Abstract
Left ventricular diastolic dysfunction (LVDD) and heart failure with preserved ejection fraction (HFpEF) are microcirculation defects following diabetes mellitus (DM). Unrecognized HFpEF is more prevalent in women with diabetes compared to men with diabetes and therefore sex-specific diagnostic strategies are needed. Previously, we demonstrated altered plasma miRs in DM patients with microvascular injury [defined by elevated plasma Angiopoietin-2 (Ang-2) levels]. This study hypothesized the presence of sex-differences in plasma miRs and Ang-2 in diabetic (female) patients with LVDD or HFpEF. After a pilot study, we assessed 16 plasma miRs in patients with LVDD (n = 122), controls (n = 244) and female diabetic patients (n = 10). Subsequently, among these miRs we selected and measured plasma miR-34a, -224 and -452 in diabetic HFpEF patients (n = 53) and controls (n = 52). In LVDD patients, miR-34a associated with Ang-2 levels (R2 0.04, R = 0.21, p = 0.001, 95% CI 0.103–0.312), with plasma levels being diminished in patients with DM, while women with an eGFR < 60 ml/min and LVDD had lower levels of miR-34a, -224 and -452 compared to women without an eGFR < 60 ml/min without LVDD. In diabetic HFpEF women (n = 28), plasma Ang-2 levels and the X-chromosome located miR-224/452 cluster increased compared to men. We conclude that plasma miR-34a, -224 and -452 display an association with the microvascular injury marker Ang-2 and are particularly targeted to women with LVDD or HFpEF.
Subject terms: Biomarkers, Cardiology
Introduction
Heart failure with preserved ejection fraction (HFpEF), and its precursor left ventricular diastolic dysfunction (LVDD), are manifestations of microvascular injury in diabetes patients1. The pathophysiology of microvascular injury in this patient population is associated with more hospitalization and cardiovascular death2. Especially women with type 2 diabetes mellitus (DM) have a higher prevalence of HFpEF compared to men (28% vs. 18.4%), which often remains undiagnosed until the later stage of the disease3–7. Therefore, the need to develop appropriate diagnostic strategies specific for women is critical, whereby the assessment of plasma microRNA (miR) levels could improve the detection of HFpEF and its precursor LVDD following type 2 DM.
Previously, we demonstrated that a select subset of circulating angiogenic miRs (among others miR-126, miR-130b, miR-223 and miR-660) are increased in plasma derived from diabetic nephropathy patients (both women and men) and associate with microvascular injury, as defined by elevated plasma levels of Ang-2 levels8. In addition, we have demonstrated in a review of the literature that the differential expression of (plasma) miRs between women and men involves at least two potential mechanisms: (1) double dosage of X-chromosome located (X-linked) miRs due to incomplete X-chromosome inactivation and (2) estrogen regulation of miR transcription and processing9. The augmented expression of endothelial X-linked miRs has been established to instigate microcirculation defects9 while higher plasma levels of these miRs have previously been shown to identify microvascular injury in women with other cardiovascular disease phenotypes such as idiopathic atrial fibrillation (iAF)10.
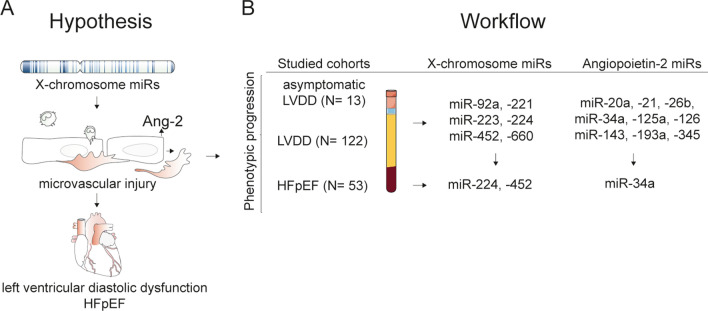
The present study hypothesizes that sex-specific plasma miRs are differentially expressed in (female) patients with HFpEF and its precursor LVDD (in particular in patients with diabetes) and associate with microvascular injury (defined by elevated plasma Ang-2 levels) (Fig. 1A). To test this, we assessed plasma Ang-2 (a tyrosine-protein kinase (TIE-2) receptor ligand that promotes endothelial activation and destabilization) and 16 candidate X-chromosome located (X-linked) miRs in (diabetic) LVDD and (diabetic) HFpEF patients. In addition, we performed sex-specific stratification of plasma- Ang-2 and miR level results and logistic regression analysis to assess which clinical characteristics are associated with significant differentially expressed plasma miRs.
Figure 1.
Hypothesis and workflow of the study. (A) This study hypothesized that sex-specific plasma miRs (derived from the X-chromosome) are differentially expressed in (female) patients with LVDD and HFpEF and associate with microvascular injury (defined by increased plasma Ang-2 levels). (B) In the workflow of the study we measured plasma Angiopoietin-2, X-chromosome located miRs and miRs that were previously found to associate with Ang-2 (Ref.8,10,12) in plasma from female patients with asymptomatic LVDD (n = 13). Next, we measured these miRs in patients with LVDD (n = 122) compared to their controls (n = 244). Subsequently and following analysis of the results we selected miR-34a. -224 and -452 and measured their plasma levels in patients with HFpEF (n = 52) compared to their respective controls (n = 53).
Results
Patient characteristics
Asymptomatic LVDD patients (Maastricht study)
Supplemental Table 1 displays the clinical characteristics of patients with a previous history of preeclampsia and asymptomatic LVDD (n = 13) compared to healthy controls (n = 14). Women with asymptomatic LVDD had a higher ratio of mitral peak velocity of early filling (E) to early diastolic mitral annular velocity (E') (E/E' ratio) and a higher left atrial volume index (LAVI) compared to healthy parous controls.
LVDD patients (HELPFul study)
Table 1 displays the clinical characteristics of diabetic patients with LVDD (n = 12), derived from the HELPFul cohort, consisting of patients with LVDD (Supplemental Table 2). The HELPFul cohort is an ongoing case-cohort study at a Dutch cardiology outpatient clinic enrolling patients aged 45 years and older with no prior history of cardiovascular disease, who were referred by the general practitioner for cardiac evaluation11. Women with LVDD (n = 10) had a higher systolic- and diastolic blood pressure compared to women without LVDD (Table 1).
Table 1.
(Sex-stratified) clinical characteristics of diabetes mellitus (DM) patients with or without LVDD.
| Total population | Women | Men | ||||
|---|---|---|---|---|---|---|
| DM without LVDD (N = 17) | DM with LVDD (N = 12) | DM without LVDD (N = 7) | DM With LVDD (N = 10) | DM without LVDD (N = 10) | DM with LVDD (N = 2) | |
| Sex, male, n (%) | 10 (59%) | 2 (17%)1 | 0 (0%) | 0 (0%) | ||
| Age (years) | 63.1 ± 8.7 | 66.2 ± 8.5 | 63.1 ± 6.2 | 66.2 (8.9) | 61.5 ± 10 | 68.4 ± 9.9 |
| BMI (kg/m2) | 27.8 ± 3.3 | 32.3 ± 7.01 | 28.9 ± 3.7 | 33.6 ± 6.9 | 26.9 ± 3.9 | 27.1 ± 3.4 |
| Systolic BP (mm Hg) | 149.1 ± 15.9 | 156.7 ± 16.3 | 153.3 ± 16.3 | 156.5 ± 14.5 | 147.4 ± 19.6 | 158.1 ± 16.4 |
| Diastolic BP (mm Hg) | 85.3 ± 12.8 | 87.9 ± 9.2 | 85.8 ± 5.8 | 88.0 ± 9.5 | 88.1 ± 10.9 | 93.0 ± 10.7 |
| Current or former smoker, n (%) | 11 (65%) | 8 (67%) | 4 (57%) | 6 (60%) | 55 (65%) | 27 (73%) |
| Hypertension, n (%) | 13 (76%) | 11 (92%) | 6 (86%) | 9 (90%) | 48 (58%) | 23 (64%) |
| Diabetes mellitus, n (%) | 17 (100%) | 12 (100%) | 7 (100%) | 10 (100%) | 10 (100%) | 2 (100%) |
| eGFR < 60 ml/min | 2 (12%) | 3 (25%) | 1 (14%) | 2 (20%) | 1 (10%) | 1 (50%) |
| Creatinine (umol/L) | 68.8 (63.2–79.4) | 67.6 (60.8–76) | 68.1 (64.8–79.8) | 63.8 (59.4–69.2) | 83.2 (68.3–91.9) | 95.1 (93.8–95.1) |
| Total cholesterol (mmol/L) | 4.5 ± 0.9 | 4 ± 1.1 | 4.7 ± 0.7 | 4.0 ± 1.2 | 4.4 ± 1.1 | 3.8 ± 0.6 |
| HDL-cholesterol (mmol/L) | 1.3 ± 0.3 | 1.2 ± 0.2 | 1.5 ± 0.4 | 1.2 ± 0.3 | 1.1 ± 0.1 | 1.1 ± 0.2 |
| Triglycerides (mmol/L) | 2.2 ± 1.0 | 1.7 ± 1.1 | 2.6 ± 1.2 | 1.8 ± 1.2 | 1.8 ± 0.8 | 1.3 ± 0.07 |
| Echocardiography | ||||||
| Ejection fraction | 66.8 (62.9–76) | 68.4 (63.5–73.7) | 66.8 (56.7–77.6) | 68.4 (63.8–75.9) | 66 (63.4–74.2) | 66 (61.5–66.6) |
| EA ratio | 0.8 ± 0.2 | 0.7 ± 0.1 | 0.9 ± 0.1 | 0.7 ± 0.11 | 0.8 ± 0.3 | 0.7 ± 0.1 |
| E/E’ ratio | 8.9 (8.3–10.9) | 9.4 (8.3–11.7) | 9.6 (8.2–11.5) | 10 (8.9–12.2) | 8.8 (7.9–10.9) | 8.2 (7.6–8.2) |
| LAVI (mL/m2) | 23.7 (16.7–25.4) | 25.6 (16–33.1) | 24.3 (13.5–27.0) | 24.3 (15.8–35.5) | 22.9 (16.8–24.3) | 28 (26.6–28) 1 |
| LVMI (g/m2) | 70.0 ± 15.6 | 82 ± 22.0 | 67 ± 9 | 78.3 ± 20.5 | 72 ± 19 | 100.5 ± 26.8 |
| RWT | 0.38 (0.31–0.47) | 0.46 (0.41–0.48) | 0.37 (0.31–0.39) | 0.46 (0.42–0.47) 1 | 0.45 (0.30–0.52) | 0.46 (0.41–0.46) |
| BNP (pg/mL) | 16.9 (5–23.4) | 11.5 (2.5–35.9) | 24.8 (0–47.9) | 11.4 (0–34.2) | 13.4 (7.5–21.2) | 42.5 (10.2–42.5) |
| e’ septal velocity (cm/sec) | 7 (5–8.5) | 6 (5–7) | 8 (6–9) | 6.5 (5–7.3) | 6.5 (5–8.3) | 5 (4–5) |
| e’ lateral velocity (cm/sec) | 9 (7–10) | 8 (6.3–9) | 10 (9–10) | 8 (5.8–8.3) 1 | 8 (6.8–9.5) | 9.5 (9–9.5) |
EA ratio, ratio of early (e) to late (a) ventricular filling; E/E’ ratio, ratio of mitral peak velocity of early filling (E) to early diastolic mitral annular velocity (E'); LAVI, left atrial volume index; LVMI, left ventricular mass index; RWT, relative wall thickness; BNP, brain natriuretic peptide; TPV, tricuspid valve regurgitation velocity. Parametric data is presented as mean ± SD or median ± SD. Non-parametric data is presented as median and IQR. Categorical data is presented as frequency and percentage. 1p < 0.05 versus no LVDD as determined by Independent samples t-test for all normally distributed continuous variables, Pearson chi-square test for binary variables and Independent Samples Mann Whitney U test for non-normally distributed variables.
HFpEF patients (UHFO-DM study)
Table 2 displays the clinical characteristics of DM patients with HFpEF (n = 53). HFpEF women (n = 28) had a higher E/e’ ratio than HFpEF men (n = 27), while HFpEF men had a higher LAVI and higher plasma levels of circulating brain natriuretic peptides (BNP).
Table 2.
(Sex-stratified) clinical characteristics of diabetes patients with (N = 53) or without HFpEF (N = 52).
| Total population | Women | Men | ||||
|---|---|---|---|---|---|---|
| Controls (N = 52) | HFpEF (N = 53) | Controls (N = 26) | HFpEF (N = 28) | Controls (N = 24) | HFpEF (N = 27) | |
| Age (years) | 69.8 ± 6.9 | 75.4 ± 6.81 | 69.2 ± 7.5 | 75.2 ± 5.91 | 70.4 ± 6.3 | 75.6 ± 7.71 |
| BMI (kg/m2) | 27.6 ± 5.1 | 30.1 ± 4.11 | 28.3 ± 6.0 | 31.5 ± 4.41 | 26.8 ± 4 | 28.7 ± 3.3 |
| Systolic BP (mm Hg) | 159.7 ± 21.7 | 162.3 ± 22.0 | 165.6 ± 24.8 | 162.7 ± 21.7 | 153.8 ± 16.5 | 162.7 ± 22.8 |
| Diastolic BP (mm Hg) | 89 ± 11 | 89.9 ± 11.1 | 92 ± 12.3 | 91.3 ± 11.6 | 86 ± 8.6 | 88.4 ± 10.5 |
| Current or former smoker | 5 (8%) | 9 (15%) | 3 (10%) | 2 (7%) | 2 (7%) | 7 (23%) |
| Hypertension | 38 (63%) | 44 (73%) | 23 (77%) | 26 (87%) | 15 (50%) | 18 (60%) |
| eGFR < 60 ml/min | 7 (13%) | 12 (22%) | 5 (17%) | 5 (19%) | 2 (8%) | 7 (25%) |
| Creatinine (umol/L) | 77 (65–87) | 77 (65–91) | 70 (60.5–81) | 67.5 (60.5–76.5) | 82 (73.8–92.3) | 89 (76–102) |
| Hypercholesterolemia | 45 (75%) | 38 (63%) | 22 (73%) | 20 (67%) | 23 (77%) | 18 (60%) |
| Echocardiography | ||||||
| Ejection fraction | 60.6 (54.5–65.9) | 60.8 (55.0–65.6) | 61.4 (55.8–66.6) | 61.0 (56.9–68.2) | 60.4 (54.2–63.0) | 59.3 (53.4–64.9) |
| EA ratio | 0.80 ± 0.19 | 0.83 ± 0.62 | 0.80 ± 0.19 | 0.80 ± 0.38 | 0.79 ± 0.19 | 0.87 ± 0.81 |
| E/E’ ratio | 8.6 (7.2–10.2) | 10.6 (9.2–12.7)2 | 9.8 (8.0–10.8) | 11.5 (10.3–14.7)2 | 8.3 (6.3–9.0) | 9.9 (7.8–11)2 |
| LAVI (mL/m2) | 24.2 (18.4–29.9) | 29.3 (25–34.1)2 | 24.4 (18–31.3) | 27.7 (24.5–32.2) | 24.0 (19.6–29.6) | 32.4 (25.5–37.4)2 |
| RWT | 0.31 (0.28–0.34) | 0.31 (0.26–0.38) | 0.32 (0.28–0.34) | 0.33 (0.30–0.41) | 0.31 (0.27–0.24) | 0.29 (0.24–0.36) |
| BNP (pg/mL) | 8 (5–12) | 13.5 (8–28.3)2 | 10 (5–16.5) | 13 (8–22.5) | 7 (4.8–9.3) | 15.5 (8–37.3)2 |
EA ratio, ratio of early (e) to late (a) ventricular filling; E/E’ ratio, ratio of mitral peak velocity of early filling (E) to early diastolic mitral annular velocity (E'); LAVI, left atrial volume index; RWT, relative wall thickness; BNP, brain natriuretic peptide. Parametric data is presented as mean ± SD or median ± SD. Non-parametric data is presented as median and IQR. Categorical data is presented as frequency and percentage. 1p < 0.05 (significant difference between groups) as determined by Independent samples T-test for normally distributed continuous variables. 2p < 0.05 (significant difference between groups) as determined by Independent Samples Mann–Whitney U test.
Pilot study identifies candidate miRs that associate with microvascular injury
We performed a pilot study to select candidate plasma miRs for plasma profiling in LVDD and HFpEF patients. In this study we assessed plasma levels of (1) 118 X-chromosome located miRs in healthy women and men (n = 6) (Supplemental Table 3). Out of differentially expressed miRs, we selected the X-linked miR-660 for further analysis in asymptomatic LVDD and LVDD patients (Fig. 1B).
Furthermore, based on our previously published studies into the association of plasma miRs with microvascular injury in diabetic nephropathy8, idiopathic atrial fibrillation10 and kidney transplant rejection12 as well as a review of the literature of miRs associated with angiogenesis, or their X-linked origin, we selected the following miRs for analysis in the second pilot study: miR-20a, miR-21, miR-26b, miR-34a, miR-92a, miR-125a, miR-126, miR-143, miR-193a, miR-221, miR-223, miR-224, miR-345, miR-452 (References can be found in Supplemental Table 4).
In the second pilot study, the aforementioned miRs were measured in plasma from women with a previous history of pre-eclampsia and asymptomatic LVDD (n = 13, Clinical characteristics in Supplemental Table 1) compared to healthy controls (n = 14) to determine a potential association with diastolic dysfunction. We observed that of the measured miRs, only plasma levels of miR-224 (FC 1.5, p = 0.03, 95% CI 0.095–0.598) were increased in women with asymptomatic LVDD (Supplemental Table 5 and Supplemental Figure 1A) compared to healthy parous controls.
Next, given that women with a history of preeclampsia have an increased risk for microvascular injury and heart failure13, we assessed whether women with preeclampsia and asymptomatic LVDD indeed display an association with microvascular injury. To that extent we measured markers of microvascular injury in plasma from women with a previous history of pre-eclampsia and asymptomatic LVDD (n = 13, Supplemental Table 1) As compared to healthy controls (n = 14), our assessment of Ang-2, soluble trombomodulin (sTM) and soluble fms-like tyrosine kinase-1 (sFlt-1) revealed that only plasma Ang-2 levels were higher in women with a history of preeclampsia and asymptomatic LVDD (fold change (FC) 1.4, p = 0.02, 95% CI 230.5–1,084) (Supplemental Table 5 and Supplemental Figure 1B).
Finally, we assessed the association between markers of microvascular injury (Ang-2, sTM, sFflt-1) and plasma miRs and observed moderate positive associations for Ang-2 and miR-34a (R = 0.36, FDR adjusted p = 0.02), -224 (R = 0.32, FDR adjusted p = 0.03), and miR-452 (R = 0.39, FDR adjusted p = 0.01). Similar associations were found for sTM and miR-125a (R = − 0.38, FDR adjusted p = 0.01), -126 (R = − 0.30, FDR adjusted p = 0.04) and miR-143 (R = − 0.39, FDR adjusted p = 0.01) (Supplemental Figure 1C).
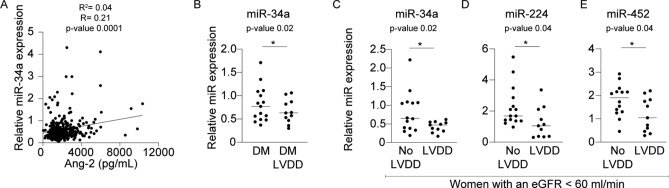
Plasma miR-34a in patients with diabetes and LVDD
Having identified a differential expression of plasma miR-224 and Ang-2 in women with asymptomatic LVDD, we next aimed to investigate whether patients with LVDD (Clinical characteristics in Supplemental Table 2) also have increased plasma miRs and Ang-2 levels. However, we observed that plasma miRs and Ang-2 were not significantly different in patients with LVDD (n = 122) compared to healthy controls (n = 244) (data not shown). Next, we assessed a potential association between plasma miRs and Ang-2 in patients with LVDD. Interestingly, in the entire cohort of patients with LVDD and controls we found that miR-34a was associated with plasma levels of Ang-2 (R2 0.04, R = 0.21, p = 0.001, 95% CI 0.103–0.312, Fig. 2A).
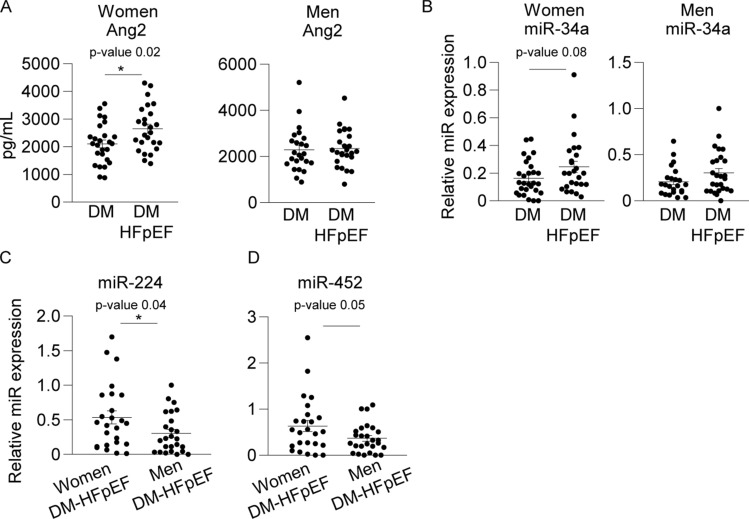
Figure 3.
Plasma Ang-2 levels and plasma miR-34a, -224 and -452 in (female) DM patients with HFpEF. (A) Increased plasma Ang-2 (Fold change 1.3, p = 0.02, 95% CI 110.5–980.9) levels in diabetic women with HFpEF compared to diabetic women without HFpEF (but not in diabetic HFpEF men compared to diabetic men without HFpEF), (B) miR-34a displayed a trend towards an increase in diabetic women with HFpEF compared to diabetic women without HFpEF only (Fold change 1.5, p = 0.08, 95% CI − 0.009 to 0.173). (C) Increased plasma levels of miR-224 (Fold change 0.57, p = 0.04, 95% CI − 0.452 to − 0.010) and (D) miR-452 (Fold change 0.58, p = 0.05, − 0.539 to − 0.002) in diabetic women with HFpEF compared to diabetic men with HFpEF. Relative miR expression values are normalized to plasma miR-16 levels, presented as mean ± standard error of the mean (SEM) and group differences are depicted as *p ≤ 0.05 according to a student T-test.
Figure 2.
Plasma Ang-2 levels and circulating miR-34a, -224 and -452 in (female) DM patients with LVDD compared controls. (A) Particularly miR-34a displayed a significant correlation with Ang-2 in the total patient population of patients with LVDD (N = 366, R2 0.04, R = 0.21, p = 0.001, 95% CI 0.103–0.312). (B) Lower levels of miR-34a in diabetic patients with LVDD compared to diabetic patients without LVDD (Fold change 1.2, p = 0.02, 95% CI − 0.428 to 0.117). (C) Lower levels of miR-34a, in women with an eGFR < 60 ml/min and LVDD compared to women without LVDD (Fold change 1.9, p = 0.03, CI − 0.737 to − 0.030). (D) Decreased plasma miR-224 in women with an eGFR < 60 ml/min and LVDD compared to women without LVDD (Fold change 1.8, p = 0.04, CI − 1.998 to − 0.059) and (E) decreased miR-452 in women with an eGFR < 60 ml/min and LVDD compared to women without LVDD (Fold change 1.5, p = 0.04, CI − 1.213 to − 0.039). Relative miR-expression values are normalized to plasma miR-16 levels, presented as mean ± standard error of the mean (SEM) and group differences are depicted as *p ≤ 0.05. Correlations between variables were calculated using the Spearman rank correlation.
Subsequently, we conducted a linear regression analysis to assess which clinical characteristics determine plasma miR-34a in patients with LVDD. This analysis (Table 3) identified that particularly sex (β = − 0.160, p value = 0.002) and the presence of DM (β = 0.121, p value = 0.02) were statistically significant determinants of this relationship while an eGFR < 60 ml/min displayed a trend towards an association, although non-significant (β = − 0.101, p value = 0.09). Given that the presence of DM was a significant determinant of plasma miR-34a, we assessed plasma levels of miR-34a in patients with diabetes, with or without LVDD (Table 1) and found significant lower plasma levels of miR-34a in diabetic patients with LVDD compared to diabetic patients without LVDD (FC 1.23, p = 0.02, 95% CI − 0.428 to 0.117, Fig. 2B).
Table 3.
Multiple linear regression analysis of the association between clinical characteristics and plasma miRs.
| miR-34a | miR-224 | miR-452 | ||||
|---|---|---|---|---|---|---|
| β | p value | β | p value | β | p value | |
| Age | 0.106 | 0.097 | 0.004 | 0.955 | 0.002 | 0.970 |
| Sex | − 0.160 | 0.002 | 0.145 | 0.007 | 0.165 | 0.002 |
| eGFR | − 0.101 | 0.099 | − 0.035 | 0.579 | − 0.101 | 0.107 |
| Hypertension | − 0.098 | 0.065 | − 0.045 | 0.412 | − 0.046 | 0.402 |
| Diabetes Mellitus | 0.121 | 0.022 | 0.033 | 0.537 | 0.020 | 0.711 |
| Obesity | 0.113 | 0.035 | 0.010 | 0.851 | − 0.074 | 0.173 |
In the linear regression model, miRs are dependent variables while age, sex, eGFR, hypertension, diabetes mellitus and obesity are independent variables. A simultaneous method of entry was used in the regression model. “β” means standardized regression coefficients; “p value” indicates significance.
Sex-specific plasma miR-34a, -224 and -452 levels in women with an eGFR < 60 ml/min and LVDD
In our pilot study in women with asymptomatic LVDD we observed significant correlations between plasma Ang-2 and miR-224 and -452. Therefore, we used linear regression analysis (Table 3) to investigate if sex could determine plasma miR-34a, -224 and -452 levels in patients with LVDD. We found that indeed sex was a significant determinant of this relationship for miR-34a (β = − 0.160, p = 0.002), miR-224 (β = 0.145, p = 0.002) and miR-452 (β = 0.165, p = 0.007). Interestingly, linear regression analysis also demonstrated that an eGFR < 60 ml/min displayed a (non-significant) trend as determinant of plasma miR-34a (β = − 0.101, p = 0.09), while an eGFR < 60 ml/min could not determine plasma miR-224 (p = 0.58) or miR-452 (p = 0.11).
Subsequently, we assessed differential expression of these miRs in patients with an eGFR < 60 ml/min with or without LVDD (clinical characteristics in Supplemental Table 6. Results from this analysis demonstrated that in particular female patients with LVDD with an eGFR < 60 ml/min displayed lower levels of miR-34a (FC 1.9, p = 0.03, CI − 0.737 to − 0,030, Fig. 2C), miR-224 (FC 1.8, p = 0.04, CI − 1.998 to − 0.059, Fig. 2D) and miR-452 (FC 1.5, p = 0.04, CI − 1.213 to − 0.039, Fig. 2E) compared to female patients with an eGFR < 60 ml/min without LVDD.
Plasma Ang-2 and miR-34a, -224 and -452 levels in women with diabetes and HFpEF
Next we hypothesized that the phenotypic progression from LVDD to HFpEF in the setting of DM could be associated with pronounced microvascular injury, and increased Ang-2 levels. For this, we measured plasma Ang-2 levels in DM patients with HFpEF (Table 2, n = 53). Here, we observed increased levels of plasma Ang-2 (FC 1.3, p = 0.02, 95% CI 110.5–980.9, Fig. 2A) in diabetic women with HFpEF (n = 28) as compared to diabetic women without HFpEF (n = 27).
Next, we selected miR-34a, -224 and -452 based on pilot study results and measured their plasma levels in DM patients with HFpEF compared to DM patients without HFpEF. In diabetic patients (both women and men) with HFpEF (n = 53) compared to diabetic patients without HFpEF (n = 52), we observed no significant differences in miR-224 and -452 levels (data not shown). However, plasma levels of miR-34a displayed a trend towards an increase in diabetic women with HFpEF (n = 28) compared to diabetic women without HFpEF (n = 27, FC 1.5, p = 0.08, 95% CI − 0.009 to 0.173, Fig. 2B). In addition, when women with HFpEF (n = 28) were compared to men with HFpEF (n = 27), the plasma levels of miR-224 (FC 0.57, p = 0.04, 95% CI − 0.452 to − 0.010, Fig. 2C) and miR-452 (FC 0.58, p = 0.05, − 0.539 to − 0.002, Fig. 2D) were significantly higher in women versus men with HFpEF.
Discussion
In this study, our main findings were (1) decreased levels of miR-34a, -224 and -452 in diabetes patients with LVDD and in female diabetes patients with an eGFR < 60 ml/min but increased plasma miR-224 and miR-452 in diabetic women with HFpEF versus diabetic men with HFpEF; (2) regression analysis demonstrated that sex, DM and renal dysfunction are associated with plasma miR-34a levels in patients with LVDD; and (3) Increased levels of plasma Ang-2 in diabetic women with HFpEF but not in diabetic men with HFpEF.
MiRs are extensively involved in manifestations of microvascular injury following type 2 DM14. In the setting of HFpEF, the X-linked miR-545-5p differentiated HFpEF patients from healthy controls15 while X-linked miR-221 distinguished HFpEF patients from patients with heart failure with a reduced ejection fraction (HFrEF)16. Nonetheless, statistical analysis of these miR expression results were not stratified for women and men, and the identified miRs were not related to molecular pathways involved in microvascular injury17. In this study, plasma miR-34a levels were decreased in diabetic patients with LVDD, while miR-34a, -224 and -452 were decreased in diabetic women with LVDD and an eGFR < 60 ml/min. In contrast, miR-34a was increased in diabetic women with HFpEF (although non-significant) while miR-224 and -452 were increased in diabetic HFpEF women versus men. This dichotomous outcome in plasma miR-34a levels could indicate different pathophysiological mechanisms of plasma miR release in different phenotypes of diastolic dysfunction. This was previously demonstrated with plasma miRs following different stages of cardiomyocyte remodeling in patients with aortic stenosis18. It could also indicate that different stages of diastolic dysfunction change the distribution of circulating miRs among plasma carriers like high density lipoprotein (HDL), extracellular vesicles and plasma Argonaute-2 protein, like we previously demonstrated following a phenotypic progression from DM to diabetic nephropathy19. Therefore, instead of the overall absolute quantity of total plasma miRs, a specific difference in the distribution of miRs among these carriers could potentially provide a better explanation for this dichotomous trend and its relationship to microvascular injury in diastolic dysfunction. Still, regression analysis in this study identified that sex was found to be a statistically significant determinant of plasma miR-34a in LVDD patients. This could potentially explain the observed increase in women as compared to men with HFpEF and suggests a similar sex specific plasma expression pattern as was previously shown for miR-34a20. Nonetheless, it could also very well be that the small sample size of diabetic women with LVDD (n = 10) has led to his differential expression of plasma miRs. Therefore, additional well powered studies are needed to investigate sex differences in plasma miR trends in different stages of diastolic dysfunction.
In this study we observed that women with asymptomatic LVDD as well as diabetic women with HFpEF had higher plasma Ang-2 levels, a finding not present in diabetic women with LVDD. Again, this could be related to the relatively small cohort size of diabetic women with LVDD (n = 10). Still, higher levels of plasma Ang-2 in the total cohort of LVDD patients and controls (n = 366) were modestly associated with miR-34a which could indicate a possible relevance of this marker for microvascular injury in these patients with LVDD. Higher plasma Ang-2 levels, indicating an association with microvascular injury in HFpEF women, is consistent with studies that demonstrated that coronary microvascular dysfunction is a female specific pathophysiology in HFpEF21,22. In addition, significantly higher plasma levels of miR-224 and -452 were seen in HFpEF women compared to HFpEF men. It could very well be that the X-chromosome origin of both miRs is associated with a differential expression in women only. Previously we reviewed that particularly X-chromosome located miRs instigate microvascular injury phenotypes which could explain why both miRs were higher in HFpEF women together with higher levels of the microvascular injury marker Ang-29. However additional validation studies are necessary to evaluate this potential.
Of the identified plasma miRs in this study, miR-34a is predominantly secreted by adipocytes and promotes a systemic inflammatory state23. Interestingly, this miR has a well-established myocardial function in women because a targeted myocardial therapy with miR-34a in murine models of myocardial hypertrophy was previously found to reduce cardiac fibrosis and improved cardiac contractility in female mice24. More evidence for sex-specific downstream effects of this particular miR comes from the fact that it regulates the expression of the long-noncoding RNA X-inactive-specific transcript (XIST), which regulates X-chromosome inactivation in female cells25. In down regulating the expression of XIST (which normally mediates X-chromosome inactivation), miR-34a could increase the expression of both miR-224 and -452 which are located on a chromosomal cluster on the X-chromosome (source miRBase version 22). Of the X-linked miR-224/452 cluster, which is also predominantly expressed in adipose tissue26, miR-224 was increased in our pilot study in women with asymptomatic LVDD (Supplemental Figure 1A) and in diabetic women with HFpEF versus HFpEF diabetic men, while both miRs were decreased in women with an eGFR < 60 ml/min and the presence of LVDD (Fig. 2D,E). Regarding miR-224, this miR is known for regulating adipocyte differentiation27, inflammation28, and (micro)vascular quiescence or activation29. Also miR-452 has a role in metabolism and inflammation because hyperglycemia regulates miR-452 expression30 and its adipocyte-specific decrease activates a TNF-α induced inflammatory response31. However, more studies are needed to investigate whether these miRs pinpoint adipocyte dysfunction as a co-contributor to microvascular injury in diabetic women with LVDD or HFpEF.
In this study we measured Ang-2 as marker of microvascular injury in patients with HFpEF and LVDD. However, Ang-2 is a single protein biomarker which may not be able to capture (microvascular) disease variability in patient populations. Therefore, additional studies are needed to assess additional parameters of endothelial and microvascular function to confirm the presence of microvascular injury over the phenotypic progression from LVDD to HFpEF. Alternatively, a comparative analysis of circulating non-coding RNAs and other protein biomarkers could potentially better capture the different molecular characteristics at the endothelial and cardiomyocyte level upon a systemic inflammation induced microvascular injury phenotype. An interesting approach for such a comparative analysis would be to measure the miR-224/452 cluster and Pentraxin-3, a miR-224 target, involved in the innate immune- and inflammatory response32, produced in the coronary microcirculation and altered upon left ventricular (LV) diastolic dysfunction in patients with HFpEF33. Such an approach might be further strengthened by adding the measurement of miR-34a, that regulates cardiac contractile function34, and its gene target Bcl-2 which is pro-fibrotic and known to be involved in the myocardial structural abnormalities of HFpEF as well35. This could clarify whether the identified plasma miRs in this study indeed pinpoint to adipocyte dysfunction as a pathophysiological substrate for endothelial dysfunction and microvascular injury in (female) patients HFpEF and LVDD.
Materials and methods
Ethics and approval
This study complied with the ethical principles of the Declaration of Helsinki and was conducted following approval by the Institutional Review Board of the Maastricht University Medical Center (MUMC), Utrecht University Medical Center (UMCU) and the Leiden University Medical Center (LUMC). All patients provided written informed consent.
Study designs
Maastricht study
Women with a history of preeclampsia (PE) were evaluated routinely for cardiovascular function at approximately 1 year postpartum. For this study, those women who were at least 4 years postpartum were invited by mail to participate in a second follow-up cardiovascular assessment. PE was diagnosed according to the criteria set by the International Society of Hypertension in Pregnancy: new-onset hypertension, systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg, after 20 weeks’ gestation and proteinuria exceeding 0.3 g/day36.
HELPFul study
Study design and procedures of the “Discovery of biomarkers for the presence and progression of left ventricular diastolic dysfunction and HEart faiLure with Preserved ejection Fraction in patients at risk for cardiovascular disease” (HELPFul) study have been published in more detail11. Briefly, HELPFul is a Dutch case-cohort in which patients from the UMCU participated who were referred by their GP for a diagnostic cardiac assessment. Patients who had a previous cardiac intervention, or who were known with congenital cardiac disease were excluded from participation. Patients that had a ratio of the peak early (E) diastolic filling velocity and early diastolic mitral annular velocity (e′) (average of septal and lateral) (E/e′) ≥ 8 with tissue Doppler echocardiography were considered to have a higher probability of having LVDD. ‘Cohort’ patients were randomly sampled from all patients aged 45 years or older, striving to include 25% of eligible participants. Information on co-morbidities, medical history, and medication use was collected. The diagnostic work-up further consisted of physical examination, blood testing of standard cardiovascular biomarkers, electrocardiogram (ECG), bicycle exercise-ECG, and transthoracic echocardiogram. A structured case record form was used to assess symptoms suggestive of cardiac pathology. Hypertension was determined by (1) self-reporting, (2) use of blood pressure lowering medication, or (3) a mean (of at least two measurements) systolic blood pressure > 140 mmHg at the outpatient center. Type 2 diabetes was determined by self-reporting or use of blood glucose lowering medication. Hypercholesterolemia was determined by self-reporting or use of lipid-lowering medication. Atrial fibrillation was determined by self-reporting or atrial fibrillation on ECG at the outpatient center. Body mass index (BMI) was calculated from dividing weight (kg) by squared height in meters (m2). Waist to hip ratio was calculated from dividing waist circumference (cm) by hip circumference (cm). The estimated glomerular filtration rate (eGFR) was calculated from both creatinine and cystatin-c with the validated CKD-EPI formula37.
UHFO-DM study
UHFO-DM is a prospective diagnostic efficiency study from the UMCU38. Patients aged 60 years and over with diabetes type 2, enlisted with the diabetes service of the Center for Diagnostic Support in Primary Care (SHL), Etten-Leur were eligible. This was a representative sample of all patients with diabetes type 2 registered with a general practitioner. The standard care of the diabetes service consists of periodically serum glucose and HbA1c assessment and yearly monitoring of other laboratory parameters and fundoscopy, to help the general practitioners with the management of patients with diabetes. Furthermore, the SHL provides a supporting service to the general practitioners of diabetic nurses, who work according to the current diabetes guidelines. In total 561 general practitioners in the region make use of the services of the Diabetic service of the SHL, with 48,175 patients with type 2 diabetes enlisted in the SHL service. In total, 100 nurse practitioners from the SHL support more than 200 general practitioners (GPs) in their work for diabetic patients. A random sample of approximately 1,200 patients were enlisted within the SHL diabetic service database and when living within 60 km of the cardiology outpatient department of the Oosterschelde hospital in Goes they were asked to participate in the study. To prevent duplicate investigations, patients known with a cardiologist-confirmed diagnosis of heart failure, were only asked to fill out the questionnaires. They also were asked for permission to scrutinize their medical files for co-morbidities and date of diagnosis of heart failure.
Echocardiography
Echocardiography measurements were carried out as previously described13 and performed in accordance with the recommendation of the American Society of Echocardiography (ASE)39. Echocardiographic measurements were made using a phased‐array echocardiographic Doppler system (Vivid 7, GE Vingmed Ultrasound, Horten, Norway). Left ventricular end‐diastolic (LVEDd), end‐systolic (LVESd) diameters (mm), end‐diastolic interventricular septum thickness (IVST; mm) and the posterior (inferolateral) wall thickness (PWT; mm) were measured using the M‐mode in the parasternal long‐axis view. Left ventricular mass (LVM; g) was determined using the formula 0.8 × (1.04((LVEDd + PWT + IVST)3 − (LVEDd)3)) + 0.6, indexed for body surface area40. Relative wall thickness (RWT) was computed using the formula (2 × PWT)/LVEDd)40. Left ventricular end‐diastolic (LVEDV, mL) and end‐systolic (LVESV, mL) volumes were determined using the Teichholz formula41. Heart rate (HR, bpm) was calculated by multiplying by 60 the reciprocal of the mean of five consecutive RR intervals on the electrocardiogram while ((LVEDV – LVESV)/(LVEDV)) × 100 was used to calculate left ventricular ejection fraction (LVEF, %). Stroke volume (SV, mL) was computed by taking the product of VTI and mid‐systolic cross‐sectional area (cm2) at the level of the left ventricular outflow tract in the parasternal long‐axis view. Mean aortic velocity time integral (VTI, cm) was calculated by averaging the outer edge tracings of five consecutive continuous wave Doppler registrations of the left ventricular outflow tract velocity. Cardiac output (CO, L/min) was calculated by multiplying SV by HR. The E/A ratio is the ratio of the early (E) to late (A) ventricular filling velocities while E/E’ is the ratio of mitral peak velocity of early filling (E) to early diastolic mitral annular velocity (E'). Using tissue doppler (TD), early (e') diastolic velocities were assessed at the septal and lateral insertion of the annulus of mitral valve. Assessments were executed offline using EchoPAC PC SW (GE Vingmed Ultrasound) version 6.1.2.
Adjudication of diagnosis of asymptomatic LVDD (Maastricht study), LVDD (HELPFul study) and HFpEF (UHFO-DM study)
Maastricht study
Asymptomatic LVDD (heart failure stage B) was diagnosed according to the guidelines of the American Heart Association42. Asymptomatic LVDD was defined as the presence of previous myocardial infarction, LV hypertrophy (left ventricular mass index (LVMi) > 95 g/m2), concentric remodeling (RWT > 0.42 and LVMi ≤ 95 g/m2), mildly impaired LVEF (> 40% and < 55%) or asymptomatic valvular disease40 . We defined asymptomatic valvular disease as mild aortic valve insufficiency or central aortic valve insufficiency. HF with preserved ejection fraction (HFpEF) in this subclinical stage was defined as LVEF ≥ 55% but with the occurrence of one of the other criteria for asymptomatic LVDD40.
HELPFul study
We applied consensus diagnosis for LVDD with an expert panel consisting of cardiologists (RM, MJC, AT) and a general practitioner specialized in heart failure (FR). This method is comparable to previous studies43,44. The expert panel used all available diagnostic information, including patient reported symptoms, risk factors, electrocardiography, echocardiography, results from the exercise test, (cardiovascular) medication use and plasma B-type natriuretic (BNP) levels. The panel based the diagnosis of LVDD on available diastolic function criteria and recommended cut-points of recent international guidelines45–47. The panel categorized patients into four groups; no LVDD, possible LVDD, probable LVDD, and definite LVDD. For the purpose of this study, we combined probable LVDD with definite LVDD into ‘LVDD’, and no LVDD and possible LVDD into ‘no LVDD’.
UHFO-DM study
Presence or absence of HF was determined by an outcome panel consisting of two cardiologists and one GP38. The panel used all available information from the diagnostic work-up, including echocardiography, but except the NT-proBNP results (to prevent incorporation bias pertaining to this particular test). In case of no consensus the majority decision was used. For HFpEF patients had to have echocardiographic diastolic abnormalities in combination with indicative symptoms and signs (that is, peripheral or pulmonary fluid retention or raised jugular venous pressure) of heart failure or indicative symptoms and echocardiographic left ventricular hypertrophy, atrial fibrillation, or anginal complaints.
RNA isolation
Plasma RNA was isolated from 200μL human plasma with 800μL Trizol reagent (Invitrogen, Breda, the Netherlands) using the RNeasy Micro Kit (Qiagen, 1082 Venlo, the Netherlands) as described previously19. Briefly, chloroform was added to the plasma/Trizol mixture and centrifuged for 15 min at 15,000 g. The aqueous phase was combined with 1.5 × the volume of 100% Ethanol, conveyed to a MinElute Spin column (Qiagen) and centrifuged for 15 s at 18.000g. Subsequently the RNA was washed with 700 μL RWT buffer, twice with 500 μL RPE buffer and centrifuged for 15 s at 18000g after the first two washing steps and 2 min at 18,000 g after the last washing step. Finally, RNA was eluted with 15 μL RNase-free water.
MicroRNA profiling
For miR cDNA synthesis, reverse transcription of total RNA was performed using the miR reverse transcription kit (Applied Biosystems, Foster City, CA). cDNA was preamplified using Megaplex PreAmp primers pools according to the protocol of the manufacturer. For the pilot study custom designed megaplex cards were generated to determine the expression of 118 X-chromosome located miRs, 2 Y-chromosome located miRs, a selected set of 48 microvacular injury associated miRNAs8,12 and U6 and miR-16 as controls. Megaplex arrays were run and analyzed on a 7900HT Fast Real-Time PCR System (Applied Biosystems). In the main patient studies, expression of individual miRNAs was detected by dedicated TaqMan qRT-PCR assays as previously described8. After comparison of miR-16 en U6 Ct-values and their respective standard deviation (SD) in asymptomatic LVDD patients, LVDD patients and HFpEF patients, we choose to normalize miR expression results using expression levels of miR-1613.
ELISA
In the Maastricht cohort, plasma soluble Flt-1 (sFlt-1), thrombomodulin (sTM) and Angiopoietin (Ang-2) concentrations were determined by ELISA (R&D System s, Minneapolis, MN and Diaclone Research, Besancon, France) according to the manufacturers’ supplied protocols. In the HELPFul and UHFO-DM cohort plasma Ang-2 concentration was determined by ELISA (R&D System s, Minneapolis, MN and Diaclone Research, Besancon, France) according to the manufacturers’ supplied protocols.
Data analyses
Baseline characteristics are presented as mean ± standard deviation (SD), while non-normally distributed data is presented as median with interquartile range (IQR) and categorical data is presented as frequency with percentage. Differences between groups were compared using a Pearson Chi-square test or a student T-test, depending on the distribution of and type of variable. MiRNA-expression values are presented as mean ± standard error of the mean (SEM) and group differences were assessed using a student’s T-test. To account for the effect of age we also assessed differences of miRNA expression values between groups with one-way analysis of covariance (ANCOVA), adjusting for age. Correlations between variables were calculated using the Spearman rank correlation while p values were adjusted with multiple testing through FDR with Benjamini Hochberg correction. In the linear regression model, a simultaneous method of entry was used in which plasma miRs were selected as dependent variables while age, sex, eGFR, hypertension, diabetes mellitus and obesity as independent variables. A p value < 0.05 was considered to be statistically significant. Data analysis was performed using SPSS version 20.0 (SPSS, Inc., Chicago, IL) and GraphPad Prism, version 5.0 (GraphPad Prism Software, Inc., San Diego, CA).
Supplementary information
Acknowledgements
This work was supported by grants from the Dutch Heart Foundation (Queen of Hearts: Improving diagnosis of CVD in women 2013T084 to A.J.V.Z and B.W.F.); CVON RECONNECT to A.J.V.Z; and the Dutch Kidney Foundation (Innovation grant 14OIP13 to A.J.V.Z, Junior Kolff grant 16OKG16 to R.B.) and The European Fund for the Study of Diabetes (EFSD/BI). The first and second (HELPFul) cohort were made possibly by funding from the Dutch Heart Foundation 2013T084 (Queen of Hearts) and the second author (GV) is supported by Dutch Heart Foundation Grant CVON2014-11 RECONNECT.
Abbreviations
- MiR
MicroRNA
- HFpEF
Heart failure with preserved ejection fraction
- HFrEF
Heart failure with a reduced ejection fraction
- LVDD
Left ventricular diastolic dysfunction
- DM
Diabetes mellitus
- X-linked
X-chromosome located
- XIST
X-inactive-specific transcript
- Ang-2
Angiopoietin-2
- sFlt-1
Plasma soluble Flt-1
- sTM
Plasma soluble thrombomodulin
- PE
Preeclampsia
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- GP
General practitioner
- ECG
Electrocardiogram
- BMI
Body mass index
- GFR
Glomerular filtration rate
- LVEDd
Left ventricular end‐diastolic diameter
- LVESd
Left ventricular end‐systolic diameter
- IVST
Interventricular septum thickness
- PWT
Posterior (inferolateral) wall thickness
- LVM
Left ventricular mass (LVM; g) was determined using the formula
- RWT
Relative wall thickness
- HR
Heart rate
- CO
Cardiac output
- TD
Tissue doppler
Author contributions
B.W.F. contributed to the conception and design of the work; the acquisition, analysis, and interpretation of data, and wrote the manuscript. G.B.V. contributed to the analysis, and interpretation of data. J.M.G.J.D. contributed to the acquisition and interpretation of data. R.M., M.J.C., A.J.T., C.G.D., F.H.R., M.E.A.S., and H.Md.R. contributed to the discussion and reviewed the manuscript. A.J.V.Z. and R.B. reviewed and edited the manuscript and provided final approval of the version to be published. A.J.V.Z. and R.B. are guarantors of this work, had full access to all the data in the study and bear responsibility for the integrity of the data and the accuracy of the data analyses.
Data availability
The datasets generated and analyzed during the current study are available in the tables as provided in this manuscript. Any additional information on the data can be requested from the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-020-70848-8.
References
- 1.Tromp J, et al. Microvascular disease in patients with diabetes with heart failure and reduced ejection versus preserved ejection fraction. Diabetes Care. 2019 doi: 10.2337/dc18-2515. [DOI] [PubMed] [Google Scholar]
- 2.Sandesara PB, et al. The prognostic significance of diabetes and microvascular complications in patients with heart failure with preserved ejection fraction. Diabetes Care. 2018;41:150–155. doi: 10.2337/dc17-0755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lam CS, et al. Sex differences in clinical characteristics and outcomes in elderly patients with heart failure and preserved ejection fraction: the Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circ. Heart Fail. 2012;5:571–578. doi: 10.1161/circheartfailure.112.970061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beale AL, Meyer P, Marwick TH, Lam CSP, Kaye DM. Sex differences in cardiovascular pathophysiology: why women are overrepresented in heart failure with preserved ejection fraction. Circulation. 2018;138:198–205. doi: 10.1161/circulationaha.118.034271. [DOI] [PubMed] [Google Scholar]
- 5.Shah SJ, et al. Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation. 2015;131:269–279. doi: 10.1161/circulationaha.114.010637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kao DP, et al. Characterization of subgroups of heart failure patients with preserved ejection fraction with possible implications for prognosis and treatment response. Eur. J. Heart Fail. 2015;17:925–935. doi: 10.1002/ejhf.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boonman-de Winter LJ, et al. High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia. 2012;55:2154–2162. doi: 10.1007/s00125-012-2579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bijkerk R, et al. Circulating microRNAs associate with diabetic nephropathy and systemic microvascular damage and normalize after simultaneous pancreas-kidney transplantation. Am. J. Transpl. 2015;15:1081–1090. doi: 10.1111/ajt.13072. [DOI] [PubMed] [Google Scholar]
- 9.Florijn BW, Bijkerk R, van der Veer EP, van Zonneveld AJ. Gender and cardiovascular disease: are sex-biased microRNA networks a driving force behind heart failure with preserved ejection fraction in women? Cardiovasc. Res. 2018;114:210–225. doi: 10.1093/cvr/cvx223. [DOI] [PubMed] [Google Scholar]
- 10.Dudink E, et al. Vascular calcification and not arrhythmia in idiopathic atrial fibrillation associates with sex differences in diabetic microvascular injury miRNA profiles. Microrna. 2019;8:127–134. doi: 10.2174/2211536608666181122125208. [DOI] [PubMed] [Google Scholar]
- 11.Valstar GB, et al. Discovery of biomarkers for the presence and progression of left ventricular diastolic dysfunction and HEart faiLure with preserved ejection fraction in patients at risk for cardiovascular disease: rationale and design of the HELPFul case-cohort study in a Dutch cardiology outpatient clinic. BMJ Open. 2019;9:e028408. doi: 10.1136/bmjopen-2018-028408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bijkerk R, et al. Acute rejection after kidney transplantation associates with circulating MicroRNAs and vascular injury. Transpl. Direct. 2017;3:e174. doi: 10.1097/txd.0000000000000699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breetveld NM, et al. Decreased endothelial function and increased subclinical heart failure in women several years after pre-eclampsia. Ultrasound Obstet. Gynecol. 2018;52:196–204. doi: 10.1002/uog.17534. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Y, Sun X, Icli B, Feinberg MW. Emerging roles for micrornas in diabetic microvascular disease: novel targets for therapy. Endocr. Rev. 2017;38:145–168. doi: 10.1210/er.2016-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong LL, et al. Circulating microRNAs in heart failure with reduced and preserved left ventricular ejection fraction. Eur. J. Heart Fail. 2015;17:393–404. doi: 10.1002/ejhf.223. [DOI] [PubMed] [Google Scholar]
- 16.Watson CJ, et al. MicroRNA signatures differentiate preserved from reduced ejection fraction heart failure. Eur. J. Heart Fail. 2015;17:405–415. doi: 10.1002/ejhf.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.microRNAs as part of the puzzle Rech, M., Barandiaran Aizpurua, A., van Empel, V., van Bilsen, M. & Schroen, B. Pathophysiological understanding of HFpEF. Cardiovasc. Res. 2018;114:782–793. doi: 10.1093/cvr/cvy049. [DOI] [PubMed] [Google Scholar]
- 18.Fabiani I, et al. MicroRNAs distribution in different phenotypes of aortic stenosis. Sci. Rep. 2018;8:9953. doi: 10.1038/s41598-018-28246-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Florijn BW, et al. Diabetic nephropathy alters the distribution of circulating angiogenic miRNAs between extracellular vesicles, HDL and Ago-2. Diabetes. 2019 doi: 10.2337/db18-1360. [DOI] [PubMed] [Google Scholar]
- 20.Guo L, Zhang Q, Ma X, Wang J, Liang T. miRNA and mRNA expression analysis reveals potential sex-biased miRNA expression. Sci. Rep. 2017;7:39812. doi: 10.1038/srep39812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taqueti VR, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur. Heart J. 2018;39:840–849. doi: 10.1093/eurheartj/ehx721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nelson MD, Wei J, Bairey Merz CN. Coronary microvascular dysfunction and heart failure with preserved ejection fraction as female-pattern cardiovascular disease: the chicken or the egg? Eur. Heart J. 2018;39:850–852. doi: 10.1093/eurheartj/ehx818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pan Y, et al. Adipocyte-secreted exosomal microRNA-34a inhibits M2 macrophage polarization to promote obesity-induced adipose inflammation. J. Clin. Investig. 2019;129:834–849. doi: 10.1172/jci123069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernardo BC, et al. Sex differences in response to miRNA-34a therapy in mouse models of cardiac disease: identification of sex-, disease- and treatment-regulated miRNAs. J. Physiol. 2016;594:5959–5974. doi: 10.1113/jp272512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shenoda BB, et al. miR-34a-mediated regulation of XIST in female cells under inflammation. J. Pain Res. 2018;11:935–945. doi: 10.2147/jpr.S159458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ludwig N, et al. Distribution of miRNA expression across human tissues. Nucleic Acids Res. 2016;44:3865–3877. doi: 10.1093/nar/gkw116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Wang Y, Wang H, Ma X, Zan L. MicroRNA-224 impairs adipogenic differentiation of bovine preadipocytes by targeting LPL. Mol. Cell Probes. 2019;44:29–36. doi: 10.1016/j.mcp.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 28.Qi R, et al. MicroRNA-224-5p regulates adipocyte apoptosis induced by TNFalpha via controlling NF-kappaB activation. J. Cell Physiol. 2018;233:1236–1246. doi: 10.1002/jcp.25992. [DOI] [PubMed] [Google Scholar]
- 29.Xu HM, Sui FH, Sun MH, Guo GL. Downregulated microRNA-224 aggravates vulnerable atherosclerotic plaques and vascular remodeling in acute coronary syndrome through activation of the TGF-beta/Smad pathway. J. Cell Physiol. 2019;234:2537–2551. doi: 10.1002/jcp.26945. [DOI] [PubMed] [Google Scholar]
- 30.Tryggestad JB, et al. Influence of gestational diabetes mellitus on human umbilical vein endothelial cell miRNA. Clin. Sci. (Lond.) 2016;130:1955–1967. doi: 10.1042/cs20160305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uchiyama T, et al. Intermittent hypoxia up-regulates CCL2, RETN, and TNFalpha mRNAs in adipocytes via down-regulation of miR-452. Int. J. Mol. Sci. 2019;20:10–20. doi: 10.3390/ijms20081960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaess BM, Vasan RS. Heart failure: pentraxin 3-a marker of diastolic dysfunction and HF? Nat. Rev. Cardiol. 2011;8:246–248. doi: 10.1038/nrcardio.2011.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matsubara J, et al. Pentraxin 3 is a new inflammatory marker correlated with left ventricular diastolic dysfunction and heart failure with normal ejection fraction. J. Am. Coll. Cardiol. 2011;57:861–869. doi: 10.1016/j.jacc.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 34.Boon RA, et al. MicroRNA-34a regulates cardiac ageing and function. Nature. 2013;495:107–110. doi: 10.1038/nature11919. [DOI] [PubMed] [Google Scholar]
- 35.Dong S, et al. microRNA-21 promotes cardiac fibrosis and development of heart failure with preserved left ventricular ejection fraction by up-regulating Bcl-2. Int. J. Clin. Exp. Pathol. 2014;7:565–574. [PMC free article] [PubMed] [Google Scholar]
- 36.Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP) Hypertens Pregnancy. 2001;20:IX–XIV. doi: 10.1081/prg-100104165. [DOI] [PubMed] [Google Scholar]
- 37.Inker LA, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 2012;367:20–29. doi: 10.1056/NEJMoa1114248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boonman-de Winter LJ, et al. Early recognition of heart failure in patients with diabetes type 2 in primary care. A prospective diagnostic efficiency study (UHFO-DM2) BMC Public Health. 2009;9:479. doi: 10.1186/1471-2458-9-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–1083. doi: 10.1161/01.cir.58.6.1072. [DOI] [PubMed] [Google Scholar]
- 40.Lang RM, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J. Am. Soc. Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Teichholz LE, Kreulen T, Herman MV, Gorlin R. Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence of absence of asynergy. Am. J. Cardiol. 1976;37:7–11. doi: 10.1016/0002-9149(76)90491-4. [DOI] [PubMed] [Google Scholar]
- 42.Jessup M, et al. 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:1977–2016. doi: 10.1161/circulationaha.109.192064. [DOI] [PubMed] [Google Scholar]
- 43.van Mourik Y, et al. Unrecognized heart failure and chronic obstructive pulmonary disease (COPD) in frail elderly detected through a near-home targeted screening strategy. J. Am. Board Fam. Med. 2014;27:811–821. doi: 10.3122/jabfm.2014.06.140045. [DOI] [PubMed] [Google Scholar]
- 44.van Riet EE, et al. Strategy to recognize and initiate treatment of chronic heart failure in primary care (STRETCH): a cluster randomized trial. BMC Cardiovasc. Disord. 2014;14:1. doi: 10.1186/1471-2261-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagueh SF, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 46.Ponikowski P, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 47.Pieske B, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) Eur. Heart J. 2019;40:3297–3317. doi: 10.1093/eurheartj/ehz641. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analyzed during the current study are available in the tables as provided in this manuscript. Any additional information on the data can be requested from the corresponding author.