ABSTRACT
As per current guidelines, whenever an advanced airway is in place during cardiopulmonary resuscitation, positive pressure ventilation should be provided without pausing for chest compression. Positive pressure ventilation can be provided through bag-valve resuscitator (BV) or mechanical ventilator (MV), which was found to be equally efficacious. In a busy emergency department, with less trained personnel use of MV is advantageous over BV in terms of reducing human errors and relieving the airway manager to focus on other resuscitation tasks. Currently, there are no guidelines specific to MV settings in cardiac arrest. We present a concept of “six-dial ventilator strategy during CPR” that encompasses the evidence-based settings appropriate during chest compression. We suggest use of volume control ventilation with the following settings: (1) positive end-expiratory pressure of 0 cm of water (to allow venous return), (2) tidal volume of 8 mL/kg with fraction of inspired oxygen at 100% (for adequate oxygenation), (3) respiratory rate of 10 per minute (for adequate ventilation), (4) maximum peak inspiratory pressure or Pmax alarm of 60 cm of water (to allow tidal volume delivery during chest compression), (5) switching OFF trigger (to avoid trigger by chest recoil), and (6) inspiratory to expiratory time ratio of 1:5 (to provide adequate inspiratory time of 1 second).
How to cite this article: Sahu AK, Timilsina G, Mathew R, Jamshed N, Aggarwal P. “Six-dial Strategy”—Mechanical Ventilation during Cardiopulmonary Resuscitation. Indian J Crit Care Med 2020;24(6):487–489.
Keywords: Cardiac arrest, Mechanical ventilation, Ventilation strategy
Dear editor
In cardiac arrest, restoring circulation with chest compressions and, if appropriate, attempted defibrillation are the priority to restart the heart. The current guidelines recommend that the attempt to secure the airway may be deferred until the patient fails to respond to initial cardiopulmonary resuscitation and defibrillation attempts or demonstrates return of spontaneous circulation (ROSC).1,2 Moreover, there is inadequate evidence to define the optimal timing of advanced airway placement in relation to other interventions during resuscitation from cardiac arrest.2 But in cases where cardiopulmonary resuscitation (CPR) is prolonged for more than few minutes, or hypoxia is the cause of arrest, it is necessary to ensure adequate oxygen delivery to the tissues. Hence, management of airway and ventilation during CPR are important pillars for successful resuscitation. It includes basic airway management such as bag-mask ventilation and advanced airway management such as supraglottic airways and endotracheal intubation.1,2 Whenever an advanced airway is inserted during CPR, continuous compressions with positive-pressure ventilation (PPV) should be delivered without pausing chest compressions.2–4
Positive-pressure ventilation can be provided through an advanced airway by bag-valve resuscitator (BV) or mechanical ventilator (MV). Both methods of ventilation were found to be equally effective in terms of blood gas measurements in a prospective interventional study of 122 cardiac arrest patients.5 In high-volume emergency departments (ED) with a smaller number of trained personnel, use of MV offers advantage over BV. It allows the airway manager to focus on other tasks during CPR such as chest compression, defibrillation, searching the cause of cardiac arrest, and so on.6 Weiss et al. had showed that healthcare professionals were able to accomplish more tasks, document more completely, and provide better patient care with the use of the MV in patients undergoing CPR with an advanced airway compared to that of BV.6 It also eliminates human error by providing a set ventilation parameters.7
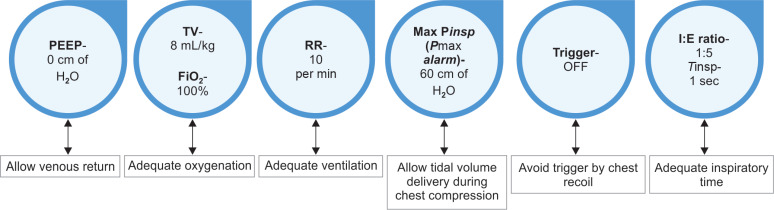
Currently, there are no evidence-based guidelines regarding the appropriate MV strategy in CPR.2 In the following section, we present a concept of “Six-dial” MV strategy during CPR, which we use frequently in our ED. “Six-dial” strategy encompasses the MV settings apt for CPR, which is in accordance with the current available evidences and guidelines (Fig. 1). Moreover, this strategy can be easily adopted in patients with IHCA who are already on MV.
Fig. 1.
Mechanical ventilator strategy in cardiopulmonary resuscitation. PEEP, positive end-expiratory pressure; TV, tidal volume; FiO2, fraction of inspired oxygen; Pmax, maximum peak inspiratory pressure alarm; I:E ratio, inspiratory to expiratory ratio; Tinsp, inspiratory time
MODE—VOLUME CONTROL VENTILATION (VCV MODE)
Dial—1: Positive End-expiratory Pressure = 0 cm of Water
Positive end-expiratory pressure (PEEP) improves oxygenation by recruitment of collapsed alveolar spaces, thus reducing intrapulmonary shunting.8 However, an increase in alveolar volume is associated with higher intrathoracic pressures and impairment of venous return during CPR in animals.9,10 The effect of PEEP during PPV in patients undergoing CPR is unknown. In a single-centered, nonrandomized study of 298 hospital cardiac arrest patients, those ventilated with 5 cm H2O PEEP had significantly higher ROSC compared to patients without PEEP (48.2% vs 22.2%, p value < 0.001). But this result lacked a multivariate analysis of other covariates influencing ROSC.11 Therefore, we suggest a zero PEEP during CPR so that it will not impede the venous return in chest recoil phase of CPR, although more evidence from human studies are needed to support this.
Dial—2: Tidal Volume = 8 mL/kg and Fraction of Inspired Oxygen = 100%
The current guidelines recommend a tidal volume of approximately 600 mL for adults for ventilation during cardiac arrest.1,2 Hence, it is suggested that a tidal volume of 8 mL/kg should be provided so as to minimize the CPR-induced ventilation–perfusion mismatch.12
Only 1 observational study of 145 of hospital cardiac arrest patients evaluated arterial oxygen saturation (PaO2) measured during CPR and cardiac arrest outcomes. The higher ranges of partial pressure of oxygen in arterial blood during CPR were associated with an increase in hospital admission rates.13 Therefore, it is recommended to use highest available fraction of inspired oxygen (in MV = 100%).1,2
Dial—3: Respiratory Rate = 10 per Minute
Hyperventilation during CPR can increase the mean intrathoracic pressure reducing venous return to the heart, increase lung volume and pulmonary vascular resistance, reduce cardiac output, and decrease coronary perfusion pressure and aortic blood pressure.14,15 But hyperventilation is very common during CPR.14 A reduced ventilation rate could be sufficient to maintain a normal ventilation to perfusion ratio during CPR, as the cardiac output generated by chest compressions is only 10–15% of normal.16 Based on these studies, a systematic review recommended a ventilation rate of 10 per minute during adult CPR with a tracheal tube (very weak recommendation based on very low-quality evidence).17
Dial—4: Maximum Peak Inspiratory Pressure (Pmax Alarm) = 60 cm of Water
During CPR with advanced airway in place, ventilation is provided asynchronous to chest compression.1 Often, it will happen that inspiratory breath of MV may coincide with compression phase of CPR. Compression phase of CPR increases the intrathoracic pressure, which may rise above the set peak inspiratory pressure (Pmax; which is usually set at 35–45 cm of water), limiting the MV to provide inspiratory breath. Hence, it is advisable to increase the Pmax alarm to 60 cm of water.7 Increasing the Pmax should caution the provider about risk of barotrauma; hence, titration of Pmax should be done on individual patient basis.18 Maximum allowable Pmax is 80 cm of water.7
Dial—5: Ventilator Trigger = OFF
The trigger sensitivity should allow the patient to trigger the ventilator easily. A trigger sensitivity that is too sensitive may cause a breath to be delivered in response to chest recoil, which may lead to induce hyperventilation and deteriorating gas exchange during CPR. A porcine study showed that there were significantly lower minute ventilation volume and mean airway pressure and higher aortic blood pressure, coronary perfusion pressure, and end-tidal carbon dioxide observed in the ventilation periods with a turned-off triggering setting compared to those with pressure or flow-triggering (p value < 0.05).19 Hence, a turned-off patient triggering is suggested for MV during CPR. If the option of stopping the trigger is not available in the ventilator, pressure trigger of −20 cm of water should be used.19
Dial—6: Adequate Inspiratory Time = 1 Second
Per current recommendations, delivering each breath by bag-valve should be of 1 second duration.1,2 As the respiratory rate is set at 10 per minute, to comply with the recommendations, inspiratory to expiratory time (I:E) ratio should be 1:5 or fraction of inspiration duration from total breath duration should be 16 to 17%.
LIMITATIONS of “SIX-DIAL” STRATEGY
Although MV has some advantage over BV, it is important to keep in mind about the complications associated with MV such as barotrauma. Lack of adequate mechanical ventilators in ED, lack of expertise to use it, and unavailability of robust human studies are hinderances to use the proposed “Six-dial strategy.”
Once ROSC is achieved, it is imperative to change the ventilatory settings from “Six-dial” to post-ROSC ventilation strategy. The current guidelines for post-ROSC care recommend using low tidal volume ventilation (6–8 mL/kg ideal body weight) with titrated levels of PEEP and aiming for normocapnia.1,20 Other parameters such as trigger, Pmax alarm, and I:E ratio should be reverted to default setting and adjusted according to patient’s requirements.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Olasveengen TM, de Caen AR, Mancini ME, Maconochie IK, Aickin R, Atkins DL, et al. 2017 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations summary. Resuscitation. 2017;;121::201––214.. doi: 10.1016/j.resuscitation.2017.10.021. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Link Mark S, Berkow Lauren C, Kudenchuk Peter J, Halperin Henry R, Hess Erik P, Moitra Vivek K, et al. Part 7: adult dvanced cardiovascular life support. Circulation. 2015;;132::S444––S464.. doi: 10.1161/CIR.0000000000000261. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Perkins GD, Olasveengen TM, Maconochie I, Soar J, Wyllie J, Greif R, et al. European resuscitation council guidelines for resuscitation: 2017 update. Resuscitation. 2018;;123::43––50.. doi: 10.1016/j.resuscitation.2017.12.007. DOI: [DOI] [PubMed] [Google Scholar]
- 4.Kleinman Monica E, Brennan Erin E, Goldberger Zachary D, Swor Robert A, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality. Circulation. 2015;;132((18 Suppl 2):):S414––S435.. doi: 10.1161/CIR.0000000000000259. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Johannigman JA, Branson RD, Johnson DJ, Davis K, Hurst JM. Out-of-hospital ventilation: bag-valve device vs. Transport ventilator. Acad Emerg Med. 1995;;2((8):):719––724.. doi: 10.1111/j.1553-2712.1995.tb03624.x. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Weiss SJ, Ernst AA, Jones R, Ong M, Filbrun T, Augustin C, et al. Automatic transport ventilator vs bag valve in the EMS setting: a prospective, Randomized trial. South Med J. 2005;;98((10):):970––976.. doi: 10.1097/01.smj.0000182177.01436.70. DOI: [DOI] [PubMed] [Google Scholar]
- 7.Gabrielli A, Layon AJ, Idris AH. Ornato JP, Peberdy MA. Cardiopulmonary Resuscitation. Totowa, NJ:: Humana Press;; 2005.. Physiology of ventilation during cardiac arrest. pp. pp. 39––94.. DOI: [DOI] [Google Scholar]
- 8.Guo L, Xie J, Huang Y, Pan C, Yang Y, Qiu H, et al. Higher PEEP improves outcomes in ARDS patients with clinically objective Positive oxygenation response to PEEP: a systematic review and meta-analysis. BMC Anesthesiol. 2018;;18((1):):172.. doi: 10.1186/s12871-018-0631-4. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hevesi ZG, Thrush DN, Downs JB, Smith RA. Cardiopulmonary resuscitation: effect of CPAP on gas exchange during chest compressions. Anesthesiology. 1999;;90((4):):1078––1083.. doi: 10.1097/00000542-199904000-00022. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Ido Y, Goto H, Lavin MJ, Robinson JD, Mangold JV, Arakawa K. Effects of Positive end-expiratory pressure on carotid blood flow during closed-chest cardiopulmonary resuscitation in dogs. Anesth Analg. 1982;;61((7):):557––560.. doi: 10.1213/00000539-198207000-00002. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Duchatelet C, Wolfskeil M, Vanwulpen M, Idrissi S-H. Effect of positive end-expiratory pressure during cardiopulmonary resuscitation on short-term survival. Resuscitation. 2019;;142::e7––e8.. doi: 10.1016/j.resuscitation.2019.06.029. DOI: [DOI] [Google Scholar]
- 12.Lurie KG, Nemergut EC, Yannopoulos D, Sweeney M. The physiology of cardiopulmonary resuscitation. Anesth Analg. 2016;;122((3):):767––783.. doi: 10.1213/ANE.0000000000000926. DOI: [DOI] [PubMed] [Google Scholar]
- 13.Spindelboeck W, Schindler O, Moser A, Hausler F, Wallner S, Strasser C, et al. Increasing arterial oxygen partial pressure during cardiopulmonary resuscitation is associated with improved rates of hospital admission. Resuscitation. 2013;;84((6):):770––775.. doi: 10.1016/j.resuscitation.2013.01.012. DOI: [DOI] [PubMed] [Google Scholar]
- 14.Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;;32((9 Suppl):):S345––S351.. doi: 10.1097/01.CCM.0000134335.46859.09. DOI: [DOI] [PubMed] [Google Scholar]
- 15.Yannopoulos D, Sigurdsson G, McKnite S, Benditt D, Lurie KG. Reducing ventilation frequency combined with an inspiratory impedance device improves CPR efficiency in swine model of cardiac arrest. Resuscitation. 2004;;61((1):):75––82.. doi: 10.1016/j.resuscitation.2003.12.006. DOI: [DOI] [PubMed] [Google Scholar]
- 16.Samson RA, Berg MD, Berg RA. Cardiopulmonary resuscitation algorithms, defibrillation and optimized ventilation during resuscitation. Curr Opin Anaesthesiol. 2006;;19((2):):146––156.. doi: 10.1097/01.aco.0000192799.87548.d3. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Vissers G, Soar J, Monsieurs KG. Ventilation rate in adults with a tracheal tube during cardiopulmonary resuscitation: a systematic review. Resuscitation. 2017;;119::5––12.. doi: 10.1016/j.resuscitation.2017.07.018. DOI: [DOI] [PubMed] [Google Scholar]
- 18.Ioannidis G, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, Lampaki S, et al. Barotrauma and pneumothorax. J Thorac Dis. 2015;;7(Suppl 1:):S38––S43.. doi: 10.3978/j.issn.2072-1439.2015.01.31. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan D, Xu J, Shao S, Fu Y, Sun F, Zhang Y, et al. Comparison of different inspiratory triggering settings in automated ventilators during cardiopulmonary resuscitation in a porcine model. PLoS ONE. 2017;;12((2):):e0171869. doi: 10.1371/journal.pone.0171869. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beitler JR, Ghafouri TB, Jinadasa SP, Mueller A, Hsu L, Anderson RJ, et al. Favorable Neurocognitive outcome with low tidal volume ventilation after cardiac arrest. Am J Respir Crit Care Med. 2017;;195::1198––1206.. doi: 10.1164/rccm.201609-1771OC. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]