Abstract
The novel coronavirus COVID-19 was first identified in China in December 2019. Its spread resulted in a pandemic, with the United Kingdom entering a period of national lockdown on 23 March 2020 to reduce disease burden on the National Health Service (NHS). King’s College Hospital is a Major Trauma Centre serving an inner-city population of 700,000 with 120,000 patients attending the emergency department (ED) annually. We aimed to determine the effect of lockdown on OMFS trauma presentations and lessons learned from emergency service provision during a pandemic. All referrals to the oral and maxillofacial surgical (OMFS) team from ED during the first six weeks of the lockdown period – 23 March 2020 - 3 May 2020 – were compared with the same six-week period in 2019. A total of 111 referrals were made to OMFS during the first six weeks of the lockdown period in 2020 compared with 380 referrals in 2019. Of these, 50.5%, (n = 192) were related to facial trauma in 2019 vs (63.1%, n = 70) in 2020. Fewer patients were admitted under OMFS: 17.4% (n = 35) in 2019 vs 2.9% (n = 2) in 2020, and a greater number of patients were discharged from OMFS care directly from the ED: 63.2% (n = 127) in 2019 vs 82.9% (n = 58) in 2020. There was profound effect of the lockdown on referrals to OMFS from the ED, in number and type of diagnosis. This is potentially reflective of the increased availability of acute/emergency dental services in South-East London during the lockdown period. This gives us valuable insight for service planning in the event of further restrictions.
Keywords: Covid, coronavirus, lockdown, Facial trauma
Introduction
The novel coronavirus, COVID-19, first identified in China in December 2019,1 is a highly infective, presumed zoonotic, virus that may cause life-threatening pneumonitis. Its spread has resulted in a global pandemic, with the United Kingdom entering a period of national lockdown on 23 March 2020 in order to reduce the disease burden. This has had a profound impact on the National Health Service (NHS) with regards to patient presentation, staffing levels, and service provision. Oral and maxillofacial surgery (OMFS) is no exception, with the government and World Health Organisation advising surgical specialties to cancel elective operating lists and outpatient clinics, and utilising telehealth options where appropriate.
The emergency department (ED) has remained open to accommodate emergency treatment, and therefore OMFS teams must be prepared to manage any acute presentations that require urgent treatment including emergency airway management, drainage of infections,2 and time-sensitive trauma.
Facial injuries are estimated to account for roughly 5%-10% of all attendances at ED in the United Kingdom,3 and are present in up to 21% of major trauma cases.4 Facial trauma has a significant impact on an individual’s overall physical and psychological health. Epidemiological analysis of maxillofacial injuries is important to identify the trauma burden and to help develop more efficient ways to plan resource allocation and to deliver care and preventative measures.5
King’s College Hospital is a major trauma centre that serves an inner-city population of 700,000,6 with approximately 120,000 patients attending the ED each year. During the severe acute respiratory syndrome (SARS) virus outbreak in Asia in 2003, a busy ED in Taiwan noted a 33.4% decrease in the number of patients attending following the date of the first hospital-associated transmission7 and we would expect to see the same.
Our aim was to determine the effect of the national lockdown on OMFS trauma presentations to our department and highlight the lessons learned from emergency service provision during a pandemic.
Method
We reviewed all referrals to the OMFS team from the ED at King’s College Hospital during the first six weeks of the lockdown period – 23 March 2020 - 3 May 2020. We compared these data with the referrals made the previous year (2019) during the same six-week period. Referral records to OMFS were obtained from the Symphony Electronic Record system (used by the ED), and their electronic patient records reviewed on Sunrise® Clinical Manager (Allscripts). Records were assessed for patient demographics, aetiology and type of trauma, and follow-up. Soft tissue injury was subcategorised into lacerations and contusions (no breach in dermis). Accidental self-harm, such as the patient who had walked into a closed glass door, has been distinguished from deliberate self-harm so these categories could be more fully explored. We have not included referrals made from outside hospitals in this study.
Results
A total of 111 referrals were made to OMFS during the first six weeks of the lockdown period in 2020. A total of 63.1% (n = 70) of these were trauma related, compared with 380 referrals in 2019 when 50.5% (n = 192) were trauma related – a dramatic decrease in overall numbers, but an increase in proportion. The proportion of male to female trauma patients decreased during lockdown from 2.8:1 (n = 141 male, n = 51 female) in 2019 to 1.7:1 (n = 44 male, n = 26 female) in 2020. The age of trauma patients referred increased from a median (range) of 28 (0.7-89) years in 2019 to 34 (1-91) years in 2020.
The proportion of trauma referrals with fractures reduced from 21.9% (n = 42) of total cases in 2019 to 17.1% (n = 12) in 2020. Dental trauma, as a proportion of referrals, increased from 14.6% (n = 28) in 2019 to 17.1% (n = 12) in 2020. However, in the soft tissue category the proportion of lacerations increased from 72.4% (n = 110) in 2019 to 96.1% (n = 49) in 2020 (Table 1 ).
Table 1.
Comparison of type of facial trauma presenting during lockdown in 2020, relative to the same period in 2019. Data are number (%).
| Variables |
2019 |
2020 |
|---|---|---|
| n (%) | n (%) | |
| Total trauma patients | 192 | 70 |
| Bony trauma cases: | ||
| Mandible | 20 (47.6) | 4 (33.3) |
| Midface | 3 (7.1) | 1 (8.3) |
| Nasal bones | 7 (16.7) | 3 (25) |
| Orbit | 8 (19.0) | 1 (8.3) |
| Zygoma | 4 (9.5) | 1 (8.3) |
| Frontal | 0 | 1 (8.3) |
| Styloid process | 0 | 1 (8.3) |
| Bony trauma total | 42 (21.9*) | 12 (17.1*) |
| Dental trauma cases: | ||
| Avulsion | 7 (25) | 5 (41.7) |
| Luxation | 11 (39.3) | 3 (25) |
| Dentoalveolar | 0 | 1 (8.3) |
| Tooth fracture | 10 (35.7) | 3 (25) |
| Dental trauma total | 28 (14.6*) | 12 (17.1*) |
| Soft tissue trauma cases: | ||
| Laceration | 110 (72.4) | 49 (96.1) |
| Contusion | 42 (27.6) | 2 (3.9) |
| Soft tissue trauma total | 152 (79.2*) | 51 (72.8*) |
N.B. Percentages reflect the proportion of subcategory. Mixed type will appear in more than one subcategory. *Percentage reflects proportion of total trauma cases.
The proportion of trauma referrals secondary to interpersonal violence was almost unchanged: 22.9% (n = 44) in 2019 compared with 24.3% (n = 17) during 2020. Referrals involving an aetiology of domestic violence decreased during the 2020 lockdown period from 5.2% (n = 10) in 2019 to 1.4% in 2020 (n = 1). The proportion of patients with trauma related to deliberate self-harm rose from 0% (n = 0) in 2019 to 2.9% (n = 2) in 2020. However, accidental self-harm fell from 8.3% (n = 16) in 2019 to 2.9% (n = 2) in 2020. Referrals related to dog-bites were reduced from 3.1% (n = 6) in 2019 to 0% (n = 0) in 2020. Road traffic incidents increased as a proportion from 9.4% (n = 18) in 2019 to 11.4% (n = 8) in 2020 (Table 2 ).
Table 2.
Comparison of the aetiology of facial trauma in patients presenting during lockdown in 2020 relative to the same period in 2019. Data are number (%).
| Aetiology |
2019 |
2020 |
|---|---|---|
| n (%) | n (%) | |
| Domestic violence | 10 (5.2) | 1 (1.4) |
| Interpersonal violence | 44 (22.9) | 17 (24.3) |
| Road traffic collision | 18 (9.4) | 8 (11.4) |
| Fall | 90 (46.9) | 37 (52.9) |
| Sports related | 8 (4.2) | 3 (4.3) |
| Self-harm – accidental | 16 (8.3) | 2 (2.9) |
| Self-harm – deliberate | 0 | 2 (2.9) |
| Dog-bite | 6 (3.1) | 0 |
| Total | 192 | 70 |
Facial trauma referrals in which patients had a past history of mental health issues increased from 0.5% (n = 1) in 2019 to 10% (n = 7) during the 2020 lockdown.
Referrals concerning intoxicants as notable factors were reduced from 11.5% (n = 22) alcohol and 2.6% drugs (n = 5) in 2019 to 10% associated with alcohol (n = 7) and none with drugs in 2020.
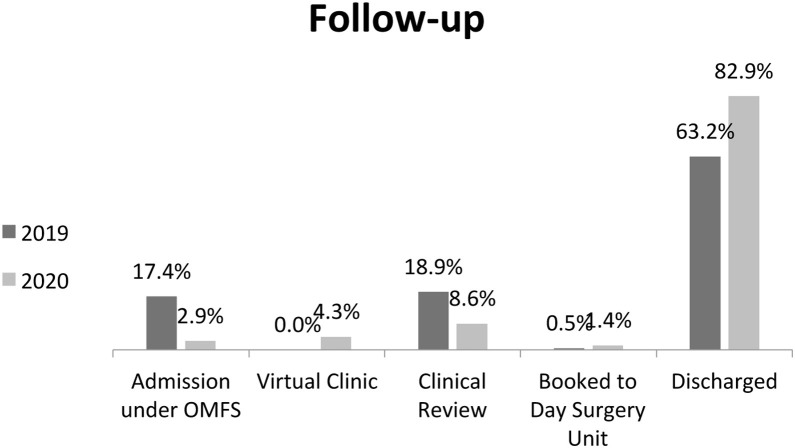
Fewer patients were admitted under OMFS during the 2020 lockdown period: 17.4% (n = 35) in 2019 but only 2.9% (n = 2) in 2020. Fewer patients were given review appointments: 18.9% (n = 38, all face to face) in 2019 as opposed to 12.9% (n = 6 face to face, n = 3 virtual) in 2020. A greater number of patients were discharged from OMFS care directly from the ED during the COVID-19 lockdown period: 63.2% (n = 127) in 2019 and 82.9% (n = 58) in 2020 (Fig. 1 ).
Fig. 1.
Comparison of admissions and follow up for facial trauma presenting during 2020 lockdown relative to the same period in 2019.
Discussion
We chose the same six-week period the previous year (2019) for comparison with the first six weeks of the 2020 lockdown period. At this point all elective operating and non-acute outpatient clinics had been cancelled. As expected, there was a distinct drop in referrals from the ED to OMFS, which is likely to reflect overall fewer presentations to the ED and a strong ‘stay at home’ message from the Government and in the media.
The proportion of trauma related referrals to OMFS increased. This is a potential reflection of the increased availability of acute/emergency dental services in South East London instituted early in the lockdown period with a six-day Acute Dental Service operating at King’s College Hospital, usually five-day, and intensified dental triage to the Queen Mary, Sidcup site taking these patients.
The overall proportion and number of referrals for facial fractures reduced, this lessened the pressure on the service to find emergency or semi-elective trauma operating space for these patients. Dental trauma fell in overall numbers but increased in proportion. Although it would be reasonable to expect that the incidence of dental injury reduced due to lockdown, some of the simpler cases will have been triaged to the Acute Dental Service for management. The proportion of soft-tissue lacerations subcategory increased significantly, potentially reflecting patients’ desire not to present to ED for more simple injuries such as bruising and swelling (soft-tissue contusions). This demonstrates that these OMFS specialist services are still required.
Trauma referrals with interpersonal violence aetiology did not appear to be particularly affected, perhaps surprisingly, as we might expect this to reduce with social distancing measures in place. In addition, we found that the proportion of trauma referrals related to domestic violence fell, when we might have expected them to rise during a period of domestic confinement. As clinicians, we must be mindful not to become complacent as this may represent increased difficulty of opportunity to access services rather than a true reduction.
The number of trauma referrals for dog-bites reduced – potentially reflecting the avoidance of dogs not belonging to the immediate household.
Accidental self-harm referrals reduced. We had hypothesised that home improvement accidents may be a factor here, but we could not demonstrate this from our findings, although one of the two cases was a branch-related injury while gardening. We may consider that less walking on the street with a distracting phone in hand may have played a role!
Referrals where patients had deliberately self-harmed and/or had a history of mental health issues increased during lockdown potentially reflecting the exacerbating nature of heightened social anxiety and the interruption to regular mental health services.
Reduced involvement of intoxicants during lockdown may be reflective of increased social distancing as public houses, restaurants, and nightclubs have been closed, and supply chains have been interrupted.
The number of patients admitted under OMFS during the 2020 lockdown period fell, fewer patients were given a review appointment and the proportion of patients discharged increased. In addition, some of the reviews were virtual (via telephone); a new development in 2020. This is potentially because they were seen by a more senior clinician earlier, due to the on-call consultant and registrar being more readily available due to reduction in overall referrals and operating, and a definitive decision made in the ED rather than a ‘just in case’ clinic review appointment given. A more conservative approach to admission and treatment of trauma cases was also adopted to minimise the strain on resources and reduce potential exposure to coronavirus through high risk aerosol generating procedures, as advocated by the experience of our European colleagues.8, 9 Trauma cases requiring operations were increasingly managed in day surgery settings.
Conclusion
We can see clearly from this study the profound effect of the lockdown period on the referrals to OMFS from the ED, both in number and type of diagnosis. This gives us valuable insight for service and workforce planning in the event of future further periods of restrictions, for example, when releasing staff for redeployment to support other high demand areas such as critical care. OMFS specialist services were still required for fracture, dental injury, and soft tissue management, so a baseline staff would still need to be retained.
Moving forward – it would also be extremely useful to analyse how the flow of emergency referrals for dental infection have been managed in order to improve the patient pathway for these in more typical times, and around traditional pressure times such as the Christmas and New Year period. Our findings regarding an apparent reduction in domestic violence are counterintuitive and we should be aware that this is potentially due to the inability of patients to attend.
Conflict of interest
We have no conflicts of interest.
Ethics statement/confirmation of patients’ permission
This project does not require ethics approval. There are no identifiable patient details.
Acknowledgements
With thanks to Holly Boyes, James Olding, Matthew Proctor, Sieuming Ng, and Harmony Ubhi for their valuable assistance with this project.
References
- 1.Yang Y., Soh H.Y., Cai Z.G., et al. Experience of diagnosing and managing patients in oral maxillofacial surgery during the prevention and control period of the new coronavirus pneumonia. Chin J Dent Res. 2020;23:57–62. doi: 10.3290/j.cjdr.a44339. [DOI] [PubMed] [Google Scholar]
- 2.Bali R.K., Chaudhry K. Maxillofacial surgery and COVID-19, the pandemic!! J Maxillofac Oral Surg. 2020;19:159–161. doi: 10.1007/s12663-020-01361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davies R., Hammond D., Ridout F., et al. British Association of Oral and Maxillofacial Surgeons’ National Facial Injury Surveys: hard tissue facial injuries presenting to UK emergency departments. Br J Oral Maxillofac Surg. 2020;58:152–157. doi: 10.1016/j.bjoms.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 4.McGoldrick D.M., Fragoso-Iñiguez M., Lawrence T., et al. Maxillofacial injuries in patients with major trauma. Br J Oral Maxillofac Surg. 2018;56:496–500. doi: 10.1016/j.bjoms.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Boffano P., Roccia F., Zavattero E., et al. European Maxillofacial Trauma (EURMAT) project: a multicentre and prospective study. J Craniomaxillofac Surg. 2015;43:62–70. doi: 10.1016/j.jcms.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Olding J., Olding C., Bew D., et al. Penetrating head & neck trauma – epidemiology and injury characteristics in terror-related violence, interpersonal violence and deliberate self-harm at a level 1 trauma centre. Surgeon. 2019;17:133–138. doi: 10.1016/j.surge.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Chen W.K., Cheng Y.C., Chung Y.T., et al. The impact of the SARS outbreak on an urban emergency department in Taiwan. Med Care. 2005;43:168–172. doi: 10.1097/00005650-200502000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Allevi F., Dionisio A., Baciliero U., et al. Impact of COVID-19 epidemic on maxillofacial surgery in Italy. Br J Oral Maxillofac Surg. 2020;58:692–697. doi: 10.1016/j.bjoms.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg. 2020;48:521–526. doi: 10.1016/j.jcms.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]