Abstract
Aim
Influenza vaccination is the most effective method in prevention of influenza disease and its complications. Our study aimed to investigate the rates of vaccination and the behaviours and attitudes against the vaccine in healthcare workers in Turkey.
Methods
This multicentre national survey is a descriptive study in which 12 475 healthcare workers. Healthcare workers were asked to answer the questionnaire consisting of 12 questions via the survey.
Results
It was found that 6.7% of the healthcare workers regularly got vaccinated each year and that 55% had never had the influenza vaccine before. The biggest obstacle against getting vaccinated was determined as not believing in the necessity of the vaccine (53.1%).
Conclusion
The rates of influenza vaccination in healthcare workers in Turkey are quite low. False knowledge and attitudes on the vaccine and disease are seen as the most important reasons to decline vaccination. It is important to detect reasons for anti‐vaccination and set a course in order to increase the rates of vaccination.
What’s known
Healthcare workers have doubts about the severity of influenza disease and the effectiveness of the vaccine.
Not believing in the effectiveness of vaccine, being afraid of getting ill because of vaccine, or side effects of vaccine why healthcare workers do not want to get the vaccine.
Also anti‐vaccination movement is increasing and that the views against vaccination take a large place especially in media.
What’s new
While the importance of the vaccine was once again understood with the outbreak of COVİD‐19, we believe that especially the wrong information and attitudes towards influenza vaccine can be replaced with the correct campaigns.
As our study is the most extensive study in our country it is important as it puts forward a nation‐wide idea especially about the issues to be emphasised while it increases the national targets of vaccination.
1. INTRODUCTION
Influenza is a highly infective acute viral infection that is transmitted by droplets, that has a short incubation period and is accompanied by systemic symptoms such as fever, shivering, muscle and joint aches, headache and fatigue. 1 According to the data from the Centre for Disease Control and Prevention (CDC), annual number of deaths because of influenza‐associated respiratory diseases was 291 000‐646 000 worldwide between 1999 and 2015. The data suggest that incidence of mortality was the highest in patients older than 65, in children under 5 and in Sub‐Saharan Africa and Southeastern Asia which had low socioeconomic level. 2
Vaccination of healthcare workers who serve as potential vectors in transmission of influenza has been recommended by CDC since 1981. 3 In addition to immunisation, the risk for influenza‐like symptoms and nosocomial infection decreases in healthcare workers and therefore, morbidity and mortality to occur in patients will considerably decrease. As an indirect result of vaccination, no loss of workforce or organisation problems arising from the absence of personnel occur. 1
There is a serious resistance to influenza vaccination in healthcare workers compared with the other vaccines (measles, rubella, mumps, hepatitis B and tuberculosis). 4 Not believing in the effectiveness of vaccine, being afraid of getting ill because of vaccine, or having side effects of vaccine and underestimating the influenza disease are among the reasons why healthcare workers do not want to get the vaccine. 5
Although vaccination has been recommended for healthcare workers and free vaccination has optionally been provided for healthcare workers by the Ministry of Health since 2002 the rates of vaccination are quite low in our country. 6 , 7 This study is the most extensive study in which behaviours and attitudes of healthcare workers on influenza vaccine are investigated. Our study aimed to understand barriers and obstacles against influenza vaccine for healthcare workers and determine the behaviours and attitudes of healthcare workers on the vaccine.
2. MATERIAL AND METHOD
In this descriptive study, 12 475 healthcare workers participated in the multicentre national survey. The questionnaire consisting of 12 questions was sent to the healthcare workers who were from seven large regions of Turkey and Turkish Republic of Northern Cyprus. Online survey was sent to the healthcare employees who wanted to participate in the study, and they were asked to answer the questions about demographic data and their behaviours about vaccine without taking personal informations.
Data were analysed after recorded on SPSS. In the evaluation of the descriptive data; number and percentage (n, %) used for categorical variables; mean, standard deviation, minimum, maximum values were used for numerical variables. Chi‐square test was used to compare categorical data in independent groups. Statistical alpha significance level was accepted as P < .05.
Ethics committee approval for the study was obtained from Izmir Bozyaka Training and Research Hospital (ethics committee number: 08.09.2016/431) and Public Health Institution of Turkey (ethics committee number: 04.05.2016/45202651).
3. RESULTS
A total of 12 475 healthcare workers across Turkey participated in the study. Demographic characteristics and groups of the participants are given in Table 1.
TABLE 1.
Demographic characteristics of the participants
| % (n) | |
|---|---|
| Demographic characteristics | |
| Gender | |
| Male | 35.1 (4376) |
| Female | 64.9 (8099) |
| Total | 100 (12 475) |
| Age (Mean ± SD) (y) | 35.4 ± 9.4 y (16‐76) |
| Educational status | |
| Primary School | 3.0 (369) |
| Secondary School | 6.0 (747) |
| High School | 15.9 (1984) |
| University‐Higher Education | 75.2 (9375) |
| Total | 100 (12 475) |
| Occupational Groups | |
| Physician | |
| Associate Professor‐Professor‐Assistant Professor | 3.2 (398) |
| Specialist Physician | 16.9 (211) |
| Assistant | 6.2 (763) |
| General Practitioner | 4.6 (565) |
| Student/Intern | |
| Med Student | 5.7 (713) |
| Intern student out of medicine | 2.9 (360) |
| Healthcare workers out of physicians | |
| Dentist | 0.4 (54) |
| Pharmacist | 0.7 (85) |
| Nurse‐midwife | 32.2 (4011) |
| Laboratory worker/Medical Technician | |
| Laboratory technician (Microbiology‐Biochemistry‐Pathology) | 3.3 (410) |
| Medical technician (Anaesthesia, Radiology, Nuclear medicine and other units) | 4.1 (508) |
| Cleaning Company Workers | |
| Cleaning worker | 4.6 (575) |
| Worker handling patients | 1.4 (173) |
| Office Worker | |
| Data‐entry clerk | 5.6 (698) |
| Administrative Unit Worker | 2.4 (303) |
| Other | |
| (Psychologist, other medical technician, kitchen, driver, teacher, workers in workshop, security, postgraduate‐doctorate) | 6.0 (742) |
| Total | 100 (12 475) |
The distribution of the participants across Turkey according to regions is given in figure. Most of the participants were from Aegean (22.6%) and Marmara (20.6%) regions (Figure 1).
FIGURE 1.
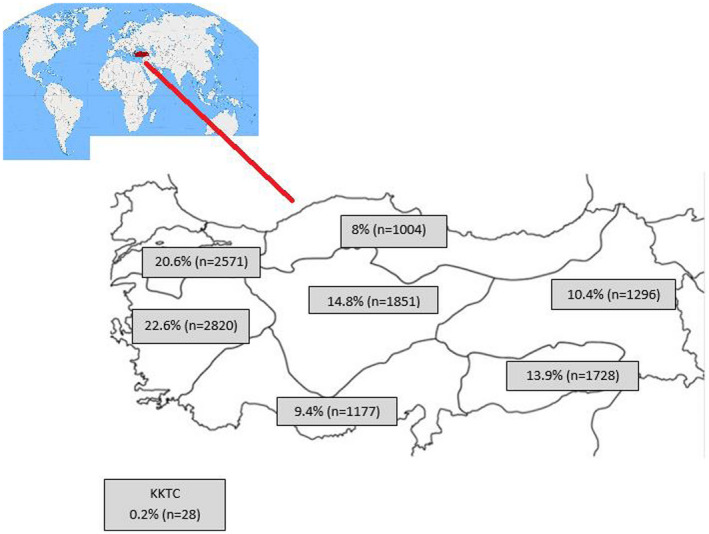
Distribution of participants according to regions
When the influenza vaccination status of the participants was questioned 18% of them did not reply to the question. Out of the participants who replied to the question, 6.7% stated that they regularly got influenza vaccine each year, 18.8% stated that they sometimes got influenza vaccine, 7.5% stated that they got influenza vaccine in case the Ministry of Health sent it and 55% stated that they never got influenza vaccine. The rate of those who did not get the flu vaccine was found statistically significant compared with those who got the flu vaccine. (P < .01) When the vaccination rates among the clinical units were evaluated, no significant difference was found in the vaccination rates between the emergency, internal and surgical units.
The ones who regularly got the influenza vaccine each year were mostly doctors (34%, n = 232) and they were followed by nurse‐midwives with the rate of 31.8% (n = 220). Vaccination rates in doctors were found to be statistically significant compared with nurses and other healthcare professionals. (P < .01) The ones who never got influenza vaccine were mostly nurse‐midwives with the rate of 31.8% (n = 2181).
When the reasons why the individuals got influenza vaccine were analysed (more than one option were marked) the option of getting the vaccine in order not to catch influenza ranked first with 38.9% (n = 1313). It was followed by the option of getting the vaccine in case of a serious outbreak with 13.7% (n = 463) and 9.0% (n = 302) got the vaccine in order to protect his or her child, 8.5% (n = 287) in order to protect the patients, 7.2% (n = 241) in order to avoid pandemic, 6.7% (n = 225) because of the presence of a comorbidity, 1.7% (n = 58) in order to protect their elderly father/mother and 15.0% (n = 507) for other reasons.
The reasons why the individuals who did not get the influenza vaccine are given in Table 2.
TABLE 2.
The reasons why people (n = 6861) decline vaccination
| Reasons a | % (n) |
|---|---|
| I think influenza vaccine is not necessary | 53.1 (3641) |
| It is not mandatory | 23.2 (1591) |
| I have a healthy body and strong immune system | 23.0 (1581) |
| I am afraid of the side effects of the vaccine | 16.2 (1114) |
| I get flu even if I get the flu shot | 16.1 (1103) |
| I do not get flu even if I do not get the flu shot | 9.6 (658) |
| I am against flu vaccination | 8.8 (602) |
| Other reasons | 19.7 (1354) |
More than one reason was marked at the same time.
4. DISCUSSION
Healthcare workers constitute a group that contains all the personnel working at hospital whether or not contacting with patients and that thereby plays a role in transmission and spread of respiratory pathogens. 1 Healthcare workers have doubts about the severity of influenza disease and the effectiveness of the vaccine. Although vaccination is the most effective and a cost‐effective method anti‐vaccination views increasingly become more common and a resistance to vaccination occurs not only in the general population, but also among the healthcare workers. 8
The healthcare workers are unaware how important their role is in the nosocomial spread of the disease. Vaccination of healthcare workers protects them against influenza infection and loss of workforce is also prevented as an indirect effect. In addition, vaccination is prevented from infecting patients and other healthcare professionals. 9 In a study, 41% of 2000 healthcare workers were found to keep serving although they had influenza‐like symptoms. 10 Infected healthcare workers who are immunosuppressed, have chronic diseases or serve to the population in the risk group in terms of complication development cause the disease to spread and thereby lead to serious problems in this patient group. In the study by Ahmed et al, influenza‐like disease symptoms decreased at a rate of 42% and mortality because of influenza decreased at a rate of 29% in case the healthcare workers were vaccinated. 11 In the study by Solay et al from Turkey, the rate of influenza vaccination among healthcare workers was found 12.2% low in 2018‐2019 season. Moreover, in the same study, nosocomial influenza have been diagnosed by 32.2% of the hospitalised patients whose swab samples were taken because of influenza‐like disease. 12 Influenza vaccine is recommended as a more effective method in preventing the nosocomial influenza transmission compared with the other methods such as washing hands and using masks. According to a study conducted by Black et al in the USA, high rates of vaccination in healthcare workers were associated with low incidence rates of influenza cases. 13
A variety of vaccination programmes are implemented for vaccination of healthcare workers, however, the rates of vaccination may differ from country to country and from continent to continent because of factors such as cultural and economic factors, implemented vaccination programmes, training programmes and accessibility to vaccine. In the USA, where the mandatory vaccination is applied 81.1% of healthcare workers were vaccinated because of influenza in season 2018‐2019 and results were similar to the ones in the other four seasons (77.3%‐79.0%). 14 This rate differed between 15.6% and 63.2% among countries when the last three seasons were evaluated in Europe. The highest rates of vaccination in healthcare workers were found in Belgium and England. 15 In an extensive study conducted with 5046 healthcare workers by Tumturk et al from our country, while a regular vaccination at a rate of 7% was found 65.8% of the healthcare workers had never got influenza vaccine before. 7 In a study by Arda et al from the Izmir region, 41.7% of healthcare workers were vaccinated as a result of the local vaccination campaign implemented during the pandemic influenza season. 16 In our study, the rate of those who did not get vaccinated was found statistically significant compared with who got vaccinated. Although there are local studies on the rates of vaccination in healthcare workers in Turkey there are no countrywide data. Our study is the first extensive study that reached the healthcare personnel from all the regions of Turkey and various healthcare institutions.
Main barriers for people who do not want to get the vaccine are as follows: not believing in the effectiveness of vaccine, being afraid of its side effects and being unaware of the high risk for influenza infection in healthcare workers and their roles in the spread of the infection. 17 In the systematic review by Schmid, the most common ones among the main reasons why healthcare workers did not want to get the vaccine were reported as the lack of confidence because of misconceptions about the vaccine and low awareness on the seriousness of the disease. 18 According to a study conducted in the 2009 pandemic by Gurbuz et al, 570 healthcare workers were evaluated and the rate of vaccination was 39.6% for H1N1 and 42.3% for seasonal flu. The reasons why healthcare workers did not want to get influenza vaccine were finding the vaccine unnecessary (79.4%) and preferring other protection methods (70.5%) for seasonal flu vaccine and not trusting the vaccine (83.7%) for H1N1 vaccine. 19 In our study, the most common reason why healthcare workers did not want to get vaccinated was determined as they not believing in the necessity of vaccine with 53%. In our study as like others studies, insufficient information about vaccine took the most important place in people's behaviour and attitudes. For Gunduz et al, 72% of the families who agreed vaccination for their children accepted it because their doctors recommended. Especially physicians should share the information about the necessity of vaccine with their patients or people around them in order to prevent the false perceptions about the vaccine. 20 According to the results obtained from all these studies, it is concluded that main reasons to decline vaccination are false knowledge and attitudes on the seriousness of the disease, risk perception and transmission ways and concerns about the reliability, effectiveness and necessity of the influenza vaccine.
While the primary priority of the healthcare workers in getting the vaccine should be not spreading the virus to their patients and protecting them the main priority of the ones who agree to get the vaccine is to protect themselves and their families as in the other vaccines. 6 In our study, the most common reason for healthcare workers for choosing to have the vaccine was found that the vaccine prevent from the catching the flu by 38.9%. On the contrary, those who prefer to have the vaccine to protect their patients were found to be low 8.9%. It was found in a study by Gramegna that 63% of the workers got the vaccine primarily to protect themselves and 31% to protect the patients. 21
While the rates of vaccination differ among the occupational groups they may also vary according to the units. In the study by Genovase, while healthcare workers in clinical units were found to get influenza vaccine more than the ones in surgical units but not statistically significant. In the same study the rate of vaccination was 11.3% in doctors, 14% in nurses and 17% in other healthcare workers. 8 In our study; when emergency, internal and surgical units are evaluated according to vaccination rates, there was no significant difference detect between the groups. In the study by Tumturk et al from Turkey, when the ones who were regularly vaccinated each year were evaluated doctors were found to have the highest rate with 49.9% and they were followed by nurses with 21%. 7 Similarly, we determined that vaccination in doctors is higher who personally contacted with the patients and who planned a treatment than nurses and it is statistically significant. In a study in which the level of knowledge in Turkish general practitioners about influenza vaccine was evaluated, 75.3% of them had a good level of knowledge about the vaccine. In addition, an important relationship was found between the level of knowledge and the rate of vaccination. It was observed that doctors who were regularly vaccinated each year encouraged their patients and the healthcare workers to get the vaccine. 22
Our study has also some weaknesses. Vaccination status of the individuals were recorded based on their remembrance of the past. We believe that these predictions and misremembrances because of these predictions may affect the reliability and accuracy of the rates.
5. CONCLUSION
Although healthcare workers in our country still have the opportunity for free vaccination and are reminded by their institutions every year the rates of vaccination are low without implementing mandatory vaccination. Despite campaigns and training programmes, vaccination rates tend to decrease rather than increase compared with previous years. We consider that the most important reasons for this may be that the anti‐vaccination movement is increasing and that the views against vaccination take a large place especially in media. Our primary target should be to correct the false facts in order to increase the rates of vaccination. Training is an important approach to inform the healthcare workers about the side effects of the vaccine and the seriousness of the disease, however, social networks, television/media, medical booklets, support of people, whose ideas and behaviours are cared about, sharing rational data on the disease and its consequences with healthcare workers will also be effective methods. In addition, positive performance and rewarding practices should perform for encouraging the vaccination. Furthermore, reminder systems and mobile vaccine services which will facilitate access to vaccine should be used to improve vaccination rates.
As our study is the most extensive study accessing personnel from each region and each kind of healthcare institution it is important as it puts forward a nation‐wide idea especially about the issues to be emphasised while it increases the national targets of vaccination.
DISCLOSURE
The authors have declared no conflicts of interest for this article.
ACKNOWLEDGEMENT
Thank you to Bülent Altuntaş for their contribution in terms of statistically evaluation of data.
Korkmaz N, Nazik S, Gümüştakım RŞ, et al. Influenza vaccination rates, knowledge, attitudes and behaviours of healthcare workers in Turkey: A multicentre study. Int J Clin Pract. 2020;75:e13659. 10.1111/ijcp.13659
REFERENCES
- 1. Dini G, Toletone A, Sticchi L, Orsi A, Bragazzi NL, Durando P. Influenza vaccination in healthcare workers: a comprehensive critical appraisal of the literature. Human Vaccine Immunother. 2018;14:772‐789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Iuliano AD, Roguski KM, Chang HH, et al. Estimates of global seasonal influenza‐associated respiratory mortality: a modelling study. Lancet. 2018;391:1285‐1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CfD C. Influenza vaccine 1981–82. MMWR Morb Mortal Wkly Rep. 1981;30:279. [PubMed] [Google Scholar]
- 4. Randall LH, Curran EA, Omer SB. Legal considerations surrounding mandatory influenza vaccination for healthcare workers in the United States. Vaccine. 2013;31:1771‐1776. [DOI] [PubMed] [Google Scholar]
- 5. To K, Lai A, Lee K, Koh D, Lee S. Increasing the coverage of influenza vaccination in healthcare workers: review of challenges and solutions. J Hosp Infect. 2016;94:133‐142. [DOI] [PubMed] [Google Scholar]
- 6. Çiftci F, Şen E, Demir N, Çiftci O, Erol S, Kayacan O. Beliefs, attitudes, and activities of healthcare personnel about influenza and pneumococcal vaccines. Human Vaccines Immunother. 2018;14:111‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tumturk A, Tosun S, Yıldız İE, et al. Seasonal influenza vaccination coverage: a multicenter cross‐sectional study among healthcare workers. Ortadoğu Tıp Dergisi. 12, 113–119. [Google Scholar]
- 8. Genovese C, Picerno IAM, Trimarchi G, et al. Vaccination coverage in healthcare workers: a multicenter cross‐sectional study in Italy. J Prev Med Hygiene. 2019;60:E12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recommendations Rep. 2018;67:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chiu S, Black CL, Yue X, et al. Working with influenza‐like illness: presenteeism among US health care personnel during the 2014–2015 influenza season. Am J Infect Control. 2017;45:1254‐1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahmed F, Lindley MC, Allred N, Weinbaum CM, Grohskopf L. Effect of influenza vaccination of healthcare personnel on morbidity and mortality among patients: systematic review and grading of evidence. Clin Infect Dis. 2014;58:50‐57. [DOI] [PubMed] [Google Scholar]
- 12. Haykır Solay AUH, Acar A, Eser FGZ, Şencan İ, Yüce D. Health workers’ attitudes toward influenza vaccine, vaccination rates, and incidence of nosocomial influenza in a tertiary care center. ANKEM J. 2020;34:6‐12. [Google Scholar]
- 13. Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel—United States, 2017–18 influenza season. Morb Mortal Wkly Rep. 2018;67:1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Influenza Vaccination Information for Health Care Workers. https://www.cdc.gov/flu/professionals/healthcareworkers.htm Accessed January 15, 2020.
- 15. Seasonal influenza vaccination and antiviral use in EU/EEA Member States. https://www.ecdc.europa.eu/sites/default/files/documents/seasonal‐influenza‐antiviral‐use‐2018.pdf. Accessed January 20, 2020.
- 16. Arda B, Durusoy R, Yamazhan T, et al. Did the pandemic have an impact on influenza vaccination attitude? A survey among health care workers. BMC Infect Dis. 2011;11:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Petek D, Kamnik‐Jug K. Motivators and barriers to vaccination of health professionals against seasonal influenza in primary healthcare. BMC Health Serv Res. 2018;18:853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schmid P, Rauber D, Betsch C, Lidolt G, Denker M‐L. Barriers of influenza vaccination intention and behavior – a systematic review of influenza vaccine hesitancy, 2005 – 2016. PLoS One. 2017;12:2005‐2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gürbüz Y, Tütüncü EE, Şencan İ, et al. İnfluenza A (H1N1) 2009 pandemisinde hastane çalışanlarının grip aşısına yaklaşımlarının araştırılması. Pamukkale Tıp Dergisi. 2013;1:12‐17. [Google Scholar]
- 20. Gündüz S, Yüksel ÇN, Aktoprak HB, Canbal M, Kaya M. Attitudes towards influenza vaccination in high socioeconomic status Turkish parents. Turk J Med Sci. 2014;44:649‐655. [DOI] [PubMed] [Google Scholar]
- 21. Gramegna A, Dellafiore S, Contarini M, et al. Knowledge and attitudes on influenza vaccination among Italian physicians specialized in respiratory infections: an Italian Respiratory Society (SIP/IRS) web‐based survey. J Prev Med Hygiene. 2018;59:E128. [PMC free article] [PubMed] [Google Scholar]
- 22. Güldal D, Gürbüz İ, Ciblak MA, Nohutçu N, Badur S. Aile hekimliğinde grip ve grip aşısı: Bilmek uygulama için yeterli mi? Türkiye Aile Hekimliği Dergisi. 2012;16:157‐163. [Google Scholar]


