To the Editor,
Quantitative and qualitative changes in peripheral blood cells have been described in adults with coronavirus disease 2019 (COVID‐19). 1 , 2 , 3 , 4 , 5 This retrospective study aims to define the peripheral blood alterations in children with COVID‐19 and compare them with patients with similar symptoms without COVID‐19.
Children admitted to the emergency department with symptoms including fever, sore throat, rhinorrhea, and cough during April 1‐15, 2020 were tested for SARS‐CoV‐2 by quantitative real‐time reverse transcription‐polymerase chain reaction from nasal and oropharyngeal swab samples. All patients’ complete blood count (CBC) and peripheral smear (Siemens ADVIA 2120i hematology analyzer with auto slide) were done on admission. CBC values were recorded and assessed according to age‐specific intervals. 6 Peripheral blood smears were evaluated blindly, and differential counts were formulated by manual counting, including reactive lymphocytes. C‐reactive protein (CRP) values noted.
The data were expressed as mean ± SD. Student's t‐test was used to compare the means, and the Mann‐Whitney U test was used to compare two independent groups. Chi‐square test was used to distribute the percentage of categorical data between groups. Pearson correlation was used to assess the relationship between two quantitative, continuous variables. P < .05 was considered significant.
Thirty symptomatic children were positive for SARS‐CoV‐2, and the remaining 40 symptomatic children were negative. All patients were hospitalized; however, there was not any critically ill patient, and none of them required intensive care. All patients recovered and discharged at the end of the isolation period (14 days).
The mean age of the whole cohort was 8.11 ± 5.71 years (4 months‐17 years). There was not any age and gender difference (P > .05). CBC parameters and CRP values of the patients with SARS‐CoV‐2 test‐positive and ‐negative groups are given in Figure 1. Of note, a positive patient had a diagnosis of aplastic anemia. The mean hemoglobin value of SARS‐CoV‐2 test‐positive and ‐negative groups was 13.1 ±1.7 g/dL (7.7‐6.4) and 12.4 ± 1.9 g/dL (8.3‐17.1), respectively (P > .05). Within the SARS‐CoV‐2 test‐positive group, two patients (6.7%) had leukocytosis, four patients (13.3%) had leukopenia, and nine (30%) of them had lymphopenia. Twelve patients (30%) with test negative also had lymphopenia. Reactive lymphocytes were noted in 85.1% of the peripheral smears of the whole cohort; these figures were 77.8 and 90% in the SARS‐CoV‐2 test‐positive and ‐negative groups. Mean absolute reactive lymphocyte counts of SARS‐CoV‐2 test‐positive and ‐negative groups were 0.7 ± 0.7 × 109/L (0‐2.9) and 1.2 ± 1.3 × 109/L (0‐ 6.3), respectively (P = .027). Four patients (13.3%) with test‐positive and 10 patients (25%) with negative‐result groups had neutrophilia. Seven (23.3%) COVID‐19 patients had neutropenia; one of them was the patient with aplastic anemia, whereas three (7.5%) patients with test negative had neutropenia. The mean CRP level of the SARS‐CoV‐2‐positive group was lower than the SARS‐CoV‐2‐negative group (P = .006).
FIGURE 1.
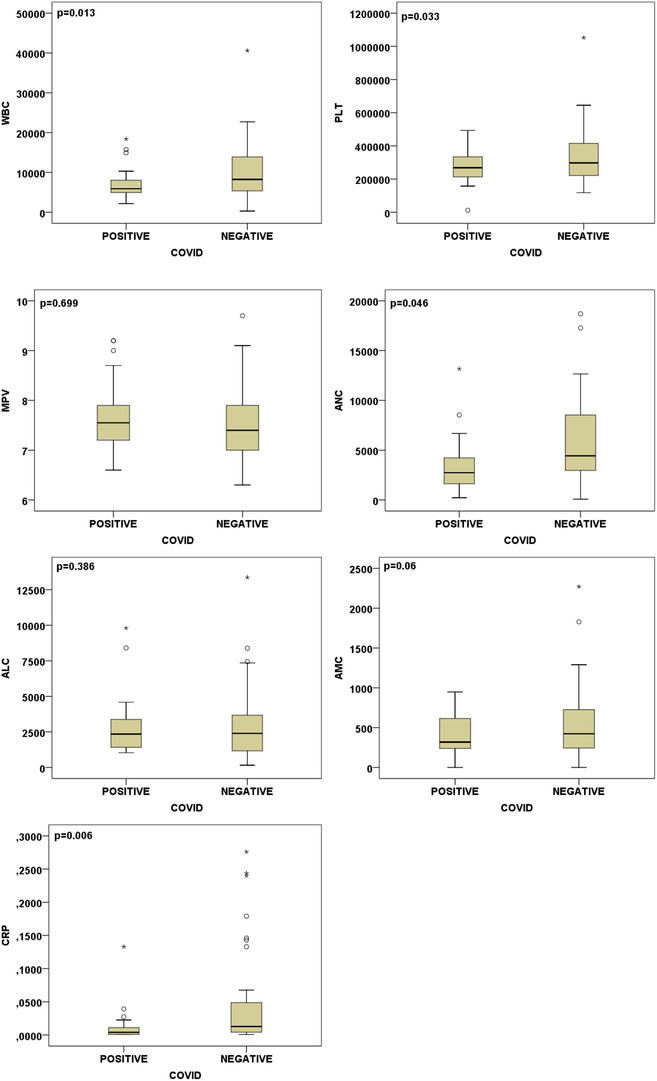
Scatter box plot of blood count parameters and CRP levels of the patients with SARS‐CoV‐2 test‐positive and ‐negative groups. ALC, absolute lymphocyte count; AMC, absolute monocyte count; ANC, absolute neutrophil count; ARL, absolute reactive lymphocyte; CRP, C‐reactive protein; MPV, mean platelet volume; WBC, white blood cell
In the whole cohort, thrombocytopenia was detected in four patients; one of them was the patient with aplastic anemia and COVID‐19, the remaining three were in the SARS‐CoV‐2‐negative group. Thrombocytosis was noted in one COVID‐19‐negative patient.
In the peripheral smears of children with COVID‐19, vacuolated monocytes (n = 3; 13.3%) and hypergranulation/lobulation abnormalities in neutrophils (n = 11; 36.7%) were noted. The respective figures within the non‐COVID‐19 group were n = 4 (10.0%) and n = 9 (22.5%). Although the MPV values were within the normal range, 20% of the COVID‐19 patients had giant platelets; however, giant platelets were also noted in 27.5% of the negative patients.
In adults, the most common hematological findings of COVID‐19 include lymphocytopenia, neutrophilia, thrombocytopenia, and, less frequently, thrombocytosis. 1 , 2 , 3 , 4 , 5 In our study, the majority of the SARS‐CoV‐2‐infected children had a normal leukocyte count. Despite normal leukocyte count, lymphopenia, neutropenia, and neutrophilia were noted in 30.0, 23.3, and 13.3% of children, respectively. Neutropenia has not been previously reported in adults affected by the disease. Viral infections are the common etiological factor of neutropenia. 6 SARS‐CoV‐2 might also be added as a causative agent of neutropenia. In response to stress and antigenic stimulation, reactive lymphocytes appear in the blood. 7 They were detected in both the test‐positive and ‐negative groups. Although a significant difference was detected in leukocyte, platelet, neutrophil, and monocyte counts, many patients’ values were in normal limits; so the leukocyte count and differentials could not help to distinguish COVID‐19 from other symptomatic patients. The CRP level might be more helpful for differential diagnosis.
In a metaanalysis, low platelet count has been associated with increased severity and increased mortality in adults with COVID‐19. 2 The absence of thrombocytopenia in our series may be related to the better clinical prognosis of the disease in children. Morphological abnormalities in neutrophil lineage and platelet morphology in adults with COVID‐19, mainly large platelets, has been reported. 8 We noted nonspecific dysplastic changes in the smear of patients. In children with COVID‐19, the upregulation of proinflammatory cytokines in the blood has been reported. 9 The dysregulation of the immunological environment might be related to those altered cytokines.
In conclusion, leukocyte and neutrophil counts were lower in children with COVID‐19. Lymphopenia and reactive lymphocytosis, dysplastic changes of granulocytes, and platelets, although not specific and diagnostic, could be noted.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- 1. Fan BE, Chong VCL, Chan SSW, et al. Hematologic parameters in patients with COVID‐19 infection. Am J Hematol. 2020;95(6):E131‐E134. [DOI] [PubMed] [Google Scholar]
- 2. Henry BM, de Oliveira MHS, Benoit S, et al. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID‐19): a meta‐analysis. Clin Chem Lab Med. 2020;58(7):1021‐1028. [DOI] [PubMed] [Google Scholar]
- 3. Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease in 2019 (COVID‐19) infections: a meta‐analysis. Clin Chim Acta. 2020;506:145‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang F, Nie J, Wang H, et al. Characteristics of peripheral lymphocyte subset alteration in COVID‐19 pneumonia. J Infect Dis. 2020;221(11):1762‐1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walkovich KL, Newburger PE. Leukopenia. In: Kliegman RM, Stanton BF, St Geme JW III, Schor NF, Behrman RE, eds. Nelson Textbook of Pediatrics. 20th ed. International Edition: Elsevier; 2016:1047‐1055. [Google Scholar]
- 7. Bain BJ. Blood Cells. 5th ed. Wiley Blackwell; 2015. [Google Scholar]
- 8. Zini G, Bellesi S, Ramundo F, d'Onofrio G. Morphological anomalies of circulating blood cells in COVID‐19. Am J Hematol. 2020;95(7):870‐872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Molloy EJ, Bearer CF. COVID‐19 in children and altered inflammatory responses. Pediatr Res. 2020. 10.1038/s41390-020-0881-y [DOI] [PubMed] [Google Scholar]


