Abstract
Background
The 2019 novel coronavirus disease (COVID-19) pandemic has directly and indirectly impacted health care systems, including residency programs. Social distancing, cancellation of elective cases, and staff re-deployment have compromised clinical and academic teaching. We describe the neurosurgical experience at Emory University during the COVID-19 pandemic and the impact of COVID-19-related policies on resident experience.
Methods
We retrospectively reviewed all neurosurgical cases performed at Emory University Hospital between March 16, the day cancellation of elective cases was effective, and April 15, 2020, and the same period in the preceding 3 years. For the study period, we collected the number of cases and their distribution by subspecialty along with total hospital charges.
Results
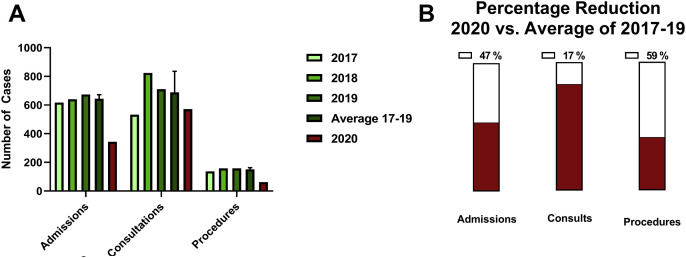
Compared with an average of 606 cases performed during the study period over the past 3 years, only 145 neurosurgical cases were performed between March 16 and April 15, 2020, which corresponds to an 80% reduction in case volume and 66% decrease in hospital revenue in 2020. When divided by subspecialty, the most significant reduction was observed in functional (84%; P < 0.01) followed by spine (78%; P < 0.01) surgery, although all subspecialties were significantly impacted. Assessing junior resident experience, we observed a significant reduction in number of neurosurgical admissions (47%; P < 0.01) and bedside procedures (59%; P < 0.01) in the study period in 2020 compared with the past 3 years, with no significant reduction in number of consultations (17%; P > 0.1).
Conclusions
Even at academic centers that were not hugely impacted by the COVID-19 pandemic, prophylactic and preparedness measures still exhibited an unprecedented toll on neurosurgical resident and fellow experience.
Key words: COVID-19, Neurosurgery training, Pandemic
Abbreviations and Acronyms: ACGME, Accreditation Council for Graduate Medical Education; CNS, Congress of Neurological Surgeons; COVID-19, 2019 novel coronavirus disease; ICU, Intensive care unit; NICU, Neurointensive care unit
Introduction
The severe acute respiratory syndrome coronavirus 2 and resulting 2019 novel coronavirus disease (COVID-19) pandemic have impacted all aspects of life in the United States with the highest toll on the health care system. Early in the outbreak, academic and private medical centers enacted multiple prophylactic measures to mitigate the challenges imposed by an anticipated overwhelming number of patients with COVID-19. The majority of hospitals rescheduled all nonurgent and nonemergent surgeries as recommended by governmental and nongovernmental organizations to spare ventilator use and limit exposure of patients and health care workers to COVID-19.
In addition to the direct impact of COVID-19 itself, these prophylactic measures have imposed an additional burden on health care systems by revenue lost owing to canceled cases and the need to furlough nonessential employees as well as on resident education, especially residents in surgical training including neurosurgery. Reports from institutions at the center of the outbreak have described the impact of the pandemic on residents' experience and education1, 2, 3 and emphasized the need for measures to compensate for lost training experience secondary to COVID-19–related measures. A similar impact has also been noted at institutions with minimal COVID-19 impact including our center. As the pandemic continues, there remains a need for strategic planning from neurosurgical national and institutional leadership to ensure adequate compensatory measures are taken to amend the educational deficit. Quantification of the impact of the pandemic on the actual case volume and resident experience is a critical step toward understanding the magnitude of the deficit as well as the differential impact on various stages of training, different subspecialties, and different training programs. In this report, we provide a detailed quantification of the neurosurgical experience at Emory University (main and midtown campuses) and Grady Memorial Hospital (neurosurgery trauma center) during the COVID-19 pandemic and the impact of COVID-19–related policies on resident education. The experience at Emory University highlights the impact of these policies at a high-volume center that has been less severely affected by the COVID-19 pandemic.
Materials and Methods
All neurological surgery cases performed at Emory University (main and midtown campuses) and Grady Memorial Hospital (neurosurgery trauma center) between March 16 and April 15 during the years 2017–2020 were retrospectively reviewed. The date of March 16 was chosen based on the timing of implementation of COVID-19–related mitigation policies. Cases were grouped by different subspecialties (vascular, tumor, functional, spine, and trauma). The vascular category was further divided into endovascular and open vascular cases. Similarly, the tumor category was subdivided into endoscopic and open surgical cases. All bedside procedures, consultations, and admissions during the same time periods were also reviewed. Hospital charges of all the neurosurgical cases performed during the same period of time in 2017–2020 were obtained from the financial department at Emory. The number of occupied neurological intensive care unit (ICU) beds at midnight each day during the specified study period was examined and noted.
Statistical analyses were performed using GraphPad Prism 8 (GraphPad Software, San Diego, California, USA). Generalized linear models were used to predict expected 2020 case volume by interpolating data from 2017–2019. Univariate analyses were performed using χ2 test for categorical variables and Student t test or analysis of variance for parametric variables. A P value <0.05 was considered statistically significant.
Results
Neurosurgical Case Triage During COVID-19 Outbreak
The decision to reschedule all elective and nonurgent/nonemergent neurosurgical cases at the Department of Neurosurgery at Emory was effective on March 16, 2020, following close monitoring of the COVID-19 outbreak status in Georgia and discussion with hospital leadership. The rationale behind this decision was to preserve ventilators, personal protective equipment, and ICU beds while minimizing the exposure of essential medical staff to COVID-19.
A 4-tier system was implemented to categorize surgical cases based on time sensitivity with the purpose of achieving maximal reduction of case volume without compromising clinical outcome. Tier 1 cases included emergencies that need to be done within 1 hour from presentation. Tier 2 cases included urgent cases that should be done within 24 hours of presentation. Tier 3 cases included time-sensitive cases that need to be done within 4 weeks of diagnosis. Examples of these are patients with high-grade glioma or patients with idiopathic intracranial hypertension and threatened vision. Tier 4 cases included essential surgeries that can be postponed for >1 month. Urgent and emergency cases were posted as usual, and all were able to be accommodated without delay. Preapproval was required from the chairman of the neurosurgery department for all time-sensitive cases to ensure that the above-mentioned criteria were fairly implemented.
Impact of COVID-19 Regulations on Neurosurgical Case Volume
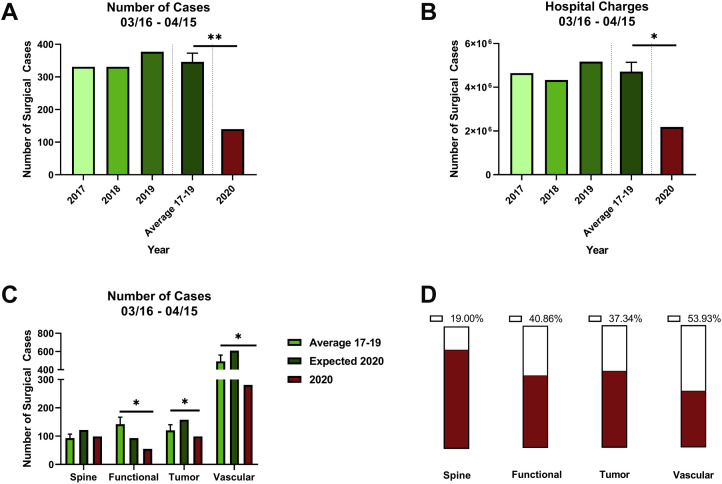
Following the implementation of the 4-tier system, only 145 neurosurgical cases were performed between March 16 and April 15, 2020, at Emory University Hospital and Emory University Hospital Midtown. During the same period in the past 3 years (2017–2019), an average of 606 cases was performed (80% reduction in 2020; P < 0.01) (Figure 1A ). Given the anticipated increase in annual number of cases, the COVID-19 regulations have resulted in an 85% reduction in volume compared with that predicted for 2020 based on general linear models. In parallel to the loss in case volume, the hospital revenue from neurosurgical cases has also significantly decreased from an average of $6.6 million to $2.2 million (66% reduction; P < 0.05) (Figure 1B) as well as 70% reduction compared with the anticipated hospital charges in 2020. At our trauma center (Grady Memorial Hospital), we observed a similar significant reduction in overall case volume (51%) (Figure 1C).
Figure 1.
(A) Number of overall neurosurgical cases at Emory University in 2020 compared with 2017–2019. One-sample t test was used compared 2020 with average of past 3 years. ∗∗P < 0.01. (B) Hospital charges for neurosurgical cases in 2020 compared with 2017–2019. ∗P < 0.01. (C) Distribution of neurosurgical cases by subspecialty for 2020 compared with average of 2017–2019 and the expected case volume in 2020 based on generalized linear model of the past 3 years. One-sample t test was used to compare 2020 with average of past years. ∗P < 0.01. (D) Percentage reduction in case volume per subspecialty. Red bars show proportion of expected cases in 2020 that were actually done.
Impact of COVID-19 Regulations on Subspecialty Experience and Case Volume
All neurosurgical subspecialties have seen significant reduction in case volume secondary to COVID-19 regulations (Figure 1C). Functional neurosurgical cases experienced the highest reduction in case volume (84% reduction) followed by spine (78%), vascular and endovascular (62%), tumor (55%), and trauma (51%) (Figure 1D). These findings are expected given the relatively lower likelihood of spine and functional cases to be emergent or urgent compared with tumor and vascular cases. Examples of functional cases performed during the outbreak included baclofen pump replacements and select neurostimulator generator replacements. Examples of spine cases performed were decompression surgery for cauda equina syndrome and fixation of unstable burst fractures. Trauma cases showed the lowest reduction in case volume over the study period as anticipated given the urgency of these cases.
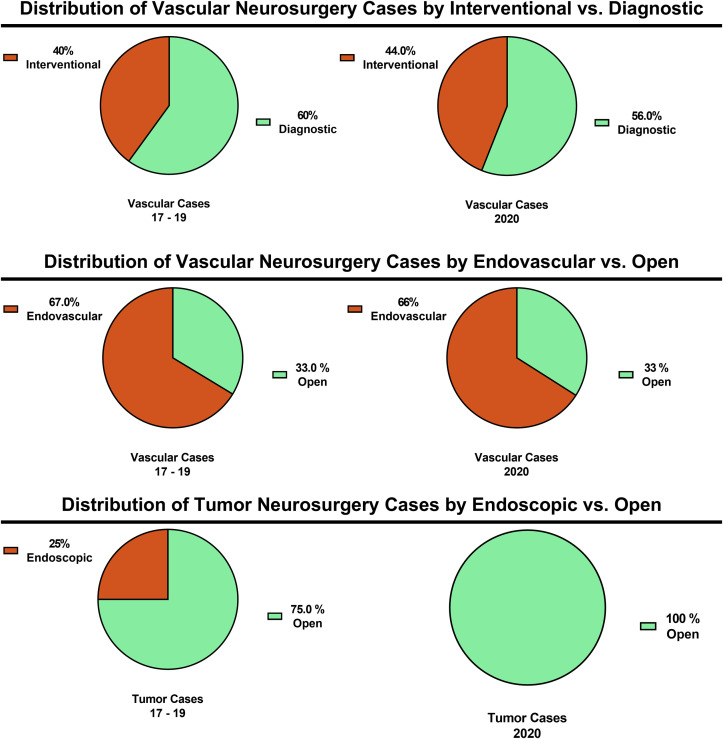
Among cerebrovascular cases, the distribution of cases into diagnostic and interventional was comparable in 2020 to the preceding years 2017–2019 (60% vs. 56% diagnostic; P > 0.1) (Figure 2 ). Similarly, there was no difference in distribution of open and endovascular cases between the 2 study periods (Figure 2). These findings are not surprising given that the decision to pursue open versus endovascular surgery is not based on case urgency.
Figure 2.
Distribution of vascular neurosurgery cases in 2020 compared with 2017–2019 by goal (interventional vs. diagnostic) and type (endovascular vs. open) showing a similar distribution despite downscaling the total case volume. Distribution of tumor cases by endoscopic and open surgery showing complete cessation of endoscopic procedures.
Among tumor cases, no endoscopic surgeries were performed during the study period in 2020 compared with 15 cases on average in the past 3 years that accounted for 25% of all tumor cases (Figure 2). Given the high risk associated with endoscopic endonasal surgeries4 and the nonurgent nature in most of the patients, these cases all were rescheduled during the study period.
Effect of COVID-19 on Neurosurgical Admissions, Consultations, and Bedside Procedures
Neurosurgical case volume reduction is likely to affect more senior neurosurgical residents. Junior resident experience, although affected, may not be as severely impacted by the reduction of case volume. Another measure of overall junior resident experience is the change in admissions, consultations, and bedside procedures (e.g., external ventricular drains, lumbar drains, lumbar punctures) performed by junior residents during this period. During the study period, the number of neurosurgical admissions at Emory University and Grady Memorial Hospital was 344 compared with an average of 644 in the preceding 3 years (Figure 3A ). We observed a significant reduction in number of neurosurgical admissions (47% reduction) and bedside procedures (59%) in the study period of 2020 compared with the past 3 years. However, the number of consultations was not significantly changed and showed an overall 17% reduction compared with 2017–2019 (χ2 test, P > 0.1) (Figure 3B).
Figure 3.
(A) Number of overall neurosurgical admissions, consultations, and procedures for junior residents at Emory University in 2020 compared with 2017–2018. One-sample t test was used to compare 2020 with average of past 3 years. No significant difference in number of consultations. (B) Percentage reduction in volume of admission, consultations, and procedures. Red bars show proportion of expected volume in 2020 of admissions, consultations, and procedures that actually occurred.
Impact of COVID-19 on Neurointensive Care Unit Occupancy
In parallel to the reduction in neurosurgical case volume, the occupancy of the neurointensive care unit (NICU) also decreased during the study period; however, this reduction was not apparent until 8 days after implementation of COVID-19 protocols owing to the time needed to discharge existing and postoperative patients. We observed a 20% reduction in occupancy of NICU beds during the COVID-19 pandemic compared with 2017–2019 (37 vs. 30 patients; P < 0.01) (Figure 4 ). A lower proportion of neurosurgery patients contributed to the NICU census during the study period in 2020 relative to 2017–2019. In fact, the number of available NICU beds decreased, as part of the NICU was converted to COVID-19 dedicated beds, and the NICU beds were temporarily moved to our preoperative holding area.
Figure 4.
Occupancy in the neurointensive care unit during the study period of 2020 compared with the same period in 2017–2019. Multiple 1-sample t tests. ∗∗P < 0.01. Dashed line represents mean for each group. Student t test for comparison of mean. ∗P < 0.001.
Contingency Plans for Neurosurgical Staff and Residents During the COVID-19 Pandemic
In conjunction with the state-wide measure to maintain social distancing and minimize viral spread, contingency plans were set in place by the different departments including neurosurgery to plan for combating a rapidly growing outbreak. Given the relatively low COVID-19 case volume at Emory and in Georgia in general, the decision was made to plan re-deployment of neurosurgery residents and staff to cover the neurosurgical ICUs if the need arose. This was in response to the need to support the neurocritical care attending physicians, fellows, and advanced practice providers, who were in turn enlisted to support other surgical and medical ICUs when required. The goal was to minimize the loss of neurosurgical experience during the period of the pandemic. In addition, this approach was chosen to maintain the presence of neurosurgical staff and residents, whose experience in emergent procedures and management of neurosurgical patients cannot be replaced by nonneurosurgical staff. Fortunately, all COVID-19 cases remained within the current medical and surgical ICU capacity, and re-deployment of neurosurgery residents was ultimately not needed.
In conjunction with this contingency plan and given the reduction in overall case volume, clinical encounters and patient care were limited to the minimal number of residents, while remaining residents on backup were participating in educational activities, participating in research projects, or studying for the neurosurgical board examinations. Backup residents were readily available to fill any arising need secondary to COVID-19 infection or exposure quarantine. During the study period, 1 postgraduate year 3 resident was quarantined until testing negative and required coverage from a co-resident. The number of advanced practice providers was reduced by half to allow for similar backup. To support the resident team, the majority of neurosurgical faculty also signed up via a survey indicating their willingness to cover for junior residents in case residents were deployed to different services or required to stay home for quarantine. Many volunteered to work in the emergency department, ICUs, or labor and delivery, but were not needed.
Educational Activities During COVID-19 Pandemic
Weekly morbidity and mortality conferences have been held virtually via Zoom teleconferencing and included both live presentations from speakers at Emory and presentations from the Congress of Neurological Surgeons (CNS) virtual lectures. Additionally, COVID-19–related educational activities were hosted in conjunction with the neurocritical care team for all faculty, residents, and staff as described before.5 Specialty-specific conferences included virtual spine conferences, tumor boards, stroke conferences, and neuropathology conferences that were held by Zoom teleconferencing.
New Admissions and Perioperative Considerations
Given cessation of all elective surgeries, new admissions during the COVID-19 pandemic were limited to patients admitted from the emergency department or patients directly admitted to the NICU. These patients were considered patients under investigation for COVID-19 until proven otherwise. Any medical personnel that needed to be in direct contact with these patients were required to wear full personal protective equipment (N95 mask, surgical hair cover, eye goggles, gloves, gown), and COVID-19 testing was then performed, including either rapid testing (Sofia SARS Antigen Fluorescent Immunoassay; Quidel Corporation, San Diego, California, USA) or polymerase chain reaction–based tests (in-house test at Emory University Hospital). In cases of patients expected to undergo an invasive procedure or surgery, polymerase chain reaction testing was done as a confirmatory test for the patients testing negative on rapid testing.
For all urgent/time-sensitive cases in which patients were admitted through the emergency department or NICU, the patients underwent both rapid and polymerase chain reaction COVID-19 testing. Rapid testing was usually done for emergency cases. Ambulatory patients considered time-sensitive cases were always tested for COVID-19 if they were symptomatic, and most were tested if they were to have an inpatient stay after surgery. All patients (including COVID-19–negative/asymptomatic patients) were intubated by anesthesia in the operating room where surgery was scheduled 15 minutes before other medical personnel including neurosurgery residents were allowed to enter the operating room. This was hypothesized to allow time for air exchange in the operating room to reduce risk of exposure to aerosolized droplets from the intubation process. Similarly, during extubation, all medical personnel left the room except for the anesthesia team, who donned appropriate personal protective equipment for extubation. Neurosurgery residents participating in cases where patients tested negative for the virus were allowed to wear regular surgical masks, but were provided with N-95 masks if they preferred. The implemented university-wide protocol was that all COVID-19–positive patients were supposed to be intubated in a negative pressure operating room, which is reserved only for this purpose before transferring the patient to the reserved operation room. Extubation was required to be done in the same manner. Notably, no COVID-19–positive patient required a neurosurgical intervention through the period described in this report.
Discussion
The impact of the COVID-19 pandemic on health care systems, including residency programs, has been unprecedented and imposes new challenges to program and departmental leadership. As the COVID-19 outbreak progresses in the United States and in preparation for measures to mitigate the educational and financial deficits, it is important to quantify the impact of the COVID-19 pandemic and its related measures on neurosurgical case volume, hospital charges, and resident experience. In this article, we describe the impact of COVID-19–related measures on neurosurgical experience at a high-volume neurosurgical center that was not overwhelmed with COVID-19 cases. Despite the lack of need to use neurosurgical beds for patients with COVID-19, the measures to prepare for the outbreak and preserve critical medical staff resulted in an unprecedented reduction in case volume to less than a quarter of that in prior years. This was associated with a significant reduction in hospital charges as well as a decrease in resident neurosurgical experience.
With the steep decrease in the number of elective cases, admissions, and bedside procedures, there has been a significant educational and clinical gap that is likely to impact the ability to meet Accreditation Council for Graduate Medical Education (ACGME) requirements by residents, especially residents at more senior years. However, junior and senior residents as well as fellows all are impacted by these losses. Reduction in case volume, especially complex and elective cases, has decreased the experience of fellowship trainees, especially in both functional and spine neurosurgery, the 2 subspecialties that were most impacted by case cancellation. Tumor fellows, specifically individuals training on endoscopic endonasal approaches, were also among the most impacted given the cessation of these procedures early during the outbreak, as they posed a very high risk of viral transmission during disruption of the nasal mucosa intraoperatively. At Emory during the study period, no endoscopic transsphenoidal adenectomies were performed (Figure 2). However, these procedures have been resumed as of April 23, 2020, as reliable testing is feasible, and patients can be tested before surgery. Similarly, reduction in overall case volumes across subspecialties has an equally high toll on senior and chief residents who have limited experience during 20% of their senior year. Residency programs with modular schedules during which residents spend dedicated periods of time across different subspecialties (e.g., pediatrics, endovascular) may experience a differential impact of reduction in case volume even among residents of the same year. The increased availability of COVID-19 testing at our institution and nationally and its implementation in preoperative settings have led to an increase in the number of time-sensitive and select elective cases. This is likely to help prevent worsening of the deficit in operative experience over the upcoming months.
At a more junior level, reduction in total patient census and number of bedside procedures may result in delay in acquisition of independent management and procedural skills. However, these gaps can still be sealed during upcoming years, especially if the gaps are recognized early and strategies to alleviate them are implemented in a timely manner. Efforts from neurosurgical departments as well as neurosurgery leadership societies to implement educational activities via lectures and virtual conferences are highly commended. However, these measures still fall short when it comes to surgical hands-on experience missed by residents.
Another important factor to consider is hospital revenue. This unprecedented and unanticipated loss in two thirds of institutional revenue has imposed significant financial challenges that are likely to impact both residents and staff and add another burden on program leadership. This is likely to result in a cut in departmental spending, which may impact maintaining full staffing as well as limiting spending on educational activities.
Conclusions
The impact of the COVID-19 pandemic on neurosurgical experience has been significant even in regions not severely impacted by the outbreak. The reduction in neurosurgical case volume is likely to continue and not recover fully at least in the foreseeable future. Given the impact the pandemic has already imposed and that it is expected to continue to affect neurosurgical resident experience and institutional financial support, strategic planning based on quantification as described in this article is necessary to help mitigate further losses and compensate for lost opportunities. With respect to resident experience, alternative education modalities, including daily virtual didactic lectures about surgical topics and nuances, should be implemented. Simulation laboratories and use of virtual reality platforms may also provide a unique opportunity to help develop technical and anatomic skills. Equally important during these times is consideration of the significant stress the pandemic may cause at the personal level. The availability of stress management and mental health support sessions at institutions will play a significant role in limiting its impact.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Hassan Saad and Ali Alawieh are co–first authors.
References
- 1.Clark V.E. Impact of COVID-19 on neurosurgery resident research training. https://doi.org/10.3171/2020.4.JNS201034 [e-pub ahead of print]. J Neurosurg. accessed May 9, 2020. [DOI] [PMC free article] [PubMed]
- 2.Ammar A., Stock A.D., Holland R., Gelfand Y., Altschul D. Managing a specialty service during the COVID-19 crisis. https://doi.org/10.1097/ACM.0000000000003440 [e-pub ahead of print]. Acad Med. accessed May 10, 2020. [DOI] [PMC free article] [PubMed]
- 3.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: Adaptation under fire: Two Harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery. 2020;87:E173–E177. doi: 10.1093/neuros/nyaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel Z.M., Fernandez-Miranda J., Hwang P.H. In Reply: Precautions for endoscopic transnasal skull base surgery during the COVID-19 Pandemic. Neurosurgery. 2020;87:E160–E161. doi: 10.1093/neuros/nyaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bray D.P., Stricsek G.P., Malcolm J. Letter: Maintaining neurosurgical resident education and safety during the COVID-19 pandemic. Neurosurgery. 2020;87:E189–E191. doi: 10.1093/neuros/nyaa164. [DOI] [PMC free article] [PubMed] [Google Scholar]