ABSTRACT
Background and aims
Multiple scoring systems are designed and prepared nowadays that can be used to determine and predict the severity, morbidity, and mortality rate of patients. Among them, the rapid emergency medicine score (REMS) system has been designed to predict the motility of nonsurgical patients admitted to the emergency department (ED). This study was performed with the aim of evaluating the predictive value of REMS in the mortality rate of nonsurgical patients.
Materials and methods
This study was carried out in 2017 among 300 nonsurgical patients referred to the ED. Data were collected using a checklist containing two parts of demographic information and REMS scale.
Results
Based on the results, we found a significant correlation between the duration of hospitalization and other parameters of the study. The results of this study indicated that the REMS of patients increased by 11%, 3%, and 5%, per each unit rise in patient’s age, heart rate, and respiratory rate, respectively. On the contrary, 12% and 22% decrements for every unit increase in SPO2 and GCS levels were observed, respectively. All the reported findings were statistically significant.
Conclusion
In sum, the outcomes of the present study corroborate the REMS system as a successful scale in predicting mortality and the duration of hospitalization in nonsurgical ED patients.
How to cite this article
Ala A, Vahdati SS, Jalali M, Parsay S. Rapid Emergency Medicine Score as a Predictive Value for 30-day Outcome of Nonsurgical Patients Referred to the Emergency Department. Indian J Crit Care Med 2020;24(6):418–422.
Keywords: Emergency department, Outcome, Rapid emergency medicine score, Scoring system
INTRODUCTION
In recent decades, several grading systems have been developed to provide a measuring method for evaluating the severity of illness and predicting patients’ outcomes, morbidity, and mortality. These scores are mainly designed for critically ill patients in order to assess any alterations in physiopathological variables of these patients. Such scores aim to bring the severity of the specific emergency and certain disease into an objective measurement, which is applicable and differentiable by any physician all over the world.1–3
With these tools, therapists can make an early assessment of each individual, consider the best approach, prioritize patients, and optimize the necessary care. The latter is more important in an emergency setting (especially in traumatic patients), who might need special attention because of their critical condition. Hence, achieving a standard scoring system is the mainstay of recent studies, notably those are contributed to the emergency department (ED).4,5
In patients admitted to the emergency room (ER), the outcomes of the disease are estimated by the severity of the illness at the time of admission. Measuring the patient’s vital signs is one of the best assessment tools to evaluate the severity of their condition. Likewise, deterioration in a patient’s condition or sudden death, primarily, presents with alteration in their vital signs. Any responsible situation for deteriorating a patient’s physical status is usually preventable if it is detected one time. Therefore, obviously, making a prompt action in patients’ management is crucial.6,7
The acute physiology and chronic health evaluation (APACHE-II) score is one of the classification systems used for determining the severity of illness among patients who require intensive care.8 It has been established as a valid modality for evaluating both surgical and general intensive care patients. Since the APACHE-II score includes several laboratory-dependent parameters, it is time-consuming and not conveniently suitable for the ER staff.9,10
The rapid acute physiology score (RAPS) is an alternative to APACHE-II score which includes only the physiologic variables: Glasgow coma scale (GCS), blood pressure (BP), respiratory rate (RR), and pulse rate (PR).11 The recent four parameters are easily obtained, yielding the RAPS generally usable in the ER. In order to make more precise and accurate emergency scoring system, a new scoring system is developed by adding the patient’s peripheral blood oxygenation rate (SPO2), body temperature (BT), and age (as an independent mortality risk factor for an acute illness) to the previously described RAPS, which is known as rapid emergency medicine score (REMS).1,7,12
The REMS firstly was introduced to predict the mortality rate among nonsurgical patients (the patients who were not planned to undergo surgical management based on the nature of their illness) admitted to the ED. It has seven parameters, as mentioned earlier, and a score ranging 0–30 on paper.
Based on the REMS, patients are classified into three major categories: high (REMS > 13), medium (6 < REMS < 13), and low (REMS < 6) mortality risk. For each point in which REMS is greater than 13, the patient’s mortality rate increases by 7.8 up to 17.1%.1,7
Because of the small number of studies on the outcome of nonsurgical patients referred to the ED, and considering that this study has not been carried out in Iran so far, we performed this study on a large sample size to evaluate the predictive value of REMS in the mortality rate of nonsurgical patients. All the patients were referred to the ED of Imam Reza Hospital of Tabriz University of Medical Sciences, as the major referral center of the northwest of Iran, in 2017.
MATERIALS AND METHODS
This analytic cross-sectional study was performed on 300 nonsurgical patients who were selected from those presented to the ER by using the convenient sampling method. The inclusion criteria were all nonsurgical patients who were willing to participate in the study, and the exclusion criterion was patients with cardiac arrest who did not respond to the cardiopulmonary resuscitation (CPR). All data were collected by a checklist (Table 1) for each patient which was prepared in two parts; a standard and broadly used REMS checklist followed by a section for patients’ demographic information. The parameters of the checklist were precisely completed by a trained emergency medicine resident within a 20-minute period for each patient. These parameters include GCS, blood pressure, body temperature, pulse rate, respiratory rate, SPO2, and age for the REMS (physiologic) part, whereas gender, chief complaint, diagnosis, duration of admission, and the patient’s outcome after 30 days were embedded within the demographic information part. All data were gathered in SPSS version 21 software and were analyzed using regression and ANOVA statistical tests.
Table 1.
Scoring procedure for the parameters in RAPS, peripheral oxygen saturation, body temperature, and age
| Physiological variable | High abnormal range | Low abnormal range | |||||||
|---|---|---|---|---|---|---|---|---|---|
| +4 | +3 | +2 | +1 | 0 | +1 | +2 | 3+ | +4 | |
| 1. Points to age have been assigned as follows (age, points): <45, 0; 45–54, 2; 55–64, 3; 66–74, 5; >74, 6. | |||||||||
| Body temperature | >40.9 | 39–40.9 | 38.5–38.9 | 36–38.4 | 34–35.9 | 32–33.9 | 30–31.9 | <30 | |
| Mean arterial pressure | >159 | 130–159 | 110–129 | 70–109 | 50–69 | <49 | |||
| Heart rate | >179 | 140–179 | 110–139 | 70–109 | 55–69 | 40–54 | <39 | ||
| Respiratory rate | >49 | 35–49 | 25–34 | 12–24 | 10–11 | 6–9 | <5 | ||
| Peripheral oxygen saturation | <75 | 75–85 | 86–89 | >89 | |||||
| Glasgow coma scale | <5 | 5–7 | 8–10 | 11–13 | >13 | ||||
| Total sum of scoring points | |||||||||
*REMS, rapid emergency medicine score
**RAPS, rapid acute physiology score
Appendix: REMS* point checklist
ETHICAL CONSIDERATION
Patients’ information entered to this study from records of individuals with a codename without mentioning the names of any participants. None of the patients’ personal information was included in this research.
Written informed consent was obtained from all the patients or their legal relatives before entering the study.
RESULTS
Totally 300 patients participated in this study. Among them, 154 (51.3%) of patients were male and 146 (48.7%) were female. The mean age of the patients was 59.21 ± 19.86 years, with a minimum age of 14 and a maximum of 95 years. The results of the physiological variables of patients are shown in Table 2.
Table 2.
Physiologic variables
| Age | Blood pressure | Heart rate | Respiratory rate | SPO2 | GCS | Body temperature | |
|---|---|---|---|---|---|---|---|
| Mean | 59.21 | 121.37 | 84.06 | 17.5 | 91.20 | 14.73 | 36.40 |
| Standard deviation | 19.86 | 21.98 | 17.28 | 8.35 | 9.42 | 2.23 | 1.74 |
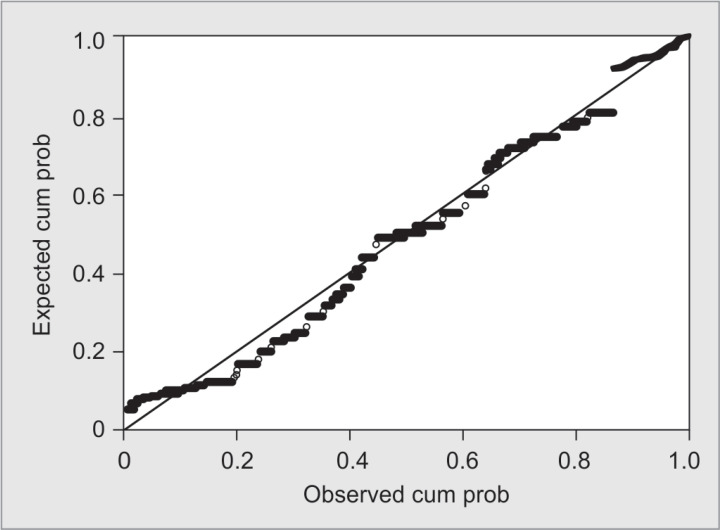
According to the results of this study, 13.3% of the patients died in the ED. Furthermore, 7% of them died in the first 48 days of admission. Likewise, 52.7% of patients discharged with complications, and 25.3% of them were discharged after complete healing. The most frequent REMS among all the patients was zero (22.7%), followed by seven (13.3%) which is explicitly demonstrated in Table 3. Most of the patients were hospitalized for more than ten days. Only 6.7% of the patients were intubated at the ED, and 66 (22%) were discharged from the ER. Based on the results of the regression test, there was a significant relationship between the duration of hospitalization and other variables of the study. This finding depicts that the duration of hospitalization was elevated by 5 (B = 0.05_ p = 0.01), 4 (B = 0.41_ p = 0.02), and 12 (B = 0.12_ p = 0.001) percent per each unit increase in patient’s age, pulse rate, and REMS point, respectively. The duration of hospitalization in patients with severe conditions is 1.5 times greater than that of other patients (B = 1.06_ p = 0.001). All these data were considered statistically significant. Figure 1 demonstrates the p–p plot graph of the effect of REMS on the duration of hospitalization.
Table 3.
Rapid emergency medicine score value frequency percentile
| Score | Frequency | Percent |
|---|---|---|
| 0 | 68 | 22.7 |
| 1 | 1 | 0.3 |
| 2 | 21 | 7 |
| 3 | 33 | 11 |
| 4 | 8 | 2.7 |
| 5 | 38 | 12.7 |
| 6 | 38 | 12.7 |
| 7 | 40 | 13.3 |
| 8 | 21 | 7 |
| 9 | 16 | 5.3 |
| 10 | 10 | 3.3 |
| 11 | 2 | 0.7 |
| 12 | 2 | 0.7 |
| 13 | 2 | 0.7 |
| Total | 300 | 100 |
Fig. 1.
Regression p–p plot graph of the effect of REMS on the duration of hospitalization
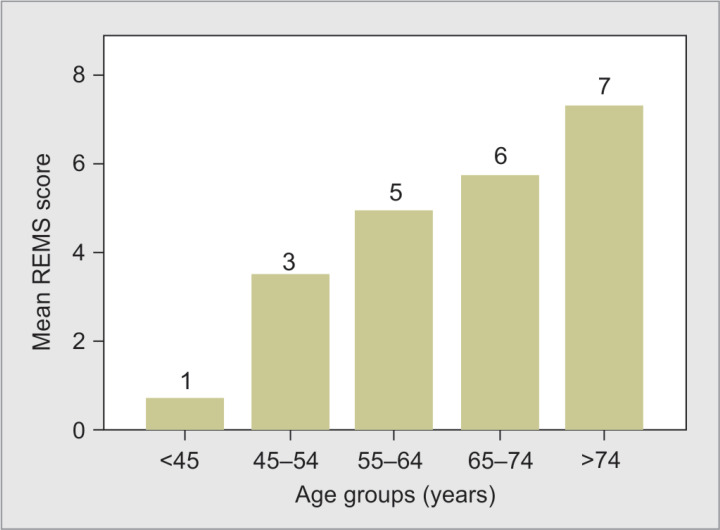
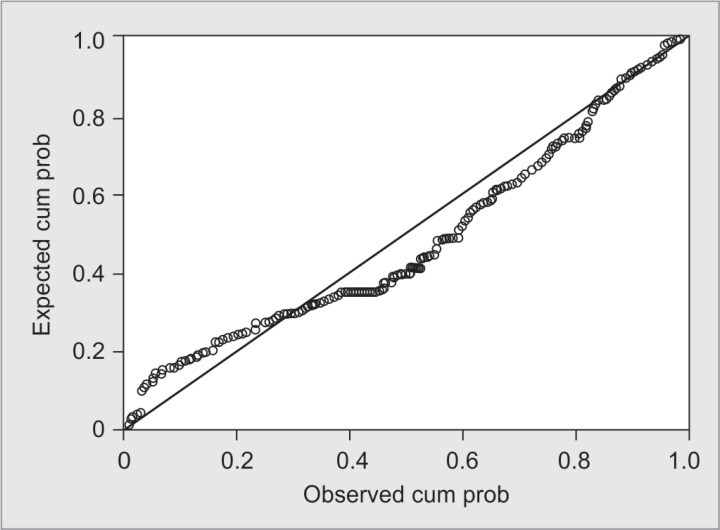
Furthermore, the REMS of patients increased by 11% (B = 0.11_ p = 0.000), 3% (B = 0.035_ p = 0.02), and 5% (B = 0.05_ p = 0.001), per each unit rise in patient’s age, heart rate, and respiratory rate, respectively (Table 4 and Figs 2 and 3) while the current score is decreased by 12% (B = 0.12_ p = 0.000) and 22% (B = 0.22_ p = 0.008) for each unit increase in SPO2 and GCS levels, respectively. The REMS is 0.078 units less in female individuals in comparison with males. Based on the regression test results, the REMS was 2% lower among the discharged patients than that of the others (B = 0.025_ p = 0.016).
Table 4.
Mean rapid emergency medicine score in each age, HR, and RR groups
| Parameter | Groups | Mean score | Number | Std. deviation | p value |
|---|---|---|---|---|---|
| Age groups | <45 | 0.74 | 76 | 1.886 | 0.000 |
| 45–54 | 3.48 | 33 | 2.489 | ||
| 55–64 | 4.98 | 54 | 2.499 | ||
| 65–74 | 5.76 | 54 | 1.801 | ||
| >74 | 7.29 | 83 | 2.051 | ||
| Total | 4.52 | 300 | 3.254 | ||
| HR groups | 0 point | 4.25 | 262 | 3.062 | 0.02 |
| +2 point | 6.65 | 31 | 3.720 | ||
| +3point | 5.14 | 7 | 4.880 | ||
| Total | 4.52 | 300 | 3.254 | ||
| RR groups | 0 point | 4.39 | 281 | 3.225 | 0.001 |
| +1 point | 6.19 | 16 | 3.331 | ||
| +3 point | 7.67 | 3 | 2.082 | ||
| Total | 4.52 | 300 | 3.254 |
HR, heart rate; RR, respiratory rate
Fig. 2.
Mean REMS in each of the age groups
Fig. 3.
Regression p–p plot graph of the effect of increase in the age on REMS
DISCUSSION
In this study, the predictive values of REMS in estimating the 30-day outcomes of nonsurgical patients referred to the ED of Imam Reza Hospital of Tabriz University of Medical Sciences, in 2017, were evaluated. The 30-day outcomes of patients in this study include the rates of patients’ death in ED, death in the first 48 hours of admission, discharge with complication, discharge with full recovery, and death at home. Based on what we mentioned earlier, the results showed a significant statistical relationship between REMS and patients outcome after 30 days of admission. The REMS value was lower in females by 0.078 points, and it was 2% less among the discharged patients. Besides, there was a statistically significant relationship between the duration of hospitalization and other variables of the study.
The REMS system was first described by Olsson et al., on nonsurgical emergency ward patients. In their study, the REMS system score had a direct relationship with the prediction of the duration of hospitalization and inpatient mortality rate. Their findings demonstrated an increase in the mortality rate and hospitalization period for each patient, by increasing in REMS value.1
In another study, the REMS system was found as a valuable scoring system in predicting inpatient mortality rate and duration of hospitalization.7
In the present study, for each unit increase in REMS, the duration of hospitalization increased by 12%, and the mortality rate increased by 3%, which is consistent with similar studies.
Goodarc et al. showed that the REMS system tends to be a good predictor of morbidity in patients admitted to the ED. In addition, age, GCS level, and SPO2 of patients might be independent variables for predicting the mortality rate in patients. Furthermore, the REMS of elderly patients was 1.7-fold greater than younger individuals. The REMS of patients with higher GCS and SPO2 levels was 2.1 and 1.3 times greater than those with low GCS and SPO2, respectively, which is also compatible with the results of this study.13
As mentioned earlier, based on the REMS, patients are classified into three risk stratification categories, including high (REMS > 13), medium (6 < REMS < 13), and low (REMS < 6) mortality risk. The higher the REMS value, the higher the mortality rate. Our findings depicted this very well, as each point increase in REMS was accompanied by 7.8%–17.1% increment in mortality rate.1,7
In various studies, the REMS system has been reported valuable for the prediction of the mortality rate among surgical, nonsurgical, and traumatic patients, in the setting of ER.12,14 Based on their results, by increasing the REMS, the mortality rate increases, which confirms the results of our study.
Another research assessed the predictive value of REMS and WPS (worthing physiological scoring system) in the 30-day mortality rate of nonsurgical patients admitted to the ED. The results revealed that the risk of 30-day mortality of patients increased by 30% (HR:1.28_ 95% CI 1.23–1.34) per each unit increase in REMS, and 60% (HR:1.6_ 95% CI 1.5–1.7) per each unit of WPS, which is also compatible with our study.15
In a study in Taiwan, which was performed on the HPVG (hepatic portal venous gas) patients, who were admitted to the ED, sensitivity, specificity, and accuracy of REMS were reported as 92.1%, 89.3%, and 90.9%, respectively, in predicting mortality of these patients.16 These findings were well-aligned with the results of our study, as well.
CONCLUSION
This analytic cross-sectional study was performed to assess the predictive value of REMS in a 30-day outcome of nonsurgical patients referring to Imam Reza Hospital of Tabriz University of Medical Sciences, in 2017, which was conducted for the first time in Iran. With the information obtained from this study, a suitable platform for prioritizing patients referred to the ED could be provided. These findings might improve the provision of the best curative option for patients and reduce the mortality rate. Another advantage of the REMS system, which was introduced in this study, was its comprehensive application, which could easily be used in the ED.
The results of this study confirmed that the REMS system could be successful in predicting mortality and the duration of hospitalization in nonsurgical ED patients. However, the parameters of this system such as age, heart rate, respiratory rate, and SPO2 of patients are independent variables for predicting mortality and the hospitalization period of such patients. Therefore, interventional studies based on the findings of this study are needed to improve the health and the status of the patients referred to the ED, followed by the development of a comprehensive program and choosing the appropriate policy in this field.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This manuscript was approved by the ethics committee of Tabriz University of Medical Science.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all the patients or their first-degree relatives—in case the patient was not able to give the consent—before they participated in the study. It was also assured to the patients that all personal information would remain confidential and the results of the study would be published in general.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Olsson T, Terént A, Lind L. Rapid emergency medicine score: a new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J Intern Med Suppl. 2004;;255((5):):579––587.. doi: 10.1111/j.1365-2796.2004.01321.x. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Toma T, Abu-Hanna A, Bosman R-J. Discovery and inclusion of SOFA score episodes in mortality prediction. J Biomed Inform. 2007;;40((6):):649––660.. doi: 10.1016/j.jbi.2007.03.007. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Howell MD, Donnino MW, Talmor D, Clardy P, Ngo L, Shapiro NI. Performance of severity of illness scoring systems in emergency department patients with infection. Acad Emerg Med. 2007;;14((8):):709––714.. doi: 10.1197/j.aem.2007.02.036. DOI: [DOI] [PubMed] [Google Scholar]
- 4.Rahimzadeh P, Taghipur Anvari Z, Hassani V. Estimation of mortality rate of patients in surgical intensive care unit of Hazrat-Rasul hospital. Hakim Res J. 2008;;11::22––28.. [Google Scholar]
- 5.Brabrand M, Folkestad L, Clausen NG, Knudsen T, Hallas J. Risk scoring systems for adults admitted to the emergency department: a systematic review. Scand J Trauma Resusc Emerg Med. 2010;;18((1):):8.. doi: 10.1186/1757-7241-18-8. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coslovsky M, Takala J, Exadaktylos AK, Martinolli L, Merz TM. A clinical prediction model to identify patients at high risk of death in the emergency department. Intensive Care Med. 2015;;41((6):):1029––1036.. doi: 10.1007/s00134-015-3737-x. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olsson T, Lind L. Comparison of the rapid emergency medicine score and APACHE II in nonsurgical emergency department patients. Acad Emerg Med. 2003;;10((10):):1040––1048.. doi: 10.1197/S1069-6563(03)00342-7. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;;13((10):):818––829.. doi: 10.1097/00003246-198510000-00009. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Chen Y-C, Hsu H-H, Kao K-C, Fang J-T, Huang C-C. Outcomes and APACHE II predictions for critically ill patients with acute renal failure requiring dialysis. Ren Fail. 2001;;23((1):):61––70.. doi: 10.1081/jdi-100001284. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Challen K, Goodacre SW. Predictive scoring in non-trauma emergency patients: a scoping review. Emerg Med J. 2011;;28((10):):827––837.. doi: 10.1136/emj.2010.099291. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Rhee KJ, Fisher CJ, Willitis NH. The rapid acute physiology score. Am J Emerg Med. 1987;;5((4):):278––282.. doi: 10.1016/0735-6757(87)90350-0. DOI: [DOI] [PubMed] [Google Scholar]
- 12.Imhoff BF, Thompson NJ, Hastings MA, Nazir N, Moncure M, Cannon CM. Rapid emergency medicine score (REMS) in the trauma population: a retrospective study. BMJ Open. 2014;;4((5):):e004738. doi: 10.1136/bmjopen-2013-004738. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodacre S, Turner J, Nicholl J. Prediction of mortality among emergency medical admissions. Emerg Med J. 2006;;23((5):):372––375.. doi: 10.1136/emj.2005.028522. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bulut M, Cebicci H, Sigirli D, Sak A, Durmus O, Top AA, et al. The comparison of modified early warning score with rapid emergency medicine score: a prospective multicentre observational cohort study on medical and surgical patients presenting to emergency department. Emerg Med J. 2014;;31((6):):476––481.. doi: 10.1136/emermed-2013-202444. DOI: [DOI] [PubMed] [Google Scholar]
- 15.Ha DT, Dang TQ, Tran NV, Vo NY, Nguyen ND, Nguyen TV. Prognostic performance of the rapid emergency medicine score (REMS) and worthing physiological scoring system (WPS) in emergency department. Int J Emerg Med. 2015;;8((1):):18.. doi: 10.1186/s12245-015-0066-3. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seak C-J, Yen DH-T, Ng C-J, Wong Y-C, Hsu K-H, Seak JC-Y, et al. Rapid emergency medicine score: a novel prognostic tool for predicting the outcomes of adult patients with hepatic portal venous gas in the emergency department. PLoS ONE. 2017;;12((9):):e0184813. doi: 10.1371/journal.pone.0184813. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]