Abstract
Introduction
The COVID‐19 pandemic has transformed lives across the world. In the UK, a public health driven policy of population “lockdown” has had enormous personal and economic impact.
Methods
We compare UK response and outcomes with European countries of similar income and healthcare resources. We calibrate estimates of the economic costs as different % loss in Gross Domestic Product (GDP) against possible benefits of avoiding life years lost, for different scenarios where current COVID‐19 mortality and comorbidity rates were used to calculate the loss in life expectancy and adjusted for their levels of poor health and quality of life. We then apply a quality‐adjusted life years (QALY) value of £30,000 (maximum under national guidelines).
Results
There was a rapid spread of cases and significant variation both in severity and timing of both implementation and subsequent reductions in social restrictions. There was less variation in the trajectory of mortality rates and excess deaths, which have fallen across all countries during May/June 2020. The average age at death and life expectancy loss for non‐COVID‐19 was 79.1 and 11.4 years, respectively, while COVID‐19 were 80.4 and 10.1 years; including adjustments for life‐shortening comorbidities and quality of life plausibly reduces this to around 5 QALY lost for each COVID‐19 death. The lowest estimate for lockdown costs incurred was 40% higher than highest benefits from avoiding the worst mortality case scenario at full life expectancy tariff and in more realistic estimations they were over 5 times higher. Future scenarios showed in the best case a QALY value of £220k (7xNICE guideline) and in the worst‐case £3.7m (125xNICE guideline) was needed to justify the continuation of lockdown.
Conclusion
This suggests that the costs of continuing severe restrictions are so great relative to likely benefits in lives saved that a rapid easing in restrictions is now warranted.
Keywords: COVID‐19, economics, strategy, unlock
What is know
COVID‐19 is the disease associated with the 2019 novel coronavirus severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2). The pandemic related to this virus has transformed life for billions of people across the globe.
Estimates made in March 2020 put the likely level of UK deaths if there was no change in behaviour at 500 000. Based on that, and other, assessments the UK government followed the example of several other European countries in introducing severe restrictions on individual movement.
That slowed the spread of the virus and signalled to people that they needed to quickly change behaviours, but it also generated great costs—both economic and health related.
The precise extent to which the lockdown contributed to a subsequent slowing in the rate of new infections and deaths is not clear.
What’s new
Quantitatively links the economic costs to the health benefits in terms of possible quality‐adjusted life years (QALYs) saved
We find that the costs of lockdown in the UK are so high relative to likely benefits that continuing the lockdown for three months was unlikely to be warranted.
One would need to value any possible future QALYs at over £220,000—over seven times the NICE guideline value of £30,000 to have made a continuation of the lockdown beyond June warranted.
There is a need to normalise how we view COVID‐19 because its costs and risks are comparable to other health problems (such as cancer, heart problems, diabetes) where governments have made resource decisions for decades.
While there are inevitable risks in easing restrictions there are very clear costs in not doing so—a policy of not easing restrictions until the point at which there is virtually no chance of a resurgence in infection rates rising is not a policy in the interests of the population as a whole.
Movement away from blanket restrictions that bring large, lasting and widespread costs and towards measures targeted specifically at groups most at risk is prudent.
1. INTRODUCTION
Severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2), also known as COVID‐19 virus, was spreading alarmingly in early March 2020. The matter of whether the National Health Service (NHS) would be able to deal with rapidly rising numbers of seriously ill people was unclear. A group at Imperial College put the likely level of United Kingdom (UK) deaths if there was no change in behaviour at 500 000. 1 The UK government followed the example of several other European countries in with the Prime Minister announcing severe restrictions on individual movement. 2 The key message was to stay at home to protect the NHS to save lives. This was a lockdown. The precise extent to which the lockdown contributed to a subsequent slowing in the rate of new infections and deaths is not clear, though that it did so to some extent seems very likely.
As a highly infectious disease, the government response was to “Save Lives” through “Stay at Home” to reduce transmission outside the home, curtailing non‐essential recreation, travel and suggesting people work from home. “Protect the NHS” reflected concern that the key services such as hospitals, especially Intensive Care Units (ICU), would have been overloaded and unable to treat the potentially large number of very ill patients and so there would have been increased mortality.
The evidence from the first 3 months suggests that most of these measures worked. However, some quickly became less relevant.
The NHS rapidly put in place sufficient surge hospital & ICU capacity to cope with the very high level of expected demand, so service overload was no longer an immediate concern. Mateen et al 3 showed that NHS converted 2000 normal acute beds into ICU and further 11 000 beds were coming on stream within the five additional Nightingale Units (there were further 1200 beds booked in private ICUs. 4 This gave a total potential capacity of over 14 000 ICU beds. They also showed at the peak in early April 3000 ICU beds were being used by COVID‐19 patients in the context of what turned out to be 60 000 excess deaths, that is, 1 ICU bed to 20 excess deaths. This suggests that the 10 000 surge ICU beds gave technically sufficient ICU capacity to support a pandemic size resulting in up to 200 000 excess deaths. In the general wards, 3 showed around 12 000 beds were occupied by COVID‐19 patients, which gave a ratio of 1 General and Acute (G&A) bed to 5 excess deaths. There were still 30 000 beds free and a further 8000 beds in private hospitals had been booked 4 ; these 38 000 G&A beds gave sufficient headroom for a pandemic up to 200 000 excess deaths. The NHS through its own extreme efforts was far from being overwhelmed.
While it is clear that the cost of the lockdown has been large, the UK Finance Minister covered some of these in his summer statement, 5 just how great it is will not be known for many years. This cost—as well as the benefits of lockdowns—should be measured in terms of human welfare in the form of length and quality of lives. Such measurement is profoundly difficult. Yet measurement of the costs of restrictions needs to be weighed against the benefits of different levels of restrictions to assess what is the best policy now. We use rules that the National Institute for Clinical Excellence use to guide decisions on public health expenditure by the NHS 6 and which implicitly value years of lives saved to assess benefits of the lockdown relative to its likely cost—costs both in narrow economic terms but also in health terms.
The cost of severe restrictions plausibly rises more than in proportion to the length of a lockdown. There is some evidence that the benefits of maintaining a lockdown may be diminishing as described in Bongaerts et al (2020). 4
In this article, we aimed to calibrate what the costs and benefits of severe restrictions might be and what that implies about the policy that should now be followed in the UK.
2. METHODS/STRUCTURE
Bringing together costs and benefits is necessary if good policy decision is to be made. There is no simple way to do this that is clearly ethically justifiable, empirically reliable and widely accepted. However, to make no assessment is just to make policy in a vacuum.
We selected 10 European countries with populations over 5 million and average income/person over £15 000/year and examine the relation between the outcomes of the excess death as reported in Human Mortality Database of the University of California 5 and the different levels of lockdown as calculated and reported as a composite measure based on nine response indicators including school closures, workplace closures, hospitality venue closures and travel bans, in the Government Response Stringency from Blavatnik School of Government, University of Oxford 6 to see if there were any clear relationships. A detailed breakdown by country is described in the Results section.
Another approach is to focus on quality‐adjusted life years (QALYs) that may have been saved as a result of restrictions that have been in place in the UK up to early June and to convert that to a metric that can be compared with estimates of the cost of the restrictions. To that, we add estimates of the value of health care resources saved (both now and into the future) because lockdown reduced the numbers of sick people. That is the strategy we follow. We then go on to make estimates of costs and benefits of alternative ways forward with restrictions eased to different extents.
We make use of the guidelines established in the UK by the National Institute for Health and Care Excellence (NICE) for the use of resources in the UK health system (see NICE (2013) 7 ). These are guidelines applied to resource decisions that have a direct impact on lives saved. It is hard to see how you could run a public health care system without such rules.
The benefits are measured as the number of quality life‐years gained compared with the potential with different levels of lockdown. To establish these total quality life years, we examine the number of deaths directly reported and those excess deaths which were defined as the number of deaths above the average over comparable periods for recent years. 10 We examine the international situation to see if there was any relationship between level of lockdown and levels of excess deaths. We look at the ages of those that died to based on the normal ONS evaluate their life expectancy at those and then their comorbidities to establish a quality of life.
We add to these estimates of the saving of NHS resources from a much‐reduced demand upon its resources as lockdown slowed the numbers who became seriously sick.
To implement this, we need to assess how many likely extra years of good life might be enjoyed by the people who would have died but for a lockdown. We assume that the age and health of those who would have died are similar to that of those who have died with the virus. The ONS has been publishing each week the number of deaths where COVID‐19 has been recorded as a possible cause by quinary age and gender. By applying the average life expectancy 11 to the actual recorded COVID‐19 deaths by age and gender a total life expectancy years loss can be calculated. The average figure for years of life lost does not account for the fact that those who have died with COVID‐19 have often been in poor health, conditional on their age. We, therefore, examine reports on their actual levels of serious comorbidities and assessed their life‐shortening impact. We evaluate the quality of life they might have expected in those remaining years. We report benefits finding against both the full life expectancy loss and the quality of life adjusted loss.
The lockdown has reduced the amount of Intensive Care Unit (ICU) and General and Acute (G&A) ward costs required by the potential COVID‐19 patients. We evaluate reports on the current levels of use and against the number of deaths that occurred and extrapolated to the higher numbers seen in the scenarios.
To estimate the future costs of the lockdown we consider the wider shorter and longer‐term economic, social and health effects but feel they would all be reflected within the impact on Gross Domestic Product, and so take the latest measured values from the ONS and the latest estimates of future values from the Bank of England, Office of Budget Responsibility (OBR) and other experts. It seems plausible that a large fraction of these estimates of lost output is due to the lockdown. However, even without a government‐mandated lockdown there would have been some reduction in incomes so only a part of the lockdown effect is incorporated into our model.
Finally, we apply the same methodology to evaluate the future policy over the timing and rate of easing of the lockdown.
3. RESULTS
3.1. Section 1 – Preamble: Recorded cases, deaths and excess deaths
Infections rose dramatically in many European countries between February and March of 2020 and, with some lag, so did deaths attributed to the virus. Excess deaths are a more reliable measure of the overall cost in lives of the virus given the policies that were adopted for dealing with it. Figure 1 shows how a measure of excess deaths for a group of European countries with similar levels of income and health care provision to the UK. This is total deaths above the average of such deaths over the comparable months in previous years. Figure 2 shows a measure of the stringency of government restrictions introduced in European countries to counter the spread of the virus.
FIGURE 1.
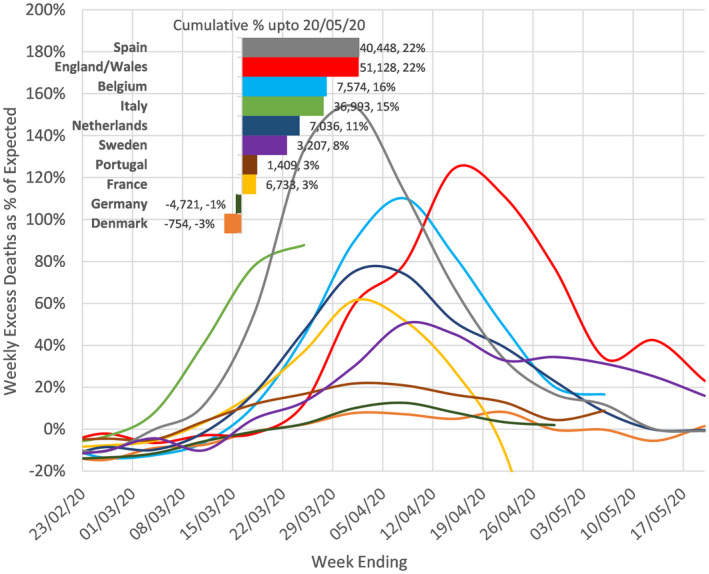
Excess Deaths in weeks 8‐21 of 2020. Difference to average in the same week in the previous 3 years (2017/2018/2019) and shown as % of average. 50 Source: The Human Mortality Database Department of Demography at the University of California, Max Planck Institute for Demographic Research, Center on the Economics and Development of Aging (CEDA) www.mortality.org. 8 Downloaded 9/6/2020
FIGURE 2.
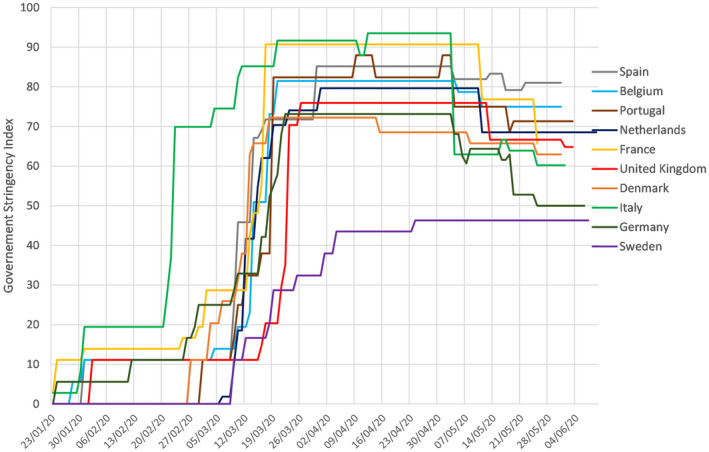
Date of Implementation and Relaxation of National responses in selected countries. The series is the COVID‐19 Government Response Stringency Index which is a composite measure based on nine response indicators including school closures, workplace closures, and travel bans, rescaled to a value from 0 to 100 (100 = strictest response). 9 Source: Blavatnik School of Government, University of Oxford, https://www.bsg.ox.ac.uk/research/research‐projects/coronavirus‐government‐response‐tracker
In late February or early March 2020, many European countries brought in severe restrictions on movement meaning that the majority of populations stayed home and numbers able to work fell dramatically. New cases of the infection and of deaths ascribed to the virus were significantly lower within a few weeks of restrictions being introduced.
3.2. Section 2: The costs of lockdowns
Evaluation of the Economic Impact of the lockdowns by sector using the number of staff furloughed reported by Her Majesty's Revenue and Customs (HMRC) 12 as metric for the reduction in GDP 13 also shows that 60% of the loss in GDP comes from those areas of the economy (real estate, manufacturing, administration, construction, professional services, IT, energy and water, financial) that have lower interaction with vulnerable groups while only 40% come from areas that could be seen to have a higher impact with vulnerable groups (retail, accommodation & food services, arts, entertainment, transport, health and social work) suggesting broad‐based lockdown may not have been the best use of resources.
For the UK the Office for Budget Responsibility (OBR) and the Bank of England estimate that GDP is likely to have fallen by between 25% and 35% in Q2 2020 and by 10%‐15% in 2020 relative to 2019; unemployment may rise to around 10%. The OBR central estimate, and the illustrative scenario for the Bank of England made in May 2020, is that in 2020 the UK GDP will be around 13%‐14% lower than in 2019. The National Institute for Economic and Social Research (in its May quarterly report) put the cumulative loss of output in the UK over 10 years at over 30% of annual GDP.
The estimates from the Bank of England and the OBR assume that easing of restrictions after June 2020 will mean that the lockdown is then soon over; it seems plausible that their estimates of economic cost are therefore estimates of the impact of the lockdown that had been in place in the UK from March to June and not of a continuation of the lockdown into the second half of 2020 and beyond. The OBR is explicit about this; in describing their forecasts they note: “The table below summarises the results of our three‐month lockdown scenario where economic activity would gradually return to normal over the subsequent three months.” The Bank of England in its May economic assessment takes a similar line: “Underlying the illustrative scenario for both the UK and the rest of the world is an assumption that enforced social distancing measures remain in place until early June and that they are then lifted gradually over the following four months, until the end of Q3”. In that illustrative scenario, GDP in 2020 is 14% below the 2019 level (Table 1A, Bank of England May Monetary Policy Report). 14
TABLE 1.
Life years lost to deaths in non‐COVID and COVID‐19 in 2020 up to the week ending 24th May
| Up to 24th May 2020 | Total deaths | COVID‐19 total deaths | Life expectancy each (years) | Total expected life years lost | ||||
|---|---|---|---|---|---|---|---|---|
| Age group | Male | Female | Male | Female | Male | Female | Non COVID | COVID‐19 |
| <1 | 576 | 446 | 2 | 0 | 79.3 | 82.9 | 82,476 | 159 |
| 1–4 | 89 | 64 | 0 | 1 | 77.1 | 80.7 | 11,949 | 81 |
| 5–9 | 56 | 31 | 0 | 0 | 72.6 | 76.3 | 6432 | 0 |
| 10–14 | 61 | 54 | 0 | 1 | 67.7 | 71.3 | 7907 | 71 |
| 15–19 | 203 | 100 | 5 | 4 | 62.7 | 66.3 | 18,787 | 579 |
| 20–24 | 325 | 142 | 13 | 9 | 57.8 | 61.4 | 26,214 | 1305 |
| 25–29 | 465 | 208 | 29 | 16 | 53.0 | 56.5 | 33,950 | 2440 |
| 30–34 | 654 | 358 | 46 | 29 | 48.2 | 51.6 | 46,259 | 3712 |
| 35–39 | 1003 | 635 | 65 | 49 | 43.4 | 46.7 | 68,081 | 5110 |
| 40–44 | 1406 | 856 | 139 | 81 | 38.7 | 41.9 | 81,497 | 8772 |
| 45–49 | 2326 | 1568 | 256 | 153 | 34.1 | 37.1 | 123,136 | 14,412 |
| 50–54 | 3884 | 2469 | 476 | 277 | 29.6 | 32.5 | 172,061 | 23,085 |
| 55–59 | 5633 | 3625 | 876 | 417 | 25.2 | 27.9 | 209,590 | 33,741 |
| 60–64 | 7640 | 5019 | 1234 | 617 | 21.0 | 23.6 | 238,458 | 40,495 |
| 65–69 | 10,575 | 6848 | 1643 | 845 | 17.1 | 19.3 | 268,990 | 44,464 |
| 70–74 | 16,314 | 11,331 | 2665 | 1406 | 13.4 | 15.4 | 335,960 | 57,429 |
| 75–79 | 20,131 | 15,452 | 3640 | 2235 | 10.2 | 11.7 | 322,234 | 63,145 |
| 80–84 | 24,854 | 22,256 | 4782 | 3478 | 7.3 | 8.5 | 306,689 | 64,625 |
| 85–89 | 25,537 | 28,624 | 4650 | 4234 | 5.1 | 5.9 | 249,665 | 48,572 |
| 90+ | 22,873 | 42,080 | 3812 | 5509 | 2.9 | 3.2 | 172,665 | 28,711 |
| Total | 144,605 | 142,166 | 24,333 | 19,361 | 2,783,000 | 440,907 | ||
| Mean age | 76.9 | 81.5 | 78.7 | 82.5 | ||||
| Non Covid‐19 | 243,077 | Covid‐19 | 43,694 | Lost years/death | 11.4 | 10.1 | ||
It is important to point out that any elements of the cost of the lockdown in the UK are not reflected at all in current incomes, employment and GDP. Health costs—including mental health—are not yet showing up in a measurable way. They are likely to be large and long‐lasting. Referrals for cancer investigations were 70% down in April 2020 15 ; there were hardly any follow‐up routine appointments for long term conditions in UK Primary Care between mid‐March 2020 and the beginning of June 2020; outpatients seen were 64% down and elective admissions were 75% down 16 ; attended appointments in General Practice were down 35%. 17 The impact of the stress of the ‘Lockdown’ on anyone with a pre‐existing mental health condition, let alone the population as a whole, is yet to be determined. This was eloquently addressed by Kilgore et al in their recent paper 18 which described greater loneliness and elevated depression and higher suicidal ideation in those socially isolating on a standard clinical screening instrument. The observed effect sizes were large, suggesting that social isolation is likely to have a tangible and meaningful impact when considered at the population level.
Furthermore, the cost from disrupted education of children and students will be felt over a horizon of many years, even decades.
3.3. Section 3 – Bringing costs and benefits together
The guidelines in the UK set out by NICE are that treatments that are expected to increase life expectancy for a patient by one year (in quality of life adjusted years, QALYs) should cost no more than £30 000. 7 We apply that figure to possible total numbers of QALYs saved by restrictions to estimate their benefit.
The ONS published in total up to the week ending 22 May, 43 694 deaths associated with COVID‐19 in England and Wales. (This total is 21% below the excess all causes deaths figure of 55 504 up to w/e 24 May (Week 21) calculated by comparing the actual recorded number in 2020 to the average deaths over previous 3 years in the same period).
Table 1 shows the calculation of ONS Life expectancy lost by age and gender. Average life expectancy loss comes out at 10.1 years per COVID‐19 death. (The average life expectancy years lost for a non‐COVID‐19 death are higher at 11.4 years confirming that the age for COVID‐19 mortality is slightly older than normal mortality). The median COVID‐19 age at death is around 80 and the average life years lost for the older 50% is 5 years and for younger 50% is 15 years.
In their detailed study of 23 804 hospital deaths in England from COVID‐19 from 1 March 2020 to 11 May 2020, Valabhji et al (2020) 19 found that various life‐shortening risk factors were significantly more prevalent in those patients who died of COVID‐19 than in the general population. This included diabetes (33% vs 5%), and previous hospital admission for significant cardiovascular comorbidities including coronary heart disease (31% vs 3.5%), cerebrovascular disease (19.8% vs 1.5%) and heart failure (17.7% vs 1%).
Other comorbidities such as dementia in its various forms, chronic obstructive pulmonary disease (COPD), vitamin D deficiency and hyperlipidaemia were not collected and compared, but it is plausible that these would also show similar levels of differences. Each of these comorbidities has been shown to significantly increases the risk of early death. The National Diabetes Audit in their mortality study 20 found that the presence of diabetes increases a person standard mortality risk by a factor of 1.6.
It is, therefore, plausible that those patients who died of COVID‐19 were, on average, already in relatively poor health for their age and this poor health would give them a life expectancy, on average, significantly below that of the age‐equivalent general population.
These comorbidities and conditions also reduce the person's quality of life, as well as its quantity. 21 The impact of poor health through long‐term conditions and comorbidities are usually incorporated into modelling through a quality of life utility factor which ranges from 1 (healthy) to 0 (death); this is used to adjust the total life years. Beaudet et al (2014), 22 found that the basic type 2 diabetes without complication had a factor of 0.79 and then other comorbidities would reduce this further including myocardial infarction −0.06, ischemic heart disease −0.09, heart failure −0.11 and stroke −0.16. An average poor health utility factor of 0.8 could be applied to the population of those who have died with COVID‐19. Both Gentry et al in “The Fatality and Morbidity Components of the Value of Statistical Life” 23 and Murphy et al in “The Value of Health and Longevity” 24 report similar trends.
A substantial downwards adjustment to the 10 years estimate of the residual life expectancy based on the general population would seem appropriate for the group who have died with COVID‐19. How great an adjustment is hard to be precise about, but with an adjustment for quality of life included, it might plausibly be by one half. In the calculations below we apply either no adjustments for co‐morbidities or an adjustment of one‐half, using lost average quality‐adjusted life years per COVID‐19 death of 10 or 5 years.
3.3.1. Other benefits besides saved lives
In the current situation, the following existing costs are associated with the current 60 000 excess deaths. The following associated hospital activity was reported.
ICU: The Intensive Care National Audit and Research Centre (ICNARC report) 25 showed that 10 130 patients with COVID‐19 were treated (including 72% advanced respiratory support, 30% advanced cardiovascular support, 26% renal support) for a median of 11 days, which based on reference costs of £1 503/day for a mix of 1/2/3 organ support 26 gives a total £16 500/ICU admission. From the current ratio, 1 ICU admission is associated with 6 excess deaths, this is equivalent to £2600 ICU costs incurred/ excess death.
General and Acute (G&A); The Cabinet daily briefing on the 26th June 27 reported total 125 000 COVID‐19 hospital admission and each had 7 days Length of Stay (LOS) 28 @£ 462/day average costs for non‐elective infectious disease 29 ; this gave £3250 G&A costs/admission. From the current ratio of 2 admissions associated with each excess death, this is equivalent to £6500 G&A costs incurred/ excess death.
Together they add up to £9000 overall hospitalisation costs/ excess death.
The lockdown has also reduced the potential impact of other further life‐shortening conditions on survivors. This was evaluated by assuming that the current 6000 ICU survivors, 25 who had an average age of 55, were most at risk. If the post COVID‐19 condition were like chronic obstructive pulmonary disease (COPD) Stage 3 (too short of breath to leave the house, breathless while dressing and undressing) they would have a life expectancy of 10 years 29 so would have lost 15 life years of their full life expectancy. 19 If 20% of ICU survivors experience these effects, there would be a total loss of 18 000 life years in the future relative to the current 60 000 excess deaths or 0.3 QALY/excess death, which if valued at @£30 000/QALY gives £9000 QALY value lost/excess death.
Together these would bring approximately £20 000 healthcare benefits for each excess death avoided through the lockdown.
3.4. A cost‐benefit analysis of the lockdown
3.4.1. The benefit in terms of estimated lives saved
Suppose that a group of people who each had expected quality‐adjusted remaining years of life of 5 years, and who might have died with the virus, has been spared that because of government restrictions (“the lockdown”). We will assume that the benefit of the restrictions that prevented such deaths is the value of 5 quality‐adjusted years of life multiplied by the number of lives saved. The NICE £30 000 threshold is an assessment of the (maximum) resource cost that would be justified for the UK health service to make an expected saving of one quality‐adjusted year of life. To save 5 QALY would be worth up to £150 000.
We apply this figure of £150 000 (or a figure of £300 000 if we make no adjustment for co‐morbidities and take 10 life years lost per death) to estimates of the possible number of lives saved as a result of lockdowns to give an overall benefit number. To that, we add an estimate of £20 000 other health costs saved (per life saved) based on the evidence summarised above. We compare that aggregate number with an estimate of the lost resources from the lockdown.
As noted above there is no single, reliable estimate of lives that have been saved by the UK lockdown and nor is there a widely accepted single figure for the comprehensive overall cost of the lockdown (which should include lost and damaged lives into the future as a result of severe restrictions and not just lost incomes in 2020). So, we present a range of estimated costs and benefits based on a wide range of assumptions that we think encompass plausible upper and lower limits on both costs and benefits.
At the high end of estimated lives saved is the difference between the projected deaths from the study of Professors Ferguson's group at Imperial assuming no change in behaviour (500 000) 1 less an estimate of excess UK deaths (~60 000 by June 2020). These 440 000 net lives saved number is likely to be a significant overestimate of likely lives saved. As noted above it does not account for changes in behaviour that would have occurred without the government lockdown; it does not count future higher deaths from side effects of the lockdown (extra cancer deaths for example); it does not allow for the fact that some of those “saved” deaths may just have been postponed because when restrictions are eased. In the absence of a vaccine or of widespread immunity, deaths may pick up again. (If the epidemic is dying out anyway those deaths will not come as the lockdown is eased but in this case, the 440 000 saved lives are also excessive because the lockdown may have come as a decline in infections was happening for other reasons).
The Hospitalised Fatality Rate 30 has fallen from 6%/day at the start of April to 1.5% in mid‐June. So, the estimate of 500 000 deaths made back in March and based upon fatality rates then may have been particularly pessimistic.
At the other end of the spectrum would be estimates of net saved lives that are effectively zero. We set the lowest estimated net set lives well above that and use (rather arbitrarily) a “lowest” estimate of 20 000.
For each life saved we apply a factor of either 5 or 10 quality‐adjusted extra years of life, each valued with the NICE guideline figure of £30 000. 7 We also factor in that alongside fewer deaths there would have been far fewer demands made upon the resources of the public health system and we have placed a value of that per potential life saved of £20 000.
The cost
On the cost side the lowest resources cost is just to count the GDP that would have been produced in 2020 but for the lockdown established in March and assuming the lockdown to be eased from the end of June. This assumes a rapid bounce back by the end of the year so there is no effect on incomes and output from the start of 2021 onwards. That was the scenario envisaged by the Bank of England in their May 2020 assessment of the economic outlook when they put the GDP loss in 2020 at around 14%. The OBR estimate for lost output in 2020, also based on an assumed rapid recovery in the second half of the year, is close to 13%. It seems plausible that a large fraction of these estimates of lost output is because of the lockdown. But even absent a government‐mandated lockdown there would have been some reduction in incomes. If the lockdown effect was only two‐thirds of the total, then the Bank of England and OBR estimates might imply around a 9% fall in GDP as a result of it.
At the high end of the spectrum would be an estimate of 15% of GDP lost in 2020 and lower output for the next few years on top of that as economic activity does not return to normal for several years with some firms permanently damaged by the lockdown and the large rise in unemployment slow to be reversed, even if restrictions are quickly removed from mid‐2020. A shortfall of GDP of 15% in 2020; 7.5% in 2021 and 2.5% in 2022 (so that the cumulative lost output would then be 25% of GDP). That would be at the more pessimistic end of the spectrum for the impact of the March‐June lockdown. For many economists, such a figure seems realistic rather than pessimistic. Layard et al 31 put the likely economic cost on a central forecast as high as our most pessimistic case; and as noted the National Institute of Economic and Social research put their best guess of the narrowly defined economic cost higher again.
Cost/benefit balance
Tables 2 and 3 show the cost‐benefit calculations of the lockdown based on such ranges: In each cell, we report three numbers: benefits (+), costs (‐) and (in red) the balance of the two—all measured as £ billion.
TABLE 2.
Benefits (+), costs (−) and net benefits of March‐June UK lockdown; converted to an index of £ billion (b)
| 9% GDP loss | 15% GDP loss | 20% GDP loss | 25% GDP loss | |
|---|---|---|---|---|
| Lives not lost | ||||
| 440,000 | £75b, ‐£200b, | £75b, ‐£330b, | £75b, ‐£440b, | £75b, ‐£550b, |
| ‐£125b | ‐£255b | ‐£365b | ‐£475b | |
| 200,000 | £34b, ‐£200b, | £34b, ‐£330b, | £34b, ‐£440b, | £34b, ‐£550b, |
| ‐£166b | ‐£296b | ‐£406b | ‐£516b | |
| 100,000 | £17b, ‐£200b, | £17b, ‐£330b, | £17b, ‐£440b, | £17b, ‐£550b, |
| ‐£183b | ‐£313b | ‐£423b | ‐£533b | |
| 50,000 | £9b, ‐£200b, | £9b, ‐£330b, | £9b, ‐£440b, | £9b, ‐£550b, |
| ‐£191b | ‐£321b | ‐£431b | ‐£541b | |
| 20,000 | £3b, ‐£200b, | £3b, ‐£330b, | £3b, ‐£440b, | £3b, ‐£550b, |
| ‐£197b | ‐£327b | ‐£437b | ‐£547b |
5 Quality‐Adjusted Life Years (QALY) is assumed lost for each COVID‐19 death. Each life saved is estimated to result in 5 more quality‐adjusted years of life. The NICE resource threshold of £30,000 is applied to each of these quality‐adjusted years. The further benefits of reduced ICU and ward admission costs and longer‐term life‐shortening residual effects are taken at £20,000 for each life saved. The money value of Gross Domestic Product (GDP) losses are taken as a proportion of 2019 GDP of £2.2 trillion. All resulting figures are in £ billion.
TABLE 3.
Benefits (+), costs (‐) and net benefits of March‐June UK lockdown; converted to an index of £ billion (b)
| 9% GDP loss | 15% GDP loss | 20% GDP loss | 25% GDP loss | |
|---|---|---|---|---|
| Lives not lost | ||||
| 440,000 | £141b, ‐£200b, | £141b, ‐£330b, | £141b, ‐£440b, | £141b, ‐£550b, |
| ‐£59b | ‐£189b | ‐£299b | ‐£409b | |
| 200,000 | £64b, ‐£200b, | £64b, ‐£330b, | £64b, ‐£440b, | £64b, ‐£550b, |
| ‐£136b | ‐£266b | ‐£376b | ‐£486b | |
| 100,000 | £32b, ‐£200b, | £32b, ‐£330b, | £32b, ‐£440b, | £32b, ‐£550b, |
| ‐£168b | ‐£298b | ‐£408b | ‐£518b | |
| 50,000 | £16b, ‐£200b, | £16b, ‐£330b, | £16b, ‐£440b, | £16b, ‐£550b, |
| ‐£184b | ‐£314b | ‐£424b | ‐£534b | |
| 20,000 | £6b, ‐£200b, | £6b, ‐£330b, | £6b, ‐£440b, | £6b, ‐£550b, |
| ‐£194b | ‐£324b | ‐£434b | ‐£544b |
10 QALY is assumed lost for each COVID‐19 death. Each life saved is estimated to result in 10 more quality‐adjusted years of life. The NICE resource threshold of £30,000 is applied to each of these quality‐adjusted years. The further benefits of reduced ICU and ward admission costs and longer‐term life‐shortening residual effects are taken at £20,000 for each life saved. The money value of Gross Domestic Product (GDP) losses are taken as a proportion of 2019 GDP of £2.2 trillion.
For every permutation of lives saved and GDP lost the costs of lockdown exceed the benefits by a wide margin. Even if lives saved are as high as 440 000, each of which means an extra 10 years of quality‐adjusted life—and when the lost output (assumed to be a sufficient and comprehensive measure of all costs of the lockdown) is simply the likely shortfall in incomes in 2020—costs are still over 40% higher than benefits of lockdown (benefits = £141 billion; costs = £200 billion). In all other cases costs are a multiple of benefits. In most cases, costs are 10 times or more the scale of benefits. This result reflects the fact that the economic costs of the lockdown—even on the most conservative estimate of £200 billion (0.9% of GDP)—is far larger than annual total expenditure on the UK national health service (which runs at around £130 billion); the benefits of that level of resources applied to health and using the NICE guidelines would be expected to generate far more lives saved than is plausibly attributable to the lockdown in the UK.
Another way of making the same point is that the cost per QALY saved of the lockdown looks to be far in excess (by a factor of at least 3 and often by a factor of 10 and more) of that considered acceptable for health treatments in the UK.
Might it be that the calculations massively understate the benefits of lockdown? That would be the case if the value of lives saved is dramatically too low; some would say that it is. Estimates used in the US for the statistical value of a life place it slightly above $10 million. 23 , 24 For a new‐born who might expect 80 good years of life the NICE £30 000 number would generate a life value of £2.4 million—just under a third of the value if a statistical life is worth $10 million. Goldstein and Lee (2020) 32 note that US health economists use values of around $125 000 per year of life. That is also a bit over three times the NICE figure.
However, the £30 000 figure per QALY is the figure used in evidence‐based resource decisions within the UK health system. It is not an arbitrary number. It is not based on likely future earnings lost or the value of future consumption—calculations that are open to the moral objection that they reduce the value of human life to how much people would have spent on commodities.
Instead, the figure we use for the value of a QALY is a measure of what is considered the highest level of resources (ie what part of GDP) in the UK health system that should be used to generate extra quality‐adjusted years of life—and it is saving of lives which is what the lockdown was for. In using this yardstick, we are treating decisions on how to face COVID‐19 in the same way as decisions in the UK are made about resources to apply to the treatment of cancer, heart disease, dementia and diabetes. On that basis, it would seem as though the benefits of the lockdown were far lower than its costs. Yet even if one used valuation of a QALY three times as great the figures in Tables 2 and 3 (with benefits raised by a factor of 3) this would still generate costs of the lockdown in excess of benefits in nearly all the cases considered.
That judgement is, however, made with the benefit of hindsight: we now know more about the scale of the economic costs of the lockdown than was known in March, and also know about how deaths and new infections have evolved across Europe. The more interesting policy issue is what it is best to do now: how quickly should the lockdown be eased given what we know now? That issue we consider in the next section.
3.5. Section 4: what policy to adopt now?
We apply a similar cost‐benefit methodology to consider policy options for the level of restrictions applied in the UK over the next 3 months (July‐September 2020). The options we consider fall under two broad headings:
Carry on with only very limited easing of restrictions
Move quickly to minimal lockdown (easing restrictions rapidly and relying on existing tracking of the cases/deaths to prevent re‐emergence of the virus)
We consider the following scenarios for the consequences of each policy for the evolution of COVID‐19 deaths:
Very limited easing of restrictions results in a continuing steady fall in the death rate over 13 weeks down to single figures per week at the end of three months. Each week deaths are assumed to be 0.7 x deaths of the previous week.
-
For the policy of rapid easing of restrictions, we consider three possible scenarios:
Deaths continue to fall but at a slower rate than with a slow and limited easing of lockdown; each week deaths are 0.9 x deaths of the previous week
Deaths continue at the start‐June level of 1230 per week and do not fall further
Deaths steadily increase back up to levels seen at the height of the UK pandemic; each week they are 15% higher than the week before.
The assumed paths of deaths under the four scenarios are shown in Table 4. In each case, we set the initial level of deaths in the week prior to each scenario at the last ONS recorded figure for UK deaths in the week to 12 June (1230 deaths).
TABLE 4.
Deaths and costs of deaths under different unlocking scenarios
| From 6th December 2020 | Continue lockdown (0.7) | Ease scenario I (0.9) | Ease scenario II (1) | Ease scenario III (1.15) |
|---|---|---|---|---|
| Week 1 | 861 | 1107 | 1230 | 1415 |
| Week 2 | 603 | 996 | 1230 | 1627 |
| Week 3 | 422 | 896 | 1230 | 1871 |
| Week 4 | 295 | 806 | 1230 | 2152 |
| Week 5 | 207 | 725 | 1230 | 2475 |
| Week 6 | 145 | 653 | 1230 | 2846 |
| Week 7 | 102 | 588 | 1230 | 3273 |
| Week 8 | 71 | 529 | 1230 | 3764 |
| Week 9 | 50 | 476 | 1230 | 4329 |
| Week 10 | 35 | 428 | 1230 | 4978 |
| Week 11 | 25 | 385 | 1230 | 5725 |
| Week 12 | 18 | 347 | 1230 | 6584 |
| Week 13 | 13 | 312 | 1230 | 7572 |
| Total expected deaths | 2847 | 8248 | 15,990 | 48,611 |
| Additional expected deaths compared to continue lockdown | 5401 | 13,143 | 45,764 | |
| Cost of easing (£ billions)—each add. death = 5 QALY valued at £30,000 | £0.92 | £2.23 | £7.786 | |
| Cost of easing (£ billions)—each add. death = 10 QALY valued at £30,000 | £1.73 | £4.21 | £14.64 | |
Deaths are assumed to evolve week by week from the level in the week ending 12 June (1230) by a factor 0.7; 0.9; 1.0; 1.15 for the lockdown and scenarios I, ii and ii, respectively. Benefits of lived saved include £20,000 per life saved for lower medical costs as well as the value of QALYs saved.
The implied cost of the extra deaths from the easing policies (under scenarios i, ii. and iii) are shown towards the bottom of the table. These are the projected excess deaths under each easing scenario relative to the policy of continuing with the lockdown multiplied by the lost QALY per death and valued at £30 000 per QALY; there is an additional £20 000 per life lost for associated medical costs. These numbers are in £ billion and should be set against the estimated benefits from easing the lockdown.
Our low‐end estimate of the (narrowly defined) cost of the March to early June lockdown was 9% of GDP—a figure of a little over £200 billion. One might assume that a continuation of the lockdown over the next three months with only a very limited easing of restrictions generates a further cost of the same size. But the rapid easing of restrictions is unlikely to generate zero costs. Such costs may still be substantial, though likely far lower than a continuation of lockdown policies. A conservative estimate of the benefits of easing the lockdown is that the £200 billion costs under lockdown might be half that size. This would generate a benefit from easing of £100 billion over three months to be set against any extra lives lost.
Under all scenarios the cost of easing is a small fraction of the benefits—the maximum cost of £14 billion should be set against a conservative estimate of benefits of £100 billion. One would need to value QALYs at £220 000—over 7 times the NICE guideline value of £30 000 to make a continuation of the lockdown warranted in the scenario of the greatest number of live years not lost with costs/ QALY much higher for less live years saved. That runs counter to agreed UK policy on the economic viability of health interventions. 7
Figure 3 presents the same information in a slightly different way, calculating the net costs of an extension of the lockdown relative to a policy of immediate easing. Even taking the best estimate of lives not lost, the benefits of lives not lost, relative to the easing of restrictions, the cost of continued lockdown for a further 3 months from mid‐June 2020 is £86.3 billion.
FIGURE 3.
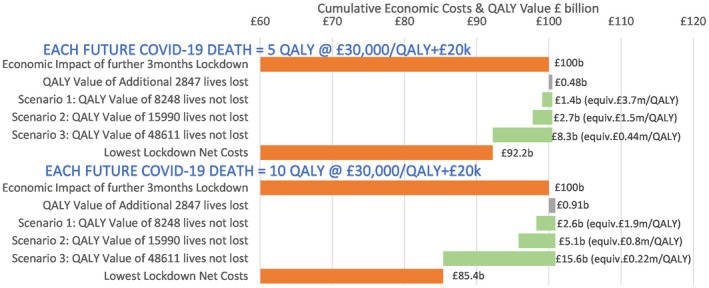
Net extra economic costs of the lockdown relative to the easing of restrictions are assumed to be £100 billion. To that is added the cost of lives lost under lockdown. The benefits of lives not lost, relative to the easing of restrictions, is then deducted from the lockdown costs to generate a net cost figure under the three scenarios. The easing scenarios are: (a) deaths still decline but slower than in Lockdown, (b) deaths remain at start June 2020 levels (c) deaths increase again back up to April 2020 peak levels. The equivalent cost/QALY is calculated by dividing the Lockdown costs (£100 billion) by the net number of lives not lost in that scenario times the number of Quality‐Adjusted Life Years (QALYs) for each death
4. DISCUSSION
4.1. How much of the slowdown in infections was because of lockdowns?
It is not straightforward to assess exactly how much of the slowing in new infections and deaths is directly attributable to the lockdown. People were altering their behaviour before severe restrictions were introduced—mobile phone data reveals sharp declines in the movement of people some weeks ahead of lockdown. Some changes in behaviour (washing hands, avoiding crowds) may have been effective in reducing infections but at a low economic cost.
It is also possible that a significant degree of immunity may have built up by the time severe restrictions were introduced because the infection may have spread quite widely and largely unnoticed with the asymptomatic a very large fraction of the infected.
A substantial proportion of the population may have been effectively immune from the virus when lockdowns started not just because of recovery from past infections that conferred a degree of immunity but also because a significant proportion of the population may never have been susceptible. In this regard at least two studies reported possible immunity against SARS‐CoV‐2 because of previous infections with harmless Coronaviruses. Braun et al 33 showed the presence of SARS‐CoV‐2 reactive T cells in COVID‐19 healthy donors and Grifoni et al 34 reported the detection of SARS‐CoV‐2‐reactive CD4+ T cells in ∼40%–60% of unexposed individuals, suggesting cross‐reactive T cell recognition between circulating “common cold” coronaviruses and SARS‐CoV‐2.
All three factors described above may have played a role, and all would mean that deaths and new infections would have slowed in the absence of severe government restrictions. There is some evidence that all these factors played some role in bringing down infections alongside severe government restrictions.
An Oxford University research team used death data to estimate the proportion of the population who might have built up some form of immunity before the UK lockdown was introduced in mid‐March 2020. They put that fraction at around 60% (Lourenço et al 2020). 35 Stedman et al (2020) 36 used data on differences in the spread of the infection across English regions to assess how many might have been infected and put that fraction at similarly high levels. Dimdore‐Miles and Miles (2020) 37 fitted a SIR (Susceptible‐Infected‐Recovered) model to data on new cases of infections across several countries and estimated that the numbers who might have been infected with no (or few) symptoms were likely to be at least 10 times (and possibly as much as 200 times) as large as those who had symptoms and were more likely to have been tested up to late April 2020.
Wieland (2020) 38 modelled the spread of the infection across Germany and concluded that infections were past their peak and starting to decline ahead of the introduction of government restrictions there. The results were summarised thus: “In a large majority of German counties, the epidemic curve has flattened before the social ban was established (March 23). In a minority of counties, the peak was already exceeded before school closures.”
Friston 39 and Levitt 40 both conclude that the numbers of people not susceptible to the COVID‐19 virus were already very substantial before lockdowns were introduced and that the virus was burning itself out.
Testing based on the presence of antibodies, however, put the level of those who have had the infection in European countries where the virus has spread most rapidly at only 5%‐10%, though in some areas within countries it is still high enough to have had a significant impact on the R‐value, which is the number of people subsequently infected by each infected person. Antibody testing itself is not a perfect tool and additional research is needed to determine if and to what extent a positive antibody test means a person may be protected from reinfection with SARS‐CoV‐2. Serology tests should not be used as a stand‐alone tool to make decisions about personal safety related to SARS‐CoV‐2 exposure, Lerner et al 41
4.2. The evidence from countries with different policies
In contrast to many other European countries, the Swedish strategy has been one of adopting much less restrictive measures that is far short of a lockdown (see Figure 2). Infections and deaths have been far higher than in neighbouring Denmark and Norway, but excess deaths are lower than in many European countries and only one third the level (relative to population) in the UK. In terms of overall impacts, there is contradictory evidence. Born et al (2020) 42 and Krueger, Uhlig and Xie (2020) 43 argue that the Swedish strategy has been successful. But health outcomes in countries most similar in terms of climate, the density of population and standard of living (that is Denmark and Norway) appear to be much better.
The UK data show a significantly higher cumulative death rate than Sweden; Figure 1 and 43 show excess deaths relative to expected in the UK at more than twice the Swedish level by early June 2020. On this measure, Sweden sits near the middle of the pack for European countries. Death rates in several countries with harder “lockdowns” have been significantly higher than in Sweden.
4.3. The economics of lockdown
A great deal of evidence is already emerging on the (narrow) economic impacts of restrictions. Estimates made by Deb et al (2020) 44 to identify the particular effect of restrictive policies (lockdown) suggest that they reduced economic activity by 15% in the 30 days after they were adopted. They find that stay‐at‐home requirements and workplace closures are the costliest in economic terms. Preliminary estimates from the UK Office for National Statistics showed a slightly more than 20% fall in GDP in April 2020, the first full month after the lockdown. Bonadio et al (2020) 45 put the impact on output and incomes (ie GDP) of policies to counter the spread of the infection on GDP averaged across 64 countries even higher, at around 30%. Costs which will come further down the road because of disruption to healthcare 46 and education are harder again 47 to measure relative to the more immediate effects on economic production and employment. 48
The lockdown can be seen as having 2 elements: a social lockdown (distancing, no social gathering, recreation or sports events etc) and an employment lockdown (not travelling or going to non‐essential work). The latter is not likely to be the most effective response as infection amongst the employed was not a major source of mortality. Linking the total population by age group with employment 49 and COVID‐19 Age‐specific Mortality rate 50 by age group shows that only 7% of those that have died may have been in employment. Coronavirus (COVID‐19) Community Infection Survey 51 showed that the infection rate amongst employed age group 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 was 70% higher than the stay at home age groups, and combining this with the population by age group shows 51% of all infections and 1% of deaths were recorded within this age group.
4.4. How effective was the lockdown?
In the UK, it is hard to be sure of the scale of benefits of the lockdown in terms of lives saved and the avoidance of the resources of the health service being exhausted. In terms of lives saved estimates range from very few lives saved to a high of perhaps 450 000 lives saved (that is the difference between the 500 000 or so deaths projected by Ferguson et al (2020) 1 on the basis of no change in behaviour and the 50 000 or so deaths that might have resulted in the UK by early June 2020).
There are reasons to be sceptical of figures at the high end of that scale which puts the saving of lives from the lockdown at several hundreds of thousands:
The low cost of effective forms of behavioural change (washing hands, avoiding crowds) adopted by individuals makes it unlikely that in the UK there would have seen 500 000 deaths even with no government restrictions; the 500 000 figure from Ferguson et al (2020) 1 was based on an assumption of no change in individual behaviour
The evidence of a turn in the curve before lockdowns are likely to have had much effect is disputed but not easily dismissed
Even if lockdowns stopped such huge numbers of deaths over the period March‐June 2020 they have not permanently stopped them happening if wider immunity has not significantly risen so that any substantial easing of restrictions will just bring them back
In many countries deaths were concentrated in care homes for the elderly 53 and have been disproportionately among older people so a blanket lockdown (“don't leave home”) may have been inefficient—it generated huge costs (see below) and may have yielded limited health benefits, over and above what might have been achieved with measures which focused on groups most at risk.
Infections caught within hospitals and care homes have been shown to be a major source of mortality because of vulnerability, while here these have not been restricted by the lockdown. Covid‐19 may now be a nosocomial disease. DELVE Initiative Scoping Report on Hospital and Health Care Acquisition of COVID‐19 and its Control” 54 and the Office for National Statistics (ONS) Coronavirus (COVID‐19) Infection Survey pilot 52 provide values that suggest over 20% of infections may have occurred in hospitals and residential care homes. The ONS data on reported deaths by location 10 (including for transfers from care homes to hospital and those infected within the hospital) suggest over 50% of the current deaths may have resulted from those infections within the hospital or care homes. A larger number of vulnerable people receive regular support and care within their own homes, these contacts with their care support staff could have also been a further source of increased risk, infections and mortalities.
The benefits of a lockdown are, however, not just in terms of lives saved—though that is of immense value. Valuing the health care resources saved because the lockdown reduced the numbers of sick people is also an important element of its benefits.
5. CONCLUSION
There is a need to normalise how we view COVID‐19 because its costs and risks are comparable to other health problems (such as cancer, heart problems, diabetes) where governments have made resource decisions for decades. Treating possible future COVID‐19 deaths as if nothing else matters is going to lead to bad outcomes. Good decision making does not mean paying little attention to the collateral damage that comes from responding to a worst‐case COVID‐19 scenario.
The lockdown is a public health policy and we have valued its impact using the tools that guide health care decision in the UK public health system. On that basis and taking a wide range of scenarios of costs and benefits of severe restrictions, we find the lockdown has consistently generated costs that are greater—and often dramatically greater—than possible benefits.
Weighing up costs and benefits of maintaining general and severe restrictions is necessary. That is how decisions over a wide range of public policy issues are made—many directly concerning public health issues. While there are inevitable risks in easing restrictions there are very clear costs in not doing so ‐ a policy of “let's wait until things are clearer” is not reliably prudent. A policy of not easing restrictions until the point at which there is virtually no chance of a resurgence in infection rates rising is not a policy in the interests of the population.
Movement away from blanket restrictions that bring large, lasting and widespread costs and towards measures targeted specifically at groups most at risk offers is now prudent. Such a policy has now been implemented.
6. ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The analysis used nationally available general practice‐level data with no patient identifiable data. Therefore, we felt that Ethics Permission was not required.
CONFLICT OF INTEREST
No author has any conflict of interest.
CONSENT FOR PUBLICATION
All authors consent to the publication of this article.
ACKNOWLEDGEMENTS
None declared.
Miles DK, Stedman M, Heald AH. “Stay at Home, Protect the National Health Service, Save Lives”: A cost benefit analysis of the lockdown in the United Kingdom. Int J Clin Pract. 2021;75:e13674. 10.1111/ijcp.13674
REFERENCES
- 1. Ferguson NM, Laydon D, Nedjati‐Gilani G, et al. Impact of non‐pharmaceutical interventions (NPIs) to reduce COVID‐ 19 mortality and healthcare demand. Imperial College COVID 19 Response team report. 16 March 2020.
- 2. Prime Minister's statement on coronavirus (COVID‐19): 23 March 2020. https://www.gov.uk/government/speeches/pm‐address‐to‐the‐nation‐on‐coronavirus‐23‐march‐2020. Accessed June 11, 2020.
- 3. Mateen BA, Dennis JM, Duncan A, et al. A geo‐temporal survey of hospital bed saturation across England during the first wave of the COVID‐19 Pandemic. 10.1101/2020.06.24.20139048. [DOI] [PMC free article] [PubMed]
- 4. HSJ‐NHS block books almost all private hospital sector capacity to fight covid‐19. By James Illman 21 March 2020.
- 5. Bongaerts D, Mazzola F, Wagner X. Closed for business. London: Centre for Economic Policy Research; 2020. https://cepr.org/active/publications/discussion_papers/dp.php?dpno=14814. [Google Scholar]
- 6. The Chancellor’s summer economic update: Background briefing Wednesday 8 July. http://researchbriefings.files.parliament.uk/documents/CBP‐8957/CBP‐8957.pdf. Accessed July 31, 2020.
- 7. NICE . How NICE measures value for money in relation to public health interventions. 1 September 2013. nice.org.uk/guidance/lgb10. Accessed June 26, 2020
- 8. The Human Mortality Database Department of Demography at the University of California . Max Planck Institute for Demographic Research, Center on the Economics and Development of Aging (CEDA). 2020. www.mortality.org. Accessed July 30, 2020.
- 9. COVID‐19 Government Response Stringency Index Blavatnik School of Government. University of Oxford. https://www.bsg.ox.ac.uk/research/research‐projects/coronavirus‐government‐response‐tracker. Accessed June 30, 2020.
- 10. ONS . Deaths registered weekly in England and Wales, provisional: week ending. 26 June 2020.
- 11. ONS National life tables: UK. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/datasets/nationallifetablesunitedkingdomreferencetables. Accessed June 10, 2020.
- 12. HMRC coronavirus (COVID‐19) statistics. https://www.gov.uk/government/collections/hmrc‐coronavirus‐covid‐19‐statistics. Accessed June 11, 2020.
- 13. ONS Monthly GDP and main sectors to four decimal places. https://www.ons.gov.uk/economy/grossdomesticproductgdp/datasets/monthlygdpandmainsectorstofourdecimalplaces. Accessed June 30, 2020.
- 14. Bank of England Monetary Policy Report May 2020. https://www.bankofengland.co.uk/‐/media/boe/files/monetary‐policy‐report/2020/may/monetary‐policy‐report‐may‐2020#. Accessed June 11, 2020.
- 15. Philpotts E GP urgent cancer referrals decline by more than 70% as 'fewer patients come forward' Pulse Today 24 April 2020. http://www.pulsetoday.co.uk/clinical/clinical‐specialties/respiratory‐/gp‐urgent‐cancer‐referrals‐decline‐by‐more‐than‐70‐as‐fewer‐patients‐come‐forward/20040662. Accessed June 11, 2020.
- 16. NHS England Monthly Hospital Activity Data. https://www.england.nhs.uk/statistics/statistical‐work‐areas/hospital‐activity/monthly‐hospital‐activity/mar‐data/ Accessed June 11, 2020.
- 17. NHS Digital Appointments in General Practice ‐ April 2020. https://digital.nhs.uk/data‐and‐information/publications/statistical/appointments‐in‐general‐practice/april‐2020. Accessed June 30, 2020.
- 18. Killgore WDS, Cloonan SA, Taylor EC, Dailey S. Letter to the Editor. Loneliness: a signature mental health concern in the era of COVID‐19. Psychiatry Res. 2020;290:113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Valabhji J, Holman N, Knighton P, et al. Type 1 and type 2 diabetes and COVID‐19 related mortality in England: a cohort study in people with diabetes. Lancet Diabetes Endocrinol. 2020. 10.1016/S2213-8587(20)30272-2 [Epub ahead of print]. PMCID: PMC7426088 PMID: 32798472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. NHS Digital National Diabetes Audit ‐ Report 2 Complications and Mortality, 2017‐18 Audit Publication Date:13 Dec 2019. https://digital.nhs.uk/data‐and‐information/publications/statistical/national‐diabetes‐audit/report‐2–complications‐and‐mortality‐2017‐18. Accessed June 10, 2020.
- 21. Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ‐5D (UKPDS 62). Med Decision Making. 2002;22:340‐349. [DOI] [PubMed] [Google Scholar]
- 22. Beaudet A, Clegg J, Thuresson P, Lloyd A, McEwan P. Review of utility values for economic modeling in type 2 diabetes. Value Health. 2014;17(4):462‐470. [DOI] [PubMed] [Google Scholar]
- 23. Gentry EP, Viscusi WK. The fatality and morbidity components of the value of a statistical life. J Health Econ. 2016;46:90‐99. [DOI] [PubMed] [Google Scholar]
- 24. Murphy KM, Topel RH. The value of health and longevity. J Polit Econ. 2006;114:871‐904. [Google Scholar]
- 25. The Intensive Care National Audit and research centre (ICNARC) report on COVID‐19 in critical care. 2020.
- 26. Reference Cost Collection: National Schedule of Reference Costs ‐ Year 2017–18 ‐ NHS trust and NHS foundation trusts. https://www.england.nhs.uk/national‐cost‐collection/. Accessed June 30, 2020.
- 27. Slides and datasets on coronavirus: 26 June 2020. https://www.gov.uk/government/publications/slides‐and‐datasets‐on‐coronavirus‐26‐june‐2020
- 28. Preprint report Docherty et al . Features of 16,749 hospitalised UK patients with COVID‐19 using the ISARIC WHO Clinical Characterisation Protocol. 10.1101/2020.04.23.20076042. [DOI]
- 29. Shavelle RM, Paculdo DR, Kush SJ, et al. Life expectancy and years of life lost in chronic obstructive pulmonary disease: findings from the NHANES III Follow‐up Study. Int J Chron Obstruct Pulmon Dis. 2009;4:137‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mahon J, Oke J, Heneghan C. Declining death rate from COVID‐19 in hospitals in England. June 24, 2020 article for The Centre for Evidence‐Based Medicine CEBM. https://www.cebm.net/covid‐19/declining‐death‐rate‐from‐covid‐19‐in‐hospitals‐in‐england/. Accessed July 1, 2020.
- 31. Layard R, Clark A, De Neve J‐E, et al. When to release the lockdown: A wellbeing framework for analysing costs and benefits. Center for Economic Performance at the LSE, Occasional paper 49. http://eprints.lse.ac.uk/id/eprint/104276.
- 32. Goldstein JR, Lee RD. Demographic Perspectives on Mortality of COVID‐19 and other Pandemics. NBER Working Paper 27043. https://ideas.repec.org/p/nbr/nberwo/27043.html.
- 33. Braun J, Loyal L, Frentsch M, et al. Presence of SARS‐CoV‐2 reactive T cells in COVID‐19 patients and healthy donors. medRxiv. 2020. 10.1101/2020.04.17.20061440. [DOI] [PubMed] [Google Scholar]
- 34. Grifoni A, Weiskopf D, Ramirez SI, et al. Targets of T cell responses to SARS‐CoV‐2 coronavirus in humans with COVID‐19 disease and unexposed individuals. Cell. 2020;181:1489‐1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lourenco J, Paton R, Ghafari M, et al. Fundamental principles of epidemic spread the immediate need for large‐scale serological surveys to assess the stage of the SARS‐CoV‐2 epidemic. medRxiv. 2020. 10.1101/2020.03.24.20042291. [DOI] [Google Scholar]
- 36. Stedman M, Davies M, Lunt M, et al. A phased approach to unlocking during the COVID‐19 pandemic – Lessons from trend analysis. Int J Clin Pract. 2020;7:e13528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dimdore‐Miles O, Miles D. Assessing the spread of the novel coronavirus in the absence of mass testing. Covid Economics. 2020;16:161‐176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wieland T.Flatten the Curve! Modelling SARS‐CoV‐2/COVID‐19 Growth in Germany on the County Level. 2020. https://www.medrxiv.org/content/10.1101/2020.05.14.20101667v3.
- 39. Friston KJ, Parr T, Zeidman P, et al. Dynamic causal modelling of COVID‐19. Wellcome Open Res. 2020;5:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Levitt M. The corona chronologies. https://www.dropbox.com/s/r4gxdvlcnrxet1i/1.The_Corona_Chronologies.%20Part%20I%20‐%20China.%20Part%20II.%20Rest_of_World_Michael_Levitt%2CStanford_r.pdf?dl=0. Accessed June 30, 2020.
- 41. Lerner A, et al. COVID‐19 serology studies workshop: meeting report. Immunity. 2020. https://www.cell.com/immunity/pdf/S1074‐7613(20)30267‐3.pdf. Accessed June 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Born B, Dietrich AM, Müller GJ. Do lockdowns work? A counterfactual for Sweden. Covid Economics CEPR Discussion Papers 14744, C.E.P.R. Discussion Papers. 2020. https://www.cell.com/immunity/pdf/S1074‐7613(20)30267‐3.pdf. Accessed June 1, 2020. [Google Scholar]
- 43. Krueger D, Uhlig H, Xie T. “Macroeconomic dynamics and reallocation in an epidemic. Covid Economics NBER Working Papers 27047, National Bureau of Economic Research, Inc. 2020. [Google Scholar]
- 44. Financial Times Coronavirus tracked: the latest figures as countries start to reopen. https://www.ft.com/content/a26fbf7e‐48f8‐11ea‐aeb3‐955839e06441. Accessed June 12, 2020
- 45. Deb P, Furceri D, Ostry JD, Tawk N. The economic effects of Covid‐19 containment measures. COVID Economics, CEPR The Centre for Economic Policy Research (CEPR) COVID ECONOMICS ISSUE 19 18 MAY 2020. 2020. [Google Scholar]
- 46. Bonadio B, Huo Z, Levchenko AA, Pandalai‐Nayar N. Global Supply Chains in the Pandemic. NBER Working Paper 27224, May 2020. [DOI] [PMC free article] [PubMed]
- 47. Aum S, Lee SY, Shin Y. Doesn't need lockdowns to destroy jobs: the effect of local outbreaks in Korea. CEPR Discussion Paper 14822. 2020. [DOI] [PMC free article] [PubMed]
- 48. Coibion O, Gorodnichenko Y, Weber M. “Labor markets during the Covid‐19 crisis: A preliminary view. COVID Economics The Centre for Economic Policy Research (CEPR) COVID ECONOMICS ISSUE 19 18 MAY 2020. 2020. [Google Scholar]
- 49. Coibion O, Gorodnichenko Y, Weber M. The cost of the COVID‐19 crisis: Lockdowns, macroeconomic expectations, and consumer spending. Covid Economics The Centre for Economic Policy Research (CEPR) COVID ECONOMICS ISSUE 19 18 MAY 2020. 2020. [Google Scholar]
- 50. ONS . A05 SA: employment, unemployment and economic inactivity by age group (seasonally adjusted). https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/datasets/employmentunemploymentandeconomicinactivitybyagegroupseasonallyadjusteda05sa. Accessed June 30, 2020.
- 51. ONS Deaths involving COVID‐19, England and Wales: deaths occurring. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19englandandwales/previousReleases. Accessed June 30, 2020.
- 52. ONS coronavirus (COVID‐19) infection survey pilot: age specific Mortality rate. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/previousReleases. Accessed June 30, 2020.
- 53. Comas‐Herrera A, Joseba Zalakaín J, Charles Litwin C, et al. Mortality associated with COVID‐19 outbreaks in care homes: early international evidence. https://ltccovid.org/2020/04/12/mortality‐associated‐with‐covid‐19‐outbreaks‐in‐care‐homes‐early‐international‐evidencePDF. Accessed June 26, 2020.
- 54. DELVE Initiative . Scoping Report on Hospital and Health Care Acquisition of COVID‐19 and its Control. DELVE Report No. 3. 2020. http://rs‐delve.github.io/reports/2020/07/06/nosocomial‐scoping‐report.html. Accessed June 30, 2020.


