generally more satisfied), present real challenges to understanding patient centeredness in kidney care. Researchers and funders should prioritize the development and validation of measures to assess trust, patient centeredness, and satisfaction with kidney care and kidney education. These efforts should include patients, caregivers, clinicians, and other key stakeholders to ensure that measures are both reflective of factors that matter most to patients and their families and also clinically relevant.
Improving patient-centered kidney care requires consensus about the content of early CKD education, integrated care models to ensure consistent and accessible education and follow-up, and more accurate measures to assess patient centeredness. Critically, all 3 components require partnership and collaboration between patients, caregivers, clinicians, payors, and regulatory agencies to achieve meaningful change. As Barrett et al demonstrate, intervening early and collaborating with PCPs is a necessary first step to improving awareness and patient-centered care for persons with kidney disease.
Article Information
Authors’ Full Names and Academic Degrees
Keren Ladin, PhD, MSc, and Ana Rossi, MD, MPH.
Support
Research reported in this work was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (CDR-2017C1-6297).
Financial Disclosure
The authors declare that they have no relevant financial interests.
Disclaimer
The views, statements, and opinions in this publication are solely the responsibility of the authors and do not necessarily represent the views of PCORI, its Board of Governors, or its Methodology Committee.
Peer Review
Received June 30, 2020, in response to an invitation from the journal. Direct editorial input by the Editor-in-Chief. Accepted in revised form July 23, 2020.
References
- 1.Centers for Disease Control and Prevention . US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2019. Chronic Kidney Disease in the United States, 2019. [Google Scholar]
- 2.Barrett T.M., Green J.A., Greer R.C. Advanced CKD care and decision making: which health care professionals do patients rely on for CKD treatment and advice? Kidney Med. 2020;2(5):532–542. doi: 10.1016/j.xkme.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tuot D.S., Wong K.K., Velasquez A. CKD awareness in the general population: performance of CKD-specific questions. Kidney Med. 2019;1(2):43–50. doi: 10.1016/j.xkme.2019.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chu C., McCulloch C., Banerjee T. CKD awareness among US adults by future risk of kidney failure. Am J Kidney Dis. 2020;76(2):174–183. doi: 10.1053/j.ajkd.2020.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tummalapalli S.L., Vittinghoff E., Crews D.C. Chronic kidney disease awareness and longitudinal health outcomes: results from the REasons for Geographic And Racial Differences in Stroke Study. Am J Nephrol. 2020;51(6):463–472. doi: 10.1159/000507774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Narva A.S., Norton J.M., Boulware L.E. Educating patients about CKD: the path to self-management and patient-centered care. Clin J Am Soc Nephrol. 2016;11(4):694–703. doi: 10.2215/CJN.07680715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurella Tamura M., Li S., Chen S.C. Educational programs improve the preparation for dialysis and survival of patients with chronic kidney disease. Kidney Int. 2014;85(3):686–692. doi: 10.1038/ki.2013.369. [DOI] [PubMed] [Google Scholar]
- 8.Kidney Disease: Improving Global outcomes (KDIGO) CKD work group KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. [Google Scholar]
- 9.Ladin K., Lin N., Hahn E., Zhang G., Koch-Weser S., Weiner D.E. Engagement in decision-making and patient satisfaction: a qualitative study of older patients’ perceptions of dialysis initiation and modality decisions. Nephrol Dial Transplant. 2017;32(8):1394–1401. doi: 10.1093/ndt/gfw307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green J.A., Boulware L.E. Patient education and support during CKD transitions: when the possible becomes probable. Adv Chronic Kidney Dis. 2016;23(4):231–239. doi: 10.1053/j.ackd.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Sperati C.J., Soman S., Agrawal V. Primary care physicians’ perceptions of barriers and facilitators to management of chronic kidney disease: a mixed methods study. PLoS One. 2019;14(8) doi: 10.1371/journal.pone.0221325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Avorn J., Bohn R.L., Levy E. Nephrologist care and mortality in patients with chronic renal insufficiency. Arch Intern Med. 2002;162(17):2002–2006. doi: 10.1001/archinte.162.17.2002. [DOI] [PubMed] [Google Scholar]
- 13.Greer R.C., Ameling J.M., Cavanaugh K.L. Specialist and primary care physicians’ views on barriers to adequate preparation of patients for renal replacement therapy: a qualitative study. BMC Nephrol. 2015;16:37. doi: 10.1186/s12882-015-0020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayliss E.A., Bhardwaja B., Ross C., Beck A., Lanese D.M. Multidisciplinary team care may slow the rate of decline in renal function. Clin J Am Soc Nephrol. 2011;6(4):704–710. doi: 10.2215/CJN.06610810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Humalda J.K., Klaassen G., de Vries H. A self-management approach for dietary sodium restriction in patients with CKD: a randomized controlled trial. Am J Kidney Dis. 2020;75(6):847–856. doi: 10.1053/j.ajkd.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 16.Richards N., Harris K., Whitfield M. Primary care-based disease management of chronic kidney disease (CKD), based on estimated glomerular filtration rate (eGFR) reporting, improves patient outcomes. Nephrol Dial Transplant. 2008;23(2):549–555. doi: 10.1093/ndt/gfm857. [DOI] [PubMed] [Google Scholar]
- 17.Levin A. The need for optimal and coordinated management of CKD. Kidney Int Suppl. 2005;99:S7–S10. doi: 10.1111/j.1523-1755.2005.09902.x. [DOI] [PubMed] [Google Scholar]
- 18.Oskoui T., Pandya R., Weiner D., Wong J., Koch-Weser S., Ladin K. Advance care planning among older adults with advanced non–dialysis-dependent CKD and their care partners: perceptions versus reality? Kidney Med. 2020;2(2):116–124. doi: 10.1016/j.xkme.2019.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]